Abstract
The study was to investigate the feasibility and effectiveness of posterior-only approach combining with puncture drainage under CT-guide in staged treatment of thoracic and lumbar spinal tuberculosis with flow injection abscess. We retrospectively analyzed 15 patients (came from 72 cases with thoracic and lumbar spinal tuberculosis) with flow injection abscesses underwent surgery from January 2007 to February 2009, and evaluated the American Spinal Injury Association (ASIA) scoring system of nerve function, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), abscess absorption time and the Oswestry Disability Index (ODI), preoperatively and postoperatively. 15 patients were followed up for 13-37 months, no recurrence of tuberculosis, no fixation loosening and neurologic symptoms aggravated. The flow injection abscesses are absorbed within 3-6 months postoperative operation. In final follow-up, ESR went down to 5.2±2.1 mm/h from preoperative 79.6±14.8 mm/h, CRP decreased from preoperative 49.3±7.5 mg/L to 1.8±0.7 mg/L, ODI changed from 75.13±20.15 to 16.72±8.62, all of them changed significantly (P<0.05). In conclusions, one-stage posterior debridement, interbody fusion, pedicle screw fixation and two-stage CT-guided interventional therapy were safe and effective in treatment of the thoracic and lumbar spinal tuberculosis with flow injection abscess.
Keywords: Spinal tuberculosis, thoracic and lumbar spine, flow injection abscess, staged treatment, puncture drainage
Introduction
In recent years, the incidence of tuberculosis has continuously increased worldwide, together with increased mobility, the continuous appearance of drug resistant tuberculosis, and increased incidence of autoimmune diseases in the general population. Spinal tuberculosis is the most common in bone tuberculosis that causes the most severe damage such as serious kyphosis and paralysis, except general symptoms of TB; and it seriously affects the quality of life of patients [1-3]. According to statistics, spinal tuberculosis accounts for 50% of bone tuberculosis; and among patients with spinal tuberculosis, 75% of cases are accompanied by paraspinal abscesses and/or flow injection abscess [4]. However, no studies have evaluated the incidence rate of flow injection abscess. Due to the continuous development of surgical techniques and internal fixation devices, more scholars tend to prefer one-stage posterior debridement, interbody fusion and pedicle screw fixation for patients with operative indications; followed by treatment of first-line anti-tuberculosis drugs for 12-18 months after surgery. This study focuses on one-stage posterior surgery alone and two-stage puncture drainage under CT-guidance for patients with thoracic and lumbar spinal tuberculosis with flow injection abscess.
Materials and methods
General information
From January 2007 to February 2009, our department treated 70 cases of thoracic and lumbar spinal tuberculosis; and among them, 15 cases were accompanied with flow injection abscess (eight cases were bilateral). Among these 15 cases, eight patients were male and eight patients were female patients, and their age ranged from 18 to 68 years old with an average age of 37.7 year old. The course of the disease lasted for 3-23 months. These 15 cases involved 37 vertebral bodies: two cases of T10, four cases of T11, four cases of T12, three cases of L1, four cases of L2, four cases of L3, six cases of L4, seven cases of L5, three cases of S1, and seven cases that involved three kinds of vertebral bodies. In addition, 14 cases had neurological symptoms according to American Spinal Injury Association (ASIA) grade: two cases with grade A, four cases with grade B, five cases with grade C, three cases with grade D, and one case with grade E (Table 1). Preoperative erythrocyte sedimentation rate (ESR) was 40-117 mm/h with an average of 79.6±14.8 mm/h, and C-reactive protein (CRP) was 22.7-71.6 mg/L with an average of 49.3±7.5 mg/L. All cases were treated with one-stage posterior debridement, interbody fusion, pedicle screw fixation, and two-stage puncture drainage under CT-guidance; followed by local administration of anti-tuberculosis drugs.
Table 1.
Details of patients
| Cases | Age | Gender | Involved lesion | Location of abscess | Preoperative ASIA | Time of abscess absorption (mon) |
|---|---|---|---|---|---|---|
| 1 | 35 | Male | L2-L3 | Left | D | 3 |
| 2 | 21 | Female | T10-11 | Both | C | 4 |
| 3 | 25 | Female | T11-L1 | Both | D | 3 |
| 4 | 18 | Male | L4-L5 | Both | A | 3 |
| 5 | 29 | Female | L3-L5 | Right | C | 4 |
| 6 | 28 | Male | L4-L5 | Both | B | 5 |
| 7 | 37 | Female | L5-S1 | Right | E | 3 |
| 8 | 56 | Female | L1-L2 | Left | B | 6 |
| 9 | 61 | Male | L3-L5 | Both | C | 4 |
| 10 | 31 | Female | T11-T12 | Right | B | 3 |
| 11 | 41 | Male | T12-L2 | Left | A | 3 |
| 12 | 28 | Female | T10-T12 | Both | C | 5 |
| 13 | 37 | Female | L5-S1 | Both | B | 3 |
| 14 | 64 | Male | L4-S1 | Right | D | 6 |
| 15 | 55 | Female | L2-L4 | Both | C | 3 |
ASIA, the American Spinal Injury Association.
Treatment methods
Preoperative preparation
Liver and renal function, tuberculosis antibody, ESR and CRP tests, as well as chest X-ray, lumbar X-ray, CT exam and MRI exam, were performed in all patients. Active pulmonary tuberculosis was also ruled out. Preoperative regular quadruple chemotherapy (0.3 g of isoniazid po qd, 0.45 mg of rifampicin po qd, 0.45 mg of pyrazinamide po qd, and 0.75 mg of ethambutol po qd) with anti-tuberculosis drugs were administered for 2-4 weeks with auxiliary liver-protective drug treatment. One case presented with jaundice with a marked increased in uric acid, and was administered with anti-tuberculosis drugs.
Posterior open surgical procedure
Using tracheal intubation with general anesthesia, the patient was placed in prone position. With the pathologic vertebrae centered, two vertebral bodies were exposed bilateral to the lateral facet joint. A pedicle screw was inserted between adjacent vertebral bodies via C-arm X-ray positioning, the need for insertion into the pathologic vertebrae depended on its destruction, and long-segment fixation was adopted. First, the milder side was temporarily fixed with a moderate pre-bending titanium rod to expose the spinal canal and protect the spinal cord and nerve root. The severe side of the articular process and transverse process was bit to reveal the intervertebral space, and 1-2 intercostal nerves were cut when necessary. The necrotic intervertebral disc and invasion cartilage endplate were removed; and the pathologic vertebrae and peripheral abscess, sequestrum, caseous necrosis and granulation tissues were shaved.
The operation area was irrigated with saline solution after debridement. After irrigation, stripe bone grooves were made along the residential vertebral bodies with a bone knife, and embedded the same size allograft bone or self-iliac bone into the grooves. After thorough irrigation and strict hemostasis, the operation area was treated with 1 g of streptomycin and 0.3 g of isoniazid, and fixed the other side of the connection rod using a screw. Debridement of the opposite side must be done, if needed. Correct kyphosis by internal fixation force and distraction function according to the situation of lost vertebral body and kyphosis was revealed in the X-ray before the operation. Correction of the kyphosis was confirmed by C-arm X-ray, the drainage was fixed, and the wound was closed in layers.
The two-stage treatment
General vital signs, double-limb sensory conditions, and the amount of drainage were closely observed after surgery. Drainage was pulled out 24-72 hours after the operation, and this period was delayed in particular cases. Postoperative antibiotic prophylaxis and routine anti-tuberculosis treatment was performed, and ESR and CRP were re-examined. At 1-2 weeks after the operation, the location and depth of the puncture was identified under CT-guidance in supine position. Then, the area was sterilized, drapes were placed, and 2% lidocaine local anesthesia was administered.
After the puncture, the depth was identified via CT scan (Figure 1). The needle core was pulled out, drew pyogenic fluids, and washed with large amounts saline solution. Then, 0.3 g of isoniazid was infused. The needle core was pulled out and a guide wire was placed. The puncture needle was pulled out after the guide wire reached the vomica, and the sheath core and guide wire were pulled out after placing the bile duct sheath. The strengthened wire was lead into the vomica, the bile duct sheath was dropped, and an indwelling pigtail catheter was placed. Fluid was extracted from the vomica daily and infused with 0.3 g of isoniazid. The catheter was removed when the amount of extracted fluid was ≤5 ml. During this period, systemic anti-tuberculosis and hepatic protection treatment was administered. A periodic review was carried-out on the ESR, CRP and X-ray results of the thoracic and lumbar vertebra, as well as the CT results of the abscess site.
Figure 1.
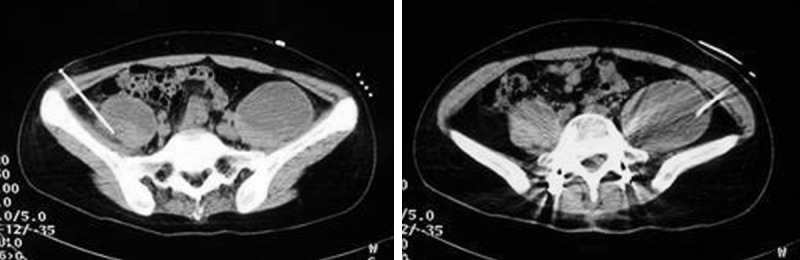
CT-guided drainage of abscess. The needle core was pulled out, drew pyogenic fluids, and washed with large amounts saline solution. Then, 0.3 g of isoniazid was infused. The needle core was pulled out and a guide wire was placed. The puncture needle was pulled out after the guide wire reached the vomica, and the sheath core and guide wire were pulled out after placing the bile duct sheath. The strengthened wire was lead into the vomica, the bile duct sheath was dropped, and an indwelling pigtail catheter was placed.
Evaluation indicators
Pre-operation and end-stage follow-up of the spinal cord injury were evaluated according to the ASIA Classification, assimilation and organization time of the paraspinal abscess and/or flow injection abscess, and pre- and post-operation changes in ESR and CRP were evaluated. The functional status of each patient for both pre-treatment and final follow-up was graded using the Oswestry disability index (ODI).
Statistical analysis
Using SPSS 19.0 software, ODI scores, ESR and CRP were statistically analyzed by an independent-samples t-test preoperatively, postoperatively and/or during follow-up (Tables 1 and 3); and neurological function was statistically analyzed by Wilcoxon signed rank test preoperatively (Table 2) and during follow-up. Discrepancy of the normal distribution was analyzed by rank-sum test with a significance level of 0.05. Results are reported as mean ± standard deviation (SD).
Table 3.
Changes of ESR and CRP of all patients
| Index | Pre-operation | One week after one stage* | Two weeks after two stages# | Final follow up※ |
|---|---|---|---|---|
| ESR (mm/h) | 79.6±14.8 | 87.3±6.7 | 7.8±3.1 | 5.2±2.1 |
| CRP (mg/L) | 49.3±7.5 | 56.7±3.8 | 3.4±1.2 | 1.8±0.7 |
ESR, erythrocyte sedimentation rate; CRP, C-reactive protein;
There is no significant statistic difference between one week after one stage and pre-operation, P>0.05;
There is significant statistic difference between two weeks after two stage and pre-operation, final follow up and pre-operation, P<0.05;
There is significant statistic difference between two weeks after two stage and pre-operation, final follow up and pre-operation, P<0.05.
Table 2.
Neurological function grading of all cases by ASIA in pre-operation and final follow-up
| ASIA | Cases | Final follow-up (case) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| A | B | C | D | E | ||
| A | 2 | 1 | 1 | |||
| B | 4 | 1 | 2 | 1 | ||
| C | 5 | 5 | ||||
| D | 3 | 3 | ||||
| E | 1 | 1 | ||||
ASIA, American Spinal Injury Association. The neurological function was statistically analyzed by Wilcoxon signed rank test preoperatively and during follow-up, P<0.05.
Results
Follow-up period ranged from 13-37 months with an average follow-up period of 18.5 months. Thorough planted bone fusion was observed in all cases by X-ray examination (some by CT examination). Fusion time was 4-8 months with an average of 5.8 months. No bone nonunion or pseudarthrosis was found until the final follow-up. No sinus formation and mixed infection of postoperative wound and puncture drainage area was found. Paraspinal abscesses and/or flow injection abscess were organized within 3-6 months after the operation (Table 1).
Neuronal functions of the 15 cases recovered to different degrees. Among these cases, eight cases fully recovered at the time of final follow-up, in which two cases of Grade A recovered to Grade B (one case) and Grade C (one case); while four cases of Grade B recovered to Grade C (one case), Grade D (two cases) and complete recovery (one case), in which all Grade B and C cases recovered eventually (Table 2). Based on statistical analysis, neuronal function significantly improved (P<0.05).
Changes in ESR and CRP before operation, one week after one-stage posterior operation, and two weeks after two-stage intervention operation are shown in “Table 3”. There was no significant improvement in ESR and CRP at one week after one-stage posterior surgery and pre-operation (P>0.05). ESR and CRP recovered to normal levels at two weeks after two-stage intervention operation, which significantly improved compared to final follow-up and pre-operation (P<0.05).
Average ODI was 75.13±20.15 before operation and 16.72±8.62 upon final follow-up, and the difference was statistically significant (t=21.42, P<0.001).
Discussion
Characteristics of thoracic and lumbar spinal tuberculosis with flow injection abscess
Flowing abscess of thoracic and lumbar spinal tuberculosis has irregularly spread to a large range. Paraspinal abscesses, after being accumulated to a certain amount, causes increased pressure, penetrates the periosteum, moves downward along the muscular fasciae space, and forms an abscess in sites away from the lesions. The thoracic and lumbar fester often accumulates in the sheath of the psoas major and forms a psoas abscess, while the lumbosacral vertebrae fester often accumulates in the bilateral fossa iliaca and forms an abscess, or penetrates the lumbar fascia to the lumbar triangle and forms an abscess, or flows to the lesser trochanter of the femur and forms a deep abscess of the groin [3,5].
There are various types of severe bone destruction of the thoracic and lumbar spine. Majority of these include tuberculosis of the intervertebral space, subperiosteum, and center of the vertebral body; and these can easy implicate the adjacent vertebrae and present progress or jumpy damage. There were seven cases with severely damaged vertebral bodies (≥3), which accounts for 46.7% (7/15); and all appears to be kyphosis.
The canalis vertebralis is liable to be damaged, in which neurological function is mostly impaired. Paraspinal abscesses can easily to invade the canalis vertebralis, which could make the spinal cord and nerve root immerse in the fester for a long period of time and cause possible clinical manifestations of neurological function even without neurothlipsis. Since multiple vertebral bodies are frequently implicated by thoracic and lumbar spinal tuberculosis with flow injection abscess, severe bone destruction and kyphosis are liable to occur; which could cause spinal cord and nerve root compression [6].
Difficulties in the treatment of flowing abscess are as follows: (1) the wall of the abscess is too thick, which causes insufficient local blood supply and lower concentration of the drug; (2) drug-resistance is likely to be developed; (3) the long period of time of immersion in the fester makes tuberculosis more toxic; (5) the treatment time for anti-tuberculosis needs to be extended for flowing abscesses to increase drug reaction and reduce patient compliance [7,8].
The choice of operation for thoracic and lumbar spinal tuberculosis with flow injection abscess
Currently, patients with spinal tuberculosis accompanied with small amounts of paraspinal abscess can achieve complete remission after anti-tuberculosis treatment if there are no neurological signs and evident kyphosis; however, if patients have clear indications for surgery as mentioned above, anti-tuberculosis treatment with one-stage posterior debridement, interbody fusion and pedicle screw fixation are often adopted to achieve complete remission [9,10]. For patients with flow injection abscess, simple flow injection abscess and posterior operation usually fails to achieve a satisfactory therapeutic effect. Therefore, some scholars [11] propose anterior debridement, interbody fusion and pedicle screw fixation or anterior debridement, interbody fusion and posterior internal fixation for thoracic and lumbar spinal tuberculosis with flow injection abscess. They consider that an anterior approach could thoroughly remove the abscess and sequestrum under direct vision, bone grafting and internal fixation, to ensure the stability for the spine; thereby achieving a good therapeutic effect. Lee et al. [12] agreed with the treatment plan of posterior debridement, interbody fusion and internal fixation; and argues that an anterior operation would cause a lot of postoperative complications, especially together with an iliac abscess, in which the topographic structure is complicated with serious injuries and poor patient tolerance. Guzey [13] and Rath [14] et al. consider that an abscess could not be thoroughly removed by simple posterior surgery, particularly for patients with flow injection abscess; while anterior debridement exhibits a marked treatment effect on tuberculosis, but with major surgical trauma.
Although an anterior debridement operation is performed under direct vision, the author believes that operation time is longer with more surgical trauma and bleeding. In particular, during debridement of the bilateral iliac abscess, anterior vessels and nerves are likely to be injured with more postoperative complications [2,3]. Furthermore, the effect of the operation of the so-called “thorough debridement” is relative, in which an anterior approach could not thoroughly clear the injuries. Postoperative recurrence of spinal tuberculosis is mostly caused by low concentrations of anti-tuberculosis drugs on the injured site, emergence of drug-resistant strains, or postoperative chemotherapy irregularities. If simple posterior surgery is performed without dealing with paraspinal flow abscess, a longer time for abscess absorption and organization can be observed even without absorption; and ESR and CRP will not show any decrease (Figure 2). ASIA grade and ODI for all patients enrolled in this study markedly improved. However, ESR and CRP did not improve. It has been reported that [15] this might be associated with surgical stress. However, the author believes that ESR and CRP should significantly decrease one week after surgery in most patients with spinal tuberculosis; which may be related to the flow injection abscess residue in front of the spine.
Figure 2.

One patient with thoracic spinal tuberculosis combined with left paraspinal abscess (A) after nine months of posterior-only surgery was shown no absorption of the abscess by the cross-section and coronary CT-scan (B, C).( ESR: 79.2 mm/h, CRP: 43 mg/L).
The feasibility of CT-guided puncture and drainage for thoracic and lumbar spinal flow injection abscess
Some surgeons [16] proposed interventional therapy by puncture drainage to clear the abscess and local drug delivery for spinal tuberculosis with paraspinal abscesses, to achieve a better therapeutic effect. Some studies have shown that systemic administration is 2,000-100,000 times when drug concentration is 0.5 µg/ml during systemic chemotherapy and local chemotherapy concentration is 1-50 mg/ml [17,18]. Tuberculosis bacilli can rapidly be killed by persistent and high concentrations of local drug delivery, effectively preventing liver and kidney dysfunction caused by anti-tuberculosis drugs. ESR, CRP and other inflammatory biomarkers significantly decreased in all 15 patients in this study after two-stage CT-guided puncture drainage and local drug delivery treatments; which shows that tuberculosis was effectively controlled. During follow-up, all abscess organizations in patients were observed in 3-6 months after surgery without recurrence. Nevertheless, attention should be given when administering CT-guided puncture drainage. (1) If the fester is thick and inadequate drainage occurs, the position of the patient should be changed, washing with pressure with copious saline should be done, and multiple puncture drainage in the abscess should be made. However, if this fails, an anterior-lateral open operation must be performed for debridement. In this study, no inadequate drainage occurred among the 15 patients after CT-guided puncture drainage. (2) More negative pressure drainage tubes should be placed often in case of tube blockage and slippage, and the tube has to be sutured closely with the skin. (3) Irrigating fluid oozing over the wound often causes drainage tube blockage. Hence, timely dredging of the tube is needed when this occurs. (4) The mouth of tube is susceptible to infection. Hence precautions such as ensuring adequate tube drainage and timely medication and nursing are necessary (Figure 3).
Figure 3.

A. Preoperative CT showed the formation of bilateral flow injection abscess in lumbar; B. post operative CT showed the disappearance of abscess after the interventional therapy in the final follow-up.
In conclusion, posterior debridement, interbody fusion and internal fixation treatments are effective for neurological changes, but have limited effects in curing tuberculosis with flow abscess. A total of 14 patients in this study presented varying degrees of recovery according to post-operation ASIA grades, especially in patients with grade C and D that achieved complete recovery. ODI rating dramatically decreased and patient function significantly improved after surgery, which is in line with other reports [19,20]. Prompt treatment of the flow injection abscess under CT-guidance and local drug delivery is crucial for the thorough treatment of spinal tuberculosis. This study has some limitations such as small sample size, relative short follow-up time, and the lack of a randomized comparison between a pure posterior approach and an anterior-posterior approach for surgery.
Acknowledgements
This publication was funded in part by the National Natural Science Foundation of China (81171736).
Disclosure of conflict of interest
None.
References
- 1.Moon MS, Moon YW, Moon JL, Kim SS, Sun DH. Conservative treatment of tuberculosis of the lumbar and lumbosacral spine. Clin Orthop Relat Res. 2002;398:40–49. doi: 10.1097/00003086-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Zeng H, Shen X, Luo C, Xu Z, Zhang Y, Liu Z, Wang X. Comparison of three surgical approaches for cervicothoracic spinal tuberculosis: A retrospective case-control study. J Orthop Surg Res. 2015;10:100. doi: 10.1186/s13018-015-0238-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeng H, Wang X, Pang X, Luo C, Zhang P, Peng W, Wu P, Xu Z. Posterior only versus combined posterior and anterior approaches in surgical management of lumbosacral tuberculosis with paraspinal abscess in adults. European Journal of Trauma and Emergency Surgery. 2014;40:607–616. doi: 10.1007/s00068-013-0367-2. [DOI] [PubMed] [Google Scholar]
- 4.Lindahl S, Nyman RS, Brismar J, Hugosson C, Lundstedt C. Imaging of tuberculosis. IV. Spinal manifestations in 63 patients. Acta Radiol. 1996;37:506–511. doi: 10.1177/02841851960373P215. [DOI] [PubMed] [Google Scholar]
- 5.Geraghty A, Kettlewell S, Arestis N. Cholecystocutaneous abscess: Diagnostic difficulty in a groin lump. BMJ Case Rep. 2012:2012. doi: 10.1136/bcr.03.2012.5997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zeng H, Zhang P, Shen X, Luo C, Xu Z, Zhang Y, Liu Z, Wang X. One-stage posterior-only approach in surgical treatment of single-segment thoracic spinal tuberculosis with neurological deficits in adults: A retrospective study of 34 cases. BMC Musculoskelet Disord. 2015;16:186. doi: 10.1186/s12891-015-0640-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Terada Y, Matsunobe S, Nemoto T, Tsuda T, Tonomura S. Contents of chest wall cold abscess flowing into the epidural space in miliary tuberculosis. Chest. 1992;101:590–591. doi: 10.1378/chest.101.2.590-b. [DOI] [PubMed] [Google Scholar]
- 8.Pang X, Shen X, Wu P, Luo C, Xu Z, Wang X. Thoracolumbar spinal tuberculosis with psoas abscesses treated by one-stage posterior transforaminal lumbar debridement, interbody fusion, posterior instrumentation, and postural drainage. Arch Orthop Trauma Surg. 2013;133:765–772. doi: 10.1007/s00402-013-1722-9. [DOI] [PubMed] [Google Scholar]
- 9.Pang X, Wu P, Shen X, Li D, Luo C, Wang X. One-stage posterior transforaminal lumbar debridement, 360 degrees interbody fusion, and posterior instrumentation in treating lumbosacral spinal tuberculosis. Arch Orthop Trauma Surg. 2013;133:1033–1039. doi: 10.1007/s00402-013-1751-4. [DOI] [PubMed] [Google Scholar]
- 10.Pang X, Li D, Wang X, Shen X, Luo C, Xu Z, Zeng H, Wu P, Zhang P, Peng W. Thoracolumbar spinal tuberculosis in children with severe post-tubercular kyphotic deformities treated by single-stage closing-opening wedge osteotomy: Preliminary report a 4-year follow-up of 12 patients. Childs Nerv Syst. 2014;30:903–909. doi: 10.1007/s00381-013-2328-9. [DOI] [PubMed] [Google Scholar]
- 11.Suh KT, Seong YJ, Lee JS. Simultaneous anterior and posterior surgery in the management of tuberculous spondylitis with psoas abscess in patients with neurological deficits. Asian Spine J. 2008;2:94–101. doi: 10.4184/asj.2008.2.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee JS, Moon KP, Kim SJ, Suh KT. Posterior lumbar interbody fusion and posterior instrumentation in the surgical management of lumbar tuberculous spondylitis. J Bone Joint Surg Br. 2007;89:210–214. doi: 10.1302/0301-620X.89B2.17849. [DOI] [PubMed] [Google Scholar]
- 13.Guzey FK, Emel E, Bas NS, Hacisalihoglu S, Seyithanoglu MH, Karacor SE, Ozkan N, Alatas I, Sel B. Thoracic and lumbar tuberculous spondylitis treated by posterior debridement, graft placement, and instrumentation: A retrospective analysis in 19 cases. J Neurosurg Spine. 2005;3:450–458. doi: 10.3171/spi.2005.3.6.0450. [DOI] [PubMed] [Google Scholar]
- 14.Rath SA, Neff U, Schneider O, Richter HP. Neurosurgical management of thoracic and lumbar vertebral osteomyelitis and discitis in adults: A review of 43 consecutive surgically treated patients. Neurosurgery. 1996;38:926–933. doi: 10.1097/00006123-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Lee SH, Sung JK, Park YM. Single-stage transpedicular decompression and posterior instrumentation in treatment of thoracic and thoracolumbar spinal tuberculosis: A retrospective case series. J Spinal Disord Tech. 2006;19:595–602. doi: 10.1097/01.bsd.0000211241.06588.7b. [DOI] [PubMed] [Google Scholar]
- 16.Lazaro D, Nicolas AI, De Castro P. [Diagnostic imaging of sacral osteomyelitis with prevertebral abscess involving erector spinae muscles. Normalization following drainage by needle puncture and specific antibiotic treatment] . Neurologia. 2001;16:376. [PubMed] [Google Scholar]
- 17.An SW, Yoon CJ, Seong NJ, Kang SG, Han HS, Cho JY, Yoon YS, Kim HH, Kim YJ, Woo YN, Kim YS. Inaccessible postoperative abdominal abscess: percutaneous drainage technique with puncture of a sinus tract. J Vasc Interv Radiol. 2013;24:586–591. doi: 10.1016/j.jvir.2012.12.015. [DOI] [PubMed] [Google Scholar]
- 18.Lam J, Henriquez R, Rojas O, Marina V. [Percutaneous puncture and drainage previous to elective surgical resection of a pheochromocytoma presenting as a retroperitoneal abscess: Report of one case] . Rev Med Chil. 2007;135:501–505. [PubMed] [Google Scholar]
- 19.Zhang HQ, Li JS, Zhao SS, Shao YX, Liu SH, Gao Q, Lin MZ, Liu JY, Wu JH, Chen J. Surgical management for thoracic spinal tuberculosis in the elderly: Posterior only versus combined posterior and anterior approaches. Arch Orthop Trauma Surg. 2012;132:1717–1723. doi: 10.1007/s00402-012-1618-0. [DOI] [PubMed] [Google Scholar]
- 20.Shen X, Liu H, Wang G, Pang X, Luo C, Zeng H, Xu Z. The role of single-stage posterior debridement, interbody fusion with titanium mesh cages and short-segment instrumentation in thoracic and lumbar spinal tuberculosis. J Neurosurg Sci. 2015 doi: 10.23736/S0390-5616.16.03333-6. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


