Abstract
Background: The most critical thing in breast augmentation surgery is to determine the location for implant placement. However, few researches on this were carried out in China. We therefore conducted this retrospective study to compare the recovery period, complications and patient satisfaction at two different implant placement locations-the subglandular plane and the subpectoral plane. Methods: A total of 144 patients were included. All of them have undergone primary aesthetic breast augmentation with cohesive silicone gel implant. Then they were divided into two groups according to the implant location: group A (in the subglandular plane) and group B (in the subpectoral plane). Data collected were patient data, surgery-related indicators, recovery, complications and patient satisfaction. Results: Thirty-nine patients were assigned to group A, and 105 patients to group B. In terms of patient data, no significant difference was found in age, follow-up time and the size of prosthesis between the two groups, but there existed statistically significant difference in body mass index (BMI) and the preoperative mammary tissue thickness (P < 0.05). For surgery-related indicators and recovery, group A was better than group B in surgical blood loss, duration of pain and indwelling drainage tube, with statistical significance (P < 0.05). But regarding the complications, significant difference was found only in the nipple-areola numbness (P < 0.05). Overall, 76% of the patients reported they were “satisfied” with the outcome or the outcome was “perfect”. Conclusion: Implant placement in the subglandular plane has a shorter recovery period than that in the subpectoral plane. The occurrence of complications and degree of patient satisfaction are similar in the two groups.
Keywords: Breast augmentation, subglandular, subpectoral
Introduction
According to the American Society of Plastic Surgeons, the number of plastic surgery procedures continues to grow steadily in United States. A total of 15.1 million cosmetic surgery procedures were performed in US in 2013, which have been increased by 3% since 2012. Among them, 290 thousand breast augmentation surgeries were performed in 2013; surgery of this kind continues to be the top cosmetic surgical procedure since 2006 [1]. In china, breast augmentation is also one of the most popular cosmetic procedures. However, there is a lack of research on the recovery period, complications and patient satisfaction of the procedures.
Selecting pocket location for breast implant is the most important decision in breast augmentation [2]. Internationally, there are four main locations: subglandular, subpectoral, subfacial and dual-plane locations. In china, the first two are selected very commonly. In this study, we will compare the recovery period, complications and patient satisfaction of these two kinds of locations.
Patients and methods
A retrospective study was conducted in the Department of Plastic and Reconstructive Surgery of Southwest Hospital, with the approval of the Ethics Committee of the Third Military Medical University. A total of 144 women were included in this study. They underwent primary aesthetic breast augmentation with cohesive silicone gel implant between March 2009 and December 2013. All of them received a subglandular or subpectoral breast implant and attended a follow-up appointment for at least 1 month after surgery. The surgical procedures were performed at the Department of Plastic and Reconstructive Surgery of Southwest Hospital. Patients in group A received breast implants in the subglandular plane, while those in group B received in the subpectoral plane.
Data collected were patient data, surgery-related indicators, recovery, complications and patient satisfaction. Patient data included age, pregnancy, body mass index (BMI), smoking status, surgical time, implant volume, and so on. Surgery-related indicators and recovery involved operative time, surgical blood loss, duration of pain, and duration of hospital stay. And complications and patient satisfaction were included in the follow-up.
Surgery
The volume of breast implant depended on the breast size, thickness of the mammary soft-tissues, stretchability of skin, patient’s height, patient’s expectation and some other factors. All implants were round with textured surfaces. Whether to place them in the subglandular or subpectoral plane was mainly determined by thickness of the mammary soft-tissues and the surgeon’s experience. Intravenous (IV) antibiotics were given once both preoperatively and postoperatively.
The boundaries of implant pocket were marked preoperatively by the surgeon with the patient in standing position. All procedures were performed under general anesthesia. Adrenaline 1/200,000 dilution was injected at the operation sites to reduce surgical blood loss. Axillary or periareolar incision was made in all cases. The surgeon created pocket manually or using blunt dissectors, and then inserted and adjusted the implant manually. Drains were used in most patients based on the surgeon’s preference and the implant pocket.
Satisfaction
Patients were interviewed by telephone about their satisfaction, which included overall satisfaction, satisfaction with breast shape and attitudes toward some complications. The follow-up time was no less than 3 months after breast augmentation. Satisfaction was rated on a scale of 1 to 5, in which 5 = very satisfied, 4 = somewhat satisfied, 3 = neither satisfied nor dissatisfied, 2 = somewhat dissatisfied, and 1 = very dissatisfied.
Statistical analysis
Statistical analysis was performed using the SPSS 17.0 statistical software for Windows. Measurement data (such as average age, BMI, follow-up time, thickness of the mammary tissues, Follow-up time, implant volume, operative time, surgical blood loss, duration of pain, duration of indwelling drainage tube and duration of postoperative hospital stay) were compared with t test. The enumeration data (such as smoking, previous pregnancy, CC and asymmetry/displacement and complications) were analyzed mainly by chi-square statistics. The comparisons of infection, nipple-areola numbness and reoperation rate were made with Fisher’s exact test. The Wilcoxon rank-sum test was used to compare patients’ satisfaction. The ordinal logistic regression was used to analyze all the related factors probably influencing patients’ satisfaction, which was included pre-operative general conditions, surgery-related indicators, post-operation recovery and complications.The significance test was two-tailed. A p value < 0.05 was considered statistical significant.
Results
Patient data
A total of 144 patients were enrolled in our study. The 39 patients in group A received silicone-filled breast implants in the subglandular plane, while the 105 patients in group B received in the subpectoral plane. The average age in group A was 38.1 years (ranged from 22 to 63 years), and in group B was 31.21 years (ranged from 18 to 55 years). BMI ranged from 17.10 to 23.10 kg/m2 (mean = 20.19 kg/m2) in group A, and from 15.20 to 24.70 kg/m2 (mean = 19.17 kg/m2) in group B. The preoperative thickness of mammary soft-tissues was measured by color Doppler ultrasound at later-superior quadrant, with a mean of 9.39 mm in group A, and 7.78 mm in group B. Patients were followed up for a mean of 32.50 months (ranged from 8 to 51 months) in group A, and 30.99 months (ranged from 3 to 57 months) in group B. The mean size of prosthesis was 201.92 ml and 199.62 ml in group A and group B, respectively. There was no significant difference in age, follow-up time, implant volume and smoking status between the two groups, but great significant difference in BMI, the preoperative thickness of mammary tissues and previous pregnancy status (P < 0.05) (Table 1).
Table 1.
Pre-operative general conditions of patients
| Characteristics | Subglandular | Subpectoral | P Value |
|---|---|---|---|
| No. of patients (%) | 39 (27%) | 105 (73%) | |
| Age, years | |||
| Mean (SD) | 38.10 (8.12) | 31.21 (7.54) | 0.00 |
| Range | 22~63 | 18~55 | |
| BMI, kg/m2 | |||
| Mean (SD) | 20.19 (1.47) | 19.17 (1.94) | 0.04 |
| Range | 17.10~23.10 | 15.2~24.7 | |
| Smoking | 0.35 | ||
| Yes | 2 | 12 | |
| No | 37 | 93 | |
| Previous pregnancy | 0.00 | ||
| Yes | 36 | 66 | |
| No | 3 | 39 | |
| Mammary tissue thickness, mm | |||
| Mean (SD) | 9.39 (4.56) | 7.87 (2.39) | 0.03 |
| Follow-up, months | 0.77 | ||
| Mean (SD) | 32.50 (13.80) | 31.66 (14.20) | |
| Range | 8~51 | 3~59 | |
| Implant volume, cc | |||
| Mean (SD) | 201.92 (17.15) | 199.62 (20.97) | 0.13 |
| Range | 175~225 | 175~335 |
Surgery-related indicators and recovery
Depending on the patient’s situations, we figured out some surgery-related indicators (Table 2). First of all, the mean operative time for group A and group B was 81.49 min and 78.38 min, respectively. Although no significant difference was found in operative time, there existed statistically significant difference in surgical blood loss, duration of pain and duration of indwelling drainage tube. Group A was better than group B in the three aspects. The average surgical blood loss in group A (35 ml) was less than that in group B (45.60 ml) (P < 0.05). As for the duration of pain, the mean time was 47.54 h in group A, superior to 66.92 h in group B (P < 0.05). Additionally, the mean time of indwelling drainage tube was 1.46 days in group A, and 2.98 days in group B (P < 0.05). At last, there was no statistically significant difference in the duration of postoperative hospital stay between the two groups, with a mean of 5.23 days and 6.05 days in group A and group B, respectively.
Table 2.
Surgery-related indicators and post-operation recovery
| Characteristics | Subglandular | Subpectoral | P Value |
|---|---|---|---|
| Operative time, min | |||
| Mean (SD) | 81.49 (18.42) | 78.38 (24.11) | 0.49 |
| Range | 40~114 | 35~150 | |
| Surgical blood loss, ml | |||
| Mean (SD) | 35.00 (28.87) | 45.60 (27.73) | 0.02 |
| Range | 5~130 | 10~100 | |
| Duration of pain, hours | |||
| Mean (SD) | 47.54 (17.95) | 66.92 (19.97) | 0.00 |
| Range | 18~77 | 22~123.5 | |
| Duration of indwelling drainage | |||
| Tube, days, mean (SD) | 1.46 (1.39) | 2.98 (1.21) | 0.00 |
| Range | 0~5 | 1~9 | |
| Duration of postoperative | |||
| Hospital stay, days, mean (SD) | 5.23 (3.00) | 6.05 (2.13) | 0.13 |
| Range | 2~12 | 2~12 |
Complications
The follow-up survey was conducted among 124 patients (response rate, 86.1%). Complications such as capsular contracture (CC, Baker grade III/IV), infection, asymmetry/displacement and nipple-areola numbness were summarized on implant levels. The reoperation rate was still calculated on patient level. Three augmentations developed a CC in group A, and 4 augmentations in group B. One augmentation from group B had an infection 10 months after surgery, and was treated by removing the prosthesis. There was no case of hematoma formation. No asymmetry/displacement was found in group A, but 10 were found in group B. In contrast, no nipple-areola numbness was observed in group B, but 3 were found in group A. One patient from group A underwent reoperation because she felt uncomfortable with breast implant after operation. One patient from group B experienced reoperation because of infection. Significant difference existed in nipple-areola numbness (P < 0.05), but not in the other complications (P > 0.05) (Table 3).
Table 3.
Post-operative complications in the two groups
| Characteristics | Subglandular | Subpectoral | P Value |
|---|---|---|---|
| No. of patients (Response Rate) | 35 (89.7%) | 89 (84.8%) | |
| Capsular contracture (III/IV) | 3 (4.3%) | 5 (2.8%) | 0.85 |
| Infection | 0 (0%) | 1 (0.56%) | 1.00 |
| Asymmetry/displacement | 0 (0%) | 10 (5.6%) | 0.10 |
| Nipple-areola numbness | 5 (7.14%) | 0 (0%) | 0.00 |
| Reoperation | 1 (2.86%) | 1 (1.12%) | 0.49 |
Patient satisfaction
Patients were asked to grade their overall satisfaction level (Figure 1) on a scale of 1 (poor) to 5 (perfect). 76% of patients in group A and 74% of patients in group B were satisfied with the outcome. They rated their overall satisfaction greater than 4 points. Then in group A, 24% of patients rated their satisfaction as 3 points. In group B, 20% of patients gave their overall satisfaction 3 points, indicating that they were neither satisfied nor dissatisfied with the outcome. Finally, 6% of patients in group B were dissatisfied with the result. These women rated the overall satisfaction as 1 or 2 points. The satisfaction with breast shape was similar to overall satisfaction (Figure 2). All the grades in two groups had no statistically significant difference (P > 0.05). The analysis of ordinal Logistic regression showed that patients’ satisfaction was only related to the happening of capsular contracture (OR = e2.935) and asymmetry/displacement (OR = e1.384). That meant the happening of capsular contracture and asymmetry/displacement were the risk factors to reduce the patients’ satisfaction (P < 0.05), while other factors such as the implant location and the happening of nipple-areola numbness had no obvious relationship with patients’ satisfaction (P > 0.05).
Figure 1.
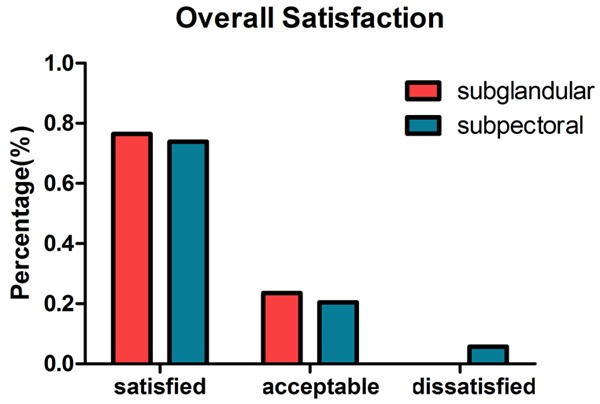
The patients’ overall satisfaction in the two groups.
Figure 2.
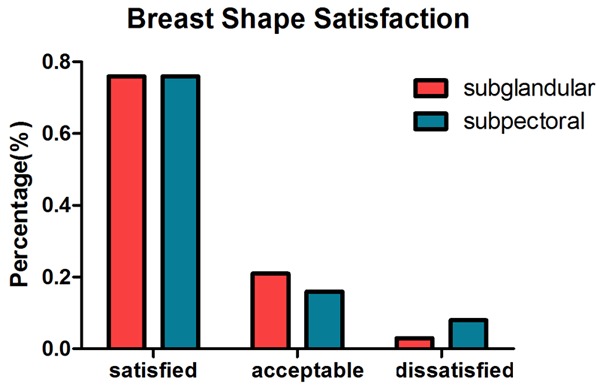
The patients’ breast shape satisfaction in the two groups.
Discussion
The number one priority in breast augmentation is to select pocket location for implant, which determines the quality and quantity of long-term soft tissue coverage of breast im-plants [2]. The four commonly selected implant pocket locations are subglandular, subpectoral, subfacial and dual-plane, each of which has specific indications as well as limitations [3,4]. Our study only focuses on subglandular and subpectoral planes. For patients with more mammary tissue and subcutaneous fat, it is more appropriate to place the implant in the subglandular plane. In contrast, for those with less mammary tissue and subcutaneous fat, the prosthesis is often implanted in the subpectoral plane [5]. As the latter patients are usually slim with a low BMI, group B had a lower BMI and thinner mammary tissue than group A.
It is well known that Asian women are usually short and slim with small breasts. Most of them wear B cup bras, and some wear A cup [6]. Subpectoral breast augmentation is appropriate for those women with small breasts. Therefore, in our study, the number of patients in group B is larger than that in group A, and the volume of the implants for Asian women is smaller than that for white women.
CC is the most common complication in primary breast augmentation. In our study, the rates of CC in the two groups were 4.3% and 2.8% respectively, similar to the incidence of 4%-5% during the first 2 years after surgery as reported previously [7,8]. Theoretically, subpectoral augmentation has a lower incidence of CC than subglandular augmentation [9,10]. As shown previously, the longer the follow-up was, the greater the risk of developing capsular contracture would be [11]. In our research, group B did have a lower rate of CC than group A, but the difference was not significant. A possible explanation for this may be inadequate sample size and short-term follow-up.
The rates of infection and reoperation in our study are lower than those in previous studies [12,13]. In group A, no cases of infection were reported, and the reoperation rate was 2.86%. One patient felt uncomfortable one year after surgery and requested to remove the implant. Actually, judging by surgeons, nothing was abnormal with her breasts, which suggests that the subjective feeling of patients is also an important factor that can affect reoperation rate. In group B, one patient experienced both infection and reoperation. The infection was caused by a boil in breast skin, which kept growing that the implant had to be removed at last. In our study, no hematoma and seroma were reported.
It has been reported that subpectoral augmentation has a high incidence of implant displacement and breast asymmetry [14], and this might be attributed to muscle contractions of the pectoralis [15-17], which is consistent with the results of our research. The rate of asymmetry/displacement was 5.6% in group B, while it was 0 in group A. However, there was no statistical significance. Increase in sample size may lead to positive results.
Nipple-areola numbness was only observed in group A. Five implanted breasts experienced persistent nipple-areola numbness after surgery, while the incidence in group B was 0. The incidence of the two groups in our study was lower than that reported by some other papers [18,19]. However, the persistent numbness incidence of group A was 7.14%, higher than that reported by Swanson E, et al. [20]. Most of their patients accepted inframammary incision and submuscular location. In our study, a majority of patients in group A were performed periareolar incision, and patients in group B mainly underwent axillary incision. Incision, implant position and size of the prosthesis are considered the three major factors that could lead to nipple-areola numbness. Mofid MM et al. has clarified that implant position is impossible to affect sensory outcome [21], and the relationship of the prosthesis size with nipple-areola numbness remains controversial [19,21,22]. Therefore, we prefer to consider that the nipple-areola numbness is an incision-related complication.
Although many studies report high rates of overall patient satisfaction with the breast augmentation [20,22-24], our results are a little disappointing in this regard. Generally speaking, complications or some side effects will affect the level of patient satisfaction. Given the low complication incidence in our study, we attribute the low rates of overall satisfaction to too high expectations and inadequate preoperative communication. In addition, very few patients will rate their overall satisfaction as 1 or 2 points. Those who gave 3 points had a vague answer. Some of them were evaluated as satisfying with both the breast softness and shape in the later interview at hospital. In the next stage of work, we will upgrade our method and be more conscientious with the investigation of patient satisfaction.
In the present study, patients in group A have a better recovery. They have significantly less surgical blood loss, and shorter duration of pain and indwelling drainage than group B. Previous studies have also reported that subpectoral augmentation caused significant postoperative breast pain [25,26], which, we think, is a meaningful outcome. Sometimes both planes are acceptable for a woman, and the planes leading to better postoperative recovery or less surgical injury should be chosen, which is validated by our research.
Our research has a number of limitations. First, it is a retrospective study conducted in only one center; thus, the number of patients is limited. Second, as it is difficult to obtain long-term follow-up, some of implant recipients are lost to follow-up. Third, this research is only performed in Chinese women.
Conclusions
In summary, each of the implant placement location has its indications and complications. When choosing a pocket plane, we must take all the factors into consideration. The two groups in our study have similar rates of satisfaction. Little difference exists in the incidence of complications, except for the rate of nipple-areola numbness. Importantly, patients in group A have a shorter recovery period after surgery than those in group B. In addition, Group A has less surgical blood loss, shorter duration of pain, and earlier pulling out of drainage tube.
Disclosure of conflict of interest
None.
References
- 1.American Society of Plastic Surgeons National Clearinghouse of Plastic Surgery Procedural Statistics. 2013 Plastic Surgery Statistics Report. American Society of Plastic Surgeons. 2014 [Google Scholar]
- 2.Tebbetts , John B. Augmentation mammaplasty: redefining the patient and surgeon experience. Elsevier Health Sciences. 2009 [Google Scholar]
- 3.Ji K, Luan J, Liu C, Mu D, Mu L, Xin M, Sun J, Yin S, Chen L. A prospective study of breast dynamic morphological changes after dual-plane augmentation mammaplasty with 3D scanning technique. PLoS One. 2014;9:e93010. doi: 10.1371/journal.pone.0093010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2006;118:81–102. doi: 10.1097/00006534-200612001-00012. [DOI] [PubMed] [Google Scholar]
- 5.Spear SL, Bulan EJ, Venturi ML. Breast augmentation. Plast Reconstr Surg. 2006;118:188–198. doi: 10.1097/01.PRS.0000135945.02642.8B. [DOI] [PubMed] [Google Scholar]
- 6.Cheng MH, Huang JJ. Augmentation mammaplasty in asian women. Semin Plast Surg. 2009;23:48–54. doi: 10.1055/s-0028-1111101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Handel N, Cordray T, Gutierrez J, Jensen JA. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. 2006;117:757–767. doi: 10.1097/01.prs.0000201457.00772.1d. [DOI] [PubMed] [Google Scholar]
- 8.Henriksen TF, Fryzek JP, Holmich LR, Mc-Laughlin JK, Kjoller K, Hoyer AP, Olsen JH, Friis S. Surgical intervention and capsular contracture after breast augmentation: a prospective study of risk factors. Ann Plas Surg. 2005;54:343–351. doi: 10.1097/01.sap.0000151459.07978.fa. [DOI] [PubMed] [Google Scholar]
- 9.Henriksen TF, Holmich LR, Fryzek JP, Friis S, McLaughlin JK, Hoyer AP, Kjoller K, Olsen JH. Incidence and severity of short-term complications after breast augmentation: results from a nationwide breast implant registry. Ann Plast Surg. 2003;51:531–539. doi: 10.1097/01.sap.0000096446.44082.60. [DOI] [PubMed] [Google Scholar]
- 10.Rohrich RJ, Kenkel JM, Adams WP. Preventing capsular contracture in breast augmentation: in search of the Holy Grail. Plast Reconstr Surg. 1999;103:1759–1760. doi: 10.1097/00006534-199905060-00033. [DOI] [PubMed] [Google Scholar]
- 11.Codner MA, Mejia JD, Locke MB, Mahoney A, Thiels C, Nahai FR, Hester TR, Nahai F. A 15-year experience with primary breast augmentation. Plast Reconstr Surg. 2011;127:1300–1310. doi: 10.1097/PRS.0b013e318205f41b. [DOI] [PubMed] [Google Scholar]
- 12.Bengtson BP, Van Natta BW, Murphy DK, Slicton A, Maxwell GP. Style 410 highly cohesive silicone breast implant core study results at 3 years. Plast Reconstr Surg. 2007;120:40–48. doi: 10.1097/01.prs.0000286666.29101.11. [DOI] [PubMed] [Google Scholar]
- 13.Cunningham B. The mentor core study on silicone memorygel breast implants. Plast Reconstr Surg. 2007;120:19–32. doi: 10.1097/01.prs.0000286574.88752.04. [DOI] [PubMed] [Google Scholar]
- 14.Strasser EJ. Results of subglandular versus subpectoral augmentation over time: one surgeon’s observations. Aesthet Surg J. 2006;26:45–50. doi: 10.1016/j.asj.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 15.Lesavoy MA, Trussler AP, Dickinson BP. Difficulties with subpectoral augmentation mammaplasty and its correction: the role of subglandular site change in revision aesthetic breast surgery. Plast Reconstr Surg. 2010;125:363–371. doi: 10.1097/PRS.0b013e3181c2a4b0. [DOI] [PubMed] [Google Scholar]
- 16.Araco A, Gravante G, Araco F, Delogu D, Cervelli V, Walgenbach K. A retrospective analysis of 3,000 primary aesthetic breast augmentations: postoperative complications and associated factors. Aesthet Plast Surg. 2007;31:532–539. doi: 10.1007/s00266-007-0162-8. [DOI] [PubMed] [Google Scholar]
- 17.Spear SL, Schwartz J, Dayan JH, Clemens MW. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthet Plast Surg. 2009;33:44–48. doi: 10.1007/s00266-008-9275-y. [DOI] [PubMed] [Google Scholar]
- 18.Okwueze MI, Spear ME, Zwyghuizen AM, Braun SA, Ajmal N, Nanney LB, Hagan KF, Wolfort SF, Shack RB. Effect of augmentation mammaplasty on breast sensation. Plast Reconstr Surg. 2006;117:73–85. doi: 10.1097/01.prs.0000191202.19657.6d. [DOI] [PubMed] [Google Scholar]
- 19.Banbury J, Yetman R, Lucas A, Papay F, Graves K, Zins JE. Prospective analysis of the outcome of subpectoral breast augmentation: sensory changes, muscle function, and body image. Plast Reconstr Surg. 2004;113:701–711. doi: 10.1097/01.PRS.0000101503.94322.C6. [DOI] [PubMed] [Google Scholar]
- 20.Swanson E. Prospective outcome study of 225 cases of breast augmentation. Plast Reconstr Surg. 2013;131:1158–1166. doi: 10.1097/PRS.0b013e318287a0e1. [DOI] [PubMed] [Google Scholar]
- 21.Mofid MM, Klatsky SA, Singh NK, Nahabedian MY. Nipple-areola complex sensitivity after primary breast augmentation: a comparison of periareolar and inframammary incision approaches. Plast Reconstr Surg. 2006;117:1694–1698. doi: 10.1097/01.prs.0000214252.50167.84. [DOI] [PubMed] [Google Scholar]
- 22.Niechajev I, Jurell G, Lohjelm L. Prospective study comparing two brands of cohesive gel breast implants with anatomic shape: 5-year follow-up evaluation. Aesthetic Plast Surg. 2007;31:697–710. doi: 10.1007/s00266-006-0057-0. [DOI] [PubMed] [Google Scholar]
- 23.Murphy DK, Beckstrand M, Sarwer DB. A prospective, multi-center study of psychosocial outcomes after augmentation with natrelle silicone-filled breast implants. Ann Plas Surg. 2009;62:118–121. doi: 10.1097/SAP.0b013e31817f01f8. [DOI] [PubMed] [Google Scholar]
- 24.Cash TF, Duel LA, Perkins LL. Women’s psychosocial outcomes of breast augmentation with silicone gel-filled implants: a 2-year prospective study. Plast Reconstr Surg. 2002;109:2112–2123. doi: 10.1097/00006534-200205000-00049. [DOI] [PubMed] [Google Scholar]
- 25.Pereira LH, Sterodimas A. Transaxillary breast augmentation: a prospective comparison of subglandular, subfascial, and submuscular implant insertion. Aesthet Plast Surg. 2009;33:752–759. doi: 10.1007/s00266-009-9389-x. [DOI] [PubMed] [Google Scholar]
- 26.Zhibo X, Miaobo Z. Effect of sustained-release lidocaine on reduction of pain after subpectoral breast augmentation. Aesthet Surg J. 2009;29:32–34. doi: 10.1016/j.asj.2008.10.008. [DOI] [PubMed] [Google Scholar]


