Abstract
Purpose: To assess clinical outcomes related to conservative management of women with cesarean scar pregnancies (CSPs), specifically through uterine artery embolization (UAE) with local and systemic methotrexate (MTX) treatment (UAE-MTX), or ultrasound-guided local and systemic MTX treatment (USG-MTX). Methods: Forty-five patients with CSP were randomly allocated to receive UAE-MTX (n = 24) or USG-MTX (n = 21). Participants’ clinical outcomes were compared, and clinical characteristics of failed cases were evaluated relative to successful cases. Results: The 2 groups were similar in clinical characteristics, success rate (83.3% cf. 80.9%), time to normalization of serum beta (β) human chorionic gonadotropin (β-hCG), and percentage of patients receiving multiple doses of systemic MTX. However, within the failed cases, the percentages of patients with gestational sac > 5 cm (87.5%), or type II CSP (75.0%) was significantly higher than in the successful cases (13.5% and 18.9%, respectively; P < 0.001, both), without regard to treatment group. According to the logistic regression model, a gestational sac diameter > 5 cm or type II CSP were independent risk factors for failed CSP management (gestational sac > 5 cm: OR 51.87, 95% CI 3.48-775.91, P < 0.01; type II CSP: OR 15.54, 95% CI 1.25-193.36, P < 0.05). Conclusion: The conservative treatments UAE-MTX and USG-MTX were similarly effective in treating CSP patients. Either treatment was likely to fail for CSP patients with gestational sac > 5 cm or type II CSP.
Keywords: Cesarean scar pregnancy, conservative management, methotrexate, uterine artery embolization, ultrasound
Introduction
Cesarean scar pregnancy (CSP) is a rare ectopic pregnancy in which the embryo implanted in a scar from previous Cesarean section. The incidence of CSP ranges from one in 1800 to one in 2216 pregnancies [1-3]. The Cesarean scar is usually located at the lower segment of the uterus, where a thin layer of myometrium is supported by a rich blood supply. If a CSP is allowed to grow without interruption, life-threatening uterine rupture and severe hemorrhage are likely [4]. The etiology of CSP is not fully known, but injuries to the uterine myometrium and endometrium have been implicated [4].
There is no consensus on the management of CSP. An invasive intervention, such as excision of the gestational sac through elective laparotomy, can reduce recurrence but the large wound will affect the patient’s fertility, with the possibility of post-operative adhesion and a long recovery [5,6]. Other invasive options, such as wedge resection and laparoscopic repair, can also lead to loss of fertility and tissue adhesion [6,7]. Traditional management with curettage and suction of a CSP is usually dangerous because blood loss is difficult to control [8,9], and if uncontrolled bleeding occurs, hysterectomy is usually required [9].
CSP can be diagnosed with ultrasound and magnetic resonance imaging before severe complications occur, allowing conservative (non-surgical) management. This is especially important for young women who want to keep their fertility. Some reports have suggested that systemic administration of methotrexate (MTX), an antifolate commonly applied in medical management of choriocarcinoma and ectopic pregnancies [10,11], can directly destroy the trophoblasts of the embryo. However, systemic MTX has a relatively high rate of associated massive bleeding and more incidence of abdominal or pelvic pain, and laparotomy is usually required in failed cases and not a favorable option for ectopic pregnancy [3,12,13]. Given the low efficacy of systemic MTX, local MTX administration may be more advantageous in CSP management. It has been reported that uterine artery embolization (UAE) and ultrasound-guided MTX injection can efficiently manage several other types of ectopic pregnancies [11].
Investigations regarding optimal treatment for CSP are limited, largely due to its rarity and small samples sizes. During 6 years of clinical practice, we recruited 45 patients with CSP for the present study. We prospectively analyzed the efficacy of UAE with local and systemic MTX treatment (UAE-MTX), and ultrasound-guided local and systemic MTX treatment (USG-MTX), for CSP patients.
Materials and methods
Recruitment of patients
The Institutional Review Board of Xijing Hospital approved this study. Between July 2008 and January 2014, 45 patients with CSP were recruited from the departments of Obstetrics and Gynecology of Xijing Hospital, Fourth Military Medical University, and General Hospital of the People’s Liberation Army, Chengdu Military Region, China.
Included in the study were patients with CSP who were hemodynamically stable and eligible for conservative treatment, not willing to have expecting surgical therapy, and available for follow-up. Acceptance into the study did not depend on patients’ initial serum β-human chorionic gonadotropin (β-hCG) levels or presence of fetal cardiac activity. Excluded were patients with acute severe blood loss (hemoglobin < 6 g/dL) or hypovolemic shock; patients with clinically established renal failure (creatinine > 150 mmol/L), active pelvic infection or clotting disorders; patients with moderate or severe abdominal pain; those who could not comply with follow-up; or patients requesting surgery.
Patients who met the criteria of inclusion were randomized into two groups according to a randomization list, generated by a random number generator with the help of a statistician. Patients of the 2 treatment groups received UAE with local and systemic MTX injection (UAE-MTX; n = 24), or ultrasound-guided local and systemic injection of MTX (USG-MTX; n = 21), respectively. Each participant provided written informed consent.
Diagnosis of CSP
All patients had a history of amenorrhoea and prior caesarean section. Transvaginal ultrasound was performed using a high-frequency transvaginal probe on a General Electric Logiq 3 ultrasound machine (GE Medical Systems, USA). Diagnosis of CSP was based on sonographic and Doppler flow findings in accordance with criteria described previously [14]: an empty uterus and cervical canal; the gestational sac located in the anterior of the uterine isthmus, with a diminished myometrial layer between the bladder and the sac; and a discontinuity in the anterior wall of the uterus, shown on a sagittal view of the uterus when the direction of the ultrasound beam runs through the amniotic sac. The concentration of β-hCG levels was not a criterion of diagnosis. Sonographic results were confirmed by two experienced gynecological sonographers. A detailed medical history of each individual patient was recorded.
Protocol of treatment
The 24 UAE surgeries procedures in the UAE-MTX group were conducted by experienced radiologists with at least 2 years clinical experience in interventional therapy, performed as similarly described in reports by Hehenkamp et al. [15]. Generally, catheters were placed at the uterine artery and 25 mg of MTX was injected bilaterally into uterine artery before the embolism procedure. The embolization was performed using gelatin sponge particles (Hangzhou Alicon Medical, Zhejiang, China).
The 21 women in the USG-MTX treatment group receive ultrasound-guided local injection with MTX (1 mL of a 25 mg/mL solution) into the gestational sac; performed by a group of gynecologists with more than 2 years training in ultrasound imaging. The ultrasound-guided puncture without analgesia or anesthesia was performed using a technique that has been described previously [11,16]. The movement of the 16-gauge ovarian cyst puncture needle (M236848, Xihuayi Beijing Science and Technology, China), guided by a transvaginal ultrasonography probe, was monitored on a screen.
The day of either UAE or ultrasound-guided local injection of MTX was considered as the first day of this regimen. In accordance with the American Congress of Obstetricians and Gynecologists (ACOG) guidelines [17] (Table 1), β-hCG levels were remeasured on days 4 and 7. If β-hCG levels decreased by 15% or more, the measurement was repeated weekly. Another dose of systemic MTX (50 mg/m2 body surface area, intramuscularly) was administrated if serum β-hCG levels failed to decrease 15% between days 4 and 7. More systemic MTX was administered during the entire follow-up period if serum β-hCG levels plateaued or increased. Hence, during follow-up, patients in both groups received systemic MTX injection(s) after day 1. Patients were followed until serum β-hCG titers declined to less than 20 mIU/mL. Failed cases were defined as after either UAE-MTX or USG-MTX and necessary systemic MTX treatment, patients showed no resolution of hCG or no disappearance of gestational sac. Patients of either group who failed the medical treatment were admitted to surgery.
Table 1.
Protocols of treatment regimens
| Evaluations | Treatment | |
|---|---|---|
| Pretreatment | Serum β-hCG, complete blood count, liver and kidney function tests, blood type | None |
| Day 1 | Serum β-hCG | MTX (1 mL, 25 mg/mL) local injection guided by ultrasound or UAE with local injection of MTX (1 mL, 25 mg/mL) |
| Day 4 | Serum β-hCG | None |
| Day 7 | Serum β-hCG, ultrasound evaluation | If β-hCG < 15% between days 4 and 7: MTX 50 mg/m2 IM |
| Day 14 | Serum β-hCG, ultrasound evaluation | If β-hCG plateaued or increased: MTX 50 mg/m2 IM |
IM, intramuscular.
Evaluation of clinical outcomes
The definition of treatment success was complete disappearance of the gestational sac with normal uterine cavity, as shown by transvaginal ultrasound, and complete normalization of serum β-hCG during follow-up.
Data analyses
All analyses were done with two-sided tests using SPSS software (version 16.0; SPSS, Chicago, IL, USA). For continuous variables, data are expressed as mean ± standard deviation if normally distributed, and Student’s t-test was performed for comparison between groups. Non-normally distributed variables are expressed as median (range) and their comparisons were made through a non-parametric test (Mann-Whitney U test). Categorical data are expressed as number (percentage) and compared by chi-squared test. The risk factors of failed management of CSP were determined by logistic regression and shown as odds ratios (OR) and 95% confidence intervals (CI). Clinical characteristics including age, gestational age, symptoms, prior caesarean deliveries, time since last caesarean delivery, β-hCG level before treatment, diameter of the gestational sac (≤ 5 or > 5 cm) and types of CSP (type I and type II), were introduced into the logistic regression model to identify risk factors associated with failed management. P < 0.05 was considered statistically significant.
Results
Clinical characteristics of the two groups
During the entire study period, 21 624 women gave birth via Cesarean section at our centers. Among them, 75 patients received diagnoses of CSP; hence, the incidence of CSP was 0.35%. Sixty-two women fulfilled the criteria for receiving conservative management, and after exclusion of those who did not satisfy the inclusion criteria of the study, 46 patients were recruited. One participant was lost to follow up. Therefore, 45 participants were enrolled, and 45 finished the follow-up (Figure 1).
Figure 1.
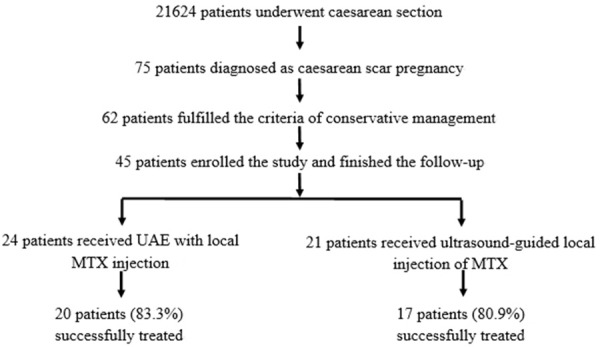
Flow chart of enrollment of participants in this study.
Among the 45 participants, 24 received UAE with local MTX injection (UAE-MTX group), and 21 patients received ultrasound-guided local injection of MTX (USG-MTX group). The median follow-up period of all participants was 3.8 weeks (range, 2 to 7 weeks). During the following up, the serum β-hCG titer, ultrasound examination, and menstrual periods were recorded.
The mean age of patients in the UAE-MTX group was 29.96 ± 4.14 years, and the mean age of patients receiving USG-MTX was 29.52 ± 4.88 years (Table 2). In the UAE-MTX and USG-MTX groups, 5 (23.8%) and 6 (25.0%) patients, respectively, had more than one cesarean section. The patients’ ages and number of prior cesarean deliveries were similar between the two groups (P > 0.05). Furthermore, the time since the last cesarean delivery, symptoms, serum β-hCG prior to treatment, diameter of the gestational sac, and types of CSP were also not significantly differ between the two groups (P > 0.05).
Table 2.
Clinical characteristics of the patients
| UAE-MTX | USG-MTX | P | ||
|---|---|---|---|---|
| Number of subjects | 24 | 21 | ||
| Age, y | 29.96 ± 4.14 | 29.52 ± 4.88 | 0.689 | |
| Prior caesarean deliveries | 1 | 18 (75%) | 16 (76.2%) | 0.926 |
| > 1 | 6 (25%) | 5 (23.8%) | ||
| Time since last caesarean delivery, mo | ≤ 2 | 0 (0%) | 1 (4.8%) | 0.385 |
| 13-120 | 21 (87.5%) | 19 (90.5%) | ||
| > 20 | 3 (12.5%) | 1 (4.8%) | ||
| Gestational age, d | 51.9 ± 2.9 | 49.3 ± 2.4 | 0.342 | |
| Symptoms | Asymptomatic | 7 (29.2%) | 5 (23.8%) | |
| Abdominal pain | 12 (50%) | 12 (57.1%) | ||
| Vaginal bleeding | 9 (37.5%) | 8 (38.1%) | ||
| β-hCG level before treatment, mIU/mL | ≤ 5000 | 0 (0%) | 0 (0%) | 0.533 |
| 5000-50000 | 23 (95.8%) | (100%) | ||
| > 50000 | 1 (4.2%) | 0 (0%) | ||
| Diameter of the gestational sac, cm | ≤ 5 | 18 (75.0%) | 15 (71.4%) | 0.787 |
| > 5 | 6 (25.0%) | 6 (28.6%) | ||
| Types of CSP | Type I | 17 (70.8%) | 15 (71.4%) | 0.965 |
| Type II | 7 (29.2%) | 6 (28.6%) | ||
| Presence of fetal cardiac activity | No | 16 (66.7%) | 16 (76.2%) | 0.528 |
| Yes | 8 (33.3%) | 5 (23.8%) |
All data are presented as mean ± standard error of the mean or number (percentage).
Clinical outcomes of the two groups
Among the 24 patients in the UAE-MTX group, the gestational sac was removed in 20 patients (83.3%), and in 17 patients (80.9%) the gestational sac was successfully removed (Table 3). The success rates of the 2 patient groups were similar (P = 0.569). The time required for patients’ serum β-hCG titer to decline to negative for patients in the UAE-MTX group (27.6 ± 7.4 d) was also comparable to that of the USG-MTX group (26.1 ± 8.4 d). The number of patients who received multiple doses of systemic MTX in the UAE-MTX group (7, 29.2%) was similar to that of the USG-MTX group (5, 23.8%). In 8 failed cases, we performed laparoscopic resection of the scar along with removal of the gestational products.
Table 3.
Clinical outcomes of patientsa
| UAE-MTXb | USG-MTXc | P | |
|---|---|---|---|
| Success rate, n (%) | 20 (83.3%) | 17 (80.9%) | 0.569 |
| Time for normalization of β-hCG level, d | 27.6 ± 7.4 | 26.1 ± 8.4 | 0.531 |
| Patients receiving multiple doses of systemic MTX | 7 (29.2%) | 5 (23.8%) | 0.746 |
All data are presented as mean ± standard deviation or number (percentage);
n = 24;
n = 21.
Clinical characteristics of the successful and failed cases
To understand which factors determine the success of conservative management of patients with CSP, the clinical characteristics between successful and failed cases were compared (Table 4). We found no significant differences in age, number of prior cesarean sections, time from last cesarean delivery, gestational age, patients’ symptoms, initial serum β-hCG titer, presence of fetal cardiac activity, or percentage of patients receiving multiple doses of systemic MTX between the successful and failed cases.
Table 4.
Clinical characteristics of successful and failed management cases
| Successful | Failed | P | ||
|---|---|---|---|---|
| Number of subjects | 37 | 8 | ||
| Age, y | 29.6 ± 4.5 | 30.4 ± 4.4 | 0.590 | |
| Prior caesarean deliveries | 1 | 29 (78.4%) | 5 (62.5%) | 0.382 |
| > 1 | 8 (21.6%) | 3 (37.5%) | ||
| Time since last caesarean delivery, mo | ≤ 12 | 1 (2.7%) | 0 (0%) | 0.544 |
| 13-120 | 32 (86.5%) | 8 (100%) | ||
| > 120 | 4 (10.8%) | 0 (0%) | ||
| Gestational age, d | 50.4 ± 3.0 | 51.9 ± 2.9 | 0.737 | |
| Symptoms | Asymptomatic | 12 (32.4%) | 0 (0%) | 0.062 |
| Abdominal pain | 16 (43.2%) | 8 (100%) | ||
| Vaginal bleeding | 14 (37.8%) | 3 (37.5%) | ||
| β-hCG level before treatment, mIU/mL | ≤ 5000 | 0 (0%) | 0 (0%) | 0.178 |
| 5000-50000 | 37 (100%) | 7 (87.5%) | ||
| > 50000 | 0 (0%) | 1 (12.5%) | ||
| Diameter of the gestational sac, cm | ≤ 5 | 32 (86.5%) | 1 (12.5%) | 0.000* |
| > 5 | 5 (13.5%) | 7 (87.5%) | ||
| Type of CSP | Type I | 3 0 (81.1%) | 2 (25.0%) | 0.000* |
| Type II | 7 (18.9%) | 6 (75.0%) | ||
| Treatment modalities | UAE with MTX | 20 (54.1%) | 4 (50%) | 0.569 |
| Ultrasound-guided MTX | 17 (45.9%) | 4 (50%) | ||
| Fetal cardiac activity | No | 28 (75.7%) | 4 (50%) | 0.202 |
| Yes | 9 (24.3%) | 4 (50%) | ||
| Received multiple doses of systemic MTX | No | 28 (75.7%) | 5 (62.5%) | 0.661 |
| Yes | 9 (24.3%) | 3 (37.5%) |
All data are presented as mean ± standard error of the mean, or number (percentage).
The treatments did not differ significantly in success rates: among 37 successful cases were 20 (54.1%) in the UAE-MTX group, and 17 (45.9%) in the USG-MTX group. For the 8 failed cases, 4 (50%) were in the UAE-MTX group, and 4 (50%) were in the USG-MTX group.
Among the failed treatment cases, 87.5% (7 patients) had gestational sacs with diameters > 5 cm, while this rate was only 13.5% (5 patients) for the successful cases (P < 0.001). In addition, 6 of the 8 failed cases had type II CSP (75.0%), while only 7 patients of the 37 successful cases had type II CSP (18.9%, P < 0.001).
Determination of risk factors for failed management
A logistic regression model was applied to determine the risk factors for failed conservative management of CSP (Table 5). A gestational sac diameter > 5 cm and type II CSP were found to be independent risk factors of failed treatment (respectively, OR 51.97, 95% CI 3.48-775.91, P = 0.004; and OR 15.54, 95% CI 1.25-193.36, P = 0.033, where OR is the odds ratio, and CI is the confidence interval).
Table 5.
Risk factors for failed management of CSP
| OR | 95% CI | P | |
|---|---|---|---|
| Diameter of gestational sac > 5 cm | 51.97 | 3.48-775.91 | 0.004 |
| Type II CSP | 15.54 | 1.25-193.36 | 0.033 |
Discussion
In this study, the efficacy of two strategies of conservative management of CSP was assessed. The clinical outcomes of these two modalities for managing CSP were similar, with success rates of 83.3% and 80.9%, respectively.We also found that patients with a relatively large gestational sac (> 5 cm in diameter) or type II CSP were much more likely to have an unsuccessful outcome.
Systemic intramuscular MTX was previously reported as a treatment option for CSP patients. Haimov-Kochman et al. [18] reported two cases of CSP who were successfully managed by intramuscular MTX, with complete disappearance of the gestational sacs. However, in that study the time to β-hCG normalization (5 and 8 weeks) was much longer than in our study (within one month). This may be due to the low concentration of MTX at lesions after systemic administration. Some researchers have further suggested that systemic MTX may be effective for CSP patients with β-hCG < 5000 mIU/mL, but less effective for those with higher serum β-hCG concentrations [3].
Selective UAE was initially developed to control massive hemorrhage in various gynecological disorders [19]. Recently, direct administration of MTX to the gestational mass after bilateral UAE has proved to be an effective conservative management strategy for patients with CSP [20]. Sugawara et al. [21] reported three cases of CSP that were successfully managed by UAE and direct injection of MTX to the gestational mass and surrounding myometrium; systemic MTX was also administrated when β-hCG normalization was not satisfied. Another case report showed that systemic MTX administration, bilateral UAE, and local injection of potassium chloride was an effective method for treating one patient with CSP [20]. Through selective UAE, MTX can work directly on the gestational sac, with high local concentration and activity. Hence, through UAE the concentration of MTX at the target tissue could increase 9- to 68-fold than that of the concentration when using systemic administration, and the potency of MTX can improve 2- to 22-fold [6]. In addition, the blood flow of the target tissue declined because of UAE, which further resulted in a delayed reduction of MTX concentration [4].
Ultrasound-guided local administration of MTX has been presented as therapy in several case reports. A 40-year-old woman was diagnosed as CSP after receiving in vitro fertilization and embryo transfer [22]. Intra-amniotic administration of MTX under USG showed excellent results, as the β-hCG declined from 23 328 mIU/L to 8 mIU/L within 2 months [22]. Another two CSP patients with viable embryos were reported as successfully managed by ultrasound-guided local administration of MTX and systemic MTX [23]. Jurkovic et al. [1] reported a 71% success rate of medical treatment for 7 CSP patients using transvaginal ultrasound-guided MTX administration.
Thus, USG-MTX injection appears to be an excellent treatment option for CSP patients. In the present study, both UAE-MTX and USG-MTX therapy showed satisfactory results. Multiple doses of systemic MTX were administrated when the reduction of β-hCG was not satisfied. By combining local and systemic MTX, we obtained high success rates (83.3% and 80.9%).
Most published case reports of CPS have concerned the successful management of patients with a gestational sac less than 3 cm. Limited information is available regarding conservative management of CSP patients with a gestational sac larger than 5 cm. Here, we report that of 8 failed cases, 7 (87.5%) were patients with a gestational sac > 5 cm, and of the 12 patients with a gestational sac this large, only 5 (41.7%) were successfully managed by conservative medical treatment. Our findings show that a gestational sac > 5 cm in CSP is an independent risk factor for the failure of conservative treatment.
Two distinguishable types of CSP have been reported by Vial et al. [6]. Type I is characterized by a gestational sac implanted on the prior scar, progressing towards the cervicoisthmic region or towards the uterine cavity. Type I can sometimes harbor a viable fetus, but there is high risk of massive bleeding. The gestational sac in type II has implanted at the post-cesarean section defect, with progression towards the bladder or abdominal cavity. A type II CSP is more dangerous than type I, because the likelihood of life threatening bleeding and rupture is greater. Because CSP is so rare, reports that compare the efficacy of conservative treatment of the two types are limited. In the present study, we found that among 8 failed cases, 6 of them (75.0%) presented as type II CSP. Among all 13 cases of type II CSP, only 7 (53.8%) were successfully managed by conservative treatment, either by UAE-MTX or USG-MTX. According to our analysis, type II CSP is an independent risk factor for failed conservative medical management of CSP.
There have been only a handful of case reports that describe the management of CSP. Here, we investigated a relatively large population of CSP cases over a 6-year study period. The majority of these patients were successful managed by conservative medical treatment. To our knowledge, this is the first report suggesting that a gestational sac > 5 cm and type II CSP are significant factors contributing to the failure of conservative treatment.
A possible limitation of this study is that disappearance of the gestational sac was not included in the follow-up. Another limitation is that no follow-up of future pregnancy status was performed. This is partly due to the one-child policy in China; most women do not plan to get pregnant. Hence, the preservation of reproductive function cannot be assessed in this study.
Conclusions
In summary, although the optimal method to manage CSP is not definitive, our results indicate that the two conservative medical treatment we used were associated with a high success rate, especially for those with a gestational sac < 5 cm and type I CSP. It is important to emphasize that conservative medical treatments are not favorable for CSP patients with gestational sac > 5 cm and type II CSP.
Disclosure of conflict of interest
None.
References
- 1.Jurkovic D, Hillaby K, Woelfer B, Lawrence A, Salim R, Elson CJ. First-trimester diagnosis and management of pregnancies implanted into the lower uterine segment Cesarean section scar. Ultrasound Obstet Gynecol. 2003;21:220–227. doi: 10.1002/uog.56. [DOI] [PubMed] [Google Scholar]
- 2.Zhuang YL, Huang LL. Uterine artery embolization compared with methotrexate for the management of pregnancy implanted within a cesarean scar. Am J Obstet Gynecol. 2009;201:152, e1–3. doi: 10.1016/j.ajog.2009.04.038. [DOI] [PubMed] [Google Scholar]
- 3.Seow KM, Huang LW, Lin YH, Lin MY, Tsai YL, Hwang JL. Cesarean scar pregnancy: Issues in management. Ultrasound Obstet Gynecol. 2004;23:247–253. doi: 10.1002/uog.974. [DOI] [PubMed] [Google Scholar]
- 4.Yin XH, Yang SZ, Wang ZQ, Jia HY, Shi M. Injection of MTX for the treatment of cesarean scar pregnancy: comparison between different methods. Int J Clin Exp Med. 2014;7:1867–1872. [PMC free article] [PubMed] [Google Scholar]
- 5.Wang CJ, Chao AS, Yuen LT, Wang CW, Soong YK, Lee CL. Endoscopic management of cesarean scar pregnancy. Fertil Steril. 2006;85:494, e1–4. doi: 10.1016/j.fertnstert.2005.07.1322. [DOI] [PubMed] [Google Scholar]
- 6.Vial Y, Petignat P, Hohlfeld P. Pregnancy in a Cesarean scar. Ultrasound Obstet Gynecol. 2000;16:592–593. doi: 10.1046/j.1469-0705.2000.00300-2.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee CL, Wang CJ, Chao A, Yen CF, Soong YK. Laparoscopic management of an ectopic pregnancy in a previous Caesarean section scar. Hum Reprod. 1999;14:1234–1236. doi: 10.1093/humrep/14.5.1234. [DOI] [PubMed] [Google Scholar]
- 8.Valley MT, Pierce JG, Daniel TB, Kaunitz AM. Cesarean scar pregnancy: Imaging and treatment with conservative surgery. Obstet Gynecol. 1998;91:838–840. doi: 10.1016/s0029-7844(97)00426-2. [DOI] [PubMed] [Google Scholar]
- 9.Chuang J, Seow KM, Cheng WC, Tsai YL, Hwang JL. Conservative treatment of ectopic pregnancy in a caesarean section scar. BJOG. 2003;110:869–870. [PubMed] [Google Scholar]
- 10.Pascual MA, Hereter L, Graupera B, Tresserra F, Fernandez-Cid M, Simon M. Three-dimensional power Doppler ultrasound diagnosis and conservative treatment of ectopic pregnancy in a cesarean section scar. Fertil Steril. 2007;88:706, e5–7. doi: 10.1016/j.fertnstert.2006.11.183. [DOI] [PubMed] [Google Scholar]
- 11.Wang M, Chen B, Wang J, Ma X, Wang Y. Nonsurgical management of live tubal ectopic pregnancy by ultrasound-guided local injection and systemic methotrexate. J Minim Invasive Gynecol. 2014;21:642–649. doi: 10.1016/j.jmig.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 12.LH W, YL Z, LL H. Clinical analyses of seventy pregnancies within caesarean scar. Chin J Obstet Gynecol. 2007;42:487–488. [Google Scholar]
- 13.Jimenez-Caraballo A, Rodriguez-Donoso G. A 6-year clinical trial of methotrexate therapy in the treatment of ectopic pregnancy. Eur J Obstet Gynecol Reprod Biol. 1998;79:167–171. doi: 10.1016/s0301-2115(98)00036-0. [DOI] [PubMed] [Google Scholar]
- 14.Wang YL, Su TH, Chen HS. Operative laparoscopy for unruptured ectopic pregnancy in a caesarean scar. BJOG. 2006;113:1035–1038. doi: 10.1111/j.1471-0528.2006.01031.x. [DOI] [PubMed] [Google Scholar]
- 15.Hehenkamp WJ, Volkers NA, Donderwinkel PF, de Blok S, Birnie E, Ankum WM, Reekers JA. Uterine artery embolization versus hysterectomy in the treatment of symptomatic uterine fibroids (EMMY trial): peri- and postprocedural results from a randomized controlled trial. Am J Obstet Gynecol. 2005;193:1618–1629. doi: 10.1016/j.ajog.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 16.Timor-Tritsch IE, Monteagudo A, Lerner JP. A ‘potentially safer’ route for puncture and injection of cornual ectopic pregnancies. Ultrasound Obstet Gynecol. 1996;7:353–355. doi: 10.1046/j.1469-0705.1996.07050353.x. [DOI] [PubMed] [Google Scholar]
- 17.American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 94: Medical management of ectopic pregnancy. Obstet Gynecol. 2008;111:1479–1485. doi: 10.1097/AOG.0b013e31817d201e. [DOI] [PubMed] [Google Scholar]
- 18.Haimov-Kochman R, Sciaky-Tamir Y, Yanai N, Yagel S. Conservative management of two ectopic pregnancies implanted in previous uterine scars. Ultrasound Obstet Gynecol. 2002;19:616–619. doi: 10.1046/j.1469-0705.2002.00719.x. [DOI] [PubMed] [Google Scholar]
- 19.Thompson AB, Teschler H, Rennard SI. Pathogenesis, evaluation, and therapy for massive hemoptysis. Clin Chest Med. 1992;13:69–82. [PubMed] [Google Scholar]
- 20.Ghezzi F, Lagana D, Franchi M, Fugazzola C, Bolis P. Conservative treatment by chemotherapy and uterine arteries embolization of a cesarean scar pregnancy. Eur J Obstet Gynecol Reprod Biol. 2002;103:88–91. doi: 10.1016/s0301-2115(02)00003-9. [DOI] [PubMed] [Google Scholar]
- 21.Sugawara J, Senoo M, Chisaka H, Yaegashi N, Okamura K. Successful conservative treatment of a cesarean scar pregnancy with uterine artery embolization. Tohoku J Exp Med. 2005;206:261–265. doi: 10.1620/tjem.206.261. [DOI] [PubMed] [Google Scholar]
- 22.Seow KM, Cheng WC, Chuang J, Lee C, Tsai YL, Hwang JL. Methotrexate for cesarean scar pregnancy after in vitro fertilization and embryo transfer. A case report. J Reprod Med. 2000;45:754–757. [PubMed] [Google Scholar]
- 23.McKenna DA, Poder L, Goldman M, Goldstein RB. Role of Sonography in the recognition, assessment, and treatment of cesarean scar ectopic pregnancies. J Ultrasound Med. 2008;27:779–783. doi: 10.7863/jum.2008.27.5.779. [DOI] [PubMed] [Google Scholar]


