Abstract
Purpose: Few studies have investigated the efficacy of silodosin, a recently introduced selective alpha 1-A adrenoceptor antagonist, in medical expulsive therapy (MET) for ureteral calculi. The results of these studies, which all evaluated the efficacy of 8 mg/day, indicate that silodosin is a potential treatment for ureteral calculi. This study investigated the efficacy of 4 mg/day of silodosin for MET of distal ureteral stones 4 to 10 mm in diameter. Material and Method: After 70 patients had been randomized into 2 groups of 35 patients each, both the control and experimental groups (groups 1 and 2, respectively) were advised to take 75 mg/day of diclofenacsodiumas needed for pain relief but only the experimental group to take 4 mg/day of silodosin. After 21 days, the groups were compared regarding the stone expulsion rate and duration, number of renalcolicepisodes, and analgesicdosage. Results: The median expulsion rates were 71.4% and 91.4% in groups 1 and 2, respectively, and the difference between them was significant (P=0.031). The median expulsion durations were 12.91±6.14 and 8.03±4.99 days, respectively, and the difference between them was significant (P<0.001). No significant differences were found regarding the median number of renal colic episodes or median analgesic dosage. While no patients in group 1 experienced side effects, 5 patients (14%) in group 2 experienced retrograde ejaculation. Conclusion: These results indicate that 4 mg/day of silodos in facilitates the expulsion of distal ureteral stones 4 to 10 mm in diameter but does not significantly reduce the number of renal colic episodes or analgesic dosage.
Keywords: Medical expulsive therapy, renal colic, silodosin, ureteral calculi, ureteral stone, alpha blocker
Introduction
Ureteral stones constitute 20% of all urinary tract stones and 70% of all ureteral stones are located in the distal ureter [1]. Although ureteral stones less than 10 mm in diameter spontaneously expulse in a significant percentage of patients without any intervention [2,18], they can lead to serious problems without appropriate medical attention.
Deficiency of and complications with treatment options such as extracorporeal shock wave lithotripsy (ESWL), ureteroscopy (URS), and open/laparoscopic ureterolithotomy have become concerns with the treatment of ureteral stones. These concerns in addition to the high rate of spontaneous expulsion of ureteral stones have led the use of drug therapies that could facilitate stone clearance to become a primary consideration. Of the many drugs that have been tested for medical expulsive therapy (MET) in the treatment of ureteral stones, alpha blockers and calcium channel blockers (CCBs), specifically the CCBnifedipin, are the only treatment modalities for which sufficient data have been collected [19]. Of these modalities, alpha blockers have been found superior to CCBs in terms of the stone expulsion rate and side effect profile [6,8,12,15]. Alpha blockers are thus recommended by the American Urological Association (AUA) and the European Association of Urology (EAU) for MET of distal ureteral stones less than 10 mm in diameter [17,18].
Alpha 1-A receptors are the most important adrenoreceptors for ureteral contraction [21]. Silodosin, which has greater specificity to alpha 1-A than other alpha blockers [19,20] is the latest alpha blocker approved for use. Thus, our knowledge regarding silodosin in MET is less than that regarding other alpha blockers. According to a MEDLINE search, no trial has evaluated the efficacy of administration of low-dose (4 mg/day) silodosin for MET. To fill this research gap we investigated the effect of administration of 4 mg/day ofsilodosin on ureteral stone expulsion rate and duration, number of renal colic episodes, and need for analgesics in patients with distal ureteral stones.
Materials and methods
One hundred thirteen patients who visited our outpatient clinic with distal ureteral stones 4 to 10 mm in diameter between March 2013 and May 2014 were considered for inclusion in this study. To determine whether the patients were eligible for inclusion (i.e., met all of the inclusion criteria and none of the exclusion criteria), complete urine study; urine culture; blood chemistry testing; urinary system X-ray; urinary system ultrasonography; and, if necessary, low-dose abdominal tomography without contrast were performed. The stone size was determined by calculating the widest diameter of the stone via review of abdominal X-ray or tomography images. The inclusion criteria were detection of a distal ureteral stone 4 to 10 mm in diameter. The exclusion criteria were age under 18 or over 65 years; presence of multiple stones; Grade 3 or 4 hydronephrosis; solitary or transplanted kidney; urinary tract infection; recurrent and persistent renal colic in reaction to analgesic administration; renal failure; allergic reaction to NSAID or alpha blocker treatment; hypotension; and/or current intake of alpha blockers, CCBs, or steroids. After the 43 patients who met one or more the exclusion criteria were excluded, the remaining 70 patients completed an informed consent form granting their permission to be included in the study for 21 days. The study was approved by the local ethical committee. Patients were then randomized into two groups (groups 1 and 2) of 35 patients each (Figure 1). No patients withdrew during the course of the study.
Figure 1.
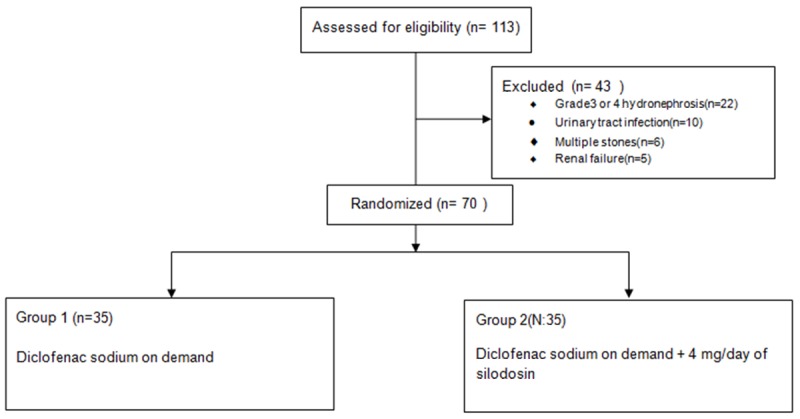
Flowchart of sample selection and categorization process.
To determine the efficacy of silodosin administration in MET via comparison of the groups, group 1 served as a control while group 2 was administered 4 mg/day of oral silodosinfor 21 days. The patients in both groups were advised to take 75 mg/day of diclofenac sodium as an analgesicas necessary. Both groups were also advised to remain active, drink at least 2 L of water daily, and pass their urine through filtersto catch any passing stones.
Patients were invited to the clinic for weekly control visits to be questioned regarding any adverse effects related to medical therapy, stone expulsion, need for analgesics (i.e., dosage of diclofenac sodium being taken), and the number of renal colic episodes experienced. All the collected data were recorded. At these weekly visits the results of urinary system ultrasonography, complete urinary study, and blood chemistry regarding renal function were reviewed. Patients who experienced stone passage were also invited for weekly control visits to record the passage duration and confirm passage of radiopaque stones by X-ray or radiolucent stones by low-dose unenhanced abdominal tomography.
Using the collected data, the groups were compared regarding stone expulsion rate, stone passage duration, number of renal colic episodes, need for analgesics. The association between sex, age, and stone size and stone expulsion rate and the associations among stone expulsion rate, stone expulsion duration, number of renal colic episodes, analgesic dosage, and stone size were analyzed. After 21 days those patients who had experienced no stone passage underwent URS or ESWL.
Statistical analysis
Descriptive statistics were reported in terms of the number (n), percentage (%), median, and range (minimum-maximum) of values. Fisher’s exact test and Pearson’s chi-squared test were performed for analysis of categorical data. Assumption of normality is controlled with the Shapiro-Wilk test. The Mann-Whitney U test was performed to compare the differences between the two groups. The Spearman correlation test was performed to determine the quantitative variants. All analyses were performed using SPSS version 18.0 (Chicago, IL, USA). P values less than 0.05 were considered statistically significant.
Results
Review of the demographics of the two groups revealed that group 1 was 57.1% male and 42.9% female and of median age of 35.23±11.20 years and group 2 was 54.3% male and 45.7% female and of a median age of 35.31±11.55 years. No statistically significant differences were found between the two groups regarding sex or age (P>0.05; Table 1).
Table 1.
Patient characteristics
| Group 1 | Group 2 | P | |
|---|---|---|---|
| Sex# n (%) Male | 20 (57.1%) | 19 (54.3%) | 0.810 |
| Female | 15 (42.9%) | 16 (45.7%) | |
| Age҂ (years) | 35.23±11.20 | 35.31±11.55 | 0.953 |
| Stone size҂ (mm) | 6.34±1.57 | 6.40±1.61 | 0.848 |
Data analyzed with the Pearson chi-squared test.
Data analyzed with the Mann-Whitney U test.
The stone size of the two groups ranged from 4 mm to 10 mm. The median stone size was 6.40±1.61 mm in group 1 and 6.34±1.57 mm in group 2. No significant difference was found regarding the stone size between two groups (P>0.05; Table 1). The stone expulsion rate at the end of day 21 was 71.4% in group 1 and 91.4% in group 2. The difference between these rates was found to be statistically significant (P=0.031). The median duration until stone expulsion was 12.91±6.14 days in group 1 and 8.03±4.99 days in group 2. The difference between these durations was found to be statistically significant (P<0.001). The number of renal colic episodes was 1.49±1.48 in group 1 and 1.17±1.44 in group 2. The difference between these numbers was not found to be significant (P=0.266). The median dosage of diclofenac sodium usage was 156.43±140.16 mg in group 1 and 113.57±130.38 mg in group 2. The difference between these dosages was not found to be statistically significant (Table 2).
Table 2.
Stone expulsion rate and duration, number of renal colic episodes, and analgesic dosage
| GROUP 1 | GROUP 2 | P | |
|---|---|---|---|
| Stone expulsion (+)# n (%) | 10 (28.6) | 3 (8.6) | 0.031* |
| Stone expulsion (-) | 25 (71.4) | 32 (91.4) | |
| Stone expulsion duration (days) | 12.91±6.14 | 8.03±4.99 | <0.001* |
| Renal colic episodes҂ (number) | 1.49±1.48 | 1.17±1.44 | 0.266 |
| Analgesic dosage҂ (mg) | 156.43±140.16 | 113.57±130.38 | 0.159 |
Data analyzed with the Pearson chi-squared test.
Data analyzed with the Mann-Whitney U test.
Significant difference.
Comparison of the patients who experienced stone expulsion with those who did not during the 21-day follow-up revealed no significant differences between them regarding sex, age, orstone size (P>0.059; Table 3).
Table 3.
Association between sex, age, and stone size andstoneexpulsion rate
| Expulsion+ | Expulsion- | P | |
|---|---|---|---|
| Sex# n (%) Male | 32 (56.1) | 7 (53.8) | 0.881 |
| Female | 25 (43.9) | 6 (46.2) | |
| Age҂ (years) | 35.33±11.44 | 35±11.05 | 0.964 |
| Stone size҂ (mm) | 6.19±1.41 | 7.15±2.08 | 0.092 |
Data analyzed with the Pearson chi-squared test.
Data analyzed with the Mann-Whitney U test.
Analysis of the association between the duration of stone expulsion with the number of renal colic episodes, analgesic dosage, and stone size revealed a positive but weak correlation (Table 4; P<0.001). A positive and strong correlation was found between the number of renal colic episodes and analgesic dosage (P<0.001), a positive but weak correlation between number of renal colic episodes and stone size (P=0.015) and a positive but weak correlation between analgesic dosage and stone size (P<0.05).
Table 4.
Associations among stone expulsion duration, number of renal colic episodes, analgesic dosage, and stone size
| Stone expulsion duration | Number of renal colic episodes | Analgesic dosage | Stone size | ||
|---|---|---|---|---|---|
| Stone expulsion duration | P | <0.001* | <0.001** | 0.001** | |
| r | 0.476 | 0.439 | 0.389 | ||
| Number of renal colic episodes | P | <0.001** | 0.015* | ||
| r | 0.967 | 0.290 | |||
| Analgesic dosage | P | 0.032* | |||
| r | 0.257 |
P<0.05;
P<0.01.
Data analyzed with the Spearman correlation test. r values show the correlation coefficient.
Discussion
While a large proportion of ureteral stones spontaneously expulse, the passage of some cause complications, such as hydronephrosis, complex urinary tract infections, and renal dysfunction [9], indicating the necessity of individualized treatment. According to EAU urolithiasis guidelines, URS is the first treatment option for distal ureteral stones greater than 1 cm in length, whereas both URS and ESWL are the preferred treatment options for stones less than 1 cm [17]. The choice of optimal treatment may depend on the physician’s experience and/or the instruments and equipment available. Although URS is a successful treatment method, it has several disadvantages, including the need for general anesthesia and hospitalization; high cost [25]; and the possibility of complications, such as strictures and, rarely, avulsion. In recent years the possibility of use of holmium laser with flexible ureterorenoscopy, as well a decrease in instrument calibration, has led to a reduction in complication rates [24].
ESWL is a safe method for treatment of ureteral stones that has been used since the early 1980s. Its main advantages over URS are that it does not require general anesthesia or hospitalization and allows patients to return to work shortly after undergoing the procedure. However, it has the disadvantages of being less effective for the treatment of stones of intense composition, [3] being contraindicated for some conditions [17], and having a high cost [25]. Because of the disadvantages of the available treatment modalities and the high expulsion rates associated with MET, urologists provide MET more than they have in the past. MET is indicated if there is no benefit for active removal of a stone less than 1 cm in length and when the patient’s comfort will not be affected using this approach [17].
To date, alpha blockers, anticholinergics, trigliserilnitrat, steroids, alpha-1 receptor antagonists, and CCBs have been tested for MET. Of these, alpha blockers and CCBs have proven effective in MET and are widely used in daily practice. Sufficient evidence has been collected that alpha 1 receptor blockers, including tamsulosin, silodosin, doxazosin, terazosin, alfuzosin, and naftopidil, as well as the CCB nifedipine, are efficacious for MET. These agents decrease the need for analgesic administration and the number of renal colic episodes as well as facilitate stone expulsion [17].
Most studies of administration of alpha blockers for MET have focused on treatment of stones in the distal ureter [3]. All data collected to date indicate that irreversible renal damage does not tend to occur with an incomplete obstruction for the first 4 weeks in the absence of an aggravating factor, such as urinary tract infection. Therefore, a logical approach in the absence of aggravating factors appears provision of MET only after the passage of 4 weeks [9,17]. To narrow the safety margin in our study, we provided MET after the passage of 3 weeks.
A meta-analysis of 328 patients revealed that 47% of ureteral stones 5 to 10 mm in diameter spontaneously expulse [18]. Another study found that 95% of ureteral stones 4 mm and below in diameter spontaneously expulse within 40 days [2]. To further examine these findings, we investigated MET for ureteral stones 4 to 10 mm in diameter, as have many other studies of MET. Our investigation of 70 patients with distal ureteral stones 4 to 10 mm in diameter over one year revealed that silodosin administration facilitated stone expulsion rates without serious side effects but did not decrease the number of renal colic episodes or the need for analgesics.
In a meta-analysis of 16 studies of alpha blockers and 9 studies of CCBs, Singh et al. found that while both agents increased stone expulsion rates, 4% of patients administered alpha blockers experienced side effects while 15.2% of patients taking CCBs did so [15]. This finding indicates that administration of alpha blockers can be more advantageous than administration of CCBs for MET. In our study 5 (14%) patients experienced retrograde ejaculation and one patient (3%) experienced nasal congestion.
Except for those that examined silodosin, studies comparing alpha blockers for MET found their efficacy to be mostly equivalent [7,10,11]. Trials that compared tamsulosin with nifedipine, the most commonly used CCB for medical for MET, found that tamsulosin is superior to nifedipine in stone expulsion [17]. In a study of 187 patients with proximal, mid, or distal ureteral stones, Itoh et al. compared a group administered 8 mg/day of silodosin with a control group [5]. The researchers found that silodosin did not affect stone expulsion rates, expulsion duration, or analgesic need in patients with proximal and mid ureteral stones. In contrast, they found that silodosin decreased stone expulsion duration but did not affect stone expulsion rate or analgesic need in patients with distal ureteral stones. In the same study, subgroup analysis of distal ureteral stones 6 to 9 mm in diameter revealed that silodosin increased stone expulsion rates and decreased stone expulsion duration but did not affect analgesic need. However, the findings should be viewed with caution because the study included only men.
Amulti-institutional, randomized, placebo-controlled, prospective trial of 232 patients found that administration of 8 mg/day of silodosin increased stone passage rates compared to a placebo in patients with distal ureteral stones but not in patients with proximal and mid stones [22].
While the alpha-1A blockade of silodosin is 56 times higher than its alpha 1-D blockade, the alpha 1-D blockade of naftopidilis 3 times higher than its alpha-1A blockade [13]. In a comparison of administration of 8 mg/day of silodosin and 50 mg/day of naftopidil 50 mg in 74 patients with ureteral stones, Tsuzaka et al. found that silodosin achieved an 84% expulsion rate and naftopidila 61% rate (P=0.039) [4]. In all segments of the ureter, a greater number of alpha 1-D receptors are present than alpha 1-A receptors [26]. While these findings suggest that alpha-1A receptor is more important than alpha 1-D receptor in ureteral contraction, they should be viewed with caution, as the study did not conduct subgroup analysis of proximal, mid, and distal ureteral stones.
In a comparison of administration of 0.4 mg/day of tamsulosin and 8 mg/day of silodosinin patients with mid and distal ureteral stones less than 10 mm in diameter, Gupta et al. found a stone expulsion rate of 58% for tamsulosin and 82% for silodosin (P=0.008). They also found that not only is the expulsion rate significantly greater with silodosin (P=0.008) but also that the stone expulsion duration was significantly shorter with silodosin (P=0.001) [14]. These findings may be the result of silodosin’s greater selectivity for the alpha 1-A receptor compared to tamsulosin.
One disadvantage of administration of 8 mg/day of silodosin for MET may be its greater side effect profile compared to a lower dose of the agent. In one trial, 8 mg/day of silodosin was found to result in greater dizziness, nasal congestion, and other side effects compared to 4 mg/day of silodosin 4 [16]. We therefore recommend that the advantages of 4 mg/day of silodosin compared to 8 mg/day of silodosin be considered when planning MET.
Conclusion
In the light of foregoing silodosin 4 mg is considered to be a safe and effective agent in noncomplicated distalureteral stones below 10 mm size. Further studies comparing head to head silodosin 4 mg and 8 mg with other alpha blockers will show more conclusive data in efficacy and side effects.
Disclosure of conflict of interest
None.
References
- 1.Pak CY. Kidney stones. Lancet. 1998;351:1797–801. doi: 10.1016/S0140-6736(98)01295-1. [DOI] [PubMed] [Google Scholar]
- 2.Miller OF, Kane CJ. Time to stone passage for observed ureteral calculi: a guide for patient education. J Urol. 1999;162:688–90. doi: 10.1097/00005392-199909010-00014. discussion 690-1. [DOI] [PubMed] [Google Scholar]
- 3.Seitz C, Liatsikos E, Porpiglia F, Tiselius HG, Zwergel U. Medical therapy to facilitate the passage of stones: what ıs the evidence? Eur Urol. 2009;56:455–71. doi: 10.1016/j.eururo.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 4.Tsuzaka Y, Matsushima H, Kaneko T, Yamaguchi T, Homma Y. Naftopidil vs silodosin in medical expulsive therapy for ureteral stones: a randomized controlled study in Japanese male patients. Int J Urol. 2011;18:792–5. doi: 10.1111/j.1442-2042.2011.02850.x. [DOI] [PubMed] [Google Scholar]
- 5.Itoh Y, Okada A, Yasui T, Hamamoto S, Hirose M, Kojima Y, Tozawa K, Sasaki S, Kohri K. Efficacy of selective α1A adrenoceptor antagonist silodosin in the medical expulsive therapy for ureteral stones. Int J Urol. 2011;18:672–4. doi: 10.1111/j.1442-2042.2011.02810.x. [DOI] [PubMed] [Google Scholar]
- 6.Dellabella M, Milanese G, Muzzonigro G. Efficiency of tamsulosin in the medical management of juxtavesical ureteral stones. J Urol. 2003;170:2202–5. doi: 10.1097/01.ju.0000096050.22281.a7. [DOI] [PubMed] [Google Scholar]
- 7.Yılmaz E, Batislam E, Basar MM, Tuglu D, Ferhat M, Basar H. The comparison and efficacy of 3 different alpha1-adrenergic blockers for distal ureteral stones. J Urol. 2005;173:2010–2. doi: 10.1097/01.ju.0000158453.60029.0a. [DOI] [PubMed] [Google Scholar]
- 8.Porpiglia F, Ghignone G, Fiori C, Fontana D, Scarpa RM. Nifedipine versus tamsulosin for the management of lower ureteral stones. J Urol. 2004;172:568–71. doi: 10.1097/01.ju.0000132390.61756.ff. [DOI] [PubMed] [Google Scholar]
- 9.Hübner WA, Irby P, Stoller ML. Natural history and current concepts for the treatment of small ureteral calculi. Eur Urol. 1993;24:172–6. doi: 10.1159/000474289. [DOI] [PubMed] [Google Scholar]
- 10.Agrawal M, Gupta M, Gupta A, Agrawal A, Sarkari A, Lavania P. Prospective randomized trial comparing efficacy of alfuzosin and tamsulosin in management of lower ureteral stones. Urology. 2009;73:706–9. doi: 10.1016/j.urology.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Ahmed AF, Al-Sayed AY. Tamsulosin versus alfuzosin in the treatment of patients with distal ureteral stones: prospective, randomized, comparative study. Korean J Urol. 2010;51:193–7. doi: 10.4111/kju.2010.51.3.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ye Z, Yang H, Li H, Zhang X, Deng Y, Zeng G, Chen L, Cheng Y, Yang J, Mi Q, Zhang Y, Chen Z, Guo H, He W, Chen Z. A multicentre, prospective, randomized trial: comparative efficacy of tamsulosin and nifedipine in medical expulsive therapy for distal ureteric stones with renal colic. BJU Int. 2011;108:276–9. doi: 10.1111/j.1464-410X.2010.09801.x. [DOI] [PubMed] [Google Scholar]
- 13.Takei R, Ikegaki I, Shibata K, Tsujimoto G, Asano T. Naftopidil, a novel alpha 1 adrenoceptor antagonist, displays selective inhibition of canine prostatic pressure and high affinity binding to cloned human alpha 1 adrenoceptors. Jpn J Pharmacol. 1999;79:447–54. doi: 10.1254/jjp.79.447. [DOI] [PubMed] [Google Scholar]
- 14.Gupta S, Lodh B, Singh AK, Somarendra K, Meitei KS, Singh SR. Comparing the efficacy of tamsulosin and silodosin in the medical expulsion therapy for ureteral calculi. J Clin Diagn Res. 2013;7:1672–4. doi: 10.7860/JCDR/2013/6141.3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007;50:552–63. doi: 10.1016/j.annemergmed.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 16.Nickel JC, O’Leary MP, Lepor H, Caramelli KE, Thomas H, Hill LA, Hoel GE. Silodosin for men with chronic prostatitis/chronic pelvic pain syndrome: results of a phase II multicenter, double-blind, placebo controlled study. J Urol. 2011;186:125–31. doi: 10.1016/j.juro.2011.03.028. [DOI] [PubMed] [Google Scholar]
- 17.Tiselius HG, Ackermann D, Alken P, et al., editors. Guidelines on urolithiasis. European Association of Urology [website] 2008 Mar. http://www.uroweb.org/fileadmin/user_upload/Guidelines/Urolithiasis.pdf. Accessed January 28, 2014. [DOI] [PubMed]
- 18.Management of ureteral calculi: EAU/AUA nephrolithiasis panel. American Urological Association [website] 2007. http://www. auanet.org/education/guidelines/ureteral-calculi.cfm. Accessed January 29, 2014.
- 19.Martin DJ, Lluel P, Guillot E, Coste A, Jammes D, Angel I. Comparative alpha-1 adrenoceptor subtype selectivity and functional uroselectivity of alpha-1 adrenoceptor antagonists. J Pharmacol Exp Ther. 1997;282:228–35. [PubMed] [Google Scholar]
- 20.Tatemichi S, Kobayashi K, Maezawa A, Kobayashi M, Yamazaki Y, Shibata N. Alpha1-adrenoceptor subtype selectivity and organ specificity of silodosin (KMD-3213) Yakugaku Zasshi. 2006;126:209–16. doi: 10.1248/yakushi.126.209. [DOI] [PubMed] [Google Scholar]
- 21.Sasaki S, Tomiyama Y, Kobayashi S, Kojima Y, Kubota Y, Kohri K. Characterization of α1-adrenoceptor subtypes mediating contraction in human isolated ureters. Urology. 2011;77:762, e13. doi: 10.1016/j.urology.2010.09.034. [DOI] [PubMed] [Google Scholar]
- 22.Sur RL, Shore N, L’Esperance J, Knudsen B, Gupta M, Olsen S, Shah O. Silodosin to facilitate passage of ureteral stones: a multi-institutional, randomized, double-blinded, placebo-controlled trial. Eur Urol. 2015;67:959–64. doi: 10.1016/j.eururo.2014.10.049. [DOI] [PubMed] [Google Scholar]
- 23.Moursy E, Gamal WM, Abuzeid A. Tamsulosin as an expulsive therapy for steinstrasse after extracorporeal shock wave lithotripsy: a randomized controlled study. Scand J Urol Nephrol. 2010;44:315–9. doi: 10.3109/00365599.2010.494616. [DOI] [PubMed] [Google Scholar]
- 24.Hong YK, Park DS. Ureteroscopic lithotripsy using Swiss Lithoclast for treatment of ureteral calculi: 12-years experience. J Korean Med Sci. 2009;24:690–4. doi: 10.3346/jkms.2009.24.4.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parker BD, Frederick RW, Reilly TP, Lowry PS, Bird ET. Efficiency and cost of treating proximal ureteral stones: shock wave lithotripsy versus ureteroscopy plus holmium: yttrium-aluminum-garnet laser. Urology. 2004;64:1102–6. doi: 10.1016/j.urology.2004.07.040. [DOI] [PubMed] [Google Scholar]
- 26.Itoh Y, Kojima Y, Yasui T, Tozawa K, Sasaki S, Kohri K. Examination of alpha 1 adrenoceptor subtypes in the human ureter. Int J Urol. 2007;14:749–53. doi: 10.1111/j.1442-2042.2007.01812.x. [DOI] [PubMed] [Google Scholar]


