Abstract
The aim of this study was to explore the influence of combination therapy in different administration time on antihypertensive efficacy and blood pressure variability in patients with essential hypertension. A total of 86 patients with stage II to III essential hypertension were randomly divided into 4 groups: taking indapamide and losartan potassium together in the morning or in the evening 2 to 4 hours before sleep, indapamide in the morning and losartan potassium in the evening, losartan potassium in the morning and indapamide in the evening. Ambulatory blood pressure monitoring was performed before and 12 weeks after the medication. The result showed that statistically significant reductions from baseline of systolic blood pressure/diastolic blood pressure occurred in all treatment groups. There was no significant difference of the reductions or SI among the four groups, neither the rate of decline of BP in the night or the circadian rhythm. In group B, the numbers of rapid rise in BP in the morning hours were significantly less after the medication, while not in the other groups. It is concluded that independent of the administration time, both once-daily treatment and component-based dual therapy had significant antihypertensive effect, but the night taken-together combination resulted in reductions of BP, SI and morning blood pressure peak that may have advantages over the other combinations, without the increased incidence of hypotension at night. Medicines should be taken 2 to 4 hours before sleep.
Keywords: Hypertension, chronotherapy, indapamide, losartan potassium, therapeutic efficacy
Introduction
Hypertension is considered to be a major risk factor for cardiovascular and cerebrovascular morbidity and mortality [1-3]. The diagnosis of hypertension is based on the traditional method of taking auscultatory measurements (office blood pressure, OBP) in a clinical setting [4,5]. However, because of the white-coat and the masked hypertensive phenomena, OBP may be unrepresentative of the true blood pressure in about 30% of the patients who visit hypertension clinics [6]. Previous studies showed that ambulatory blood pressure (ABP) and home blood pressure (HBP) measurements are more reproducible than OBP measurements [7-10]. An important aspect of the information provided by ABP measurement (ABPM) is the ability to quantify the degree of BP variability over 24 h [11-13], which has been shown to be a significant and independent risk factor for cardiovascular morbidity and mortality [14-16]. Antihypertensive treatment has differential effects on OBP measurements and 24 h ABPM [17]. Typically, the effect of antihypertensive treatment is greater on OBP measurements than on 24 h average ABP values, and is unevenly distributed between day and night [18]. This suggests that a more systematic adoption of ABPM in clinical trials should be implemented, as ABPM adds valuable information to OBP readings, in particular when assessing the homogeneity of BP reduction in daily life induced by antihypertensive treatment. Several clinical trials have shown that different combinations of drugs at different times in the day may have exerted to different effects. This is the first investigation designed to explore the effects of single night dosing combination therapy on BP and BPV in patients with grade 2 and above essential hypertension.
Methods
Subjects’ information
Between May 2012 and April 2013, 156 patients with essential hypertension grade 2 and above were enrolled from clinic hypertension screening. As 2 cases of monotherapy for low BP, 4 shift-workers, and 67 cases loss to follow-up were removed, a total of 83 cases aged 35-77 years participated in the study finally.
Inclusion and exclusion criteria
A diagnosis of grade 2 and above essential hypertension was made using the criteria of the “Chinese Guidelines for Prevention Treatment of Hypertension (Revised Edition 2005)”, based on repeated conventional BP measurements and corroboration by ABPM at the time of recruitment. A positive diagnosis of hypertension based on ABPM required either the 24-h mean SBP/DBP was ≥130/80 mmHg (1 mmHg = 0.133 kPa), the diurnal mean value was ≥135/85 mmHg, or the nocturnal mean value was ≥120/70 mmHg. The selected subjects were either previously untreated or drugs withdrawal for two weeks or more. The study protocol was approved by the Ethics Committee of the Second Affiliated Hospital of Hebei Medical University, while written informed consents were obtained from all the patients before randomly assigned. Patients were excluded if they showed evidence of secondary hypertension, type 1 diabetes mellitus, unstable angina pectoris, life-threatening cardiac arrhythmias, severe hepatic and renal disfunction that confirmed by clinical and laboratory examination, as well as those shift-workers or known allergies or contraindications to study drugs.
Groups of trial
In accordance with the principle of randomized, single-blinded and parallel-controlled methods, the 86 cases were divided into 4 groups: group A: Patients received indapamide 2.5 mg and losartan potassium 50 mg together at 6-8 am in the morning, group B: indapamide 2.5 mg and losartan potassium 50 mg together at 19-21 pm at night (2-4 h before sleep), group C: indapamide 2.5 mg at 6-8 am and losartan potassium 50 mg at 7-9 pm separately, group D: losartan potassium 50 mg at 6-8 am and indapamide 2.5 mg at 7-9 pm separately. Per protocol, 24-h ABPM was conducted at baseline before randomization and 8 weeks after treatment. Patients were fitted on the non-dominant arm with a MGY ABPM device. They were assessed while adhering to their usual diurnal activity (6/7 to 10/11 PM for most) and nocturnal sleep routines. Participants were instructed to go about their usual activities with minimal restrictions but to follow a similar schedule during the 2 days of ABPM. The ambulatory monitoring was performed with automatic readings every 30 minutes in the daytime and every 60 minutes at night. The daytime and nighttime BPs were defined as the values in the awake period between 06:00/07:00 hours and 22:00/23:00 hours and in the sleeping period between 22:00/23:00 hours and 06:00/07:00 hours, respectively. Thus, readings with SBP >260 or <70 mmHg, DBP >150 or <40 mmHg, and pulse pressure (difference between SBP and DBP) >150 or <20 mmHg were automatically discarded, and only subjects with 80% success were included. SI, morning blood pressure surge (MBPS), decreasing ratio of BP in the nighttime conforms to the standard suggested in the Blood Pressure Measurement Guideline of China.
Statistical analysis
All statistical data were completed using epidata 3.1 double entry and validation, and analysed by SPSS 18.0. The measurement data are presented as mean ± SD. Changes from baseline were evaluated using a t-test for paired data. Between-treatment differences were analyzed using ANOVA with treatment as a factor. Categorical variables were compared using the Chi-square test. P<0.05 was considered statistically significant.
Results
Baseline characteristics are presented in Table 1. Mean age of the 86 patients was 55.8 years, and 55% of the patients were female while 45% were male. Nearly three-fourths (75%) had grade 2 (n = 60 [70%]) or grade 3 (n = 4 [5%]) hypertension. Baseline BP in the overall population was 165.8±12.6/93.5±5.6 mmHg. No patients had severe renal dysfunction. Overall, there were no significant differences in the baseline characteristics between the 4 treatment groups in sex and age distribution, BPs in the daytime, nighttime and 24 h, as well as the percentage of decline of BP during sleep. The 4 treatment time groups were comparable.
Table 1.
Baseline characteristics of hypertensive patients eligible to receive combination therapy
| N = 86 | |
|---|---|
| Demographic characteristics | |
| Age (years) | 55.8±12.5 |
| Sex (male) | 39 (45%) |
| Current smoker | 8 (9%) |
| Body mass index (kg/m2) | 25.8±5.7 |
| Cardiovascular risk | |
| Systolic blood pressure (mmHg) | 158.5±12.6 |
| Diastolic blood pressure (mmHg) | 95.5±5.6 |
| Coronary artery disease | 3 (3%) |
| TC/HDL ratio | 4.0±0.6 |
| Left ventricular hypertrophy | 3 (3%) |
| Diabetes | 13 (15%) |
| Medical history | |
| Grade 1 hypertension | 13 (15%) |
| Grade 2 hypertension | 45 (52%) |
| Grade 3 hypertension | 13 (33%) |
| Laboratory parameters | |
| Fating plasma glucose (mg/dL) | 105.6±22.6 |
| Total cholesterol (mg/dL) | 178.3±10.2 |
| LDL cholesterol (mg/dL) | 108.5±42.1 |
| HDL cholesterol (mg/dL) | 48.5±10.3 |
| Triglycerides (mg/dL) | 130.9±52.6 |
| Serum sodium (mEq/L) | 135.2±10.1 |
| Serum potassium (mEq/L) | 4.5±0.6 |
| Serum creatinine (mg/dL) | 0.8±0.3 |
BPs before and after treatment in each group: Clinic BP measurements (SBPs and DBPs at daytime, nighttime and 24 h, P<0.01), except for the percentage of decline of BP during sleep (P>0.05), were significantly different after treatment. Numbers occurred morning surge before/after treatment: group A 10/8, group B 12/5, group C 13/9, group D 11/7, only in group B resulted a statistically significant reduction of the morning BP surge from baseline. According to the types of circadian rhythm of blood pressure, before the treatment dipping, non-dipping, extreme-dipping and reverse-dipping: group A 7, 10, 2, 1 cases, group B 8, 11, 1, 1 cases, group C 9, 10, 3, 2 cases, and group D 9, 9, 2, 2 cases; After treatment: group A 6, 10, 2, 2 cases, group B 7, 9, 3, 2 cases, group C 6, 10, 3, 4 cases, and group D 7, 9, 3, 3 cases. The circadian pattern was similar before and after therapy (P>0.05).
BP reduction and SI after treatment: After 8 weeks of timed-treatment, there were no statistically significant differences among the 4 groups in the decline of diurnal, nocturnal, and 24-h mean BP, or the SI (P>0.05). After treatment, 53.8% of the subjects in group A, 53.6% in group B, 37.0% in group C and 51.9% in group D showed controlled values of ABPM (diurnal mean value was <135/85 mmHg for SBP/DBP and the nocturnal mean value was <120/70 mmHg). It revealed a lack of statistically significant differences among the treatment-time groups (P>0.05) (Table 2).
Table 2.
The comparison of step-down amplitude (mmHg) after treatment in the four groups and smoothness index (SI) (mean ± SD)
| Parameters | Group A (20 cases) | Group B (21 cases) | Group C (23 cases) | Group D (22 cases) | F | P |
|---|---|---|---|---|---|---|
| Reduction of SBP in daytime | 30.5±11.2 | 31.3±13.5 | 35.0±12.6 | 28.8±14.0 | 0.93 | 0.43 |
| Reduction of SBP in night | 24.6±12.8 | 26.5±11.8 | 22.8±14.6 | 23.7±9.7 | 0.35 | 0.79 |
| Reduction of SBP in 24 h | 28.7±11.9 | 30.5±10.5 | 28.5±15.4 | 24.9±10.6 | 0.78 | 0.51 |
| Reduction of DBP in daytime | 16.8±6.5 | 18.6±6.9 | 18.2±10.5 | 14.8±6.9 | 1.02 | 0.39 |
| Reduction of DBP in night | 14.4±8.7 | 15.4±6.9 | 15.3±9.5 | 15.0±7.5 | 0.06 | 0.98 |
| Reduction of DBP in 24 h | 15.9±6.9 | 18.0±7.9 | 16.6±9.1 | 14.6±6.3 | 0.74 | 0.53 |
| Reduction of SI of SBP in daytime | 2.1±1.6 | 2.2±1.1 | 2.3±1.2 | 1.8±0.8 | 0.72 | 0.54 |
| Reduction of SI of SBP in night | 1.6±0.9 | 2.1±1.4 | 1.4±0.9 | 1.6±0.6 | 1.97 | 0.12 |
| Reduction of SI of SBP in 24 h | 1.5±0.6 | 2.1±1.2 | 1.5±0.8 | 1.5±0.5 | 2.84 | 0.04 |
| Reduction of SI of DBP in daytime | 1.6±1.2 | 1.4±1.1 | 1.4±1.1 | 1.5±0.8 | 0.17 | 0.92 |
| Reduction of SI of DBP in night | 1.3±0.8 | 1.6±0.7 | 1.2±0.5 | 1.5±0.9 | 1.34 | 0.27 |
| Reduction of SI of DBP in 24 h | 1.4±0.7 | 1.6±0.7 | 1.3±0.6 | 1.4±0.5 | 0.87 | 0.46 |
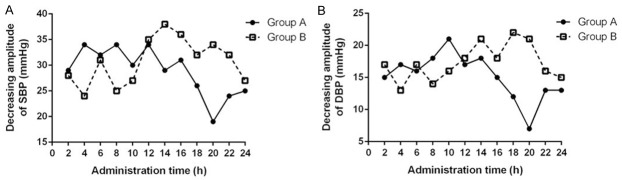
After 8 weeks treatment the circadian amplitude (extent of change in BP along the 24 h) (Figure 1): the decline of SBP in the first 12 h after ingested in group B was less than that in group A, while the DBP declines were similar. The decreasing amplitude in the first 10 h was smaller than the last 12 h of both SBP and DBP in group B.
Figure 1.
A: Decreasing amplitude of SBP during the following 24 h between group A and group B after 8 weeks treatment. B: Decreasing amplitude of DBP during the following 24 h between group A and group B after 8 weeks treatment.
Discussion
Effective BP control can significantly reduce shocks and CVD. When prescribing an antihypertensive agent, a long-acting agent is important to ensure sustained control of nighttime blood pressure and morning BP surge, as well as to prevent cardiovascular and cerebrovascular complications. Combination treatment should be considered as a first choice in patients with grade 2 and above essential hypertension to achieve an adequate BP control [19]. The CHIEF (Chinese Hypertension Intervention Efficacy Study) investigation showed that, combination therapy with a low-dose long-acting calcium channel blocker (CCB) and an angiotensin II receptor blockers (ARB) as the initial therapy can significantly improve BP control rate. ARB can reduce the common ankle edema caused by CCB. Moreover, since CCB are potent vasodilators that induce reflex activation of the sympathetic system and rapid heartbeat, the use of an ARB may buffer this excessive activation. Indapamide administered at bedtime, as opposed to morning dosing, improved the sleep time-relative blood pressure decline toward a more dipper pattern without loss in 24-h efficacy, thus highly reduced CVD risk in the morning. The efficacy of amlodipine on the 24-h mean BP was seemed to be comparable independent of the time of treatment [20,21]. From each single-agent efficacy cannot infer the effects of combination therapy on blood pressure regulation directly. This study showed, clinic BP measurements, including daytime, nighttime and 24 h mean SBP/DBP, were significantly reduced after treatment and to a comparable extent in all treatment-time groups. At the same time, the reduction of daytime, nighttime and 24 h SDP/DBP as well as the SI were similar (P>0.05) in group A (morning dosing) and group C/D (morning-evening splitting of daily doses). Previous studies have shown that SI was negatively correlated with BPV, and it could be used as predictors of long-term target organ injury. Namely the greater SI and smaller BPV is, the less injure of the target organ gains [14]. There was also a trend towards greater reduction of BP and smaller BPV with the single night dose combination therapy, although statistical significance was not reached. Thus, drugs might be expected to be cleared more slowly overnight, thus potentially prolonged their duration of action. This result was not fully agreed with Hermida et al [22]. When the drugs were administered in a single night dose, the effect on morning BP surge was obviously larger than those in other 3 groups. That maybe because that, while the first 10 h decline of SBP/DBP were significantly larger than the last 12 h and the 10th-14th h, as ingested 2-4 h before sleep, a drug peak effect on BP reduction was reached when awaked after a 7 h-sleep, which just covered the morning BP surge. In short-time BPV, the morning BP surge is closely related to the stroke risk, independent of APBM, nocturnal BP reduction and silent cerebral infarction. Hence, the reduction of morning BP surge can be used as a new therapeutic target to prevent the hypertensive target organ damage and CV events [23]. The study revealed that, as the same drugs combination therapy, the declines of SBP in the first 12 h are smaller in group B than that in group A. At the same time, the decreasing amplitude of SBP and DBP in the first 10 h in group B is smaller than the last 12 h of the dosing interval; 53.6% of the patients in group B evidenced controlled BP after treatment, which was similar to group A (53.8%); nocturnal BP decrease showed no statistically significant differences among the 4 groups. One case of ultra-dipper was added in groups A, B and D, respectively, while no change in group C after treatment. There were 2 cases in group A, 5 cases in group B, 6 cases in group C and 2 cases in group D having a DBP lower to 60 mmHg during night, of which only 1 in group D with SBP lower to 90mmHg simultaneously. Thus, a single night dose of combination therapy didn’t induct excessive BP reduction nocturnally. Our study found that, the antihypertensive effect of CCB and ARB combination was independent of the treatment time. Bedtime administration of the combination medication was found to be a safe and effective means of controlling morning BP in hypertensive patients without induction of excessive BP reduction nocturnally, and drugs should be taken 2-4 h before sleep.
In conclusion, a single night dose combination therapy can be used as one of the therapeutic regimen in patients with grade 2 and above essential hypertension, taking reduction of BPV into account, it will have better compliance and is more effective to prevent target-organ damage.
Acknowledgements
This work was supported by NHFPC Funding Project of the Nei Monggol Autonomous Region (201303056) and Science and Technology Million Project of Inner Mongolia Medical University (YKD2014KJBW006).
Disclosure of conflict of interest
None.
References
- 1.Ezzati M, Oza S, Danaei G, Murray CJ. Trends and cardiovascular mortality effects of state-level blood pressure and uncontrolled hypertension in the United States. Circulation. 2008;117:905–914. doi: 10.1161/CIRCULATIONAHA.107.732131. [DOI] [PubMed] [Google Scholar]
- 2.Miao XN, Siu KL, Cai H. Nifedipine Attenuation of Abdominal Aortic Aneurysm in Hypertensive and non-Hypertensive Mice: Mechanisms and Implications. J Mol Cell Cardiol. 2015;87:152–9. doi: 10.1016/j.yjmcc.2015.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hostalek U, Czarnecka D, Koch EM. Treatment of Hypertensive Patients with a Fixed-Dose Combination of Bisoprolol and Amlodipine: Results of a Cohort study with More Than 10,000 Patients. Cardiol Ther. 2015;4:179–190. doi: 10.1007/s40119-015-0045-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cloutier L, Daskalopoulou SS, Padwal RS, Lamarre-Cliche M, Bolli P, McLean D, Milot A, Tobe SW, Tremblay G, McKay DW, Townsend R, Campbell N, Gelfer M. A New Algorithm for the Diagnosis of Hypertension in Canada. Can J Cardiol. 2015;31:620–630. doi: 10.1016/j.cjca.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 5.Gore PN, Badar VA, Hardas MM, Bansode VJ. Comparative effect of telmisartan vs lisinopril on blood pressure in patients of metabolic syndrome. Endocr Metab Immune Disord Drug Targets. 2015;15:64–70. doi: 10.2174/1871530314666141128154152. [DOI] [PubMed] [Google Scholar]
- 6.O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848. doi: 10.1097/00004872-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Stergiou GS, Baibas NM, Gantzarou AP, Skeva II, Kalkana CB, Roussias LG, Mountokalakis TD. Reproducibility of home, ambulatory, and clinic blood pressure: implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens. 2002;15:101–104. doi: 10.1016/s0895-7061(01)02324-x. [DOI] [PubMed] [Google Scholar]
- 8.Williams B, MacDonald TM, Caulfield M, Cruickshank JK, McInnes G, Sever P, Webb DJ, Salsbury J, Morant S, Ford I, Brown MJ. Prevention And Treatment of Hypertension With Algorithm-based therapy (PATHWAY) number 2: protocol for a randomised crossover trial to determine optimal treatment for drug-resistant hypertension. BMJ Open. 2015;5:e008951. doi: 10.1136/bmjopen-2015-008951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park E, Kim J. The Impact of a Nurse-Led Home Visitation Program on Hypertension Self-Management among Older Community-Dwelling Koreans. Public Health Nurs. 2015 doi: 10.1111/phn.12220. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Cagli K, Turak O, Canpolat U, Ozcan F, Tok D, Mendi MA, Oksuz F, Siriopol D, Veisa G, Covic A, Kanbay M. Association of Serum Uric Acid Level With Blood Pressure Variability in Newly Diagnosed Essential Hypertension. J Clin Hypertens (Greenwich) 2015 doi: 10.1111/jch.12641. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Y, Zhang L, Wei FF, Thijs L, Kang YY, Wang S, Xu TY, Wang JG, Staessen JA. 3c. 09: Strategies for Classifying Patients Based on Office, Home and Ambulatory Blood Pressure Measurement. J Hypertens. 2015;33(Suppl 1):e39. doi: 10.1161/HYPERTENSIONAHA.114.05038. [DOI] [PubMed] [Google Scholar]
- 12.Ntineri A, Kollias A, Zeniodi M, Moyssakis I, Georgakopoulos D, Servos G, Vazeou A, Stergiou GS. 3b. 02: 24-Hour Ambulatory Central Blood Pressure Variability and Target-Organ Damage in Adolescents and Young Adults. J Hypertens. 2015;33(Suppl 1):e34. [Google Scholar]
- 13.Shimada K, Kario K, Kushiro T, Teramukai S, Ishikawa Y, Kobayashi F, Saito I. Differences between clinic blood pressure and morning home blood pressure, as shown by Bland-Altman plots, in a large observational study (HONEST study) Hypertens Res. 2015;38:876–82. doi: 10.1038/hr.2015.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parati G, Faini A, Valentini M. Blood pressure variability: its measurement and significance in hypertension. Curr Hypertens Rep. 2006;8:199–204. doi: 10.1007/s11906-006-0051-6. [DOI] [PubMed] [Google Scholar]
- 15.Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Bjorklund-Bodegard K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension. 2010;55:1049–1057. doi: 10.1161/HYPERTENSIONAHA.109.140798. [DOI] [PubMed] [Google Scholar]
- 16.Hermida RC, Ayala DE, Fernandez JR, Portaluppi F, Fabbian F, Smolensky MH. Circadian rhythms in blood pressure regulation and optimization of hypertension treatment with ACE inhibitor and ARB medications. Am J Hypertens. 2011;24:383–391. doi: 10.1038/ajh.2010.217. [DOI] [PubMed] [Google Scholar]
- 17.Mancia G, Parati G. Office compared with ambulatory blood pressure in assessing response to antihypertensive treatment: A meta-analysis. J Hypertens. 2004;22:435–445. doi: 10.1097/00004872-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Gu D, He J, Coxson PG, Rasmussen PW, Huang C, Thanataveerat A, Tzong KY, Xiong J, Wang M, Zhao D, Goldman L, Moran AE. The Cost-Effectiveness of Low-Cost Essential Antihypertensive Medicines for Hypertension Control in China: A Modelling Study. PLoS Med. 2015;12:e1001860. doi: 10.1371/journal.pmed.1001860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neldam S, Dahlof B, Oigman W, Schumacher H. Early combination therapy with telmisartan plus amlodipine for rapid achievement of blood pressure goals. Int J Clin Pract. 2013;67:843–852. doi: 10.1111/ijcp.12180. [DOI] [PubMed] [Google Scholar]
- 20.Jadhav U, Hiremath J, Namjoshi DJ, Gujral VK, Tripathi KK, Siraj M, Shamanna P, Safar M. Blood pressure control with a single-pill combination of indapamide sustained-release and amlodipine in patients with hypertension: The EFFICIENT study. PLoS One. 2014;9:e92955. doi: 10.1371/journal.pone.0092955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kengne AP, Patel A, Colagiuri S, Heller S, Hamet P, Marre M, Pan CY, Zoungas S, Grobbee DE, Neal B, Chalmers J, Woodward M. The Framingham and UK Prospective Diabetes Study (UKPDS) risk equations do not reliably estimate the probability of cardiovascular events in a large ethnically diverse sample of patients with diabetes: the Action in Diabetes and Vascular Disease: Preterax and Diamicron-MR Controlled Evaluation (ADVANCE) Study. Diabetologia. 2010;53:821–831. doi: 10.1007/s00125-010-1681-4. [DOI] [PubMed] [Google Scholar]
- 22.Hermida RC, Ayala DE, Fontao MJ, Mojon A, Fernandez JR. Chronotherapy with valsartan/amlodipine fixed combination: improved blood pressure control of essential hypertension with bedtime dosing. Chronobiol Int. 2010;27:1287–1303. doi: 10.3109/07420528.2010.489167. [DOI] [PubMed] [Google Scholar]
- 23.Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, Murata M, Kuroda T, Schwartz JE, Shimada K. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–1406. doi: 10.1161/01.cir.0000056521.67546.aa. [DOI] [PubMed] [Google Scholar]