Abstract
Pyoderma gangrenosum (PG), an extra-intestinal manifestation of ulcerative colitis (UC), is extremely rare. Up to now, there is no any data reported the occurrence of PG in joints, especially in China. The management of PG associated with UC is a therapeutic challenge. Our report here showed that a female patient diagnosed as UC complained a pustule in the dorsal side of left wrist, primarily was diagnosed as bone tuberculosis. The pustule progressed rapidly into a severe painful necrolytic cutaneous ulcer with a pale purple irregular destructive ulcer edge, this patient was diagnosed by UC complicated with PG, and skin lesions were cured by UC treatment. Here, we for the first time present a case acquired correct diagnosis and successful treatment of UC associated with PG of articulations carpi. We report this case here in order to provide more information about this disease to more doctors, furthermore, to decrease the rates of misdiagnosis and missed diagnosis.
Keywords: Pyoderma gangrenosum, ulcerative colitis, articulations carpi, infliximab
Introduction
Pyoderma gangrenosum (PG) associated with ulcerative colitis (UC) is extremely rare. It occurs in less than 1% of patients with UC [1,2]. In China, there is no case report regarding PG in UC patients. The management of PG associated with UC is a therapeutic challenge, especially in China. We herein present a case of wrist PG associated with UC treated with infliximab and skin graft successfully.
Case report
A 40-year-old female patient with 8 year history of UC presented with redness, swelling and pain of the left wrist dorsal skin for 1 month was primarily diagnosed as bone tuberculosis and admitted to the department of orthopedics of our hospital. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of our hospital. Written informed consent was obtained from all participants.
Admission physical examination revealed redness and swelling of the left wrist dorsal skin, which is about 4.0 cm in diameter. X-ray showed the cortical bones of her left wrist were intact, no destruction (Figure 1A). PPD test was negative. On day 2, pustule (0.8 cm in diameter) appeared at the site of dermal lesion on the left wrist. On 3rd day, the pustule ulcerated, complicated with some white viscous secretion and bloody exudation. No pathogenic bacteria were detected from the exudation. Histopathology showed inflammatory necrosis tissues, with several infiltrated neutrophils. The range of the swelling and ulceration expanded progressively (Figure 1B). Within 9 days after her admission, 8 purple pustules gradually occurred on the skin of both lower extremities, some ulcerated (Figure 1C). At the same time of her left wrist skin lesion developed, bloody mucopurulent stool occurred, about 10 times a day, with more blood. Her body temperature was from 38.1°C to 39°C. She was transferred to the Gastroenterology department. Emergency colonoscopy showed diffused hyperemia, edema, erosions, focal superficial ulcers, pseudopolyps and purple bloody bullas in the rectosigmoid (Figure 1D). Biopsy tissue pathology showed severe mucosal inflammation and ulcer (Figure 1E). Laboratory examination findings were as follows: stool test showed red blood cell (RBC) and white blood cell (WBC) in all visual fields. No pathogenic bacteria could be cultured in the stool. Erythrocyte sedimentation rate (ESR) was 106 mm/h. C-reactive protein (CRP) level was 245 mg/L. She was diagnosed as severe UC complicated with PG. The patient was commenced on mesalazine 1.0 g po. qid, prednisolone 60 mg iv by drip qd, and infliximab 300 mg (5 mg/kg body weight) five times at weeks 0, 2, 6 and every 8 weeks after that. Both the skin lesion and intestinal symptoms significantly improved after treatment. Ten days later, her stool turned formed, with normal stool test result. At the same time, laboratory examination improved: ESR decreased to 25 mm/h and CRP returned to 3.38 mg/L. The granulation tissue of her left wrist grew well, and was covering the blood vessels and tendons. She was transferred to the hand surgery department for skin graft. Seven days after surgery, skin grafts survived well (Figure 1F). Review of colonoscopy showed that hyperemia, edema and erosions were improved, and the ulcers and purple bloody bullas disappeared (Figure 1G). In the two months follow-up, her condition was stable, and her left wrist skin was healed.
Figure 1.
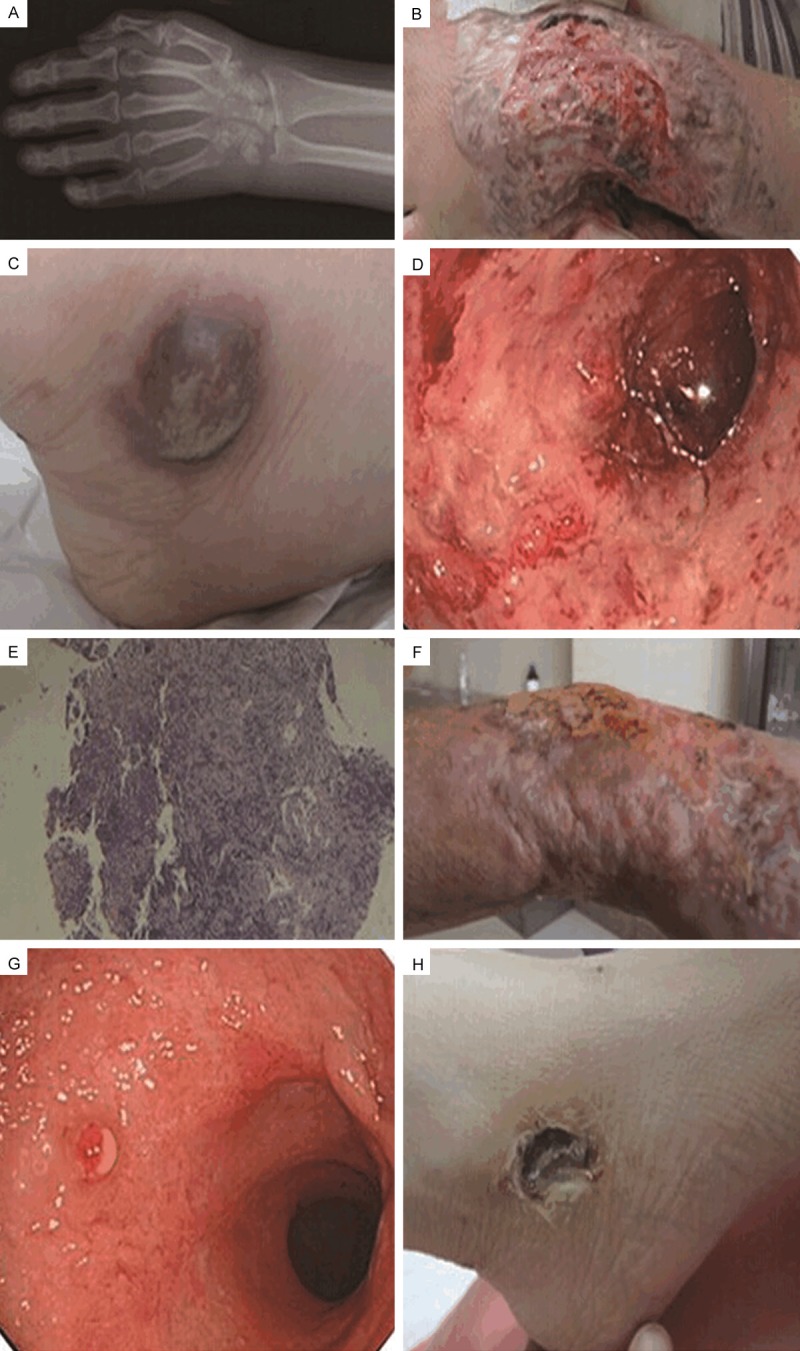
Features of PG and UC. A: X-ray plain film taken at June 21, 2011 shows that all the bones in left waist are integrated and normal. B: June 30, 2011, a 10 cm × 6 cm of skin ulceration with a pale purple irregular edge at the back of left waist is showed, and the vessels and tendons are exposed. C: June 30, 2011, a purple pustule at left lower extremity and another purple pustule at the external malleolus of right feet. D: June 30, 2011, colonoscopy exhibits that mucous membrane of colon shows hyperemia, oedemia, widespread erosion, superficial ulcer and purple blood blister. E: June 30, 2011, histopathological results of mucous membrane of colon show severe mucosal inflammation. F: October 10, 2011, skin ulceration at the left waist is healed well two months after discharge. G: August 17, 2011, rechecked colonoscopy shows hyperemia, few erosion and polypus-like hyperplasia in mucous membrane of colon. H: July 6, 2011, pustules at left lower extremity and external malleolus of right feet start to form scars.
Discussion
PG is a rare immune-mediated inflammatory neutrophilic dermatosis with unclear etiology [3]. It characteristically presents as one or more painful ulcers with violaceous, undermined borders on the lower extremities. It was reported that about 50% of PG might have association with systemic disorders, such as inflammatory bowel disease (IBD), connective tissue disease, haematological diseases, etc. [4].
As an extraintestinal manifestation of IBD, PG is the second frequently documented cutaneous lesion in IBD patients, and occurs approximately 1-2% patients with IBD [5]. The prevalence of cutaneous lesions in UC patients is 1.9% by analysis of clinical characteristics of 3100 cases of UC from 23 hospitals in China [6]. It is lower than that of 9%-19% reported in western [7]. Up to now, the exact information on the prevalence of PG associated with UC is absent in China.
The diagnosis of PG is not always straightforward in that PG associated with UC is extremely rare, and can’t be commonly encountered by clinicians. Just as the case abovementioned, the patient initially was admitted to the department of orthopedics because of obvious symptoms of left wrist, and gained correct diagnosis in time because of bowel flares. But the correlation of PG with IBD activity is controversial. One study included 14 cases of patients with UC suggested no relationship between active UC and the PG [8]. It reminds us of the importance of investigating the patient’s past medical history.
The treatment of PG associated with UC is empirical and lack of detailed data due to low incidence in China. At present, the mainstay treatment of PG remains immunosuppression and the most commonly used drugs are systemic corticosteroids. Some several case reports and reviews have demonstrated the efficacy of infliximab or etanercept, inhibitors of tumor necrosis factor-α (TNF-α), in the treatment of PG associated with IBD. The only one randomized, double blind, placebo-controlled trial indicated infliximab could improve symptoms of patients with PG significantly compared with the placebo [9]. Andrisani et al. reported a case of UC-associated PG treated with infliximab and surgery successfully [10]. The main indication of infliximab therapy in PG-associated with IBD is steroid and immunosuppressive treatment failure [11]. In our clinical situation, taking into account the progressive PG and severe UC flare-up, we chose to treat patient with infliximab and intravenous steroid in order to alleviate the patient’s symptoms as soon as possible and create appropriate condition for skin graft. Both the skin lesion (Figure 1H) and intestinal symptoms improved significantly after combined therapy.
In conclusion, here we represent a case of PG associated with UC occurred firstly in the dorsal side of left wrist. The skin lesions in the dorsal side of left wrist rapidly deteriorated in that the early onset was misdiagnosed as bone and joint disease, and rapidly alleviated by timely diagnosis and aggressive therapy. PG appeared at joints has not yet been reported, clinicians can raise awareness of diagnosis and treatment on PG associated with UC and decrease the rates of misdiagnosis and missed diagnosis by this report.
Disclosure of conflict of interest
None.
References
- 1.Naik CL, Singh G, Kumar L, Lokanatha K. Bullous pyoderma gangrenosum associated with ulcerative colitis. Indian J Dermatol Venereol Leprol. 2008;74:68–70. doi: 10.4103/0378-6323.38421. [DOI] [PubMed] [Google Scholar]
- 2.Menachem Y, Gotsman I. Clinical manifestations of pyoderma gangrenosum associated with inflammatory bowel disease. Isr Med Assoc J. 2004;6:88–90. [PubMed] [Google Scholar]
- 3.Marzano AV, Trevisan V, Lazzari R, Crosti C. Pyoderma gangrenosum: study of 21 patients and proposal of a 'clinicotherapeutic' classification. J Dermatolog Treat. 2011;22:254–260. doi: 10.3109/09546631003686069. [DOI] [PubMed] [Google Scholar]
- 4.Ueda M, Katoh M, Tanizaki H, Tanioka M, Matsumura Y, Miyachi Y. Refractory pyoderma gangrenosum associated with ulcerative colitis successfully treated with infliximab. Dermatol Online J. 2012;18:12. [PubMed] [Google Scholar]
- 5.Callen JP. Pyoderma gangrenosum. Lancet. 1998;351:581–585. doi: 10.1016/S0140-6736(97)10187-8. [DOI] [PubMed] [Google Scholar]
- 6.Infections Bursal Disease Cooperation Group of China. A retrospective study of 3100 in patients with ulcerative colitis in China. Chin J Dig. 2006;26:368–372. [Google Scholar]
- 7.Thrash B, Patel M, Shah KR, Boland CR, Menter A. Cutaneous manifestations of gastrointestinal disease: part II. J Am Acad Dermatol. 2013;68:211, e1–33. doi: 10.1016/j.jaad.2012.10.036. [DOI] [PubMed] [Google Scholar]
- 8.Thornton JR, Teague RH, Low-Beer TS, Read AE. Pyoderma gangrenosum and ulcerative colitis. Gut. 1980;21:247–248. doi: 10.1136/gut.21.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brooklyn TN, Dunnill MG, Shetty A, Bowden JJ, Williams JD, Griffiths CE, Forbes A, Greenwood R, Probert CS. Infliximab for the treatment of pyoderma gangrenosum: A randomized, double blind, placebo controlled trial. Gut. 2006;55:505–509. doi: 10.1136/gut.2005.074815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrisani G, Guidi L, Papa A, Potenza AE, Cervelli D, Armuzzi A. A case of pyoderma gangrenosum with ulcerative colitis treated with combined approach: infliximab and surgery. J Crohns Colitis. 2013;7:421–426. doi: 10.1016/j.crohns.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 11.Juillerat P, Christen-Zach S, Troillet FX, Gallot-Lavallée S, Pannizzon RG, Michetti P. Infliximab for the treatment of disseminated pyoderma gangrenosum associated with ulcerative colitis. Case report and literature review. Dermatology. 2007;215:245–251. doi: 10.1159/000106584. [DOI] [PubMed] [Google Scholar]


