Abstract
Patients with giant retroperitoneal liposarcomas are considered at great risks of perioperative complications and require meticulous anaesthetic management. There have been few reports about anaesthetic management of giant retroperitoneal liposarcoma. We present the case of a 66-year-old patient who suffered from a giant retroperitoneal liposarcoma (diameter 45 cm and weigh 4.5 kg), needing a resection surgery under general anesthesia. We successfully managed anesthesia procedures in this patient using FloTrac/VigileoTM monitoring system without major perioperative complications. The surgery was completed uneventfully and the patient recovered smoothly. After reviewing the literature, we summarize FloTrac/VigileoTM monitoring system is useful to help anaesthesiologists adjust infusion rate to maintain the stability of circulatory state. Anesthetic monitoring, fluid management and temperature control need to be focused in the anesthetic management.
Keywords: Retroperitoneal liposarcoma, general anesthesia, FloTrac VigileoTM monitoring system
Introduction
Liposarcoma is a rare type of malignant tumor that arises in fat cells in deep soft tissue [1]. Patient usually occurs symptoms of pain or functional disturbances only when the tumor is very large. Well-differentiated liposarcomas treated with surgery and radiation have a low recurrence rate (about 10%) and rarely metastasize. Five-year survival rates vary from 100% to 56% based on histological subtype [2,3]. We report the anesthetic management of a case with a giant retroperitoneal liposarcoma measuring 45 cm in diameter and 4.5 Kg in weight using FloTrac/VigileoTM monitoring system. The anesthetic management of the patient is associated with several risks and challenges. There were no major perioperative complications in hemodynamic and respiratory status, such as supine hypotensive syndrome or pulmonary edema.
Case report
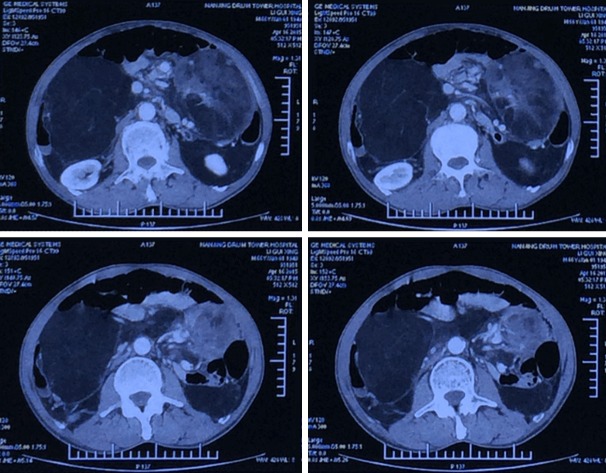
A 66-year-old man (BMI 25.95) with a giant abdominal tumor was scheduled for tumor resection under general anesthesia (Figure 1). He suffered from lower abdominal pain for 3 months and was diagnosed giant retroperitoneal tumor. On general physical examination, thoracoabdominal computed tomography demonstrated the presence of three voluminous masses connected to each other extending from the sub-hepatic space up to the pelvic cavity. One tumor was in the right upper abdominal cavity measuring 107 mm × 131 mm × 150 mm, another tumor was in the left upper abdominal cavity measuring 97 mm × 125 mm × 130 mm, the biggest tumor was in inferior abdominal cavity measuring 156 mm × 175 mm × 315 mm (Figure 2). His vital signs were blood pressure 142/72 mmHg, HR 60 per minute, and SpO2 96% to 99%. Preoperative hemogram, Random blood sugar, electrocardiogram, electrolytes, renal function tests, and chest radiograph were normal. The patient was planned for resection surgery under general anesthesia.
Figure 1.

Preoperative view of the patient showed remarkably distended abdominal tumor.
Figure 2.
CT scan showed the presence of the bulky lesion stretching from the subhepatic region to the pelvic cavity. One tumor was in the right upper abdominal cavity measured 107 mm × 131 mm × 150 mm, another tumor was in the left upper abdominal cavity measured 97 mm × 125 mm × 130 mm, the biggest tumor was in inferior abdominal cavity measured 156 mm × 175 mm × 315 mm.
Prior to induction of general anesthesia, an arterial catheter was inserted under local anesthesia to measure ABP, CI and SVV were measured with a FloTract/VigileoTM system (Edwards Lifesciences, USA). The patient was induced with midazolam 0.05 mg/kg, propofol 1.5 mg/kg, fentanyl 2 μg/kg and vecuronium 0.1 mg/kg intravenously, preoxygenation was done for 3 min before tracheal intubation was facilitated. Ventilation was mechanically controlled and adjusted to maintain end-tidal CO2 at 30-35 mmHg. A central venous catheter (Edwards ifescience, Irvine, CA, USA) was inserted in his right internal jugular vein under ultrasound guidance to monitor CVP and to administer vasoactive drugs if necessary. Electrocardiogram, ABP, SpO2, CI, SVV, CVP and nasopharyngeal temperature were continuously monitored throughout the surgery. Anesthesia was maintained with intravenous propofol at 100 μg/kg/min. Remifentanil (0.25 μg/kg/min) was administered as analgesic intravenously. Intraoperative muscle relaxation was maintained with vecuronium (0.1 mg/kg). Since exposure of skin for prolonged periods and receipt of large volumes of intravenous and irrigation fluids, we kept the patient warm actively to avoid inadvertent perioprative hypothermia.
Total surgery time was 360 mins and the blood loss was around 650 ml (Figure 3). Monitoring of CO, SVV and CVP is very important during the surgery. In this case, there were two episodes of tumor resction, following resction from the first tumor, ABP and CI decreased, but SVV remained within normal ranges. Therefore, we didn’t increase fluid administration rate. When the remaining two tumors were lifted up, both CI and SVV increased, but the increase of SVV was 10%, still within normal ranges. We only decreased the speed of tumor resection without increasing fluid administration rate for avoiding excessive transfusion (Figure 4). The vital parameters remained stable throughout the course of surgery, the intravenous fluid was titrated to maintain CVP of 8-12 mmHg and SVV below 12%. After surgery, he was transferred to the intensive care unit (ICU) and transferred to general surgery department on POD 2. He was discharged without any complication on POD 6.
Figure 3.

A picture of the removed surgical specimen including three tumors.
Figure 4.
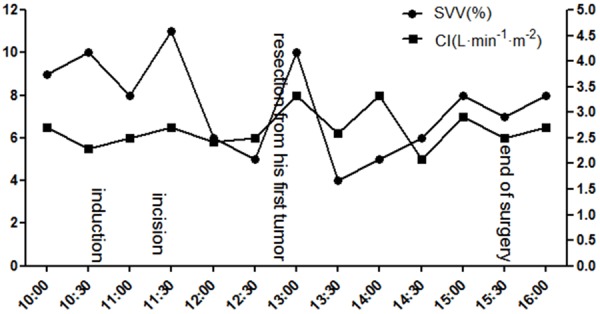
Intra-operative anesthetic management for the resection of the tumors shows that the SVV and CI changed with the tumor resection.
Discussion
Patients with giant retroperitoneal liposarcoma are considered as having greater risks of perioperative complications and require meticulous anesthetic management. The giant retroperitoneal tumor may have some features [4] which need more attention, such as (1) the tumor increase abdominal pressure, inducing retroperitoneal vascular congestion seriously; (2) the tumor compress abdominal aortic vascular and increased cardiac afterload; (3) the tumor compress the gastrointestinal tract so that make the patients malnutrition or anemia; (4) diaphragm drive up, reducing respiratory-system compliance, etc. According to these features, general anesthesia and anesthetic management for giant tumor resection in these cases have several associated risks [5,6]. Nobuko Ohashi [7] reported a patient with giant abdominal tumor causing respiratory distress and they did not use musle relaxant until surgeons completed preparation for the operation in case spontaneous respiration was lost. Fortunately, the tumor in our case did not cause respiratory distress and SpO2 could keep from 96% to 99%. We adopt normol procedure of anesthesia inducement. For intra-operative management, frequent communication between surgeons and the anesthesiologist is extremely important, as manipulation of the tumor, clamping and unclamping of the aorta.Keiko Bamba [8] reported the anesthetic management of a patient scheduled for tumor resection with a giant ovarian tumor containing 83 L of fluid. The main concerns in anesthetic management was cystic fluid should be drained slowly to maintain the stability of circulatory state. By contrast, our case had a solid mass tumor that could not be drained preoperatively. Rapid removal of tumor may lead to unexpected redistribution of blood or massive blood loss, these procedures cause complications such as hypotension, anemia, cardiac arrhymias, etc. We used FloTrac/VigileoTM monitoring system [9] and maintained stable hemodynamics in our patient. Monitoring of CO, SVV and CVP provided stable hemodynamic management during surgery.
Albergaria VF [8] presented a case of pulmonary edema after upper airways obstruction in a patient with acromegaly. Re-expansion pulmonary (RPE) develops upon rapid expansion of chronically collapsed lungs owing to increased pulmonary vascular permeability [9,10]. The risk factors include evacuation volume more than 2000 ml or lung collapse over a period of 3 or more days. There is no standard method to prevent RPE, it has been suggested that it is better to re-expand collapsed lungs slowly with spontaneous respiration [11], but not to perform a lung recruitment maneuver to prevent RPE. In our case, the removal of the tumors did not cause RPE.
Temperature management during surgery is associated with improved clinical outcomes and can be used as a quality measure [12]. Inadvertent perioperative hypothermia (a drop in core temperature to below 36°C) occurs because of interference with normal temperature regulation by exposure of skin for prolonged periods, anaesthetic drugs and receipt of large volumes of intravenous and irrigation fluids. It can adversely affect the outcome of surgery and the patient’s postoperative outcome [13]. In this case, we kept the ambient temperature in the operating room 22 degrees and infusions and irrigation fluids were warmed first, a forced-air warming blanket was prepared intraoperatively and postoperatively.
In this case, we described a successful procedure for anesthetic management for a case with giant retroperitoneal liposarcoma. FloTrac/VigileoTM monitoring system is useful to help anaesthesiologists adjust infusion rate to maintain the stability of circulatory state. Anesthetic monitoring, fluid management and temperature control need to be focused in the anesthetic management.
Acknowledgements
This research was supported by Key Subject of Anesthesiology in Jiangsu Province, China (XK 201140).
Disclosure of conflict of interest
None.
References
- 1.Perez EA, Gutierrez JC, Moffat FL Jr, Franceschi D, Livingstone AS, Spector SA. Retroperitoneal and truncal sarcomas: prognosis depends upon type not location. Ann Surg Oncol. 2007;14:1114–22. doi: 10.1245/s10434-006-9255-x. [DOI] [PubMed] [Google Scholar]
- 2.Seo IY, Won HS, Kim JS, Kim HS, Rim JS. A case of recurrent liposarcoma in retroperitoneum. Korean J Urol. 1994;35:1375–8. [Google Scholar]
- 3.Caizzone A, Saladino E, Fleres F, Paviglianiti C, Iaropoli F, Mazzeo C, Cucinotta E, Macrì A. Giant retroperitoneal liposarcoma: Case report and review of the literature. Int J Surg Case Rep. 2015;9:23–6. doi: 10.1016/j.ijscr.2015.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang IY, Herts BR. Retroperitoneal liposarcoma. J Urol. 2013;189:1093–1094. doi: 10.1016/j.juro.2012.11.122. [DOI] [PubMed] [Google Scholar]
- 5.Kotera A, Kouzuma S, Miyazaki N, Taki K, Esaki K. Anesthetic management of a patient with an ultra huge ovarian tumor. Masui. 2009;58:907–909. [PubMed] [Google Scholar]
- 6.Caizzone A, Saladino E, Fleres F, Paviglianiti C, Iaropoli F, Mazzeo C, Cucinotta E, Macrì A. Giant retroperitoneal liposarcoma: Case report and review of the literature. Int J Surg Case Rep. 2015;9:23–6. doi: 10.1016/j.ijscr.2015.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ohashi N, Imai H, Tobita T, Ishii H, Baba H. Anesthetic management in a patient with giant growing teratoma syndrome: a case report. J Med Case Rep. 2014;8:32. doi: 10.1186/1752-1947-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bamba K, Watanabe T, Kohno T. Anesthetic management of a patient with a giant ovarian tumor containing 83 l of fluid. Springerplus. 2013;2:487. doi: 10.1186/2193-1801-2-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramsingh D, Alexander B, Cannesson M. Clinical review: Does it matter which hemodynamic monitoring system is used? Crit Care. 2013;17:208. doi: 10.1186/cc11814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Albergaria VF, Soares CM, Araújo Rde M, de Mendonça WL. Negative-pressure pulmonary edema after transsphenoidal hypophysectomy. Case report. Rev Bras Anestesiol. 2008;58:391–6. doi: 10.1590/s0034-70942008000400009. [DOI] [PubMed] [Google Scholar]
- 11.Irisawa Y, Hiraoka A, Totsugawa T, Chikazawa G, Nakajima K, Tamura K, Yoshitaka H, Sakaguchi T. Re-expansion pulmonary oedema after minimally invasive cardiac surgery with right mini-thoracotomydagger. Eur J Cardiothorac Surg. 2015 doi: 10.1093/ejcts/ezv089. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.De Wolf SP, Deunk J, Cornet AD, Elbers PW. Case Report: Bilateral reexpansion pulmonary edema following treatment of a unilateral hemothorax. F1000Res. 2014;3:318. doi: 10.12688/f1000research.6000.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kondo T, Kusunoki S, Yasuuji M, Kawamoto M, Yuge O. Prevention of reexpansion pulmonary edema during resection of mediastinal tumor with atelectasis. Masui to Sosei. 2006;42:39–41. [Google Scholar]
- 14.Torossian A, Bräuer A, Höcker J, Bein B, Wulf H, Horn EP. Preventing inadvertent perioperative hypotherma. Dtsch Arztebl Int. 2015;112:166–72. doi: 10.3238/arztebl.2015.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scott AV, Stonemetz JL, Wasey JO, Johnson DJ, Rivers RJ, Koch CG, Frank SM. Compliance with Surgical Care Improvement Project for Body Temperature Management (SCIP Inf-10) Is Associated with Improved Clinical Outcomes. Anesthesiology. 2015;123:116–25. doi: 10.1097/ALN.0000000000000681. [DOI] [PubMed] [Google Scholar]