Abstract
Purpose: This study aimed to evaluate the therapeutic effects of electroacupuncture (EA) combined with clean intermittent catheterization (CIC) on spinal cord injury (SCI) induced urinary retention. Methods: A total of 107 patients with SCI induced urinary retention were randomly divided into 3 groups, including group 1 (CIC treatment), group 2 (EA combined with CIC treatment), and group 3 (sham acupuncture combined with CIC treatment). After different treatments, the residual urine volume, voided volume (each time), number of bladder balance patients, and frequency of CIC were recorded and compared. Results: There were no significant differences between group 1 and 3 in number of bladder balance patients and voided volume (ml) at the 1st month. The rate of patients reaching bladder balance was significantly higher in group 2 than group 1 and 3 (P<0.05). The frequency of CIC was significantly less in group 2 than the other groups (P<0.001). The voided volume at the 1st and the 3rd month after surgery was significantly higher in group 2 than that in group 1 and 3 (P<0.001). Meanwhile, after 1 month and 3 months of treatment, residual urine volume was significantly reduced in group 2 compared with that in group 1 and 3 (P<0.001). Conclusion: The therapeutic effects of EA were effective for SCI induced urinary retention by reducing residual urine volume and the frequency of CIC, increasing voided volume, and promoting the balance of vesical function.
Keywords: Urinary retention, spinal cord injury, electroacupuncture, clean intermittent catheterization
Introduction
Urinary retention is a common disease characterized by poor urinary stream with intermittent flow, straining, incomplete voiding, and hesitancy [1]. In clinical, urinary retention could be induced by various factors including obstructive, pharmacology, and neurology [2-5]. According to neurology, lesions on cortex, spine, and peripheral nerve are always the main cause of neurogenic non-obstructive urinary retention [6,7]. It was reported non-obstructive urinary retention was revealed in about 40% of incomplete spinal cord injury (SCI) patients [8].
Nowadays, various therapies have been performed on urinary retention, such as medication [9,10], physiotherapy [11,12], bladder catheterization [13], and surgery [8]. However, some disadvantages and side effects were also reported on these methods. Alpha-blockers and parasympathomimetics were considered to be unsuccessful in the therapy of urinary retention due to its serious side-effects [14,15]. Catheter retention was reported to be associated with a high risk of bacterial colonization, and a close correlation was revealed on urine infection and indwelling time [16,17]. Sacral neuromodulation is a surgery therapy for urinary retention in SCI patients, which also exhibit various side effects, such as the need of new implants, wound infection at implanted pulse generator site, pain, and hematoma [18,19]. Therefore, effective treatment methods with low side effects on urinary retention are urgently needed.
Clean intermittent catheterization (CIC) is a widely used mode for emptying the bladder, which has become an effective treatment method for urinary retention [20]. In addition, it is also considered to be able to reduce infection, protect urinary system and rebuild urinary continence [21]. Besides, electroacupuncture (EA) has also widely used in clinical, which exhibit effective therapeutic effects on urinary retention [22,23]. Although various researches on therapeutic effects of CIC and EA have been performed, related studies on the combination of EA and CIC in SCI induced urinary retention are rare. In this study, CIC, sham acupuncture combined with CIC, and EA combined with CIC were performed to treat SCI induced urinary retention patients, respectively. Then the outcomes of patients including residual urine volume, voided volume (each time), number of bladder balance patients, and frequency of CIC were recorded and compared. Our findings may reveal an effective therapeutic method, which is beneficial to the treatment of SCI induced urinary retention.
Methods
Study design and participants
This study was a single blind, randomized, controlled clinical trial, which was performed in the Department of Rehabilitation Medicine, Affiliated Second Hospital of Jiaxing University, Jiangxi, China. A total of 107 Chinese patients (80 males and 27 females) with urinary retention (residual urine volume > 100 ml) after SCI were collected in Affiliated Second Hospital of Jiaxing University from June 2005 to June 2008. These patients were ranged from 20 to 57 years (mean: 35.7 years) and classified into three groups according to classifications of American Spinal Injury Association (ASIA) [24], including grade B (37 cases), grade C (53 cases), and grade D (17 cases). These patients were included with meeting the following criteria: (1) they had clear consciousness, (2) they were difficulty in urination, (3) they complained of distention and pain in lower abdomen, (4) more than 500 ml residual urine were detected in their bladder. On the contrary, patients with unclear consciousness and psychosis, obstructive retention of urine due to lithangiuria or tumor, acute or chronic renal failure, severe primary diseases (including heart, liver, lung, and hemopoietic system) were excluded in this study.
This study was approved by the Committee of Human Rights related to Human Experimentation of our hospital and written informed consent was obtained from all subjects.
Treatment methods and surgical procedure
According to different treatments of urinary retention, patients were randomly divided into three groups, including group 1 (CIC treatment, n=35, grade B=11, grade C=18, grade D=6), group 2 (EA combined with CIC treatment, n=38, grade B=13, grade C=19, grade D=6), and group 3 (sham acupuncture combined with CIC treatment, n=34, grade B=13, grade C=16, grade D=5) based on the computer-generated list. These treatments lasted for 3 months. Patients were examined every week to verify the inclusion criteria by one of our physician.
CIC treatment
Before catheter placement, behavioral interventions (such as fluid schedules and regular voiding attempts) were firstly performed to induce emiction. Then CIC was carried out by the following steps: (1) Assembling all equipments, including catheter, lubricant, and drainage receptacle (container); (2) Cleaning the penis/vulva of patients, and then opening urethra; (3) Lubricating the catheter; (4) Inserting and advancing the catheter gently; (5) Continuing to advance the catheter for another 1 inch once the urine flow starts and holding it in place until the urine flow stops and the bladder is empty; (6) Removing the catheter gently to ensure the entire bladder is empty; (7) Recording the volume of urine. The exact frequency of CIC is dependent on fluid intake, bladder capacity and post-void residual urine of patients.
EA combined with CIC treatment
EA was performed on patients in the morning once a day. Simply, the patients were placed in lateral position, and filiform needles (0.38 mm in diameter and 5 cm in length) were punctured perpendicularly into Bilateral Baliao (BL) 31-34 (BL 31: Shangliao, BL 32: Ciliao, BL 33: Zhongliao, BL 34: Xialiao, located in 1th-4th posterior sacral foramen respectively, Figure 1) for 3 cm after routine sterilization. The needle punctured by twirling and rotating. When the De-qi occurred, the doctor should make the needling sensation transmit towards perineum and bladder. Then the needles in the acupoints of BL 31 and BL 34 were connected with Electronic Acupuncture Treatment Instrument (SDZ-II, Hwato, China) and lasted for 20 min with pulse frequency of 20 Hz (Figure 2). Finally, CIC was carried out after EA.
Figure 1.
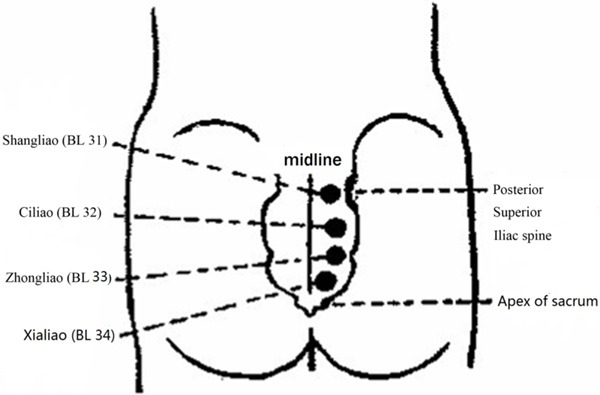
Acupoints of Bilateral Baliao 31-34. (BL 31: Shangliao, BL 32: Ciliao, BL 33: Zhongliao, BL 34: Xialiao, located in 1-4th posterior sacral foramen).
Figure 2.
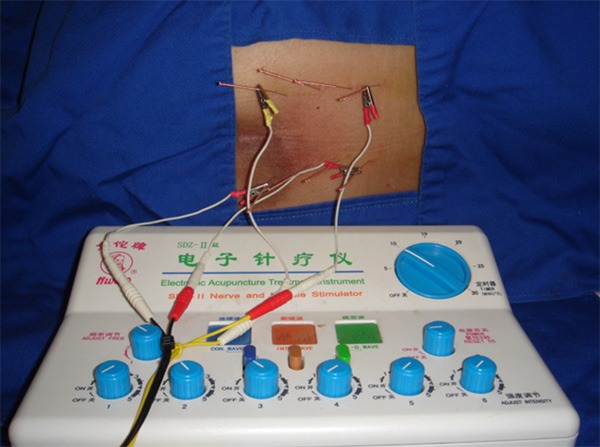
Manipulations of electroacupuncture (EA) in patients treated by EA combined with clean intermittent catheterization (CIC) (Group 2). The needles were punctured perpendicularly into BL 31-34 for 3 cm.
Sham acupuncture combined with CIC treatment
The procedure of CIC was same as described above Acupuncture was performed based on EA method, while the needle was just taping to the dermal surface of BL 31-34 by an adhesive tap without insertion. To facilitate blinding, a mock EA therapeutic instrument, emitted a sound and a blinking light, was attached to the needles (Figure 3).
Figure 3.

Manipulations of EA in patients treated by acupuncture combined with CIC (Group 3). The needle was just taping to the dermal surface of BL 31-34 by adhesive without insertion.
Outcome measurements
The residual urine volume was detected by collecting the residual urine from the catheter after patients’ automatic micturition. Changes on residual urine volume and voided volume of patients were analyzed at the first and third month after different surgeries. Then the number of bladder balance patients was recorded. The bladder was considered to be balanced when (1) adequate urine could be easily discharged at low pressure, (2) approximately 100 ml or less residual urine was left, (3) and no urinary tract infection occurred. In addition, the frequency of CIC was also evaluated based on residual urine volume.
Statistical analysis
Statistical analysis was performed by SPSS version 14.0 (SPSS Inc., Chicago, IL). Quantitative data were expressed as mean ± standard deviation (SD). One-way analyses of variance (ANOVAs) and Chi-square test were used for comparisons among different groups. Pairwise multiple comparisons of quantitative data and qualitative data were analyzed by Tukey Test and Bonferroni Test respectively. A P-value less than 0.05 was considered to be significantly difference.
Results
The clinical information of patients in different groups were listed in Table 1. No significant differences were found in gender, age, duration of SCI, residual urine, and ASIA grade among the three groups.
Table 1.
The clinical state of patients with spinal cord injury (SCI) induced urinary retention
| Group 1 (n=35) | Group 2 (n=34) | Group 3 (n=38) | P value | |
|---|---|---|---|---|
| Gender (male/female) | 1:4 | 1:4 | 1:3 | 0.979 |
| Age (years) | 40.6±9.8 | 39.6±7.6 | 40.75±12.5 | 0.987 |
| Duration of SCI (days) | 22.2±2.4 | 25.8±2.4 | 25.5±2.5 | 0.888 |
| Residual urine volume (ml) | 566.0±8.9 | 591.0±9.4 | 575.0±10.5 | 0.496 |
| ASIA grade B (n) | 11 | 13 | 13 | 0.985 |
| ASIA grade C (n) | 18 | 16 | 19 | |
| ASIA grade D (n) | 6 | 5 | 6 |
ASIA: American Spinal Injury Association. Group 1: clean intermittent catheterization (CIC) treatment; Group 2: electroacupuncture (EA) combined with CIC treatment; Group 3: sham acupuncture combined with CIC treatment.
Outcomes of patients with spinal cord injury (SCI) induced urinary retention by different treatments were listed in Table 2. As a result, there were no significant differences between group 1 and 3 in number of bladder balance patients and voided volume (ml) at the 1st month. However, the rate of bladder balance patients in group 2 was significantly higher than group 1 and 3 (group 1 vs. group 2, P=0.019; group 2 vs. group 3: P=0.019). In addition, the frequency of CIC was significantly less in group 2 than group 1 and 3 (group 1 vs. group 2, P<0.001; group 2 vs. group 3: P<0.001). After 1 month of treatment, residual urine volume was found to be significantly reduced in group 2 patients, which was less than other two groups (group 1 vs. group 2, P<0.001; and group 2 vs. group 3, P<0.001). Meanwhile, the voided volume at the 1st (group 1 vs. group 2, P<0.001; and group 2 vs. group 3, P<0.001) and the 3rd (group 1 vs. group 2, P<0.001; and group 2 vs. group 3, P<0.001) month after surgery was significantly higher in group 2 than that group 1 and 3. Furthermore, the state of residual urine volume and voided volume were identified to be further improved 3 months after surgery (group 1 vs. group 2, P<0.001; and group 2 vs. group 3, P<0.001).
Table 2.
Outcomes of patients with spinal cord injury (SCI) induced urinary retention by different treatments
| Group 1 | Group 2 | Group 3 | P1 | P2 | P3 | |
|---|---|---|---|---|---|---|
| The number of bladder balance patients (n, %)* | 21 (60.0) | 29 (85.29) | 23 (60.5) | 0.019 | 0.963 | 0.019 |
| CIC frequency (times/day) | 1.7±0.14 | 0.35±0.07 | 1.35±0.21 | <0.001 | <0.01 | <0.001 |
| Residual urine volume (ml) in the 1st month | 301.0±8.48 | 213.0±9.19 | 295.0±9.89 | <0.001 | 0.018 | <0.001 |
| Voided volume (ml) in the 1st month | 271.5±12.06 | 375.5±10.06 | 276.5±9.09 | <0.001 | 0.107 | <0.001 |
| Residual urine volume (ml) in the 3rd month | 193.5±10.6 | 113.5±12.02 | 176.5±9.19 | <0.001 | <0.001 | <0.001 |
| Voided volume (ml) in the 3rd month | 360.0±14.14 | 471.0±10.4 | 382.5±10.2 | <0.001 | <0.001 | <0.001 |
qualitative data.
Group 1: clean intermittent catheterization (CIC) treatment; Group 2: electroacupuncture (EA) combined with CIC treatment; Group 3: sham acupuncture combined with CIC treatment. P1: group 1 vs. group 2; P2: group 1 vs. group 3; P3: group 2 vs. group 3.
Discussion
Urinary retention is a common and serious clinical disease in patients with SCI, which is caused by impaired neural control of the lower urinary tract [25]. In clinical, urinary retention could lead to urinary tract infections, hydronephrosis, pyonephrosis and even chronic renal failure, which exhibits great impacts on the daily life of patients [26]. In this study, we evaluated the therapeutic effects of CIC and EA on patients suffered from SCI induced urinary retention, hoping to find an effective therapeutic method for treatment of this disease. As a result, EA combined with CIC showed much better outcomes than the other two methods, indicating that this strategy is more effective in the treatment of SCI induced urinary retention.
CIC is a recommended technique for voiding urinary retention in SCI patients. In this study, CIC was performed on SCI patients with urinary retention to empty the bladder for several times a day. As a result, the urinary retention was significantly improved and bladder balance was achieved in many patients. However, CIC was reported to be able to induce urinary tract infections due to non-sterile catheterization [27,28]. In addition, some psychological problems including discomfiture and low self-respect may also occur during this process. Though clinical management and personalized medical follow-up have been performed to reduce these complications such as psychological disorder, urinary tract injury, discomfort and infection, the high frequency of CIC could still lead to inconveniences of daily life in patients [20,29].
Recently, more and more researchers paid their attention to the use of EA in the treatment of neurogenic bladder dysfunction due to SCI. As reported, EA on BL 35 and Huiyang exhibit an obvious therapeutic effect on urinary retention induced by SCI [30]. EA on conception vessel (CV) such as CV-3, CV-4 as well as BL-32 was beneficial on the recovery time of bladder balance, which was more rapid than those receiving usual medications and training of self-catheterization [31]. EA on Hou Hsi (SI-3) and BL-62 combined with auricular acupoints could enhance the recovery of bladder function in acute SCI patients [32]. In this study, EA on BL 31-34 combined with CIC was performed on SCI induced urinary retention patients in group 2. The results showed that the rate of bladder balance patients treated with EA plus CIC was significantly higher than the other two groups (CIC treatment). In addition, the residual urine volume at each follow-up time were found to be significantly reduced than the CIC treatments, and the voided volume were found to be significantly increased at each follow-up time, indicating that the EA plus CIC treatment can significantly improve the function of bladder contraction. These phenomena further illustrated the effective role of EA on the treatment of urinary retention, and the validity of acupoints BL 31-34.
BL 31-34 was located in the 1th-4th posterior sacral foramen, which was below muscular branches of 1-4 sacral nerves. The ateral horn cells of 2-4 sacral cords were regulation center of urinary, and vesical parasympathetic ganglia could dominate detrusor muscle and bladder sphincter by postganglionic fibers. As we known, sacral neuromodulation was considered to be effective in non-obstructive urinary retention patients [8,33]. Therefore, we speculate the stimulation of EA on BL 31-34 could directly affect 1-4 nerve roots, then induce rhythmic contraction and relax vesical muscles, and finally benefit to voluntary urination and reconstruction of autonomic micturition reflex. Furthermore, EA was also found to be able to reduce the frequency of CIC in patients, which further illustrated the therapeutic effects of EA on improving the quality of life in patients with SCI induced urinary retention.
In conclusion, EA combined with CIC was considered to be more effective on the treatment of SCI induced urinary retention than CIC alone or CIC combined with sham EA by reducing residual urine volume and the frequency of CIC, increasing voided volume, and promoting the balance of vesical function.
Acknowledgements
This study was supported by grants of National Natural Science Foundation of China (NSFC, 81201504) and Zhejiang Provincial National Science Foundation of China (LY12H17004). We thank Second Hospital Affiliated Jiaxing University and Sir Runrun Hospital of Zhejiang University where the study was finished.
Disclosure of conflict of interest
None.
References
- 1.Ugare UG, Bassey IA, Udosen EJ, Essiet A, Bassey OO. Management of Lower Urinary Retention in a Limited Resource Setting. Ethiop J Health Sci. 2014;24:329–336. doi: 10.4314/ejhs.v24i4.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Addison B, Harvey M. Herpes zoster-induced acute urinary retention. Emerg Med Australas. 2013;25:279–281. doi: 10.1111/1742-6723.12079. [DOI] [PubMed] [Google Scholar]
- 3.Teuteberg W. Drug-Induced Acute Urinary Retention #287. J Palliat Med. 2015;18:187–8. doi: 10.1089/jpm.2015.1010. [DOI] [PubMed] [Google Scholar]
- 4.Tomaszewski D, Balkota M, Truszczynski A, Machowicz A. Intrathecal morphine increases the incidence of urinary retention in orthopaedic patients under spinal anaesthesia. Anaesthesiol Intensive Ther. 2014;46:29–33. doi: 10.5603/AIT.2014.0006. [DOI] [PubMed] [Google Scholar]
- 5.Kearns JT, Esposito D, Dooley B, Frim D, Gundeti MS. Urodynamic studies in spinal cord tethering. Childs Nerv Syst. 2013;29:1589–1600. doi: 10.1007/s00381-013-2136-2. [DOI] [PubMed] [Google Scholar]
- 6.Sakakibara R, Uchiyama T, Yamanishi T, Hattori T. Urinary function in patients with corticobasal degeneration; comparison with normal subjects. Neurourol Urodyn. 2004;23:154–158. doi: 10.1002/nau.20013. [DOI] [PubMed] [Google Scholar]
- 7.Lujan Marco S, Garcia Fadrique G, Ramirez Backhaus M, Arlandis Guzman S, Martinez Agullo E, Jimenez Cruz JF. Urological findings in spinal cord ischemia. Actas Urol Esp. 2008;32:926–930. doi: 10.1016/s0210-4806(08)73961-5. [DOI] [PubMed] [Google Scholar]
- 8.Lombardi G, Musco S, Celso M, Del Corso F, Del Popolo G. Sacral neuromodulation for neurogenic non-obstructive urinary retention in incomplete spinal cord patients: a ten-year follow-up single-centre experience. Spinal Cord. 2014;52:241–245. doi: 10.1038/sc.2013.155. [DOI] [PubMed] [Google Scholar]
- 9.Sharifi SH, Mokarrar MH, Khaledi F, Yamini-Sharif R, Lashay A, Soltani MH. Does sildenafil enhance the effect of tamsulosin in relieving acute urinary retention? Int Braz J Urol. 2014;40:373–378. doi: 10.1590/S1677-5538.IBJU.2014.03.11. [DOI] [PubMed] [Google Scholar]
- 10.Elbendary M, El-Gamal OM, Soliman MG, Tawfik A, Taha MR. Role of combined use of ketoconazole and tamsulosin in management of acute urinary retention due to benign prostatic obstruction (a randomized controlled trial) Prostate Cancer Prostatic Dis. 2013;16:362–366. doi: 10.1038/pcan.2013.30. [DOI] [PubMed] [Google Scholar]
- 11.Moossdorff-Steinhauser HF, Berghmans B. Effects of percutaneous tibial nerve stimulation on adult patients with overactive bladder syndrome: a systematic review. Neurourol Urodyn. 2013;32:206–214. doi: 10.1002/nau.22296. [DOI] [PubMed] [Google Scholar]
- 12.Kibar Y, Piskin M, Irkilata HC, Aydur E, Gok F, Dayanc M. Management of abnormal postvoid residual urine in children with dysfunctional voiding. Urology. 2010;75:1472–1475. doi: 10.1016/j.urology.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Brouwer TA, Rosier PF, Moons KG, Zuithoff NP, van Roon EN, Kalkman CJ. Postoperative bladder catheterization based on individual bladder capacity: A randomized trial. Anesthesiology. 2015;122:46–54. doi: 10.1097/ALN.0000000000000507. [DOI] [PubMed] [Google Scholar]
- 14.Barendrecht MM, Oelke M, Laguna MP, Michel MC. Is the use of parasympathomimetics for treating an underactive urinary bladder evidence- based? BJU Int. 2007;99:749–752. doi: 10.1111/j.1464-410X.2006.06742.x. [DOI] [PubMed] [Google Scholar]
- 15.Linsenmeyer TA, Horton J, Benevento J. Impact of alpha1-blockers in men with spinal cord injury and upper tract stasis. J Spinal Cord Med. 2002;25:124–128. doi: 10.1080/10790268.2002.11753612. [DOI] [PubMed] [Google Scholar]
- 16.Klis R, Korczak-Kozakiewicz E, Denys A, Sosnowski M, Rozanski W. Relationship between urinary tract infection and self-retaining Double-J catheter colonization. J Endourol. 2009;23:1015–1019. doi: 10.1089/end.2008.0518. [DOI] [PubMed] [Google Scholar]
- 17.Rahman MA, Alam MM, Shahjamal S, Islam MR, Haque ME. Predictive value of urine cultures in evaluation of bacterial colonization of ureteral stents. Mymensingh Med J. 2012;21:300–305. [PubMed] [Google Scholar]
- 18.Lombardi G, Del Popolo G. Clinical outcome of sacral neuromodulation in incomplete spinal cord injured patients suffering from neurogenic lower urinary tract symptoms. Spinal Cord. 2009;47:486–491. doi: 10.1038/sc.2008.172. [DOI] [PubMed] [Google Scholar]
- 19.White WM, Mobley JD 3rd, Doggweiler R, Dobmeyer-Dittrich C, Klein FA. Incidence and predictors of complications with sacral neuromodulation. Urology. 2009;73:731–735. doi: 10.1016/j.urology.2008.11.047. [DOI] [PubMed] [Google Scholar]
- 20.Seth JH, Haslam C, Panicker JN. Ensuring patient adherence to clean intermittent self-catheterization. Patient Prefer Adherence. 2014;8:191–198. doi: 10.2147/PPA.S49060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shaw C, Logan K, Webber I, Broome L, Samuel S. Effect of clean intermittent self-catheterization on quality of life: a qualitative study. J Adv Nurs. 2008;61:641–650. doi: 10.1111/j.1365-2648.2007.04556.x. [DOI] [PubMed] [Google Scholar]
- 22.Liu Z, Zhou K, Wang Y, Pan Y. Electroacupuncture improves voiding function in patients with neurogenic urinary retention secondary to cauda equina injury: results from a prospective observational study. Acupunct Med. 2011;29:188–192. doi: 10.1136/aim.2010.003913. [DOI] [PubMed] [Google Scholar]
- 23.Gao Y, Zhou X, Dong X, Jia Q, Xie S, Pang R. Electroacupuncture for bladder function recovery in patients undergoing spinal anesthesia. Evid Based Complement Alternat Med. 2014;2014:892619. doi: 10.1155/2014/892619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kirshblum SC, Memmo P, Kim N, Campagnolo D, Millis S. Comparison of the revised 2000 American Spinal Injury Association classification standards with the 1996 guidelines. Am J Phys Med Rehabil. 2002;81:502–505. doi: 10.1097/00002060-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 25.de Groat WC, Griffiths D, Yoshimura N. Neural control of the lower urinary tract. Compr Physiol. 2015;5:327–396. doi: 10.1002/cphy.c130056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hernandez Hernandez D, Tesouro RB, Castro-Diaz D. Urinary retention. Urologia. 2013;80:257–264. doi: 10.5301/RU.2013.11688. [DOI] [PubMed] [Google Scholar]
- 27.Wyndaele JJ, Brauner A, Geerlings SE, Bela K, Peter T, Bjerklund-Johanson TE. Clean intermittent catheterization and urinary tract infection: review and guide for future research. BJU Int. 2012;110:E910–917. doi: 10.1111/j.1464-410X.2012.11549.x. [DOI] [PubMed] [Google Scholar]
- 28.Kannankeril AJ, Lam HT, Reyes EB, McCartney J. Urinary tract infection rates associated with re-use of catheters in clean intermittent catheterization of male veterans. Urol Nurs. 2011;31:41–48. [PubMed] [Google Scholar]
- 29.Newman DK, Willson MM. Review of intermittent catheterization and current best practices. Urol Nurs. 2011;31:12–28. 48. quiz 29. [PubMed] [Google Scholar]
- 30.Zhou LY, Li J, Li CM, Yu ZG, Zhang WL, Zheng M, Meng QG, Wang FY, Sheng ZG. Observation on therapeutic effect of electroacupuncture at points Baliao and Huiyang (BL 35) on retention of urine induced by spinal cord injury. Zhongguo Zhen Jiu. 2006;26:237–239. [PubMed] [Google Scholar]
- 31.Cheng PT, Wong MK, Chang PL. A therapeutic trial of acupuncture in neurogenic bladder of spinal cord injured patients--a preliminary report. Spinal Cord. 1998;36:476–480. doi: 10.1038/sj.sc.3100689. [DOI] [PubMed] [Google Scholar]
- 32.Wong AM, Leong CP, Su TY, Yu SW, Tsai WC, Chen CP. Clinical trial of acupuncture for patients with spinal cord injuries. Am J Phys Med Rehabil. 2003;82:21–27. doi: 10.1097/00002060-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Gross C, Habli M, Lindsell C, South M. Sacral neuromodulation for nonobstructive urinary retention: A meta-analysis. Female Pelvic Med Reconstr Surg. 2010;16:249–253. doi: 10.1097/SPV.0b013e3181df9b3f. [DOI] [PubMed] [Google Scholar]


