Abstract
In order to maintain stable upright stance, the postural control system must account for the continuous perturbations to the body’s center-of-mass including those caused by spontaneous respiration. Both aging and disease increase “posturo-respiratory synchronization;” which reflects the degree to which respiration affects postural sway fluctuations over time. Tai Chi training emphasizes the coordination of respiration and bodily movements and may therefore optimize the functional interaction between these two systems. The purpose of the project was to examine the effect of Tai Chi training on the interaction between respiration and postural control in older adults. We hypothesized that Tai Chi training would improve the ability of the postural control system to compensate for respiratory perturbations and thus, reduce posturo-respiratory synchronization. Participants were recruited from supportive housing facilities and randomized to a 12-week Tai Chi intervention (n=28; 86±5yrs) or educational-control program (n=34, 85±6yrs). Standing postural sway and respiration were simultaneously recorded with a force plate and respiratory belt under eyes-open and eyes-closed conditions. Posturo-respiratory synchronization was determined by quantifying the variation of the phase relationship between the dominant oscillatory mode of respiration and corresponding oscillations within postural sway. Groups were similar in age, gender distribution, height, body mass, and intervention compliance. Neither intervention altered average sway speed, sway magnitude or respiratory rate. As compared to the education-control group, however, Tai Chi training reduced posturo-respiratory synchronization when standing with eyes open or closed (p<0.001). Tai Chi training did not affect traditional parameters of standing postural control or respiration, yet reduced the coupling between respiration and postural control. The beneficial effects of Tai Chi training may therefore stem in part from optimization of this multi-system interaction.
Keywords: Tai Chi, Postural Control, Ageing
INTRODUCTION
Human upright stance is inherently unstable and thus requires a complex control system in which sensory systems, motor circuitry, and cardio-respiratory activities function in concert to maintain stability of upright posture [1,5,6,13]. Spontaneous respiration continuously alters intrathoracic volume and thus influences the body’s center-of-mass [2]. When healthy adults stand with eyes open, respiration-induced perturbations to the trunk are accompanied by phasic muscle activation patterns in the lower-extremities and related angular movements about the hips, knees and ankles [4]. The postural control system thus appears to account for respiration, ostensibly with the purpose of minimizing its effect on postural sway [4,20,21,23]. As such, understanding the dynamic interaction between the respiratory and postural control systems may provide new insights into the fundamental control mechanisms associated with bipedal stance.
The dynamics of various physiological processes are naturally complex [23]. Complexity refers to the presence of non-linear, non-stationary fluctuations across multiple time scales in the dynamics of physiological outputs [14]. The dynamics of both respiration and postural sway are complex [12] and as such, quantification of their interactions is non-trivial. The metric “posturo-respiratory synchronization” was recently introduced and provides one way to quantify the influence that respiration has on postural sway [15]. This metric was derived from adaptive signal processing techniques that do not assume linearity or stationarity of involved signals. Specifically, posturo-respiratory synchronization quantifies the degree to which respiration and postural sway, as measured by center of pressure excursions beneath the feet, are synchronized over time. A larger synchronization index indicates a greater influence of respiration on postural sway [15].
Virtually all elements of the postural control system decline in functional capacity as one ages from adulthood into senescence [12,14]. This decline manifests as a diminished ability to detect, respond and overcome perturbations to the body while standing[15]. Recently, Manor et al [15] demonstrated that both aging and chronic brain damage secondary to stroke are associated with increased posturo-respiratory synchronization index; that is, a reduced capacity of the postural control system to counteract respiratory perturbations.
Tai chi, a traditional Chinese martial art form, has been used as an intervention strategy to effectively improve balance in numerous older adult populations [9,10,27,28]. This multi-component therapy incorporates a combination of slow purposeful movements, controlled diaphragmatic breathing and mind-body awareness [10]. As such, Tai Chi may be well-suited to improve the dynamic relationship between respiration and postural control. The purpose of this study was therefore to examine the effect of Tai Chi training on this multisystem interaction. We hypothesized that Tai Chi training would reduce the impact of respiration on postural control in older adults, as evidenced by a training-related decrease in posturo-respiratory synchronization. Due to the explicit goal of integrating respiration and bodily movement, we further hypothesized that the this metric would be more sensitive to Tai Chi training as compared to traditional metrics of average postural sway speed or area.
METHODS
Protocol
A randomized controlled trial was completed to compare the effects of Tai Chi and educational control interventions on numerous outcomes associated with frailty in older adults living in supportive housing facilities (NCT01136723). Eligible participants were assessed at baseline and then randomly assigned to either the Tai Chi or control group. All assessments were conducted within seven days before and after the intervention by study personnel blinded to group assignment. The study was approved by the Hebrew Senior Life Institutional Review Board and all participants provided written informed consent prior to enrollment.
Participants
Men and women >70 years of age were recruited from two supportive living facilities in the Boston area. Once facilities were identified, the study was advertised with flyers and a presentation was given by study personnel at a monthly resident’s meeting. Interested individuals were initially screened for eligibility via phone interview. Potentially eligible individuals then completed an in-person evaluation. Exclusion criteria included 1) an inability to stand or ambulate unassisted, 2) the presence of any symptomatic cardiovascular or respiratory disease, 3) a history of myocardial infarction or stroke within 6 months, 4) self-reported painful arthritis, spinal stenosis, amputation, painful foot lesions, or neuropathy, 5) systolic BP above 160 or diastolic BP above 100mmHg, 6) a known abnormal cardiac rhythm or presence of cardiac pacemaker, 7) diagnosis of Parkinson’s disease, or 8) diagnosis of metastatic cancer or immunosuppressive therapy.
There were 68 eligible participants who enrolled for the study. Six participants withdrew from the study. Reasons for withdrawal included injury unrelated to the study (n=1) and diminished interest in study participation (n=5). A total of 62 participants completed all study procedures.
Interventions
The Tai Chi intervention was conducted within a common area in each housing facility. Two, instructor-led one-hour group training sessions were completed each week for 12 consecutive weeks. Group sessions contained a maximum of 12 participants. They were taught by one of three instructors, all with greater than 10 years of experience, including experience teaching older health-impaired adults in the context of clinical trials. Tai Chi training was broadly based upon a program initially developed for patients with heart disease and balance disorders and successfully implemented in several previous studies [3,11,16,22,31–33]. The program consisted of five essential Tai Chi movements and a complementary set of traditional Tai Chi warm-up exercises. The five chosen Tai Chi movements (i.e., ‘raising the power’, ‘withdraw and push’, ‘grasp the sparrow’s tail’, ‘brush knee twist step’, and ‘wave hand like clouds’) are based on the traditional Cheng Man-Ch’ing’s Yang-style short form. The warm-up exercises focused on range-of-motion, incorporating mindfulness and imagery into movement, increasing awareness of breathing and promoting relaxation of body and mind. In addition to attending group-based sessions, participants were provided with an instructional DVD of the entire protocol and instructed to practice at home for 20 minutes at least 3 days per week.
The educational control intervention was time-matched for attention. Participants attended group sessions twice weekly within a common area of each housing facility. Sessions were led by research personnel and included health-related topics and material from published Patient Education Forms (available at http://www.americangeriatrics.org). Sessions were semi-structured and contained 30 minutes of lecture and 30 minutes of group discussion.
Assessments
Baseline and follow-up testing included a battery of cardiovascular, cognitive and physical assessments. We limited this secondary analysis to baseline and follow-up assessments of standing postural control, which was assessed during two 60-second trials of standing on a stationary force plate completed in random order; one with eyes-open and one with eyes-closed. Center-of-pressure (COP) and respiratory dynamics (recorded by a Noraxon DTS (Scottsdale, AZ) respiratory belt secured at the sternum level) were simultaneously recorded at 240 Hz. Subjects were instructed to stand as still as possible.
Quantification of Posturo-respiratory Synchronization
Respiratory and COP time-series were down-sampled to 50 Hz and used to calculate the posturo-respiratory synchronization index, which has been previously discussed in detail [15]. To summarize, the synchronization index is calculated using a three step process:
Ensemble Empirical Mode Decomposition (EEMD) was used to extract the dominant respiratory oscillations and the corresponding oscillations within the anterior-posterior (AP) and mediolateral (ML) COP time-series.
The instantaneous phases of the extracted oscillatory modes were calculated at each time point using the Hilbert transform. Phase differences between respiration and AP and ML sway were calculated separately.
A phase synchronization index was calculated based on Shannon Entropy of phase differences. The synchronization index ranges from 0 to 1 with larger values indicating stronger phase synchronization between oscillating signals.
A surrogate data analysis technique was used to determine if the value of observed synchronization would be greater than that due to chance. The original Synchronization Index was compared to indices derived from surrogate signals generated by shifting the respiration signal in time. We examined the surrogate respiration signals with time shifts from -9 sec to 9 sec (increment = 1 sec.). For a non-random synchronization, it was expected that the original index value would be larger than those indices generated from surrogate signals.
Traditional metrics of respiration and postural control were also calculated. For each trial, the area of an ellipse enclosing 95% of the COP trajectory (Area) was computed, along with the average velocity of the COP trajectory over time (Velocity). Mean respiratory rate (RR) was calculated from the extracted dominant respiratory mode.
Statistical Analysis
Analyses were performed using SAS 9.1 software (SAS Institute, Cary, NC). First, to validate that the calculated posture-respiratory synchronization index was not the result of randomly occurring phase synchronizations, standard least squares models were used to determine if time shifting the respiratory time-series relative to each COP time-series significantly altered the value of synchronization. For each participant, separate analyses were completed for eyes-open and eyes-closed conditions, and for synchronization between respiratory and COP oscillations in the ML and AP directions.
Descriptive statistics were used to summarize all variables. One-way ANOVAs were used to examine potential differences in the group characteristics of age, body mass, height, and the number of missed classes. Repeated measures MANOVA analysis was used to evaluated the effects of group (Tai Chi vs. education), visit (pre/post intervention), and condition (eyes open or close) on all of the outcome variables (center of pressure area and velocity, respiratory rate, and posturo-respiratory synchronization) collectively. The multivariate outcome in this model indicates whether there are significant differences with respect to the dependent variables across the independent variables (group, visit, and visual condition). Significant main effects and interactions from the multivariate analysis were further analyzed using one-way ANOVAs. The alpha level was set at 0.05 for all tests.
RESULTS
Demographic characteristics were similar between groups (Table 1). The Tai Chi and control groups had similar gender distribution (82% were female), age, height, and body mass. Attendance in the Tai Chi or educational classes was high (88±15%) and also similar between groups (p>0.05).
Table 1.
Group Characteristics (Means ± SD)
| Tai Chi | Control | P-value | |
|---|---|---|---|
| #Participants (M/F) | 28 (5/23) | 34 (6/28) | |
| Age (years) | 86.7±5.4 | 85.0±6.4 | 0.31 |
| Mass (kg) | 63.3±12.8 | 68.7±11.8 | 0.16 |
| Height (cm) | 154.4±10.6 | 157.2±10.2 | 0.40 |
| Classes Missed | 3±3 | 3±3 | 0.58 |
The statistical analysis confirmed that all independent variables had significant main effects: group (F4,195=7.3; P<0.0001), visit (F4,195=4.04; P<0.004), and condition (F4,195=85.49; P<0.0001).A significant group x visit interaction (F4,195=2.65; P<0.03) was also present, indicating that the collective effect of Tai Chi training on all of the outcome variables was different compared to the education control intervention. There were no significant effects for group x condition terms (P>0.05). Univariate ANOVA was employed to determine which of the outcome variables significantly contributed to the main effects we observed from the repeated measures MANOVA.
Traditional Measures of Respiration and Postural Control
The means and standard deviations for respiratory rate (RR) and postural control measures (Area and Velocity) are presented in Table 2. Univariate analyses confirmed that Area and Velocity increased when closing the eyes for both groups (p < 0.01), yet neither was influenced by the Tai Chi intervention. Respiratory rate did not change between visual conditions or after the intervention period for either group.
Table 2.
Traditional measures of respiration and postural control (Means±SD)
| Eyes Open | Eyes Closed | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Group | V1 | V2 | V2-V1 | V1 | V2 | V2-V1 | |
| RR(bpm) | Tai Chi | 15.9±3.4 | 16.8±3.9 | 0.88±3.0 | 17.2±4.4 | 16.9±3.4 | 0.38±2.6 |
| Control | 15.6±3.5 | 16.8±4.5 | 1.12±4.8 | 15.9±3.9 | 16.4±3.8 | 0.69±2.5 | |
| Area (mm2) | Tai Chi | 207.9±123.7 | 197.6±96.9 | 10.4±55.3 | 276.7±203.1 | 267.3±209.5 | 7.21±101.3 |
| Control | 219.3±139.9 | 193.4±101.8 | 15.9±69.7 | 288.9±246.8 | 254.7±199.9 | 31.8±105.3 | |
| Velocity (mm/s) | Tai Chi | 13.8±5.1 | 12.6±4.9 | 1.09±2.8 | 18.9±9.7 | 18.7±11.7 | 0.42±3.5 |
| Control | 16.8±7.8 | 15.2±7.9 | 1.63±3.4 | 20.8±11.4 | 20.5±11.4 | 0.35±5.1 | |
RR= Respiratory Rate; Area = area of the ellipse that cover 95% of the center of pressure data points during one data collect session; Velocity = Average velocity of the center of pressure data points during one data collect session;V1=Visit 1: pre-intervention measures; V2=Visit 2: post-intervention measures; V2-V1= post-intervention – pre-intervention measures.
Two-factor (Group x Vision) MANOVA with repeated measures employed to analyze V2-V1 for all outcome variables. There were no significant differences (main, nor interaction) for the three outcome variables presented in the table.
Posturo-Respiratory Synchronization
Respiration influenced COP fluctuations in the AP direction, but not in the ML direction. Specifically, across all participants, the posturo-respiratory synchronization index calculated from the non-shifted respiratory cycle and AP COP oscillations was greater (p < 0.01) than those indices derived from all time-shifted surrogates. In the ML direction, on the other hand, the synchronization index derived from the original non-shifted time-series did not differ from those indices derived from time-shifted surrogates. As such, the effects of Tai Chi and visual condition on posturo-respiratory synchronization were only examined in the AP direction.
The Effects of Tai Chi on Posturo-respiratory Synchronization
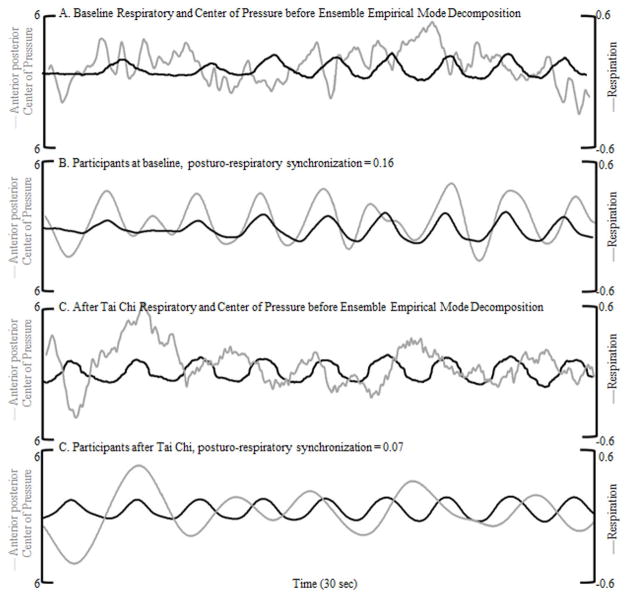
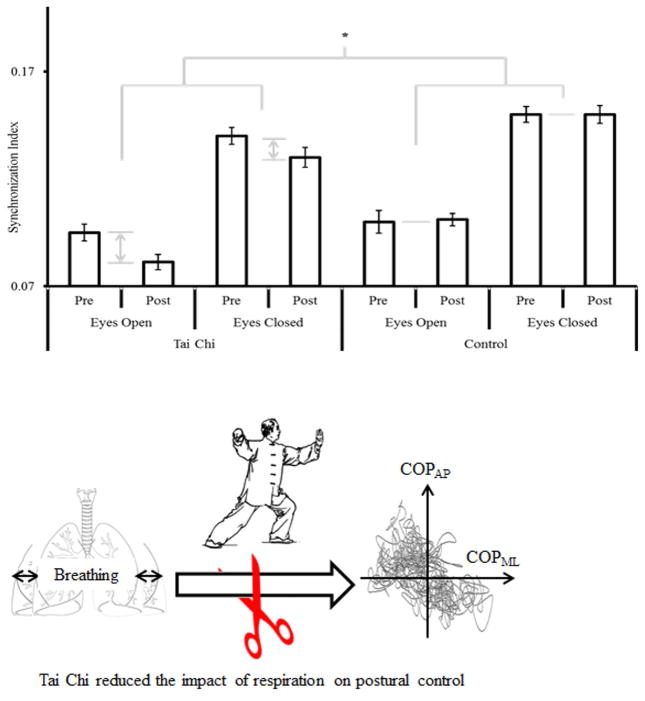
Figure 1 illustrates the relationship between respiratory and AP COP dynamics in a single subject before and after Tai Chi training. The raw time-series (A and C), as well as the dominant respiratory oscillation and corresponding AP COP oscillation as determined by EEMD (B and D)are presented. The phase synchronization between these two signals was visibly altered following the Tai Chi intervention. Figure 2 depicts the overall effects of group, visit, and visual condition on the posturo-respiratory synchronization index. Univariate analysis indicated a significant group x visit interaction (F=6.65; p=0.01). Post-hoc testing revealed that the synchronization index was 1) similar between groups at baseline, and 2) significantly lower within the Tai Chi group at follow-up as compared to the control group at follow-up and both groups at baseline. Similar to traditional measures of postural control, the posturo-respiratory synchronization index increased when closing the eyes for both groups (Condition; F=295.9; p < 0.001). No other main effects or interaction were observed.
Figure 1. Exemplar respiration and anterioposterior center of pressure data during eyes open standing before and after Tai Chi training.
Determination of respiration and anterior-posterior center of pressure dynamics were simultaneously recorded over time and compared. Ensemble Empirical Mode Decomposition (EEMD) was used to decompose each signal into oscillatory modes, each representing the frequency modulation of the signal at a specific frequency range. The raw data prior to EEMD are shown before (A) and after (C) Tai Chi. (B) Shows the decomposed respiratory and center of pressure modes of an 89 year old male before the Tai Chi intervention. The dark black line represents respiration and the light grey line shows center of pressure. After Tai Chi (D) there was less synchronization between respiration and center of pressure for this participant.
Figure 2. The effects of group, time, and visual condition on the posturo-respiratory synchronization index (means ± standard error of the mean).
In both groups, the posturo-respiratory synchronization index was greater when standing with eyes closed as compared to standing with eyes open. Tai Chi training, but not the educational control intervention, was associated with a significant decrease in posture-respiratory synchronization, irrespective of visual condition. The light grey comparison barsindicate the significant main effect of visual condition (p < 0.0001).* indicates a significant group by time interaction (p = 0.01).
DISCUSSION
A 12-week Tai Chi training program, as compared with an educational control intervention, altered the interaction between respiration and AP postural sway in older adults residing in supportive living facilities. Specifically, we applied posturo-respiratory synchronization, a novel application of the synchronization index, to quantify the influence of respiration on standing postural swayoscillations. Our analyses indicated that non-random synchronization of respiration and postural sway exists in the AP direction. Synchronization was similar between the Tai Chi and educational control group at baseline and decreased in the Tai Chi group following the 12 week intervention. The effect of Tai Chi training on the synchronization index was similar whether standing with eyes open or closed. On the other hand, neither intervention altered traditional measures of respiration or postural control. We therefore contend that regular Tai Chi training increases the capacity of the postural control system to counteract respiratory perturbations. Our results, no significant changes observed in tradition balance measures after 12-week training for a group of 87 year old, is supported by [Wolf et al 1997] 15-week Tai Chi training for a group of 77 year old, they did not seen changes either. But Tai Chi practice affects both the magnitude and temporal characteristics of respiration [8], future research is need to determine if Tai Chi practice also changes breathing depth. If so, the effects of altered breathing depth on posturo-respiratory synchronization and postural control should be investigated.
The observation that Tai Chi training reduced the synchronization index supports our primary hypothesis. The postural control system often loses its adaptive capacity as a result of normal biological aging[12–14]. Older adults, especially those with neuromuscular impairment, have a diminished capacity to maintain postural stability when responding to internal or external perturbations[12,14,15]. In our previous cross-sectional study of older adults, we observed that the posturo-respiratory synchronization index increased as a function of age, indicating age- related degradation within the control system that normally adjusts one’s postural movements to the effects of respiration on the body. Results of the current study suggest that Tai Chi training improves the capacity of the postural control system to counteract respiratory perturbations and thus, may reverse the effects of aging on this multisystem interaction.
The reduction in posturo-respiratory synchronization following Tai Chi training may have stemmed from alterations in respiratory patterns. This is unlikely, however, as neither intervention significantly influenced the mean rate of respiration. Observed reductions in the synchronization index thus more likely arose from altered functioning of the postural control system. The inherit features of Tai Chi training are particularly well-suited to enhance neuromuscular function [27]. Tai Chi stresses continuous ankle joint movement to effectively move the person’s center of gravity towards its limit of stability. It also emphasizes rotational trunk movements during upright posture and controlled diaphragmatic breathing. In the present study, the observed effects of Tai Chi training on posturo-respiratory synchronization may have resulted from active and/or passive mechanisms. Tai Chi may have trained the postural control system to actively produce counter-movements about the trunk and lower-extremity joints that more effectively canceled the impact of respiratory perturbations on postural sway. Alternatively, or in addition, Tai Chi may have increased the passive stiffness of the system, thereby dampening respiratory perturbations. Future research should, therefore, further examine the effects of Tai Chion both posturo-respiratory synchronization and lower-extremity muscular activation and stiffness during standing.
Although Tai Chi altered the interaction between respiration and postural control, it did not modify traditional measures of postural sway speed or magnitude. Several studies have reported significant reductions in similar standing postural control metrics following Tai Chi interventions[3,11,19,22,25], yet others have reported no changes or increases in these metrics following interventions [17,24,29,30]. Furthermore, for two nonlinear oscillations with weak coupling, such as the COP and respiratory systems studied here, amplitudes are not normally correlated yet their phases maybe synchronized. In other words, phase synchronization is more sensitive to weak coupling, which is a well-known phenomenon in physics and especially in nonlinear chaotic oscillators[7, 18]. Therefore, it might be expected that the effect of Tai Chi training on postural control was first pronounced in the phase relationship between postural sway and the respiration before the magnitude of postural sway and its speed were not modified the intervention.
Our study has several limitations. As considerably more women completed the study than men, caution should be exercised when generalizing results across gender. Furthermore, the control intervention was matched for time and attention, but not physical activity. It is therefore possible that the observed effect on coupling was a general effect of exercise and not a specific effect of Tai Chi. Future research should also study the effect of Tai Chi on the structure and function of passive and active lower extremity tissues with their potential contribution to postural control. Future studies should also explore the essential factors underlying the change, be it peripheral, central nervous systems, or the interactions between the two, of the respiratory-postural synchronization,
In summary, we have observed that a 12 week Tai Chi intervention reduced coupling between respiratory and postural sway in older adults. Using posturo-respiratory synchronization, novel application of the synchronization index, we observed a multisystem interaction between respiration and postural sway dynamics. Methodologically, we have observed that posturo-respiratory synchronization is a sensitive measure for evaluate the effects of respiration as perturbation on postural control.
Tai Chi training did not affect average sway speed& magnitude or respiratory rate
Yet tai Chi training reduced the impact of respiration on postural sway
The effects of Tai Chi on postural control could be optimized system interaction
Acknowledgments
This work was conducted with support of a T32 pre-doctoral fellowship (T32 AG-023480), a KL2 Medical Research Investigator Training (MeRIT) award (1KL2RR025757-04) from Harvard Catalyst, and grants from the National Institute of Health (R37-AG025037, K99-HL102241, R00-HL102241).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gandevia SC, Butler JE, Hodges PW, Taylor JL. Balancing acts: respiratory sensations, motor control and human posture. Clin Exp Pharmacol Physiol. 2002;29:118–121. doi: 10.1046/j.1440-1681.2002.03611.x. [DOI] [PubMed] [Google Scholar]
- 2.Gurfinkel VS, Kots YM, Paltsev EI, Feldman AG. The compensation of respiratory disturbances of erect posture of man as an example of the organization of interarticular interaction. In: Gelfand IM, Gurfinkel VS, Formin SV, Tsetlin ML, editors. Models of the structural functional organization of certain biological systems. Cambridge: MIT Press; 1971. [Google Scholar]
- 3.Hain TC, Fuller L, Weil L, Kotsias J. Effects of T'ai Chi on balance. Archives of Otolaryngology–Head & Neck Surgery. 1999;125(11):1191–1195. doi: 10.1001/archotol.125.11.1191. [DOI] [PubMed] [Google Scholar]
- 4.Hodges PW, Gurfinkel VS, Brumagne S, Smith TC, Cordo PC. Coexistence of stability and mobility in postural control: evidence from postural compensation for respiration. Exp Brain Res. 2002;144:293–302. doi: 10.1007/s00221-002-1040-x. [DOI] [PubMed] [Google Scholar]
- 5.Hunter IW, Kearney RE. Respiratory components of human postural sway. Neurosci Lett. 1981;25:155–159. doi: 10.1016/0304-3940(81)90324-4. [DOI] [PubMed] [Google Scholar]
- 6.Kavounoudias A, Roll R, Roll JP. Foot sole and ankle muscle inputs contribute jointly to human erect posture regulation. J Physiol. 2001;532:869–878. doi: 10.1111/j.1469-7793.2001.0869e.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurths J. Synchronization: A universal concept in nonlinear sciences. Vol. 12. Cambridge University Press; 2003. [Google Scholar]
- 8.Li F. Transforming traditional Tai Ji Quan techniques into integrative movement therapy—Tai Ji Quan: Moving for better balance. J Sport Health Sci. 2014;3(1):9–15. doi: 10.1016/j.jshs.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Glaver J, Maddalozzo G, Batya SS. Tai chi and postural stability in patients with parkinson’s disease. New Eng J Med. 2012;366:511–519. doi: 10.1056/NEJMoa1107911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li L, Manor BD. Long term tai chi exercise improves physical performance among people with peripheral neuropathy. Amer J of Chinese Med. 2010;38:449–459. doi: 10.1142/S0192415X1000797X. [DOI] [PubMed] [Google Scholar]
- 11.Lin YC, Wong AM, Chou SW, Tang FT, Wong PY. The effects of Tai Chi Chuan on postural stability in the elderly: preliminary report. Chang Gung medical journal. 2000;23(4):197–204. [PubMed] [Google Scholar]
- 12.Lipsitz LA. Physiological complexity, aging, and the path to frailty. Science's SAGE KE. 2004;16 doi: 10.1126/sageke.2004.16.pe16. [DOI] [PubMed] [Google Scholar]
- 13.Maki BE, Mcllroy WE. Postural control in the older adult. Clin Geriatr Med. 1996;12:635–658. [PubMed] [Google Scholar]
- 14.Manor B, Costa MD, Hu K, Newton E, Starobinets O, Kang HG, Peng CK, Novak V, Lipsitz LA. Physiological complexity and system adaptability: evidence from postural control dynamics of older adults. J Appl Physiol. 2010;109:1786–1791. doi: 10.1152/japplphysiol.00390.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manor BD, Hu K, Peng CK, Lipsitz LA, Novak V. Posturo-respiratory synchronization: Effects of aging and stroke. Gait & Posture. 2012;36:254–259. doi: 10.1016/j.gaitpost.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGibbon CA, Krebs DE, Wolf SL, Wayne PM, Scarborough DM, Parker SW. Tai Chi and vestibular rehabilitation effects on gaze and whole-body stability. J Vestib Res. 2004;14:467–478. [PubMed] [Google Scholar]
- 17.Nashner LM. Computerized dynamic posturography. Handbook of balance function testing. 1993;307 [Google Scholar]
- 18.Pikovsky A, Rosenblum M, Kurths J. Phase synchronization in regular and chaotic systems. International Journal of Bifurcation and Chaos. 2000;10:2291–2305. [Google Scholar]
- 19.Richerson S, Rosendale K. Does Tai Chi improve plantar sensory ability? A pilot study. Diabetes technology & therapeutics. 2007;9(3):276–286. doi: 10.1089/dia.2006.0033. [DOI] [PubMed] [Google Scholar]
- 20.Sakellari V, Bronstein AM, Corna S, Hammon CA, Jones S, Wolsley CJ. The effects of hyperventilation on postural control mechanisms. Brain. 1997;120:1659–1673. doi: 10.1093/brain/120.9.1659. [DOI] [PubMed] [Google Scholar]
- 21.Schmid M, Conforto S, Bibbo D, D’Alessio T. Respiration and postural sway: detection of phase synchronizations and interactions. Hum Mov Sci. 2004;23:105–119. doi: 10.1016/j.humov.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 22.Shih J. Basic Beijing twenty-four forms of T'ai Chi exercise and average velocity of sway. Perceptual and motor skills. 1997;84(1):287–290. doi: 10.2466/pms.1997.84.1.287. [DOI] [PubMed] [Google Scholar]
- 23.Smith M, Coppieters MW, Hodges PW. Effect of experimentally induced low back pain on postural sway with breathing. Exp Brain Res. 2005;166:109–117. doi: 10.1007/s00221-005-2352-4. [DOI] [PubMed] [Google Scholar]
- 24.Taggart HM. Effects of Tai Chi exercise on balance, functional mobility, and fear of falling among older women. Applied Nursing Research. 2002;15(4):235–242. doi: 10.1053/apnr.2002.35975. [DOI] [PubMed] [Google Scholar]
- 25.Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: the Central Sydney tai chi trial. J of the Americ Geriatr Soc. 2007;55(8):1185–1191. doi: 10.1111/j.1532-5415.2007.01244.x. [DOI] [PubMed] [Google Scholar]
- 26.Wolf S, Barnhart H, Ellison G, Coogler C. The effect of Tai Chi Quan and computerized balance training on postural stability in older subjects. Physical therapy. 1997;77(4):371–381. doi: 10.1093/ptj/77.4.371. [DOI] [PubMed] [Google Scholar]
- 27.Wolf S, Barnhart H, Kutner N, McNeely E, Coogler C, Xu T. Selected as the best paper in the 1990’s: Reducing frailty and falls in older persons: An investigation of tai chi and computerized balance training. J of the Americ Geriatr Soc. 1996;51:1794–1803. doi: 10.1046/j.1532-5415.2003.51566.x. [DOI] [PubMed] [Google Scholar]
- 28.Wolf S, Coogler C, Xu T. Exploring the basis for tai chi chuan as a therapeutic exercise approach. Arch Phys Med Rehabil. 1997;78:886–892. doi: 10.1016/s0003-9993(97)90206-9. [DOI] [PubMed] [Google Scholar]
- 29.Wolfson L, Whipple R, Derby C, Judge J, King M, Amerman P, Smyers D. Balance and strength training in older adults: intervention gains and Tai Chi maintenance. J of the Americ Geriatr Soc. 1996;44(5):498–506. doi: 10.1111/j.1532-5415.1996.tb01433.x. [DOI] [PubMed] [Google Scholar]
- 30.Woo J, Hong A, Lau E, Lynn H. A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age and ageing. 2007;36(3):262–268. doi: 10.1093/ageing/afm005. [DOI] [PubMed] [Google Scholar]
- 31.Yeh GY, McCarthy EP, Wayne PM, et al. Tai chi exercise in patients with chronic heart failure: a randomized clinical trial. Arch Intern Med. 2011;171:750–757. doi: 10.1001/archinternmed.2011.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yeh GY, Wood MJ, Lorell BH, et al. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. 2004;117:541–548. doi: 10.1016/j.amjmed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 33.Yeh GY, Wood MJ, Wayne PM, et al. Tai chi in patients with heart failure with preserved ejection fraction. Congest Heart Fail. 2013;19:77–84. doi: 10.1111/chf.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]