Abstract
Research has demonstrated the positive association between alcohol craving and alcohol use and has identified craving as a central component of alcohol use disorders (AUD). Despite potential clinical implications, few studies have examined the relationship between craving and alcohol use in individuals with AUD and common psychiatric comorbidities or explored possible moderators of the craving-alcohol use relationship. The current study used daily monitoring data to: 1) replicate previous findings detecting a positive relationship between craving and alcohol use in individuals with AUD and co-occurring posttraumatic stress disorder (PTSD) and 2) extend these findings by examining the influence of initial change motivation on the craving-use relationship and within-day associations among craving, efforts to control craving, and alcohol consumption. Participants were 84 individuals with alcohol dependence and PTSD enrolled in an intervention study. Generalized estimating equations using pre-treatment baseline daily data revealed significant main effects for craving, craving control, and motivation to change alcohol use. Daily craving was positively related to alcohol use. Greater change motivation and craving control (i.e., efforts to resist craving, avoidance of thoughts and feelings related to craving) were negatively related to alcohol use. A significant interaction was detected between baseline change motivation and daily craving indicating that the association between craving and alcohol use was significantly stronger for those with low baseline change motivation. A significant interaction was also detected between craving control and daily craving, suggesting participants were more likely to consume alcohol when experiencing high levels of craving if they reported low levels of craving control. Findings bolster the idea that efforts to prevent or ameliorate craving are critical to treatment success for individuals with AUD and PTSD who are seeking to reduce or quit drinking.
Keywords: alcohol, PTSD, craving, motivation to change
1. Introduction
Alcohol use disorders (AUDs) result in substantial personal and public harm, including losses in workplace productivity, inflated health care costs, and untold damages to personal relationships and overall functioning (Bouchery, Harwood, Sacks, Simon, & Brewer, 2011; Levola & Pitkanen, 2012). Moreover, alcohol-involved conditions and incidents are among the most prominent causes of mortality in the United States, accounting for between 2% and 4.9% of deaths annually (World Health Organization, 2011). AUDs commonly co-occur with Posttraumatic Stress Disorder (PTSD; Blanco et al., 2013) and the combination is associated with worse occupational functioning, poorer physical health, increased health care utilization, poorer treatment response, higher rates of treatment drop-out and earlier relapse (Blanco et al., 2013; Brady et al., 1994; Drapkin et al., 2011; Ouimette, Moose, & Finney, 2000; Read, Brown & Kahler, 2004).
Effective treatments for AUDs, with and without comorbidities such as PTSD, have expanded in recent years (Jung & Namkoong, 2006; Torchella, Nosen, Rostam, & Allen, 2012), yet these disorders remain largely chronic and relapsing, often causing various harms over the course of a lifetime (Heilig, Goldman, Berrettini, & O’Brien, 2011). As such, deepening our understanding of factors that may maintain problem drinking and AUD in the context of co-occurring PTSD is an important goal with both clinical and public health implications.
1.1. Alcohol Craving as a Fundamental Component of Alcohol Dependence
The construct of alcohol craving is frequently portrayed as a fundamental aspect of the former DSM-IV construct of alcohol dependence (American Psychiatric Assocation, 2000; Anton, 2000; Meyer, 2000) in that it appears to be both characteristic of alcohol dependence and to have a critical role in maintaining dependence. One study using a large community-based sample of drinkers found that craving loads onto the same latent construct as other previously identified aspects of alcohol dependence, and that adding a craving-specific symptom adds significantly to the discriminant validity of the alcohol dependence syndrome (Keyes, Krueger, Grant, & Hasin, 2011). Similarly, in the context of a study on the genetic influences of craving, Agrawal and her colleagues (2013) found that craving was typically an indicator of greater dependence severity. Other researchers have found that craving distinguishes problem drinkers from non-problem drinkers (Grusser, Morsen, & Flor, 2006; Love, James, & Willner, 1998). Craving assessed prior to an alcohol treatment episode has also been associated with treatment outcome (Connolly et al., 2013; Kranzler, Mulgrew, Modesto-Lowe, & Burleson, 1999), including findings suggesting that higher pre-treatment alcohol craving predicts earlier relapse (Flannery, Volpicelli, & Pettinati, 1999). Given these findings, it is unsurprising that craving has been added as a criterion for the diagnosis of AUD in DSM-5 (American Psychiatric Association, 2013) and may play a role in discriminating between milder and more severe forms of the disorder.
Craving has also been found to be a common clinical feature among individuals with comorbid AUD and PTSD. For instance, a number of laboratory cue exposure studies have found that both alcohol and trauma cues activate craving in this group (Coffey, et al., 2002, 2010). The linkage of craving to actual alcohol consumption, has, however not been adequately examined. Interestingly, a cue exposure study by Litt and colleagues (2000) failed to find a robust relationship between in lab craving responses to alcohol cues and alcohol use among people with an AUD only. However, Litt and colleagues did find that craving assessed via a daily monitoring protocol was strongly positively associated with post-treatment drinking and heavy drinking days (see also Kavanagh, May, Andrade, 2009).
1.2. Examining the Day-To Day Relationship Between Craving and Consumption
More recent studies involving frequent data collection methodologies (e.g., daily diary, ecological momentary analysis, etc.) have further contributed to our understanding of the relationship between alcohol craving and consumption. Using 26-days of daily dairy assessment data to examine the relationship between craving and recovery outcomes in alcohol dependent patients entering residential treatment, Oslin and colleagues (2009) identified three latent class trajectories of high, medium, and low craving. Those in the high craving class relapsed more quickly and endorsed more alcohol-related problems, more severe depression, and worse physical health functioning than those in the low craving class and worse physical health functioning and mental health functioning than the medium craving class. Additional research on craving and the use of substances other than alcohol that involved frequent monitoring protocols has also found that craving strongly predicts use (Buckner, Crosby, Silgado, Wonderlich, & Schmidt, 2012; Chandra, Scharf, & Schiffman, 2011; Preston et al., 2009) and is associated with relapse (Holt, Litt, & Cooney, 2012; Marhe, Waters, van de Wetering, & Franken, 2013).
1.3. Identifying Factors Impacting the Relationship Between Craving and Consumption
1.3.1. Motivation for change
In order to move beyond bivariate relationship between craving and consumption, it will be essential to identify variables that influence this relationship. A potentially important variable to consider in the context of the craving-consumption relationship is motivation to change alcohol use. The degree of motivation to change alcohol use is associated with AUD treatment outcomes such that those who are more motivated at the outset of treatment tend to have better treatment outcomes than those who are not (Adamson, Sellman, & Frampton, 2009; Evern, Cetin, Durkaya, & Dalbudak, 2010; Ray, Hutchison, & Bryan, 2006). Furthermore, Tiffany (1990) suggested that the quality of craving may change depending on the explicit goals of the individual. That is, those individuals who are highly motivated to change their drinking behavior may well experience more craving since alcohol is essentially off-limits to them. However, it is unknown whether motivation to change alcohol use plays a role in tempering the impact of craving on drinking, such that those with stronger motivation to reduce or quit drinking at the beginning of a treatment episode are less apt to drink when they experience craving.
1.3.2. Responses to craving: avoidance and thought suppression
How an individual responds to craving may also influence the craving-consumption relationship. One possible response to craving is to attempt to avoid thoughts and feelings associated with it (i.e., craving avoidance). Such experiential avoidance has been conceptualized as attempts to either avoid or otherwise control one’s internal experiences, including those of cravings (Hayes, 1994; Hayes, Strosahl, & Wilson, 1999). Several investigators have endeavored to evaluate these relationships with heavy drinking or AUD only samples, though typically in laboratory contexts where actual drinking is not assessed. Palfai and his colleagues (1997) showed that heavy drinkers who were instructed to suppress their urges to drink when exposed to alcohol cues more quickly endorsed alcohol-related expectancies than those who did not receive such instruction, suggesting that suppression of alcohol urges may prime access to alcohol-related memories or information. Similarly, Klien (2007) found that abstinent alcohol dependent adults who suppressed alcohol-related thoughts demonstrated greater interference on the alcohol Stroop task compared to those who freely expressed alcohol-related thoughts prior to completing the Stroop task. More recently, Garland and colleagues (2012) found that higher thought suppression was associated with lower confidence that alcohol urges could be resisted among alcohol dependent adults undergoing an alcohol cue exposure protocol (see also Muraven, Collins, & Nienhaus, 2002). However, using aggregate data collected via daily monitoring, Kavanagh et al. (2009) found that when alcohol dependent individuals attempted to not think about drinking they reported longer latency to drinking onset and drank less. Thus, although the literature is somewhat mixed and the direction of effect is not clear, attempts to suppress or avoid craving may moderate the relationship between craving and use.
1.3.3. Responses to craving: resistance
A related, but somewhat different, construct of interest is craving resistance. Here, rather than coping with craving through avoidance or thought suppression, the emphasis is on using more instrumental means to resist the urge to drink. For example, in an effort to not drink in the face of acute cravings or urges someone could engage in intra-personal strategies such as reminding oneself that craving is a temporary state or observable strategies such as attending a self-help meeting. There is a commonsense appeal to the idea that resistance of alcohol craving might be associated with less drinking and research supporting this theory has begun to emerge. In a study of alcohol and nicotine dependent individuals in outpatient treatment, Cooney and colleagues (2007) assessed self-rated ability to resist drinking, which they termed abstinence self-efficacy, along with drinking and urges to drink through a 14-day ecological momentary analysis (EMA) protocol. In this momentary assessment context, abstinence self-efficacy was associated with lower odds of returning to alcohol use. However, the relationship between craving and abstinence self-efficacy was not assessed in this study, and we therefore do not know whether this form of craving resistance impacts the relationship between craving and drinking in alcohol dependent individuals’ day-to-day lives.
1.4. The Current Study
The current study utilized daily interactive voice response (IVR) assessments from the pre-treatment baseline period of a larger experimental intervention study of mechanisms of behavior change in individuals with posttraumatic stress disorder (PTSD) and AUD. This work builds on earlier work with these data that demonstrated that PTSD symptomatology was associated with both same day, and to a lesser extent, next day drinking (Simpson, et al., 2014). The goals of the present investigation were twofold. First, we sought to replicate findings from previous frequent monitoring studies examining the relationship between craving and alcohol use in individuals with AUD and co-occurring PTSD. Based on past results in AUD only samples (e.g., Litt et al., 2000), we hypothesized that alcohol craving would be positively associated with alcohol use within each day. Second, in an effort to extend these findings we sought to identify variables that influence the relationship between craving and alcohol use. Consistent with Tiffany’s (1990) characterization of craving being especially salient among individuals actively attempting to change their drinking, we expected that the relationship between craving and use would be moderated by degree of change motivation at baseline. Specifically, we hypothesized that, at lower levels of baseline change motivation, craving would be positively related to use, while at high levels of change motivation, craving would be negatively related to use. We also evaluated whether efforts to avoid thoughts and feelings related to craving and/or efforts to resist urges to drink were related to alcohol use, hypothesizing that greater efforts to avoid and/or resist cravings would be associated with less alcohol use.
2. Method
2.1. Participants and Recruitment
Participants were adult civilians and veterans who were recruited for a larger study examining treatments for AUD and PTSD registered at ClinicalTrials.gov (protocol #: masked for review). Participants were recruited through community newspaper advertisements, flyers, and announcements made at a recurring orientation appointment for veterans pursuing addiction treatment at a major Veterans Affairs medical center. Eligible participants indicated (1) a desire to quit or decrease alcohol use, (2) were at least 18 years old, (3) met criteria for alcohol dependence as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 2000) and reported having used alcohol in the last 2 weeks, (4) met DSM-IV (American Psychiatric Association, 2000) criteria for Posttraumatic Stress Disorder (PTSD), (5) had the capacity to provide informed consent, and (6) had access to a telephone. Eligible participants also (7) denied opioid use or chronic treatment with opioid-containing medications during the past month, (8) were not currently receiving pharmacological treatment for AUD (e.g., disulfiram, naltrexone, etc.), (9) denied acute suicidality/homicidality with intent/plan, and (10) denied current psychosis.
A total of 92 participants met eligibility criteria and were enrolled in the larger study. However, three participants were excluded from the current study because they failed to complete any monitoring days and three additional participants were not included because they completed less than 50% of possible daily IVR assessments during the baseline period. An additional two participants were dropped from main analyses for failing to provide their marital status. Participants who were excluded from analyses were more likely to be employed fulltime, χ2 = 3.77, p = .05. There were no other differences between those included versus excluded in demographic variables or in baseline drinking (i.e., number of drinking days and total number of standard drinks consumed; p’s > .05). The remaining 84 participants ranged in age from 21 to 63, 48.8% were female, and 26.2% were veterans. In addition to meeting criteria for an AUD, 24.4% of participants reported cannabis use during the six weeks prior to baseline, 15.2% reported cocaine use, 5.1% reported opiate use, 3.8% reported sedative use, 1.3% reported amphetamine use, 1.3% reported sedative use, and 1.3% reported other drug use. Participants denied use of hypnotics, hallucinogens, steroids, and inhalants. Additional demographics can be found in Table 1.
Table 1.
Participant Characteristics
| Characteristics | Mean (SD) or N (%) |
|---|---|
| Female | 41 (48.8) |
| Age (M ± SD) | 44.7 (11.1) |
| Ethnicity/Race | |
| Caucasian | 34 (40.5) |
| African American | 36 (42.9) |
| Hispanic/Latino | 4 (4.8) |
| Native American | 4 (4.8) |
| Asian American | 1 (1.2) |
| Other or missing | 5 (6.0) |
| Marital Status | |
| Married or partnered | 11 (13.1) |
| Divorced or separated | 31 (36.9) |
| Never married | 35 (41.7) |
| Widowed or other | 7 (8.3) |
| Housing Stats | |
| Living in own home | 51 (60.7) |
| Homeless | 20 (23.8) |
| Other | 13 (15.5) |
| Educational Attainment | |
| Did not graduate HS | 19 (22.6) |
| Graduated HS | 12 (14.3) |
| At least some college | 53 (63.1) |
| Employment Status | |
| Employed at least part-time | 11 (13.1) |
| Unemployed | 27 (32.4) |
| Student | 9 (10.7) |
| Disabled/Retired/Other | 37 (43.8) |
| Treatment History | |
| Inpatient substance abuse | 41 (48.8) |
| Inpatient mental health | 23 (27.4) |
| Medication management | 50 (59.5) |
| Outpatient therapy | 57 (67.8) |
2.2. Procedure
2.2.1. Telephone screening
Individuals interested in the study participated in a telephone or in-person brief screening to ascertain basic eligibility criteria. Those who appeared eligible and remained interested in the study were scheduled for an in-person baseline assessment.
2.2.2. Baseline assessment
Participants provided written informed consent, which was considered valid if their breath alcohol level was .00. They then completed several screening interviews and self-report measures, and those who met study eligibility criteria were familiarized with the daily IVR procedure and the accompanying pager system. They were told that IVR calls needed to be placed by noon each day. IVR monitoring commenced the day after the baseline assessment. Participants were paid $30 for completing these baseline procedures. All study procedures were approved by the [masked for review] Human Subjects Internal Review Board.
2.2.3. Daily monitoring assessment
Ongoing IVR compliance was automatically tracked by the IVR system created and maintained by Database Systems Corp. When participants failed to call in, they were contacted within two working days by research staff to collect the data verbally and to trouble-shoot any difficulties with the IVR system. Participants were compensated $1 for every day of completed daily monitoring, with an additional $10 for completing 7 consecutive days of monitoring or an additional $7 if they only missed one day of daily monitoring during a given week. Participants were recruited for involvement in a larger study, which involved engaging in a baseline period of IVR monitoring prior to presenting to the laboratory again for a brief intervention and other procedures. The IVR assessments completed during this baseline period are the focus of the current study. Although this baseline period was designed to be 7 days, scheduling issues often resulted in this initial monitoring period being either shorter or longer. As such, participants spent a range of 6 to 20 days in this initial phase of monitoring and all available data were used.
2.3. Measures
2.3.1. Mental health diagnoses
Sections pertaining to substance use and psychotic symptoms of the Structured Interview for DSM-IV Axis I Disorders (SCID-1; First, Spitzer, Gibbon, & Williams, 1995) were used to assess for current substance use-related and psychotic disorders. The SCID-1 is a widely used interview that has sound psychometric properties (First et al., 1995). Additionally, we used the PTSD Symptom Scale-Interview Version (PSS-I; Foa, Riggs, Dancu, & Rothbaum, 1993) to assess current PTSD status using a one-month timeframe. The PSS-I is a 17-item semi-structured interview with good internal consistency, item-total correlations, and concurrent and convergent validity (Foa et al., 1993).
2.3.2. Change motivation
The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES; Miller & Tonigan, 1996) is a 19-item self-report instrument that was used to assess participants’ motivation for change. Participants endorsed items on 1 (No! Strongly disagree) to 5 (Yes! Strongly agree) scales. Sample items include, “I really want to make changes in my drinking,” and “My drinking is causing a lot of harm.” The SOCRATES has demonstrated acceptable reliability, as well as good convergent and discriminant validity (Carey, Maisto, Carey, & Purnine, 2001; Miller & Tonigan, 1996). The SOCRATES yields three sub-scales: Ambivalence, Recognition, and Taking Steps. Because the Ambivalence sub-scale addresses a construct that is not clearly aligned with strength of motivation to change, only the items from the Recognition (α = .88) and Taking Steps (α = .88) scales were summed for use in the analysis. Higher scores indicate greater motivation to change.
2.4. Daily IVR Assessment
2.4.1. Alcohol use
Participants indicated the number of standard drinks of beer, wine, and liquor (defined as 12 oz. of beer, 5 oz. of wine, and 1–1.5 oz. of liquor) they consumed the previous day, each queried separately, and added together to get the total number of drinks per day.
2.4.2. Alcohol craving
Three items were used to reflect alcohol craving: “How much did you think about drinking yesterday?” “How strong were your cravings yesterday?” and “What was your average level of craving for alcohol yesterday?” These items were rated on 0 to 8 scales, where 0 indicated no thoughts about drinking/craving and 8 indicated very frequent thoughts about drinking/strong craving. These items were summed to form the primary alcohol craving variable.
2.4.3. Craving avoidance and craving resistance
One item was used to assess craving avoidance (“How much did you try to avoid thoughts and feelings of craving yesterday?”) and one item was used to assess craving resistance (“How much did you resist or try not to give in to your craving yesterday?”) Both items were rated on 0 (no avoidance or resistance) to 8 (the most avoidance or resistance ever) scales; these questions were only asked if any of the craving items were endorsed with a 1 or higher. Although we initially conceptualized these items as tapping separate constructs, the empirical results did not support this idea (see details below in the Descriptive Statistics section). As a result, the two items were combined to form a single composite variable referred to as craving control.
2.5. Analysis
To examine the hypothesized associations between study variables and daily reports of alcohol use, we utilized generalized estimating equation (GEE; Hardin & Hilbe, 2003) models in Stata 13 (Stata Corp, 2013). The outcome variable consisted of participants’ daily reports of the number of standard drinks consumed. Because this variable represents a count that was positively skewed, negative binomial distributions with log-link functions were specified, and we obtained robust standard errors. Our initial model examined within-person associations between alcohol craving and craving control (i.e., craving avoidance/craving resistance composite variable) on total number of drinks consumed, as well as the main effects of gender, age, marital status and motivation for change. This main effects model also included a “weekend day” indicator to account for the fact that more drinking often occurs on weekends compared to weekdays. Craving and craving control variables were centered at the person mean prior to model entry and formation of interaction terms. Centering these variables at the person-mean allows for an examination of the purely within-person relationship between changes in craving and changes in craving control independent of between-persons associations (Enders & Tofighi, 2007; Raudenbush & Bryck, 2002). Baseline motivation to change, a between-persons variable, was centered at the grand mean prior to model entry and formation of interaction terms (Raudenbush & Bryck, 2002). To examine hypotheses regarding the moderating role of craving control and motivation to change, a second model was examined, which included the above-listed variables as well as all possible two-way interaction terms between craving, craving control, and change motivation1.
Participant IVR response rates were excellent during this baseline period, with only 4.7% of the possible assessment days missing. In addition, among the completed IVR assessments, less than 1% of the items assessed were skipped or incomplete. Given the low rate of missingness and the inclusion of relevant variables in the model, the quasi-maximum likelihood procedures used in the following analysis likely produced unbiased estimates of hypothesized relationships (Allison, 2009) and GEE models are likely robust to missingness of this nature.
3. Results
3.1. Descriptive Statistics
Participants in the analyzed sample (N = 84) spent an average of 7.3 (SD = 2.6, range = 4 to 16) days completing daily IVR assessments before receiving their assigned treatment intervention. A total of 612 person-days were analyzed. Participants reported drinking an average of 4.1 days (SD = 3.1, range = 0 to 12). Participants reported drinking an average of 4.0 (SD = 6.6) drinks per day during this period. Men (M = 5.6, SD = 8.4) reported drinking more per day than women (M = 2.6, SD = 3.7), t(611)=−5.72, p < .001. Participants who were not currently married (e.g., never married, divorced, separated, widowed; M = 4.4, SD = 6.9) reported consuming significantly more drinks per day compared with those who reported being married (M = 1.6, SD = 3.3), t(611) = 3.40, p < .001.
Although we initially hypothesized that craving resistance and avoidance would reflect two distinct constructs, examination of bivariate correlations suggested that these were highly, positively associated (r = .74, p < .001). As such, these items were combined in order to reflect an overall “craving control” variable that reflects both efforts to avoid and resist cravings for inclusion in the full analysis. See Table 2 for descriptive statistics and sample correlations.
Table 2.
Descriptive statistics and bivariate correlations of study variables
| Variables | Range | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | 0 – 1 | N=41/43 | -- | ||||||
| 2. Age | 21 – 63 | 44.65 | 11.14 | 0.09* | |||||
| 3. Marital status | 0 – 1 | N=73/11 | -- | −0.04 | −0.15*** | ||||
| 4. Drinks per day | 0 – 54 | 4.02 | 6.63 | 0.23*** | −0.02 | −0.14*** | |||
| 5. Alcohol craving | 0 – 24 | 13.61 | 7.07 | 0.03 | 0.02 | −0.003 | 0.36*** | ||
| 6. Craving control | 0 – 16 | 7.68 | 5.29 | 0.11** | 0.10* | 0.04 | −0.15*** | 0.27*** | |
| 7. Change motivation | 0 – 75 | 56.45 | 14.89 | 0.06 | 0.11** | 0.01 | −0.14*** | −0.08 | 0.12** |
Note. Gender was coded 0 = female, 1 = male. Marital status was coded 0 = not married, 1 = married.
p < .05.
p < .01.
p < .001.
3.2. Main Effects Model
In our initial model (Table 3), male gender was positively associated with daily drinking (incidence rate ratio [IRR] = 2.42, 95% confidence interval [CI]: 1.51 – 3.85; p <.001). Being married was significantly associated with decreased alcohol use (IRR = 0.40, 95% CI: 0.22 – 0.73; p = .003). In addition, more alcohol was consumed on weekend days than on weekdays (IRR = 1.28, 95% CI: 1.09–1.49; p = .002). Further, daily craving was positively related to alcohol use (IRR = 1.13, 95% CI: 1.10–1.16; p < .001). This indicates that a 1-unit increase in craving above the person’s average was associated with a 13% increase in drinking that day. On average, among men, this translates into .73 drinks per 1-unit increase in craving and among women this translates into .34 drinks per 1-unit increase in craving. Baseline motivation to change was negatively related to alcohol use (IRR = 0.97, 95% CI: 0.95 – 0.99; p = .001). This suggested that a 1-unit increase in baseline motivation was associated with a 3% decrease in drinking. On average, among men, this translates into a decrease of .17 drinks per 1-unit increase in motivation and among women this translates into a decrease of .08 per 1- unit increase in motivation. Finally, daily efforts to control craving were negatively related to alcohol use (IRR = 0.93, 95% CI: 0.90 – 0.96; p < .001). This suggested that a 1-unit increase in control efforts above the person’s average was associated with a 7% decrease in drinking that day. On average, among men, this translates into a decrease in .39 drinks per 1-unit increase in craving control and among women this translates into a decrease of .18 drinks per 1-unit increase in craving control.
Table 3.
Main Effects GEE Model of Same-Day Standard Drinks Consumed on Alcohol Craving, Craving Control Efforts, and Change Motivation
| Variable | b | SE | p | IRR | 95% CI |
|---|---|---|---|---|---|
| Age | −.008 | .009 | .390 | 0.99 | 0.97, 1.01 |
| Male gender | .882 | .238 | < .001 | 2.42 | 1.51, 3.85 |
| Married | −.916 | .306 | .003 | 0.40 | 0.22, 0.73 |
| Weekend Day | .247 | .078 | .002 | 1.28 | 1.10, 1.49 |
| Alcohol craving | .122 | .012 | < .001 | 1.13 | 1.10, 1.16 |
| Craving control | −.078 | .017 | < .001 | 0.93 | 0.90, 0.96 |
| Change motivation | −.029 | .009 | .001 | 0.97 | 0.95, 0.99 |
Note. Wald χ2(7) = 149.11, p < .001. IRR = Incidence rate ratio.
Alcohol craving, craving control, and change motivation were standardized prior to entry.
3.3. Moderator Model
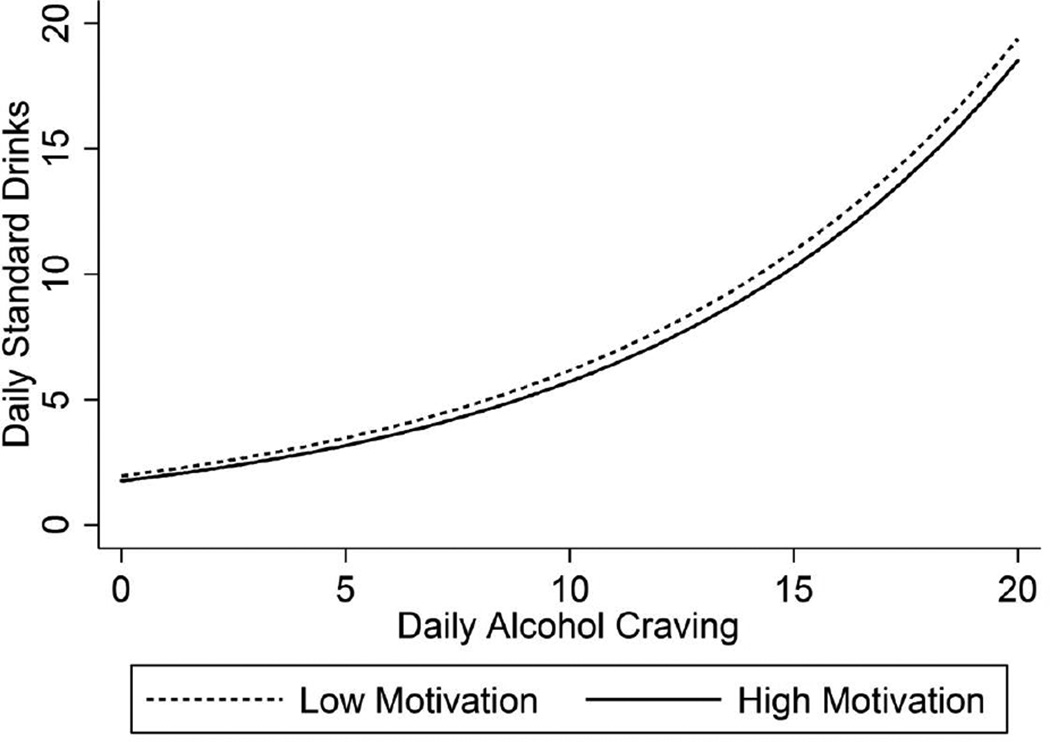
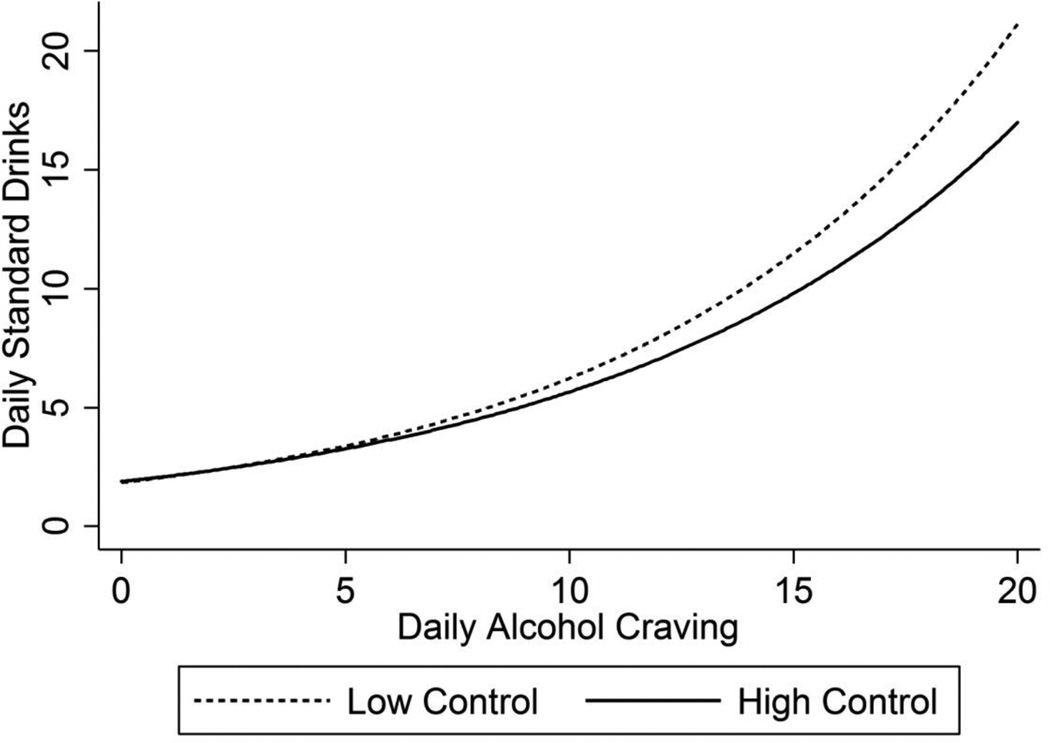
Results from our second model (Table 4) examining possible moderators of the relationship between craving and alcohol use paralleled our initial findings. Male gender, being single, and weekend days were associated with more drinking. Daily alcohol craving, craving control, and change motivation significantly predicted daily drinking. However, these main effects were superseded by significant two-way interaction effects between craving and change motivation (IRR = 1.00; 95% CI: 1.00–1.01; p < .001) and craving and craving control (IRR = .99, 95% CI: 0.99-0.99; p = .001). The significant interaction between baseline change motivation and daily craving suggests the association between craving and alcohol use was significantly stronger for those with low baseline change motivation (Figure 1). Further, the significant interaction between craving control and daily craving suggests participants were more likely to consume alcohol when experiencing high levels of craving if they reported low levels of craving control (Figure 2). The interaction between craving control and motivation to change was not significant.
Table 4.
Final GEE Model of Same-Day Standard Drinks Consumed on Alcohol Craving, Craving Control Efforts, and Change Motivation
| Variable | b | SE | p | IRR | 95% CI |
|---|---|---|---|---|---|
| Age | −.008 | .008 | .366 | 0.99 | 0.97, 1.01 |
| Male gender | .891 | .237 | < .001 | 2.44 | 1.53, 3.88 |
| Married | −.910 | .299 | .002 | 0.40 | 0.22, 0.73 |
| Weekend Day | .240 | .082 | .004 | 1.27 | 1.08, 1.49 |
| Alcohol craving | .116 | .012 | < .001 | 1.12 | 1.10, 1.15 |
| Craving control | −.070 | .017 | < .001 | 0.93 | 0.90, 0.97 |
| Change motivation | −.032 | .009 | < .000 | 0.97 | 0.95, 0.99 |
| Craving × craving control | −.006 | .002 | .001 | 0.99 | 0.99, 1.00 |
| Craving × motivation | .001 | <.001 | .008 | 1.00 | 1.00, 1.01 |
| Craving control × motivation | −.001 | <.001 | .176 | 0.999 | 0.99, 1.00 |
Note. Wald χ2(10) = 210.36, p < .001. IRR = Incidence rate ratio.
Alcohol craving, craving control, and change motivation were standardized prior to entry.
Figure 1.
Relationship between Alcohol Craving and Daily Standard Drinks by Levels of Change Motivation. Estimated values were plotted 1 standard deviation above and below the mean for change motivation.
Figure 2.
Relationship between Alcohol Craving and Daily Standard Drinks by Levels of Craving Control. Estimated values were plotted 1 standard deviation above and below the mean for craving control.
4. Discussion
The present investigation sought to replicate previous frequent monitoring study results detecting a positive association between craving and alcohol use in a sample with co-occurring PTSD/AUD and to extend these findings by exploring possible moderators of this relationship. Baseline motivation to change alcohol use was examined as a potential moderator of the relationship between daily craving and daily consumption and the relationship between daily craving control and daily consumption. Within-day associations among self-reported alcohol craving, efforts to control craving, and their potential interactions on daily drinking were also examined. Consistent with our hypotheses, we found that reports of alcohol craving were indeed associated with higher levels of alcohol use. In addition, both baseline change motivation and craving control interacted with craving to predict alcohol use. The interaction between change motivation and craving control was not significant. Each of these findings is discussed in turn.
Similar to previous investigations using frequent monitoring protocols in AUD only samples, our results demonstrate a relationship between the subjective experience of alcohol craving and alcohol use. Indeed, a 1-unit increase in craving above one’s average level of craving on a given day was associated with consuming an increase of .73 standard drinks among men and .34 among women that day. In other words, even a very small increase in craving above the individual’s average was associated with a notable increase in alcohol consumption. Extrapolating out to larger increases in craving, a relatively moderate increase of 7 points above one’s average on the IVR craving index (range is 0 to 24) on a given day would be associated with 5 more standard drinks for men and nearly 2.5 more standard drinks for women on that day. This result is consistent with a number of studies demonstrating global relationships between self-reported craving and a variety of deleterious alcohol-related outcomes (Kavanagh et al., 2009; Flannery et al., 1999; Grusser et al., 2006; Love et al., 1998). Our results also lend support to those reported by Litt and colleagues (2000) suggesting that craving frequently co-occurs with drinking at the situational level, and we extend their finding by demonstrating that modest increases in craving are associated with clinically meaningful increases in same-day alcohol consumption in a PTSD/AUD sample. Together, these studies affirm craving as an important predictor of drinking in the daily lives of those with an AUD as well as in those with PTSD/AUD, and suggest that efforts to prevent or ameliorate craving are likely critical to treatment success for individuals who are seeking to reduce or quit drinking.
In order to extend our understanding of the relationship between craving and consumption we examined baseline change motivation as it pertains to craving and to daily drinking. As hypothesized, we found a main effect of baseline change motivation such that greater motivation to change alcohol use was associated with less drinking. However, in our second model, this main effect was superseded by a significant interaction effect between craving and change motivation, indicating that change motivation appears to play at least a small role in tempering the impact of craving on drinking (see Figure 1). More specifically, those with stronger motivation to reduce or quit drinking at the beginning of treatment reported less consumption when they experienced craving. Previous studies have consistently detected a relationship between motivation to change and positive post-treatment outcomes in AUD only samples (e.g., Adamson et al., 2009; Evern et al., 2010; Ray et al., 2006). To our knowledge this is the first attempt to extend these findings by examining the relationship between craving and motivation to change as it relates to alcohol use. Although this finding will need to be confirmed through future research, our results appear to support current clinical recommendations regarding the importance of assessing and understanding a patient’s level of change motivation and delivering targeted motivational enhancement interventions to those with lower change motivation (Miller & Rollnick, 2013). This work could be further extended in the future by examining the role of both internal and external sources of motivation and the associated impact on the craving-use relationship.
In addition, we evaluated craving control efforts as they pertain to craving itself and to daily drinking. First, we found a main effect of craving control efforts such that greater control efforts were associated with less same day alcohol use. However, upon adding interaction terms to our second model, this main effect was superseded by a significant interaction between craving and craving control efforts, indicating that craving control serves to moderate the relationship between craving and daily drinking.
Germane to these findings, our single item assessments of avoidance of thoughts and feelings associated with craving and of efforts to resist craving were highly positively correlated, suggesting that they are likely not orthogonal constructs. Although some previous literature suggests that avoidance of thoughts about craving appears to be associated with greater accessibility of alcohol-related memories or imagery (Klien et al., 2007; Palfai, Monti, Colby, & Rohsenow, 1997), both our findings and those of Kavanaugh et al. (2009), suggest increased craving control efforts, including efforts to avoid thoughts and feelings pertaining to alcohol, are related to reduced drinking. It may be that while thought suppression leads to a cognitive rebound of the avoided material, there is not a corollary relationship between thought suppression and associated overt behavior. Future research is needed to determine whether specific types of avoidance and resistance control efforts are more or less related to successful reductions in use. Additionally, examining variables that may impact these cognitive processes (e.g., ambivalence, situational variables) may also be a fruitful line of research. For instance, in our study, married participants drank significantly less than single participants. It stands to reason that those who are unmarried have less access to immediate social support that could be used either as a behavioral avoidance strategy or to shore up flagging motivation. It is possible these individuals may benefit from additional tools when thinking about utilizing such control efforts (e.g., being more creative about who he/she can call to take his/her mind off of alcohol).
Regardless of the exact mechanism of action, our craving control results suggest that efforts to avoid or resist alcohol cravings may, in fact, be helpful to those with PTSD/AUD who are attempting to change their drinking. Despite the fact that there is no fail safe in that strong control efforts in the face of craving cannot guarantee abstinence, the finding that greater control efforts appear to help reduce, somewhat, the amount of drinking and may impact the relationship between craving and subsequent alcohol use is noteworthy, though the degree of clinical significance does appear limited (see Figure 2). Given that our study examined individuals with AUD and PTSD, a disorder characterized by avoidance, it is important to highlight the seemingly contradictory results detected in the present study. More specifically, studies examining individuals with PTSD suggest high levels of avoidance are associated with poorer psychological outcomes (e.g., Badour, Blonigen, Boden, Feldner, & Bonn-Miller, 2012). This suggests that the function of avoidance, and thus the subsequent treatment of avoidant behaviors, may differ in the context of each disorder. Nuanced conversations with patients diagnosed with PTSD/AUD focused on building understanding of when avoidance may be appropriate may be needed. For example, using avoidance as a control strategy may be appropriate for coping with distressing alcohol cravings in order to maintain abstinence, but it is likely not appropriate as a control effort to decrease distressing anxiety associated with situations most would consider safe.
Finally, the relationship between craving control efforts and change motivation was also explored and we did not detect a significant interaction. This somewhat surprising finding suggests that baseline motivation to change alcohol use did not influence the association between one’s use of craving control efforts and their alcohol consumption on that day. Motivation to change is often conceptualized as a dynamic state (Miller & Rollnick, 2013; Prohcaska & DiClemente, 1982). Thus, it may be that the relationship between craving control efforts and change motivation would best be examined when both variables are measured at the event-level via a frequent monitoring protocol.
4.1. Strengths and Limitations
This study has a number of notable strengths such as the use of frequent daily assessments that allow for close to real time assessment of the variables of interests as well as the examination of day-to-day variability within individuals. Further, the comorbid PTSD/AUD sample examined has approximately even numbers of men and women. The sample was also comprised of individuals seeking to make a change in their drinking and thus the current examination of craving and potential moderators of craving is highly clinically relevant.
There are, however, several pertinent limitations. First, the measure of craving employed in the daily monitoring protocol consisted of a relatively small number of items and it pertained only to alcohol. Although the administration of lengthy assessments should be balanced with advantages offered via situation-level design strategies, inferences based on our abbreviated approach should be interpreted with some caution and craving for substances other than alcohol need to be considered. In addition, this study focused on self-reported craving, and other measures of craving (e.g., psychophysical measures) may exhibit distinct relationships with substance-related outcomes. It is also possible that self-reported craving and alcohol use may be related via a third variable, such as willingness to report alcohol-related experience. That is, those who were willing to report craving may also be likely to report use. Further, as noted above, the assessment of craving avoidance and craving resistance were limited to one item each in the daily monitoring protocol.
The study sample was also comprised solely of treatment seeking individuals with both AUD and PTSD and as such, we do not know whether this pattern of results is generalizable to non-treatment seekers and/or people with AUD only or with AUD and other comorbidities. Although we have no specific reason to expect there to be pronounced differences between this group and other groups with AUD on these craving constructs, it is possible that individuals with PTSD could be especially reactive to discomfort associated with craving, perhaps leading to greater drinking to dampen the associated distress (Saladin et al., 2003). Because we used a daily data collection model rather than an ecological momentary analysis one, we were also unable to evaluate the exact temporal sequencing of craving, control efforts, and drinking could not be established by the single daily assessment measurement protocol employed in this study, our findings should be interpreted with caution. Finally, the results reported in this study are correlational, and as such, should not be interpreted as causal. Future studies that include more frequent monitoring assessments are needed to begin to examine the temporal relationships between these important constructs.
4.2. Summary
The present study replicates and extends previous research on the relationships among craving, efforts to control craving, and alcohol use by investigating these associations at the situational level in a sample of individuals with comorbid AUD and PTSD and further evaluating the role of baseline change motivation. Taken together, study findings contribute important information to the addictions treatment literature by highlighting the significance of craving in maintaining use in those attempting to change their drinking as well as the potential buffering effect of baseline change motivation and craving control efforts. These findings lend support for interventions targeting motivation to change (Smedslund et al., 2011), as well as for those that facilitate stronger control and amelioration of craving among individuals diagnosed with PTSD/AUD attempting to decrease or abstain from alcohol (Hendershot, Witkiewitz, George, & Marlatt, 2011).
Highlights.
Daily craving was positively related to alcohol use in individuals with AUD/PTSD.
Greater change motivation was negatively related to alcohol use.
Efforts to resist/avoid craving were negatively related to alcohol use.
The craving-use relationship was stronger for those with low change motivation.
Those with low craving control were more likely to drink at high craving levels.
Efforts to ameliorate craving may be critical for treatment success.
Acknowledgements
This material is the result of work supported by an NIH/NIAAA award (GRANT R21 AA 17130-01) to Dr. Tracy Simpson and by resources from the Center of Excellence in Substance Abuse Treatment and Education (CESATE), the Mental Illness Research, Education, and Clinical Center (MIRECC), the US Department of Veterans Affairs Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, and the VA Puget Sound Health Care System, Seattle, WA. The views expressed in this article are those of the authors and do not represent the views of the Department of Veteran Affairs or the United States government. Dr. Tyler Wray is now affiliated with the Department of Behavioral and Social Sciences, Brown University, School of Public Health, 121 South Main St., Providence RI 02912.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This model was also run with the ambivalence subscale included in the SOCRATES motivation for change total score and the results did not change.
References
- Adamson SJ, Sellman JD, Frampton C. Patient predictors of alcohol treatment outcome: A systematic review. Journal of Substance Abuse Treatment. 2009;36:75–86. doi: 10.1016/j.jsat.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Allison PD. Missing data. In: Millsap RE, Maydeu-Olivares A, editors. Handbook of Quantitative Methods in Psychology. Thousand Oaks, CA: Sage Publications, Inc.; 2009. [Google Scholar]
- Agrawal A, Wetherill L, Bucholz KK, Kramer J, Kuperman S, Lynskey MT, Bierut LJ. Genetic influences on craving for alcohol. Addictive Behaviors. 2013;38:1501–1508. doi: 10.1016/j.addbeh.2012.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual, text revision (DSM-IV-TR) Washington, DC: American Psychiatric Publishing; 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- Anton RF. Obsessive–compulsive aspects of craving: development of the Obsessive Compulsive Drinking Scale. Addiction. 2000;95:S211–S217. doi: 10.1080/09652140050111771. [DOI] [PubMed] [Google Scholar]
- Badour CL, Blonigen DM, Boden MT, Feldner MT, Bonn-Miller MO. A longitudinal test of the bi-directional relations between advoidance coping and PTSD severity druing and after PTSD treamtent. Behavior and Research Therapy. 2012;50:610–616. doi: 10.1016/j.brat.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Xu Y, Brady K, Perez-Fuentes G, Okuda M, Wang S. Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: Results from National Epidemiolocial Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2013;132:630–638. doi: 10.1016/j.drugalcdep.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady KT, Killeen T, Saladin ME, Dansky B, Becker S. Comorbid substance abuse and posttraumatic stress disorder. American Journal on Addictions. 1994;3:160–164. [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the U.S., 2006. American Journal of Preventive Medicine. 2011;41(5):516–524. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Crosby RD, Silgado J, Wonderlich SA, Schmidt Immediate antecedents of marijuana use: An analysis from ecological momentary assessment. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43:647–655. doi: 10.1016/j.jbtep.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Maisto SA, Carey MP, Purnine DM. Measuring readiness-to-change substance misuse among psychiatric outpatients: I. Reliability and validity of self-report measures. Journal of Studies on Alcohol. 2001;62(1):79–88. doi: 10.15288/jsa.2001.62.79. doi: http://dx.doi.org/10.15288/jsa.2001.62.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra S, Scharf D, Schiffman S. Within-day temporal patterns of smoking, withdrawal symptoms, and craving. Drug and Alcohol Dependence. 2011;117:118–125. doi: 10.1016/j.drugalcdep.2010.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Saladin ME, Drobes DJ, Brady KT, Dansky BS, Kilpatrick DG. Trauma and substance cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug and Alcohol Dependence. 2002;65(2):115–127. doi: 10.1016/s0376-8716(01)00157-0. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Schumacher JA, Stasiewicz PR, Henslee AM, Baillie LE, Landy N. Craving and physiological reactivity to trauma and alcohol cues in posttraumatic stress disorder and alcohol dependence. Experimental and mClinical Psychopharmacology. 2010;18(4):340–349. doi: 10.1037/a0019790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly JM, Kavanagh DJ, Baker A, Kay-Lambkin F, Lewin T, Davis P, Quek L. Craving as a predictor of treatment outcomes in heavy drinkers with comorbid depressed mood. Addictive Behaviors. 2013;38(2):1585–1592. doi: 10.1016/j.addbeh.2012.06.003. [DOI] [PubMed] [Google Scholar]
- Cooney NL, Litt MD, Cooney JL, Pilkey DT, Steinberg HR. Alcohol and tobacco cessation in alcohol-dependent smokers: Analysis of real-time reports. Psychology of Addictive Behaviors. 2007;21:277–286. doi: 10.1037/0893-164X.21.3.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drapkin ML, Yusko D, Yasinski C, Oslin D, Hembree EA, Foa EB. Baseline functioning among individuals with posttraumatic stress disorder and alcohol dependence. Journal of Substance Abuse Treatment. 2011;41:186–192. doi: 10.1016/j.jsat.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, Tofighi D. Centering predictor variables in cross-sectional multilevel models: A new look at an old issue. Psychological Methods. 2007;12:121–138. doi: 10.1037/1082-989X.12.2.121. [DOI] [PubMed] [Google Scholar]
- Evern C, Cetin R, Durkaya M, Dalbudak E. Clinical factors associated with relapse in male alcohol dependents during six-month follow-up. Bulletin of Clinical Psychopharmacology. 2010;20:14–22. [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview of DSM-IV Axis 1 (SCID-1) Disorders: Clinical Version. New York: Biometrics Research Department; 1995. [Google Scholar]
- Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcoholism: Clinical and Experimental Research. 1999;23(8):1289–1295. [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post- traumatic stress disorder. Journal of Traumatic Stress. 1993;6(4):459–473. [Google Scholar]
- Garland EL, Carter K, Ropes K, Howard MO. Thought suppression, impaired regulation of urges and Addiction-Stroop predict affect-modulated cue-reactivity among alcohol dependent adults. Biological Psychology. 2012;89:87–93. doi: 10.1016/j.biopsycho.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grusser SM, Morsen CP, Flor H. Alcohol craving in problem and occasional alcohol drinkers. Alcohol and Alcoholism. 2006;41(4):421–425. doi: 10.1093/alcalc/agl035. [DOI] [PubMed] [Google Scholar]
- Hardin JW, Hilbe JM. Generalized Estimating Equations. Boca Raton, FL: Chapman & Hall/CRC; 2003. [Google Scholar]
- Hayes SC. Content, context, and the types of psychological acceptance. Acceptance and change: Content and context in psychotherapy. 1994:13–32. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Press; 1999. [Google Scholar]
- Heilig M, Goldman D, Berrettini W, O'Brien CP. Pharmacogentic approaches to the treatment of alcohol addiction. Nature Reviews. 2011;12:670–684. doi: 10.1038/nrn3110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendershot CS, Witkiewitz K, George WH, Marlatt GA. Relapse prevetnion for addictive behaviors. Substance Abuse Treatment, Prevention, and Policy. 2011;6:1–17. doi: 10.1186/1747-597X-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt LJ, Litt MD, Cooney NL. Prospective analysis of early lapse to drinking and smoking among individuals in concurrent alcohol and tobacco treatment. Psychology of Addictive Behaviors. 2012;26:561–572. doi: 10.1037/a0026039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung Y-C, Namkoong K. Pharmacotherapy for alcohol dependence: anticraving medications for relapse prevention. Yonsei Medical Journal. 2006;47(2):167–178. doi: 10.3349/ymj.2006.47.2.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanagh DJ, May J, Andrade J. Tests of the elaborated intrusion theory of craving and desire: Features of alcohol craving during treatment for an alcohol disorder. British Journal of Clinical Psychology. 2009;48(3):241–254. doi: 10.1348/014466508X387071. [DOI] [PubMed] [Google Scholar]
- Keyes K, Krueger R, Grant B, Hasin D. Alcohol craving and the dimensionality of alcohol disorders. Psychological medicine. 2011;41(3):629. doi: 10.1017/S003329171000053X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klien AA. Suppression-induced hyperaccessibility of thoughts in abstinent alcoholics: A preliminary investigation. Behavior Research and Therapy. 2007;45:169–177. doi: 10.1016/j.brat.2005.12.012. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Mulgrew CL, Modesto-Lowe V, Burleson JA. Validity of the Obsessive Compulsive Drinking Scale (OCDS): does craving predict drinking behavior? Alcoholism: Clinical and Experimental Research. 1999;23(1):108–114. [PubMed] [Google Scholar]
- Levola J, Pitkanen T. P-54 - Social consequences of alcohol dependence - a review of the literature. European Psychiatry. 2012;27(Suppl 1):1. [Google Scholar]
- Litt MD, Cooney NL, Morse P. Reactivity to alcohol-related stimuli in the laboratory and in the field: predictors of craving in treated alcoholics. Addiction. 2000;95(6):889–900. doi: 10.1046/j.1360-0443.2000.9568896.x. [DOI] [PubMed] [Google Scholar]
- Love A, James D, Willner P. A comparison of two alcohol craving questionnaires. Addiction. 1998;93(7):1091–1102. doi: 10.1046/j.1360-0443.1998.937109113.x. [DOI] [PubMed] [Google Scholar]
- Marhe R, Waters AJ, van de Wetering JM, Franken HA. Implicit and explicit drug-related cognitions during detoxification treatment are associated with drugrelapse: An ecological momentary assessment study. Journal of Consulting and Clinical Psychology. 2013;81:1–12. doi: 10.1037/a0030754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer RE. Craving: what can be done to bring the insights of neuroscience, behavioral science and clinical science into synchrony. Addiction. 2000;95:S219–S227. doi: 10.1080/09652140050111780. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S, editors. Motivational interviewing: Helping people change. 3rd ed. New York, NY: Guilford Press; 2013. [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers' motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10(2):81–89. [Google Scholar]
- Muraven M, Collins RL, Nienhaus K. Self-control and alcohol restraint: An initial application of the self-control strength model. Psychology of Addictive Behaviors. 2002;16:113–120. doi: 10.1037//0893-164x.16.2.113. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Moos RH, Finney JW. Two-year mental health service use and course of remission in patients with substance use and posttraumatic stress disorder. Journal of Studies on Alcohol. 2000;61:247–253. doi: 10.15288/jsa.2000.61.247. [DOI] [PubMed] [Google Scholar]
- Oslin DW, Cary M, Slaymaker V, Colleran C, Blow FC. Daily ratings measures of alcohol craving during an inpatient stay define subtypes of alcohol addiction that predict subsequent risk for resumption of drinking. Drug and Alcohol Dependence. 2009;103(3):131–136. doi: 10.1016/j.drugalcdep.2009.03.009. doi: [DOI] [PubMed] [Google Scholar]
- Palfai TP, Monti PM, Colby SM, Rohsenow DJ. Effects of suppressing the urge to drink on the accesibility of alcohol outcome expectancies. Behavior Research and Therapy. 1997;1:59–65. doi: 10.1016/s0005-7967(96)00079-4. doi: [DOI] [PubMed] [Google Scholar]
- Preston KL, Massoud V, Schmittner J, Lin JL, Gorelick DA, Epstein DH. Cocaine craving and use during daily life. Psychopharmacology. 207:291–301. doi: 10.1007/s00213-009-1655-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy: Theory, Research and Practice. 1982;19(3):276–288. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models:Applications and data analysis methods. 2nd ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Ray LA, Hutchison KE, Bryan A. Psychosocial predictors of treatment outcome, dropout, and change processes in a pharmacological clinical trial for alcohol dependence. Addictive Disorders & Their Treatment. 2006;5:179–190. [Google Scholar]
- Read JP, Brown P, Kahler C. Substance use and posttraumatic stress disorders: Symptom interplay and effects on outcome. Addictive Behaviors. 2004;29:1665–1672. doi: 10.1016/j.addbeh.2004.02.061. [DOI] [PubMed] [Google Scholar]
- Saladin ME, Drobes DJ, Coffey SF, Dansky BS, Brady KT, Kilpatrick DG. PTSD symptom severity as a predictor of cue-elicited drug craving in victims of violent crime. Addictive Behaviors. 2003;9:1611–1629. doi: 10.1016/j.addbeh.2003.08.037. [DOI] [PubMed] [Google Scholar]
- Simpson TS, Stappenback CA, Luterek JA, Lehavot K, Kaysen DL. Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology. 2014;123:237–247. doi: 10.1037/a0035193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedslund G, Berg RC, Hammerstrøm KT, Steiro A, Leiknes KA, Dahl HM, Karlsen K. Motivational interviewing for substance abuse. Cochrane Database of Systematic Reviews. 2011;5 doi: 10.1002/14651858.CD008063.pub2. Art.No.:CD008063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stata Corp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: Role of automatic and nonautomatic processes. Psychological Review. 1990;97(2):147–168. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Torchalla I, Nosen L, Rostam H, Allen P. Integrated treatment programs for individuals with concurrent substance use disorders and trauma experiences: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. 2012;42:65–77. doi: 10.1016/j.jsat.2011.09.001. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global status report on alcohol and health. Geneva, Switzerland: WHO Press; 2011. [Google Scholar]