Abstract
Objective
This study examined racial/ethnic differences in demographic variables and the clinical presentation of treatment-seeking adults with binge eating disorder (BED) who participated in treatment research at a medical-school based program.
Method
Participants were 775 (n=195 men, n=560 women) treatment-seeking adults with DSM-IV-defined BED who self-identified as Black (n=121), Hispanic (n=54), or White (n=580). Doctoral-level research-clinicians assessed participants for BED and for eating-disorder psychopathology using the Structured Clinical Interview for DSM-IV Disorders (SCID) and the Eating Disorder Examination (EDE) interview, and measured height and weight. Participants also completed established self-report measures.
Results
Black participants had a greater proportion of women than White participants and White participants had higher education than Black and Hispanic participants. Black participants had higher body mass index (BMI) and reported more frequent binge-eating episodes than White participants but eating-disorder psychopathology (EDE scales and global severity) did not significantly differ across racial/ethnic groups. Black participants had lower depression than Hispanic and White participants. These differences in clinical presentation remained unchanged after adjusting for age, education, sex, and BMI. White participants had younger ages of onset for dieting, binge eating, and obesity, but not BED, than Black and Hispanic participants.
Conclusions
There are some racial/ethnic differences in the developmental trajectories and clinical presentation of treatment-seeking adults with BED that remain unchanged after adjusting for demographic differences. Black participants presented for treatment with higher BMI and binge-eating frequency than White participants and with lower depression than White/Hispanic groups but associated eating-disorder psychopathology levels were similar across racial/ethnic groups.
Keywords: binge eating disorder, obesity, race, ethnicity, treatment
An emerging literature has begun to establish that diverse racial/ethnic groups experience clinically significant eating-disorder psychopathology (Hudson, Hiripi, Pope, & Kessler, 2007; Marques et al., 2011). This is especially the case for binge eating disorder (BED), the most prevalent eating disorder diagnosis, which has much less disparity across sex (Hudson et al., 2007) and racial/ethnic groups than other eating disorder diagnoses (Marques et al., 2011). In epidemiological studies, BED is at least as prevalent in Black and Hispanic as White individuals (Hudson et al., 2007; Marques et al., 2011). Moreover, the World Health Organization found generally comparable BED prevalence across countries (Kessler et al., 2013).
Despite comparable prevalence of BED across racial/ethnic groups, very little is known about racial/ethnic similarities or differences in the development and clinical manifestation of BED. In community-based BED studies, Black participants have higher body mass index (BMI) than White participants (Pike, Dohm, Striegel-Moore, Wilfley, & Fairburn, 2001) but report similar frequency of binge eating episodes (Striegel-Moore, Wilfley, Pike, Dohm, & Fairburn, 2000), and lower levels of eating-disorder psychopathology (Pike et al., 2001) than White participants. Black and Hispanic participants report similar impairment due to BED as White participants (Marques et al., 2011). Despite these patterns, White participants are more likely than Black and Hispanic participants to seek any form of BED treatment, particularly mental health treatment (Marques et al., 2011).
Even less is known about racial/ethnic differences in the clinical presentation of treatment-seeking individuals with BED because treatment studies have generally had very low rates of minority group representation, and published reports do not provide information related to differential exclusion or enrollment. Taken together, the observed racial/ethnic differences in clinical characteristics (Pike et al., 2001) and treatment-seeking (Marques et al., 2011) reported in community studies, coupled with findings that there may be sampling biases in Black women seeking BED treatment (Grilo, Lozano, & Masheb, 2005), highlight the need for research on racial/ethnic differences in BED treatment research participants.
To examine racial/ethnic differences in treatment-seeking adults with BED, Franko et al (2012) pooled adults with BED from nine research sites that enrolled patients in 11 clinical trials for psychosocial treatments (Black, n=102; Hispanic, n=64; White, n=1159). Black participants had higher BMI than White participants, and Hispanic participants reported greater eating-disorder psychopathology than White participants, but binge eating frequency was not significantly different. Findings from this study require replication and extension for several reasons: (1) Franko et al (2012) pooled data obtained with similar, yet methodologically different, eating-disorder assessment tools (i.e., nine studies used interview and two used self-report); (2) sites contributing data had dramatically different racial/ethnic representation, and had potentially different recruitment strategies, inclusion/exclusion criteria, and assessment procedures; and (3) participants were seeking psychosocial treatments. Thus, additional research is needed to extend racial/ethnic findings in treatment-seeking adults with BED.
The current study aimed to examine racial/ethnic differences in BED clinical presentation and associated eating-disorder psychopathology in a large treatment-seeking group with BED at one location using a consistent, interview-based evaluation of key eating-disorder variables, and consistent recruitment strategies, inclusion criteria, and assessment protocols. We hypothesized that our findings would parallel those of Franko et al (2012). This study also expanded prior research by comparing group differences in depression, and developmental trajectories of eating-related problems.
Method
Participants
Participants (N=755) responded to advertisements for psychosocial and medication treatment studies for BED at an urban, medical-school based program located in the Northeastern US. Participants were between 18 and 65 years old and met full DSM-IV (American Psychiatric Association, 2004) criteria for BED1. Participants were excluded if they were receiving treatment for eating/weight concerns, had medical conditions that influenced eating/weight (e.g., diabetes), had a severe mental illness that could interfere with clinical assessment (e.g., psychosis), or were pregnant. Participants were included in the current analyses if they self-identified as Black (n=121, 16.0%), Hispanic (n=54, 7.2%) or White (n=580, 76.8%)2. Participants had a mean age of 45.75 (SD=9.80) and a mean BMI of 38.15 kg/m2 (SD=6.84). Participants were primarily female (n=560, 74.2%), and had varying levels of education: high school or less than high school (n=144, 19.1%), some college or an associate’s degree (n=264, 35.2%), or a college degree (n=344, 45.8%). This study received approval from the university’s ethical review board; all enrolled participants provided written informed consent.
Measures
Trained doctoral-level research clinicians, monitored to maintain reliability, evaluated participants. Research clinicians administered the Structured Clinical Interview for DSM-IV Axis I Disorders (First, Spitzer, Gibbon, & Williams, 1997) to determine DSM-IV-based BED diagnosis and age of onset, and the semi-structured Eating Disorder Examination (Fairburn & Cooper, 1993) to confirm BED diagnosis and characterize eating-disorder psychopathology. Research clinicians measured participants’ height and weight and calculated BMI (kg/m2).
Eating Disorder Examination (EDE)
The EDE (Fairburn & Cooper, 1993) is an investigator-based interview that evaluates eating-disorder psychopathology in the past 28 days, and over longer intervals corresponding to diagnostic criteria. The EDE also assesses three types of eating episodes: objective bulimic episodes (OBEs, eating an unusually large amount of food while perceiving a loss of control over eating; this is the DSM-IV definition of binge eating episodes), subjective bulimic episodes (SBEs, eating a small or typical amount of food while perceiving a loss of control) and objective overeating episodes (OOEs, eating an unusually large amount of food without perceiving a loss of control). Four subscales reflect eating-disorder psychopathology (Restraint, Eating Concern, Shape Concern, and Weight Concern), as does a Global severity score. The EDE is a well-established interview for assessing eating disorders with good inter-rater and test-retest reliability in BED (Grilo, Masheb, Lozano-Blanco, & Barry, 2004), and in diverse racial/ethnic groups (Grilo, Lozano, & Elder, 2005). EDE items in the current study were internally consistent, α=.81, with excellent inter-rater reliability3.
Self-report Questionnaires
The Beck Depression Inventory (BDI) is a well-established depression measure (Beck & Steer, 1987) that captures a broad range of negative affect and depression, and scores are useful indicators of both possible depression4 and broad psychosocial distress. The BDI has excellent psychometric properties with diverse samples (Beck, Steer, & Carbin, 1988). In the current study, internal consistency was excellent, α=.89. The Questionnaire for Eating and Weight Patterns, Revised (QEWP-R), used in DSM-IV field trials, assesses current and historical aspects of BED and obesity (Yanovski, 1993). The current study used the historical items (onset of obesity, dieting, and binge eating) and the reported race/ethnicity data.
Statistical Analyses
To evaluate racial/ethnic group differences, we compared Black, Hispanic, and White participants using chi-square tests (categorical variables), and analyses of variance (ANOVAs; continuous variables). Pairwise t-tests compared differences among groups. OBE, SBE, and OOE variables were transformed by square-root prior to analyses to meet the assumption of normality. Analyses of covariance (ANCOVAs) adjusted for age, education, sex, and BMI.
Results
Racial and Ethnic Differences in Demographic Variables
Table 1 summarizes the demographic characteristics and statistical tests examining racial/ethnic differences, which revealed significant differences in age, education, and sex5.
Table 1.
Demographic variables by racial and ethnic group.
| Black n=121 | Hispanic n=54 | White n=580 | χ2 | N | p | ϕ | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sex | 5.75 | 755 | .056 | .087 | ||||||
| Male | 17.36%c | 24.07% | 27.76%a | |||||||
| Female | 82.64%c | 75.93% | 72.24%a | |||||||
| Education | 23.34 | 751 | <.001 | .176 | ||||||
| High School or Less than High School | 26.45%c | 27.78%c | 16.67%a,b | |||||||
| Some College or Associate’s Degree | 43.80%c | 40.74% | 32.81%a | |||||||
| College Degree | 29.75%c | 31.48%c | 50.52%a,b | |||||||
| M | SE | M | SE | M | SE | F | Total df | p | ηp2 | |
| Age | 45.45b | 0.89 | 41.44a,c | 1.19 | 46.22b | 0.41 | 6.00 | 754 | .003 | .016 |
Note. Percentages reflect the proportion of participants from one racial/ethnic group (column) in the demographic category (row). Subscripts denote significant differences at the p<.05 level compared with a=Black participants, b=Hispanic participants, c=White participants.
Racial and Ethnic Differences in Weight, Eating, And Mood Variables
Table 2 summarizes the clinical characteristics along with statistical tests comparing racial/ethnic groups. Table 3 presents parallel data and statistical tests after adjusting for age, education, sex, and then parallel tests after adjusting for demographic variables and BMI. BMI was significantly higher for Black than White participants (p<.001). This relation remained significant after adjusting for demographic variables (p<.001). Black participants reported significantly more OBEs than White (p=.008) and Hispanic participants (p=.041), but differences were nonsignificant for SBEs and OOEs (all ps>.132). OBEs remained significantly more frequent for Black than White (p=.012) and Hispanic (p=.046) participants after adjusting for demographic variables, and SBEs and OOEs remained nonsignificant (all ps>.153). After adjusting for BMI as well as demographic variables, the Black/Hispanic difference in OBEs was no longer significant (p=.050), but the significance pattern otherwise remained the same. No significant racial or ethnic differences emerged in eating-disorder psychopathology (all ps>.064). Racial/ethnic differences in eating-disorder psychopathology remained nonsignificant after adjusting for demographic variables (all ps>.108), including BMI (all ps>.087). Depression levels were significantly lower in Black than White (p=.019) and Hispanic (p=.006) participants and remained significant after adjusting for demographic variables (Black vs White: p=.001; Black vs Hispanic: p=.007), and demographic with BMI (Black vs White: p<.001; Black vs Hispanic: p=.006); the difference reflected a medium effect-size (ηp2 = 0.60). After adjusting for multiple comparisons within each set of variables for ANCOVAs, the majority of omnibus tests maintained their significance. SBEs became nonsignificant after Bonferroni adjustment to .017, and Restraint became non-significant in ANCOVA without BMI after adjustment to .01.
Table 2.
Analyses of variance and pairwise comparisons.
| Black n=121 | Hispanic n=54 | White n=580 | Omnibus ANOVA | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | F | Total df | p | ηp2 | |
| BMI | 40.23c | 0.59 | 38.75 | 0.75 | 37.65a | 0.29 | 7.44 | 750 | .001 | .020 |
| Episodes | ||||||||||
| OBE | 21.67b,c | 1.16 | 16.80a | 1.74 | 17.84a | 0.53 | 3.91 | 754 | .020 | .010 |
| SBE | 9.14 | 1.15 | 8.00 | 1.73 | 7.24 | 0.53 | 1.51 | 754 | .221 | .004 |
| OOE | 3.34 | 0.73 | 3.08 | 1.11 | 3.71 | 0.34 | 0.03 | 753 | .966 | <.001 |
| EDE Global Score | 2.69 | 0.08 | 2.92 | 0.13 | 2.72 | 0.04 | 1.33 | 754 | .264 | .004 |
| Restraint | 1.80 | 0.11 | 2.09 | 0.19 | 1.84 | 0.05 | 1.03 | 754 | .356 | .003 |
| Eating | 1.98 | 0.12 | 2.29 | 0.17 | 2.11 | 0.06 | 1.09 | 754 | .338 | .003 |
| Shape | 3.73 | 0.12 | 3.98 | 0.16 | 3.68 | 0.05 | 1.73 | 754 | .178 | .005 |
| Weight | 3.27 | 0.10 | 3.32 | 0.16 | 3.25 | 0.04 | 0.14 | 754 | .869 | <.001 |
| BDI | 14.34b,c | 0.87 | 18.43a | 1.53 | 16.45a | 0.36 | 4.44 | 749 | .012 | .012 |
| Age of Onset | ||||||||||
| Obesity | 20.57c | 1.21 | 20.04c | 1.62 | 16.40a,b | 0.42 | 9.15 | 686 | <.001 | .026 |
| Dieting | 25.40c | 1.11 | 25.00c | 1.25 | 21.03a,b | 0.41 | 10.76 | 624 | <.001 | .033 |
| Binge Eating | 26.92c | 1.22 | 24.58 | 1.56 | 22.46a | 0.54 | 6.05 | 669 | .002 | .018 |
| BED | 28.51 | 1.26 | 25.49 | 1.88 | 26.67 | 0.58 | 1.18 | 691 | .308 | .003 |
Note. Subscripts denote significant differences at the p<.05 level compared with a=Black participants, b=Hispanic participants, c=White participants. Omitted subscripts indicate nonsignificant differences. Partial eta squared (ηp2) values are considered small at .01, medium at .06, and large at .14 (Cohen, 1988). OBE, SBE, and OOE variables were square root-transformed to meet assumptions of normality. However, we report non-transformed means here to facilitate interpretation. BMI=Body Mass Index; OBE=Objective bulimic episode; SBE=Subjective bulimic episode; OOE=Objective overeating episode; EDE=Eating Disorder Examination; BDI=Beck Depression Inventory; BED=Binge eating disorder.
Table 3.
Analyses of covariance pairwise comparisons adjusting for age, sex, education, and body mass index.
| Black n=121 | Hispanic n=54 | White n=580 | Omnibus ANCOVA (age, sex, edu) | Omnibus ANCOVA (age, sex, edu, BMI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | F | Total df | p | ηp2 | p | ηp2 | |
| BMI | 40.12c | 0.61 | 38.60 | 0.92 | 37.68a | 0.28 | 9.06 | 747 | <.001 | .058 | N/A | N/A |
| Episodes | ||||||||||||
| OBE | 21.55b,c | 1.18 | 16.65a* | 1.76 | 17.85a | 0.54 | 2.09 | 750 | .065 | .014 | .102 | .014 |
| SBE | 8.92 | 1.16 | 8.30 | 1.73 | 7.25 | 0.53 | 2.50 | 750 | .029 | .017 | .049 | .017 |
| OOE | 3.54 | 0.74 | 3.11 | 1.12 | 3.67 | 0.34 | 1.30 | 749 | .263 | .009 | .280 | .010 |
| EDE Global Score | 2.65 | 0.08 | 2.90 | 0.12 | 2.73 | 0.04 | 8.17 | 751 | <.001 | .052 | <.001 | .053 |
| Restraint | 1.80 | 0.12 | 2.14 | 0.18 | 1.83 | 0.06 | 2.57 | 751 | .026 | .017 | .001 | .029 |
| Eating | 1.91 | 0.12 | 2.25 | 0.18 | 2.12 | 0.06 | 5.73 | 751 | <.001 | .037 | <.001 | .039 |
| Shape | 3.66 | 0.10 | 3.93 | 0.16 | 3.70 | 0.05 | 7.59 | 751 | <.001 | .048 | <.001 | .050 |
| Weight | 3.22 | 0.09 | 3.28 | 0.14 | 3.26 | 0.04 | 6.85 | 751 | <.001 | .012 | <.001 | .044 |
| BDI | 13.65b,c | 0.81 | 17.60a | 1.22 | 16.70a | 0.37 | 9.23 | 746 | <.001 | .059 | <.001 | .060 |
| Age of Onset | ||||||||||||
| Obesity | 20.50c | 0.99 | 20.70c | 1.49 | 16.35a,b | 0.44 | 10.12 | 683 | <.001 | .070 | <.001 | .127 |
| Dieting | 25.68c | 0.95 | 25.55c | 1.39 | 20.87a,b | 0.40 | 17.00 | 621 | <.001 | .121 | <.001 | .145 |
| Binge Eating | 27.21c | 1.14 | 25.87c | 1.68 | 22.23a,b | 0.51 | 19.39 | 666 | <.001 | .128 | <.001 | .137 |
| BED | 28.49 | 1.19 | 27.34 | 1.78 | 26.47 | 0.55 | 20.08 | 688 | <.001 | .128 | <.001 | .130 |
Note. Subscripts denote significant differences at the p<.05 level compared with a=Black participants, b=Hispanic participants, c=White participants. Omitted subscripts indicate nonsignificant pairwise comparisons. Partial eta squared (ηp2) values are considered small at .01, medium at .06, and large at .14 (Cohen, 1988). OBE, SBE, and OOE variables were square root-transformed for ANCOVAs to meet assumptions of normality. However, we report non-transformed means here to facilitate interpretation. The education variable (edu) included five levels of education. BMI=Body Mass Index; OBE=Objective bulimic episode; SBE=Subjective bulimic episode; OOE=Objective overeating episode; EDE=Eating Disorder Examination; BDI=Beck Depression Inventory; BED=Binge eating disorder.
This pairwise comparison became non-significant when BMI was added to the ANCOVA. All other comparisons maintained the same significance pattern.
Exploratory Analyses of Developmental Trajectory Variables
Figure 1 depicts the developmental trajectory of obesity, dieting, binge eating, and BED as reported by participants at the time of the study. ANCOVAs adjusted for education and sex, and then parallel tests adjusted for education, sex, and BMI. Obesity onset was younger for White than Black (p<.001) and Hispanic participants (p=.020), which remained significant in ANCOVA (p<.001 and p=.005), and ANCOVA including BMI (p<.001 and p=.003). White participants reported younger dieting onset than Black (p<.001) and Hispanic (p=.008) participants, which remained significant in ANCOVA (p<.001 and p=.001), including BMI (p<.001 and p=.001). White participants reported younger binge eating onset than Black (p=.001) but not Hispanic (p=.250) participants. After adjusting for demographic variables, both binge eating onset comparisons were significant (p<.001 and p=.039), and these remained significant after also adjusting for BMI (p<.001 and p=.029). In contrast, BED onset for Black, Hispanic, and White participants were not significantly different (all ps>.182), which remained unchanged in ANCOVAs (all ps>.127), including BMI (all ps>.087).
Figure 1.
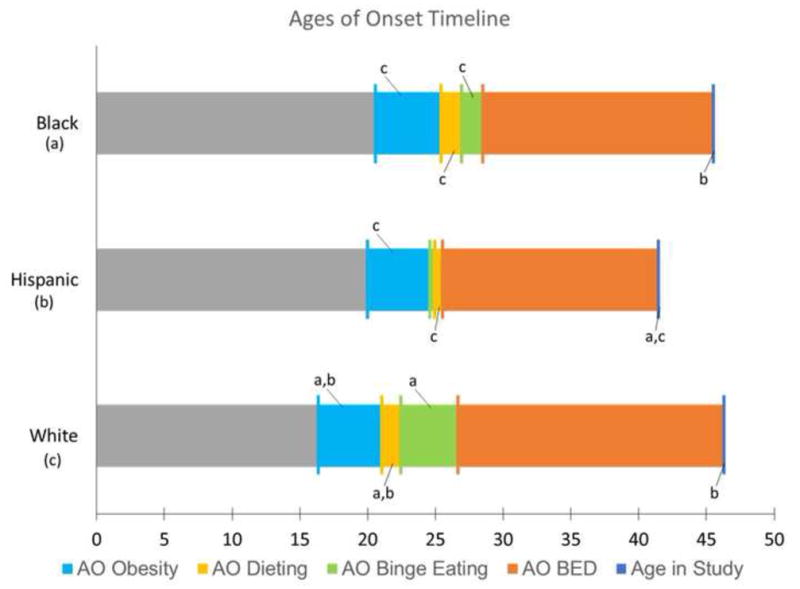
BED developmental trajectories for White, Hispanic, and Black treatment-seeking research participants.
Note. This figure depicts the mean ages of onset (AO) for obesity, dieting, binge eating, and binge eating disorder (BED) as reported by participants at the time of the study. Coefficients denote significant differences at the p<.05 level compared with a=Black participants, b=Hispanic participants, c=White participants. Omitted coefficients indicate nonsignificant pairwise comparisons
Discussion
This study examined demographic and clinical differences among treatment-seeking Black, Hispanic, and White participants with BED recruited for treatment studies. Our findings indicate that there are some racial/ethnic differences in clinical presentation, although there are also similarities. Specifically, BMI and binge eating frequency were higher in Black than White participants. Onset of dieting, binge eating, and obesity, but not BED, were younger for White than Black and Hispanic patients. Eating-disorder psychopathology was not significantly different. This suggests that Black participants are heavier and report more frequent binge eating compared with White participants but have similar concerns about weight, shape, and eating. It also appears that the developmental trajectory of BED is more rapid for Black participants than White participants. Black participants had lower depression scores (medium effect size) than White and Hispanic participants, perhaps indicating lower depression and distress levels.
Earlier research had discrepant results about racial/ethnic differences in treatment-seeking participants, and a key aim of the current study was to examine the clinical presentation of BED in a large treatment-seeking study group at one location and using interview-based assessment. Our findings that are consistent with earlier findings from Franko et al (2012) include higher BMI in Black compared with White participants, which is expected given broader trends in adult weight (Ogden, Carroll, Kit, & Flegal, 2013). However, the finding that Black participants had significantly more frequent OBEs than White participants differed from the nonsignificant findings of Franko et al (2012). Nonsignificant eating-disorder psychopathology differences in our study were discrepant from Franko et al (2012), which found that White participants have less eating-disorder psychopathology than Hispanic and Black participants, and from Pike et al (2001) that found more eating-disorder psychopathology for Black than White participants. Eating-disorder psychopathology in the current study was assessed with an investigator-based interview, unlike earlier community-based research that used self-report (Pike et al., 2001) or combined data from interview and self-report (Franko et al., 2012) methods.
Our study also provided novel findings on possible racial/ethnic differences in BED developmental trajectory. Dieting, binge eating, and obesity began at younger ages for White than Black and Hispanic participants. However, the age at which participants met BED diagnostic criteria was not significantly different across groups. These results suggest a more rapid developmental trajectory for Black participants than White participants, which warrants prospective investigation. In addition, findings suggest that the developmental trajectory for Hispanic participants may follow a different pattern than Black and White participants, with binge eating preceding dieting rather than following. These exploratory findings warrant prospective study, particularly given the limitation that onset variables were retrospective, self-report data. There is a high degree of concordance (r=.99) between current self-reported and measured BMI (Ivezaj, Kalebjian, Grilo, & Barnes, 2014), and longitudinal epidemiological work has shown strong correlations (r=.73) between recalled weight and past measured weight over ten years (Perry, Byers, Mokdad, Serdula, & Williamson, 1995). However, since recollections of when dieting, binge eating, and obesity began may be inaccurate or biased, these findings should be viewed cautiously, although they have hypothesis-generating value.
Our significant (BMI and depression) and nonsignificant (eating-disorder pathology) findings have implications for clinical practice. Patients with higher BMI may be at greater risk for obesity-related medical complications and thus require additional medical monitoring; higher depression scores may signal heightened risk for comorbid depression or distress requiring clinical monitoring. Nonsignificant differences in eating-disorder psychopathology suggest that existing BED treatments may not require modification to treat different races/ethnicities. Further research is needed to establish whether clinical presentation (e.g., Masheb & Grilo, 2008) and race/ethnicity predict BED treatment outcomes (e.g., Thompson-Brenner et al., 2013)6.
Our findings pertain to participants from a northeastern US urban environment. This study design allowed us to eliminate potential confounds due to geographical and site-specific differences that may exist in the Franko et al (2012) pooled data. The trials at our site used consistent study protocols, including consistent recruitment, eligibility determination, assessment sequencing and measures, and training and quality control. Findings from Franko et al (2012) and our study, which have similar sample sizes for Black (n=120 and n=121) and Hispanic (n=64 and n=54) groups, should be considered in conjunction with each other, as each has different strengths/limitations. Despite the strengths our study offers, there are limitations. We used a single-choice checklist to assess race/ethnicity; assessment using an open-ended, multi-choice, or dimensional racial identity assessment may yield more information on race/ethnicity and BED treatment-seeking, and larger samples of additional races/ethnicities would allow for additional group comparisons. In addition, our findings are based on treatment-seeking adults with BED who responded to recruitment for treatment studies at a university-based medical school, and we had some exclusion criteria (e.g., diabetes, pregnancy). Most were highly educated. Our findings may not generalize to those with less education, to non-treatment-seeking persons with BED, to persons with BED who seek treatment naturalistically in different clinic settings (Marques et al., 2011), or to those who do not participate in treatment research (Grilo, Lozano, & Masheb, 2005).
Examining racial/ethnic differences in clinical presentation of persons with BED is important to guide refinement of treatment and prevention efforts. Further research is needed to improve understanding of specific treatment-related needs, and whether meaningful differences across racial/ethnic groups exist in treatment. Future research should also examine whether racial/ethnic factors, along with clinical factors, influence treatment-seeking and whether they predict or moderate treatment outcomes. Replication of our findings regarding racial/ethnic differences in age at onset and developmental trajectories (e.g., older onset for Black and Hispanic than White participants, and more rapid developmental trajectory for Black participants) could support and refine prevention and early intervention efforts by identifying optimal times and patient groups for intervention.
Public Health Significance.
This study indicates the importance of race and ethnicity in research treatment studies for binge eating disorder. Among treatment-seeking research participants, there are racial/ethnic differences in development trajectories (White individuals have younger ages of onset for dieting, binge eating, and obesity than Black and Hispanic individuals) and some clinical variables (Black individuals have higher body mass index and report more frequent binge eating than Whites and lower depression than White and Hispanic individuals). We observed no racial/ethnic differences, however, in associated eating-disorder psychopathology and the patterns of similarities and differences remained unchanged after adjusting for demographic differences across groups.
Acknowledgments
This research was supported, in part, by National Institutes of Health grants K24 DK070052 and R01 DK49587 (Dr. Grilo).
Footnotes
DSM-IV (APA, 2004) BED research criteria include binge eating at least twice weekly (eating an objectively large amount of food while experiencing a subjective loss of control) for six months, without weight compensatory behaviors (e.g., purging). These criteria are more stringent than the newly published DSM-5 BED diagnostic criteria, which require binge eating at least once weekly for three months.
Race was determined using a single-choice checklist item from the QEWP-R (Yanovski, 1993). The full dataset also included potential participants who self-reported as Asian (n=10), “Other” (n=21), and those who did not report their race/ethnicity (n=23); these respondents were excluded from the current study.
In the present study, inter-rater reliability of the EDE was examined in 113 cases. The intraclass correlation coefficient for OBEs was 0.94, Global severity score was 0.92, Restraint was 0.92, Eating Concern was 0.78, Weight Concern was 0.91, and Shape Concern was 0.94.
Scores of <10 indicate no or minimal depression, 10–18 is mild-moderate depression, 19–29 is moderate-severe depression and >30 is severe depression (Beck et al., 1988).
Hispanic participants were significantly younger than both Black participants (p=.012) and White participants (p=.001). Black participants had a greater proportion of females compared with White participants (p=.018). More Black (p=.011) and Hispanic (p=.040) participants had an education of high school or less compared with White participants. More Black participants had some college or an associate’s degree compared with White participants (p=.018). Fewer Black (p<.001) and Hispanic (p=.009) participants had a college degree compared with White participants.
Thompson-Brenner et al (2013), in their study of whether race/ethnicity predicted or moderated treatment outcomes for the Franko et al (2012) study, reported generally comparable outcomes by race/ethnicity except that Black participants had higher attrition and less improvement in eating-disorder psychopathology scores. Of note, Thompson-Brenner et al (2013) did not measure depression levels which may be an important clinical variable. Our findings here suggest that Black patients with BED may present with lower depression levels and there are empirical reports that BDI scores predict treatment outcomes and attrition in BED (Masheb & Grilo, 2008).
The authors report no conflicts of interest.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: Author; 2004. Text Revision ed. [Google Scholar]
- Beck AT, Steer R. Manual for revised Beck Depression Inventory. New York: Psychological Corporation; 1987. [Google Scholar]
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment. NY: Guilford Press; 1993. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), Clinician Version. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Franko DL, Thompson-Brenner H, Thompson DR, Boisseau CL, Davis A, Forbush KT, Wilson GT. Racial/ethnic differences in adults in randomized clinical trials of binge eating disorder. Journal of Consulting & Clinical Psychology. 2012;80:186–195. doi: 10.1037/a0026700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Lozano C, Elder KA. Inter-rater and test-retest reliability of the Spanish language version of the eating disorder examination interview: clinical and research implications. Journal of Psychiatric Practice. 2005;11:231–240. doi: 10.1097/00131746-200507000-00003. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Lozano C, Masheb RM. Ethnicity and sampling bias in binge eating disorder: Black women who seek treatment have different characteristics than those who do not. International Journal of Eating Disorders. 2005;38:257–262. doi: 10.1002/eat.20183. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. International Journal of Eating Disorders. 2004;35:80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivezaj V, Kalebjian R, Grilo CM, Barnes RD. Comparing weight gain in the year prior to treatment for overweight and obese patients with and without binge eating disorder in primary care. Journal of Psychosomatic Research. 2014;77:151–154. doi: 10.1016/j.jpsychores.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, Xavier M. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biological Psychiatry. 2013;73:904–914. doi: 10.1016/j.biopsych.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, Diniz JB. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. International Journal of Eating Disorders. 2011;44:412–420. doi: 10.1002/eat.20787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Examination of predictors and moderators for self-help treatments of binge eating disorder. Journal of Consulting and Clinical Psychology. 2008;76:900–904. doi: 10.1037/a0012917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011–2012. 2013;131:1–8. [PubMed] [Google Scholar]
- Perry GS, Byers TE, Mokdad AH, Serdula MK, Williamson FD. The Validity of Self-Reports of Past Body Weights by U.S. Adults. 1995;6:61–66. doi: 10.1097/00001648-199501000-00012. [DOI] [PubMed] [Google Scholar]
- Pike KM, Dohm FA, Striegel-Moore RH, Wilfley DE, Fairburn CG. A comparison of black and white women with binge eating disorder. American Journal of Psychiatry. 2001;158:1455–1460. doi: 10.1176/appi.ajp.158.9.1455. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Wilfley DE, Pike KM, Dohm FA, Fairburn CG. Recurrent binge eating in black American women. Archives Family Medicine. 2000;9:83–87. doi: 10.1001/archfami.9.1.83. [DOI] [PubMed] [Google Scholar]
- Thompson-Brenner H, Franko DL, Thompson DR, Grilo CM, Boisseau CL, Roehrig JP, Wilson GT. Race/ethnicity, education, and treatment parameters as moderators and predictors of outcome in binge eating disorder. Journal of Consulting & Clinical Psychology. 2013;81:710–721. doi: 10.1037/a0032946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanovski SZ. Binge eating disorder: Current knowledge and future directions. Obesity Research. 1993;1:306–324. doi: 10.1002/j.1550-8528.1993.tb00626.x. [DOI] [PubMed] [Google Scholar]


