Abstract
Purpose
The study objectives are to describe the longitudinal trajectory of prescription opioid use among adolescents requiring a trauma admission and then identify predictors of sustained opioid use.
Methods
Randomly sampled adolescents (12–18 years) admitted to a Level I trauma center were surveyed. Follow-up assessments were obtained at 2-, 5- and 12-months. Self-reported prescription opioid use, defined as 'taking an opioid prescribed by a physician,' was obtained at baseline and every follow-up time point. At the baseline interview, validated mental health measures and pain scales were obtained as well as pre-injury substance use. A fixed-effects mixed Poisson regression analysis was performed to predict prescription opioid use over time.
Results
A total of 120 adolescents (mean age 15.5 years (1.9 SD), 75% male) completed the baseline interview with 98% follow-up at 12-months. At baseline, 7% of adolescents reported prescription opioid use prior to their trauma, with rates of prescription opioid use of 52% at 2-months, 13.3% at 5-months and 12.5% at 12-months after discharge. After adjusting for demographic characteristics and injury severity score, those with sustained prescription opioid use were more likely to report pre-injury marijuana use and higher baseline pain scores.
Conclusions
Approximately one in eight adolescents (12.5%) was using prescription opioids 12-months after injury hospitalization. Readily identifiable risk factors predicted sustained prescription opioid use, including pre-injury marijuana use and baseline pain score. Screening for substance use including marijuana at the time of injury could help identify patients at risk for both substance use problems and sustained prescription opioid use.
Implications and Contribution
The study objective was to determine risk factors for sustained prescription opioid use after admission for trauma. Adolescents with pre-injury marijuana use and high baseline pain scores had increased risk of sustained prescription opioid use. Screening for substance use at the time of injury could help identify patients at risk.
Introduction
Prescription opioids are often used to treat acute pain from illness or injury. Prescription opioid use, defined as using prescribed opioids to treat acute pain in the way intended by the prescriber is increasing and opioids are the most commonly prescribed controlled substance among adolescents.[1] While prescription opioid use can be an important part of the treatment for acute pain, recent studies have shown that prescription opioid use is associated with misuse of prescription opioids,[2, 3] which can lead to overdose and death.[4] Acute pain and prescription opioid use can also lead to chronic pain and chronic opioid therapy. Sustained or chronic opioid therapy is defined as prescription opioid therapy for most days in the past ninety.[5] Predictors of sustained prescription opioid use in adolescents after an episode of acute pain remain unknown.
Initiating prescription opioid therapy can lead to recurrent prescription opioid use,[6] prescription opioid misuse [7] and other adverse outcomes including overdose.[4] One in five adolescents with a prescription for opioids report misusing their prescribed opioids,[2] and 80% of high school students reporting prescription opioid misuse were initially prescribed opioids by a physician.[7] In an emergency department (ED) sample, 14.5% of adolescents and young adults reporting prescription opioid misuse had a current prescription for opioids.[8] While these previous studies suggest potential correlates of prescription opioid misuse; more information is needed to understand predictors of sustained prescription opioid use in adolescents after an episode of acute pain.
In a study limited to adolescents with idiopathic scoliosis undergoing spinal fusion, preoperative pain level and preoperative anxiety predicted higher postoperative pain at follow-up.[9] Among adult patients undergoing common surgical procedures, pre-surgical depressive symptoms were predictive of sustained opioid use at six months after surgery.[10] Likewise, patients on chronic opioid therapy tend to also have psychiatric and substance use disorders. Specifically, adolescents and young adults in outpatient clinics with mental health diagnoses have increased risk of sustained prescription opioid use compared to adolescent patients without mental health diagnoses.[11] Similarly, substance use is associated with chronic opioid therapy and is a risk factor for opioid dependence.[12] Identifying specific mental health disorders and substance use problems present prior to an injury causing acute pain could help identify adolescent patients at risk for chronic pain and thus sustained prescription opioid use after an injury and trauma admission. Currently, there are no studies that identify predictors of sustained opioid use after an acute injury among adolescents.
Opioids are often part of the initial treatment for acute post-injury pain. Limited data exists regarding the effectiveness of long-term opioid use in controlling non-acute or chronic pain.[13] Injury is the leading cause for ED visits among adolescents [14, 15] and a source of acute pain. Recognizing and understanding pre-injury risk factors for sustained prescription opioid use could help physicians to identify and intervene with high-risk injured youth, thereby reducing rates of sustained prescription opioid use and possibly opioid dependence and misuse. Therefore, this study aims to determine demographics, baseline clinical characteristics, and pre-injury substance use and mental health comorbidity that predict longitudinal prescription opioid use up to one year after admission for a trauma in a population of adolescents.
Methods
Study Site and Population
Adolescents (12–18 years old) admitted to the Harborview Medical Center (HMC) trauma service, or in the ED for greater than 24 hours, from March 1, 2008 to October 31, 2009 were randomly sampled and the adolescents and their parents were surveyed as part of a larger randomized clinical trial comparing stepped collaborative care to usual care for decreased violence, injury risk factors, substance use problems, PTSD and depression over time; approximately half of patients (n=61) participated in the intervention condition.[16] The intervention was delivered by a social worker or nurse practitioner trained in care management at a trauma center and included motivational interviewing elements targeting risk behaviors including alcohol use and drug use as well as medication therapy and elements of cognitive behavioral therapy targeting mental health conditions. The intervention did not focus specifically on pain. HMC is a large, urban, academic Level I trauma center in Seattle, WA. All adolescent patients with an injury requiring inpatient trauma care or greater than 24 hours in the ED, with a Glasgow Coma Score [17] (GCS) of 15 at the time of the baseline interview, were eligible for the study. Patients were excluded if they were non-English speakers (child or parents), incarcerated, or acutely suicidal. Patients admitted to the hospital with GCS of less than 15 were reapproached during their hospitalization if their GCS improved and was subsequently documented in the medical record to be 15 at a time during their hospital stay. Eligible participants under the age of 18 years assented and parental consent was obtained. Consent was obtained directly from participants that were 18 years old. Parents also provided consent. Study procedures were reviewed and approved by the University of Washington Institutional Review Board.
Study Procedures
All eligible adolescent participants were approached in the ED or inpatient trauma ward to complete an interview conducted by a trained Research Assistant (RA) regarding demographics, medications, pain and pre-injury substance use, mental health and health service utilization. Parent participants also completed a separate interview conducted by a trained RA at baseline. Adolescent participants were then followed for 12 months and completed follow-up outcome assessments by telephone at 2 months, 5 months and 12 months after the date of their injury.
Measures
Prescription Opioid Use
At the baseline interview, the RA asked each adolescent participant to list their pre-injury medications for the year prior to the injury hospitalization. At the baseline parent interview, the RA asked parents to independently describe adolescent pre-injury medication use. At each follow-up outcome assessment, the RA asked adolescent participants to list medications with associated doses and intervals taken since the last interview. All prescription opioids listed (e.g., codeine, hydrocodone, oxycodone, morphine, hydromorphone, and methadone) at each time point were collapsed into a single category of ‘prescription opioid use,’ and categorized as ‘yes’ or ‘no’ for each participant based off of the adolescent self-report for each time point.
Demographics
Patient age, gender, race and ethnicity were obtained through self-report from the adolescent in the baseline survey.
Baseline Clinical Variables
The number of days after injury at which the participant completed the baseline survey was documented. At the baseline assessment, current pain was assessed using the McGill short form pain scale.[18] Specifically, adolescent participants were asked to rate the severity of their current pain as ‘none’, ‘mild’, ‘moderate’ or ‘severe’ for each of fifteen different pain descriptors (e.g., throbbing, tender). Each rating corresponded to a numeric value from 0–3. The total score for each participant ranged from 0–45.
Chart Review Clinical Variables
A discharge diagnosis from the index injury hospital visit and the presence or absence of intensive care unit (ICU) level of care was determined by reviewing hospital records and using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes.[19] From the ICD-9-CM codes, an Injury Severity Score (ISS) was calculated.[20] The number of previous traumas requiring hospital admission was abstracted from the trauma registry or electronic medical record by reviewing hospital records.
Substance Use
Pre-injury alcohol abuse and dependence was assessed using the Composite International Diagnostic Index (CIDI).[21] The Alcohol Use Disorders Identification Test – Consumption (AUDIT-C) [22] was used to identify participants with problem drinking. Illicit drug use, including marijuana, cocaine, methamphetamine and opiates (e.g., heroin), were all assessed with single-item questions assessing any use (yes/no) within the year before the injury. Single item drug screens have been used before in trauma center settings,[23] and have established reliability and validity when used in general medical settings.[24] The frequency of heroin, cocaine, amphetamines or other illicit drugs was low and thus a category of ‘other drug use’ was created and collapsed into any use (yes/no) at each time point.
Mental Health
Depressive symptoms since the injury were assessed using the 9-item Patient Health Questionnaire (PHQ-9) [25] during the initial baseline interview. The PHQ-9 has established reliability and validity for the assessment of depressive symptoms in adolescents.[26]
Analysis
First, the representativeness of the population was assessed by comparing the study population to all eligible trauma patients admitted to the study site during the study time frame. Next, the frequency of prescription opioid use at each time point was determined for the study population. The frequency of parent-reported adolescent prescription opioid use in the year prior to the injury was also determined. The concordance of these answers at the baseline interview was calculated along with a kappa value to assess the degree of agreement between adolescents and parents for adolescent prescription opioid use in the year prior to the trauma injury admission.
To examine predictors of longitudinal prescription opioid use over the 12 months after the index injury hospital admission, the association between prescription opioid use and demographics, clinical characteristics, mental health and pre-injury substance use were examined using a generalized linear mixed-model Poisson regression analysis, in which the dependent variable was a repeated measurement of prescription opioid use. Specifically, the repeated measure included prescription opioid use measured pre-injury, at 2-months, 5-months and 12-months. Univariate analyses were completed in order to determine the unadjusted risk of the dependent variable associated with each predictor variable. Specific predictors assessed included each time point, age, gender, race, pre-injury substance use, baseline depression, baseline pain, ISS and ICU stay. Predictor variables with p < 0.15 in the univariate or unadjusted analysis were entered into an adjusted, multivariate model.[27] Individual variables were removed using backwards elimination, excluding the variable with the highest p value first. Once all variables with p > 0.05 had been removed, the remaining significant variables and each time point were entered to create a final model. SAS version 9.2 (SAS Institute Inc), and SPSS, version 18.0 (SPSS Inc) were used for all analyses.
Results
Over the study time period, 120 adolescents were recruited and enrolled into the study. There were no differences in age, sex or ISS between patients enrolled in the study and eligible adolescents not enrolled in the study that presented for care during the study time frame. The mean age of study participants was 15.5 years (standard deviation (SD) 1.9), 75% (n=90) were male and 61.7% (n=74) were Caucasian. Almost half of the sample (47.1%, n=56) stayed in the ICU, the mean ISS was 15.7 (SD 11.3) and 46.2% (n=55) had an ISS ≥ 16 indicating major trauma. Follow up completion rates over time were 98% (n=118) at 2-months, 99% (n=119) at 5-months and 98% (n=118) at 12-months. There was no difference in follow-up rates between the intervention and enhanced usual care (EUC) arms of the study. Descriptive statistics for all demographics, clinical variables, and pre-injury mental health and substance use for the sample are depicted in Table 1.
Table 1.
Baseline adolescent characteristics (n=120)
| Characteristic | %/M(SD) |
|---|---|
| Age Mean(SD) | 15.5 (1.9) |
| Female | 25.0 |
| Caucasian race | 61.7 |
| Number of previous traumas Mean(SD) | 2.0 (1.6) |
| AUDIT-C score for problem drinking Mean(SD) | 1.4 (2.5) |
| Past-year pre-injury marijuana use | 35.8 |
| Past-year pre-injury other drug use | 3.3 |
| PHQ-9 score for depression Mean(SD) | 7.1 (5.3) |
| McGill Pain score Mean(SD) | 8.7 (9.0) |
| Injury Severity Score Mean(SD) | 15.7 (11.3) |
| ICU stay | 47.1 |
| Intentional injury | 5.8 |
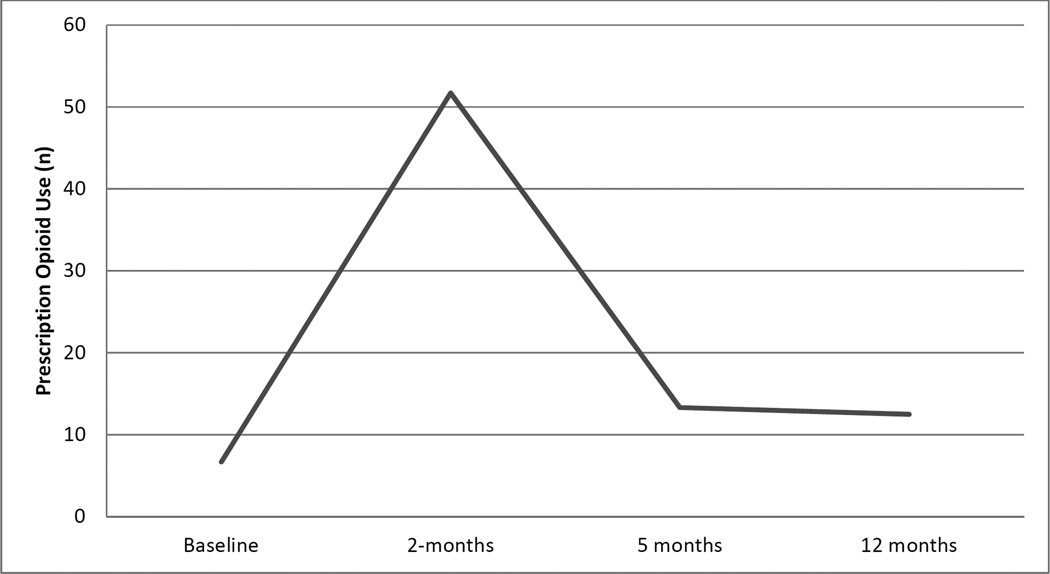
At baseline, 6.8% of the sample (n=8) reported any prescription opioid use during the 12 months prior to their injury. In over 92% (n=108) of cases, parents and adolescents concurred that adolescent patients were not using pre-injury opioid medications. In 5% of cases (n=6), adolescents reported pre-injury prescription opioid use while parents reported no use (kappa 0.34). Among these six patients, five reported marijuana use, two had other drug use and all six had used alcohol in the 12 months prior to their injury. Over half the sample (51.7%, n=62) reported prescription opioid use at the 2-month follow-up while 13.3% (n=16) and 12.5% (n=15) reported prescription opioid use at the 5-month and 12-month follow-up respectively (Figure 1).
Figure 1.
Prescription opioid use over time among adolescents admitted to the hospital for injury (n=120).
The unadjusted analysis is presented in Table 2. Age was statistically significant, with increasing age predicting increased risk of prescription opioid use over time (RR 1.11, 95% CI 1.00–1.23). All other demographics including race and gender were not significant. Previous history of trauma, current ISS, and ICU stay were not statistically significant predictors of prescription opioid use. Pain score at baseline was associated with increased risk of prescription opioid use over time (RR 1.02, 95% CI 1.01–1.04). All pre-injury substance use variables including marijuana use, other drug use and problem drinking as measured by the AUDIT-C were each was positively associated with prescription drug use over time and the baseline PHQ-9 score for depression at the time of the injury was associated with prescription opioid use over time (RR 1.03, 95% CI 1.00–1.07).
Table 2.
Univariate mixed Poisson regression predicting prescription opioid use over time
| Variable | RR (95% CI) |
|---|---|
| Intervention condition | 1.05 (0.71–1.55) |
| Time | |
| Baseline | reference |
| 2 months | 8.00 (4.19–15.35) |
| 5 months | 2.02 (0.93–4.39) |
| 12 months | 1.92 (0.84–4.38) |
| Age | 1.11 (1.00–1.23) |
| Gender, Female | 0.97 (0.60–1.57) |
| Race | |
| White | reference |
| Hispanic | 0.79 (0.31–2.03) |
| Black | 1.03 (0.51–2.07) |
| Asian | 0.53 (0.22–1.32 |
| American Indian | 0.88 (0.50–1.53) |
| Previous trauma | 1.06 (0.94–1.20) |
| Unintentional injury | 1.08 (0.44–2.65) |
| Baseline AUDIT-C score | 1.09 (1.03–1.15) |
| Marijuana use at baseline | 2.08 (1.44–3.00) |
| Other drug use at baseline | 2.10 (1.53–2.89) |
| Baseline PHQ-9 score | 1.03 (1.00–1.07) |
| Baseline McGill Pain score | 1.02 (1.01–1.04) |
| Injury Severity Score | 1.01 (0.99–1.02) |
| ICU admission | 0.91 (0.62–1.35) |
RR = Relative Risk
In the final mixed model regression analysis (Table 3) time was independently associated with prescription opioid use. Additionally, any pre-injury marijuana use (RR 1.69, 95% CI 1.09–2.61) and baseline pain score (RR 1.02,95% CI 1.00–1.03) were both independent predictors of prescription opioid use over time. ISS did not independently predict prescription opioid use (RR 1.00, 95% CI 0.99–1.02) in this adjusted model.
Table 3.
Multivariate Poisson regression analysis predicting longitudinal prescription opioid use over time
| Variable | Relative Risk |
95% Confidence Interval |
|---|---|---|
| Time | ||
| Baseline | reference | reference |
| 2 month | 12.05 | 5.18, 28.00 |
| 5 month | 3.22 | 1.30, 7.98 |
| 12 month | 3.08 | 1.17, 8.10 |
| Age | 1.04 | 0.92, 1.17 |
| Gender (female) | 0.98 | 0.63, 1.53 |
| Injury Severity Scale (ISS) | 1.00 | 0.99, 1.02 |
| Marijuana use (pre-injury) | 1.69 | 1.09, 2.61 |
| Pain score at baseline | 1.02 | 1.00, 1.03 |
Discussion
Overall, 13.3% of adolescent patients admitted to the hospital after an injury from a trauma were taking prescribed opioids five months after their admission and 12.5% of adolescent patients admitted to this hospital after an injury were still taking prescribed opioids one year after their trauma admission. While previous studies have documented trajectories of opioid use after acute pain in adults, this is the first investigation to document sustained prescription opioid use after an admission for trauma in adolescents. After controlling for multiple factors, pre-injury marijuana use and baseline pain were both predictors of sustained prescription opioid use over time.
In previous studies, 6% of adults admitted for surgery reported prescription opioid use six months after surgery,[10] and opiate-naïve adults discharged from the ED with an opioid prescription were nearly twice as likely to require additional opioid prescriptions within sixty days compared to those discharged from the ED without an opioid prescription.[6] The rate of controlled substance prescriptions for adolescents has increased dramatically over the past several years.[1] Treating acute pain is important and guidelines exist for the treatment of pain in pediatric patients that have experienced trauma. These guidelines specifically note that opioids are indicated for moderate to severe pain associated with acute trauma, and that early pain management is important.[28] However, in adolescents, prescribed opioids are often a source of nonmedical prescription opioid use [2, 3] and thus prudent and appropriate prescribing is important in this population.
Currently, opioids are not recommended for chronic non-cancer pain and practitioners should consider other treatment modalities for chronic pain especially in populations with high risk for misuse.[29] Chronic or sustained prescription opioid use has known health risks and chronic pain is often associated with medical and psychiatric comorbidities.[13] Chronic opioid use is associated with mental health disorders [11, 30] and substance use.[12] If providers are able to identify patients at-risk for sustained prescription opioid use after an injury, these patients can be closely monitored for appropriate use of opioids. Specifically, patients at risk for prescription opioid use could benefit from care management or collaborative care protocols initiated at the time of injury focused on linkage to appropriate outpatient physicians such as primary care and subspecialty pain services. Coordination of care by acute care providers with primary care providers could help guide pain management, patient expectations and evaluation by subspecialists as indicated.
In our study, injured adolescents who reported marijuana use prior to their injury had increased risk of sustained prescription opioid use. Marijuana is currently the most commonly used illicit substance among adolescents [31] and in this population, risk behaviors such as drug use and injury tend to co-occur.[32, 33] Additionally, marijuana use in this age group is associated with increased risk of polysubstance use, including misuse of prescription drugs.[8, 34] Based on our findings, screening for marijuana use at the time of injury admission could identify patients at risk for sustained prescription opioid use. Currently, the American College of Surgeons mandates universal alcohol screening and intervention for all patients admitted for injuries at Level I and Level II trauma centers.[35] Our results suggest that similar screening for drug use in trauma patients would not only assist physicians in identifying patients with substance abuse problems, but also may identify adolescents at-risk for sustained prescription opioid use. Moreover, while brief intervention for drug use has not shown effectiveness in adult outpatient populations,[36, 37] brief intervention for marijuana use in adolescents in primary care has shown promise.[38]
Interestingly, participants’ pain scores during the baseline interview (i.e., baseline pain) predicted sustained opioid use even after controlling for ISS. This finding suggests that perception of pain is more important than injury severity in predicting sustained prescription opioid use over time among this population. Among adolescents, it is possible that baseline pain scores could be related to coping and other pre-injury factors such as mental health. In the univariate analysis, there was increased risk of sustained prescription opioid use over time among patients with current depressive symptoms at the baseline interview suggesting that a component of baseline pain could be related to mental health comorbidity.
Although approximately half of our sample was admitted to the ICU (47%) and had an Injury Severity Score (ISS) of over 15 (46%), indicating major trauma, neither ISS nor ICU stays were predictive of longitudinal prescription opioid use after adjusting for other factors. In previous studies, pain catastrophizing has been associated with continued opioid use after an episode of acute pain or surgery,[39, 40] suggesting the presence of psychosocial pre-injury factors that play an important role in the perception of acute pain which may contribute to chronic pain and sustained prescription opioid use.
While this investigation provides novel information regarding predictors of sustained prescription opioid use among adolescents admitted for an injury related to trauma, there are some important limitations. First, this was a single-site study done at an urban, academic level I trauma center and the results may not be generalizable to other settings. This was a secondary data analysis of a randomized control trial and not a cohort design. However, study arm was accounted for in the analysis and was not statistically significant in the model. Prescription opioid use was determined using self-reported data on medications prescribed to the patient, and did not capture number of pills dispensed nor the location the prescription was written for (e.g., outpatient office, ED). Additionally, this self-report measure did not capture use of prescription opioids for pain if the opioids were prescribed to someone else. Parents were not surveyed about adolescent participant prescription opioid use at 2-month and 5-month time points and thus the self-reported data is derived from adolescent survey responses. While the kappa was modest, the concordance for no prescription opioid use was high at over 90%. Additionally, the motivation for prescription opioid use (e.g., pain, to get high) was not assessed and therefore identifying prescription opioid misuse was outside the scope of this investigation. The medical diagnosis for which the opioids were prescribed was not collected, and thus it is unknown if the participant developed chronic pain from their injuries. Likewise pre-injury pain scores were not collected, so it is unknown if participants had chronic pain at baseline. Further investigation regarding the health condition requiring opioid use, and adolescent use of health services to obtain prescription opioids, is needed. All variables were obtained through self-report including substance use and therefore it is possible that respondents underestimated or under-reported their pre-injury use of illegal drugs. Lastly, the sample size was limited. Therefore it is possible that we were unable to detect significance of some predictor variables due to the sample size. However the 98% follow-up rate over time and associated lack of missing data strengthens the validity of the conclusions and findings, and this sample remains the largest to date investigating longitudinal prescription opioid use in an acutely injured adolescent population.
In conclusion, one in eight adolescents reported sustained prescription opioid use one year after admission for trauma. Pre-injury marijuana use and baseline pain score predicted sustained prescription opioid use over time in this population. The dangers and health risks of chronic opioid therapy are well documented, and this investigation provides valuable information regarding predictors of sustained prescription opioid use after a hospital admission for trauma in adolescents. Physicians should consider risk for sustained prescription opioid use at the time of injury and work with patients and families to determine an appropriate pain management plan for each patient irrespective of injury severity. Screening for substance use including marijuana at the time of injury could help identify patients at risk for both substance use problems and sustained prescription opioid use after injury. Future investigations could focus on describing reasons for continued opioid therapy as well as characterizing prescribing patterns and pain management plans for adolescents after injury. Additionally, future work could include working with patients and families in the hospital for patient-centered pain approaches that take into account substance use and other comorbidity.
Acknowledgements
This work was supported by the Health Resources and Services Administration Grant H34/MC08508-01-00 and the National Institute of Mental Health Grant K24/MH086814 (Dr. Zatzick) as well as a NIDA-EMF Career Development Grant (Dr. Whiteside).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This work was presented by Dr. Whiteside as a poster at the Society for Academic Emergency Medicine national meeting in Dallas, TX, May 2014.
Conflict of Interest: None
References
- 1.Fortuna RJ, Robbins BW, Caiola E, et al. Prescribing of controlled medications to adolescents and young adults in the united states. Pediatrics. 2010;126:1108–1116. doi: 10.1542/peds.2010-0791. [DOI] [PubMed] [Google Scholar]
- 2.McCabe SE, Boyd CJ, Young A. Medical and nonmedical use of prescription drugs among secondary school students. J Adolesc Health. 2007;40:76–83. doi: 10.1016/j.jadohealth.2006.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCabe SE, West BT, Cranford JA, et al. Medical misuse of controlled medications among adolescents. Arch Pediatr Adolesc Med. 2011;165:729–735. doi: 10.1001/archpediatrics.2011.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300:2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- 5.Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. Journal of Pain. 2009;10:113–130. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoppe JA, Kim H, Heard K. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med. 2014 doi: 10.1016/j.annemergmed.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 7.McCabe SE, West BT, Teter CJ, et al. Medical and nonmedical use of prescription opioids among high school seniors in the united states. Arch Pediatr Adolesc Med. 2012;166:797–802. doi: 10.1001/archpediatrics.2012.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whiteside LK, Walton MA, Bohnert AS, et al. Nonmedical prescription opioid and sedative use among adolescents in the emergency department. Pediatrics. 2013;132:825–832. doi: 10.1542/peds.2013-0721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Connelly M, Fulmer RD, Prohaska J, et al. Predictors of postoperative pain trajectories in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2014;39:E174–E181. doi: 10.1097/BRS.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 10.Carroll I, Barelka P, Wang CKM, et al. A pilot cohort study of the determinants of longitudinal opioid use after surgery. Anesthesia and Analgesia. 2012;115:694–702. doi: 10.1213/ANE.0b013e31825c049f. [DOI] [PubMed] [Google Scholar]
- 11.Richardson LP, Russo JE, Katon W, et al. Mental health disorders and long-term opioid use among adolescents and young adults with chronic pain. J Adolesc Health. 2012;50:553–558. doi: 10.1016/j.jadohealth.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edlund MJ, Martin BC, Fan MY, et al. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: Results from the troup study. Drug Alcohol Depend. 2010;112:90–98. doi: 10.1016/j.drugalcdep.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ballantyne JC, Shin NS. Efficacy of opioids for chronic pain: A review of the evidence. Clin J Pain. 2008;24:469–478. doi: 10.1097/AJP.0b013e31816b2f26. [DOI] [PubMed] [Google Scholar]
- 14.Ziv A, Boulet JR, Slap GB. Emergency department utilization by adolescents in the united states. Pediatrics. 1998;101:987–994. doi: 10.1542/peds.101.6.987. [DOI] [PubMed] [Google Scholar]
- 15.Owens PL, Zodet MW, Berdahl T, et al. Annual report on health care for children and youth in the united states: Focus on injury-related emergency department utilization and expenditures. Ambul Pediatr. 2008;8:219–240. e217. doi: 10.1016/j.ambp.2008.03.032. [DOI] [PubMed] [Google Scholar]
- 16.Zatzick D, Russo J, Lord SP, et al. Collaborative care intervention targeting violence risk behaviors, substance use, and posttraumatic stress and depressive symptoms in injured adolescents: A randomized clinical trial. JAMA Pediatr. 2014;168:532–539. doi: 10.1001/jamapediatrics.2013.4784. [DOI] [PubMed] [Google Scholar]
- 17.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 18.Melzack R, Katz J. Handbook of pain assessment. 2nd 'edition'. New York, NY: Guilford Press; 2001. [Google Scholar]
- 19.Public Helath Service and Health Care Financing Administration. International classification of diseases, 9th revision, clinical modification. 6th Edition. Washington, DC: Public Health Service; 1998. 'edition'. [Google Scholar]
- 20.Johns Hopkins Health Services Research and Development Center. Determining injury severity from hospital discharges: A program to map icd-9-cm diagnoses into ais and iss severity scores. Baltimore: The Johns Hopkins University Pres; 1989. [Google Scholar]
- 21.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of dsm-iv disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 22.Bradley KA, DeBenedetti AF, Volk RJ, et al. Audit-c as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31:1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- 23.Zatzick D, Donovan D, Dunn C, et al. Substance use and ptsd symptoms in trauma center patients receiving mandated alcohol sbi. J Subst Abuse Treat. 2012 doi: 10.1016/j.jsat.2012.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith PC, Schmidt SM, Allensworth-Davies D, et al. A single-question screening test for drug use in primary care. Arch Intern Med. 2010;170:1155–1160. doi: 10.1001/archinternmed.2010.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JB. The phq-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richardson LP, McCauley E, Grossman DC, et al. Evaluation of the patient health questionnaire-9 item for detecting major depression among adolescents. Pediatrics. 2010;126:1117–1123. doi: 10.1542/peds.2010-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd 'edition'. New York: John Wiley & Sons; 2000. [Google Scholar]
- 28.American Academy of Pediatrics. Committee on Psychosocial Aspects of C, Family H, Task Force on Pain in Infants, C, et al. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics. 2001;108:793–797. doi: 10.1542/peds.108.3.793. [DOI] [PubMed] [Google Scholar]
- 29.Schechter NL. Pediatric pain management and opioids: The baby and the bathwater. JAMA Pediatr. 2014;168:987–988. doi: 10.1001/jamapediatrics.2014.1441. [DOI] [PubMed] [Google Scholar]
- 30.Becker WC, Sullivan LE, Tetrault JM, et al. Non-medical use, abuse and dependence on prescription opioids among u.S. Adults: Psychiatric, medical and substance use correlates. Drug Alcohol Depend. 2008;94:38–47. doi: 10.1016/j.drugalcdep.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 31.Johnston LD, O'Malley PM, Miech R, et al. Monitoring the future national results on adolescents drug use: 1975–2013 overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Resarch, The University of Michigan; 2014. [Google Scholar]
- 32.Dukarm CP, Byrd RS, Auinger P, et al. Illicit substance use, gender, and the risk of violent behavior among adolescents. Arch Pediatr Adolesc Med. 1996;150:797–801. doi: 10.1001/archpedi.1996.02170330023004. [DOI] [PubMed] [Google Scholar]
- 33.Jessor R. Risk behavior in adolescence: A psychosocial framework for understanding and action. J Adolesc Health. 1991;12:597–605. doi: 10.1016/1054-139x(91)90007-k. [DOI] [PubMed] [Google Scholar]
- 34.Whiteside LK, Cunningham RM, Bonar EE, et al. Nonmedical prescription stimulant use among youth in the emergency department: Prevalence, severity and correlates. J Subst Abuse Treat. 2014 doi: 10.1016/j.jsat.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.American College of Surgeons USDoHaHS, Department of Transportation. Alcohol screening and brief intervention (sbi) for trauma patients: Cot quick guide. Chicago: 2010. [Google Scholar]
- 36.Roy-Byrne P, Bumgardner K, Krupski A, et al. Brief intervention for problem drug use in safety-net primary care settings: A randomized clinical trial. JAMA. 2014;312:492–501. doi: 10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bogenschutz MP, Donovan DM, Mandler RN, et al. Brief intervention for patients with problematic drug use presenting in emergency departments: A randomized clinical trial. JAMA Intern Med. 2014 doi: 10.1001/jamainternmed.2014.4052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walton MA, Bohnert K, Resko S, et al. Computer and therapist based brief interventions among cannabis-using adolescents presenting to primary care: One year outcomes. Drug Alcohol Depend. 2013;132:646–653. doi: 10.1016/j.drugalcdep.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Helmerhorst GT, Vranceanu AM, Vrahas M, et al. Risk factors for continued opioid use one to two months after surgery for musculoskeletal trauma. J Bone Joint Surg Am. 2014;96:495–499. doi: 10.2106/JBJS.L.01406. [DOI] [PubMed] [Google Scholar]
- 40.Parr JJ, Borsa PA, Fillingim RB, et al. Pain-related fear and catastrophizing predict pain intensity and disability independently using an induced muscle injury model. J Pain. 2012;13:370–378. doi: 10.1016/j.jpain.2011.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]