Abstract
Objective
Bruising can indicate abuse for infants. Bruise prevalence among infants in the Pediatric Emergency Department (PED) setting is unknown. Our objective was to determine prevalence of bruising, associated chief complaints (CC), and frequency of abuse evaluations in previously healthy infants presenting to PEDs.
Methods
We conducted a prospective, observational, multi-center study of infants ≤12 months old presenting to PEDs. Structured sampling was utilized. Pediatric Emergency Medicine (PEM) clinicians performed complete skin examinations to screen for bruising. Study investigators documented skin findings, date of visit, patient's age, CC, and abuse evaluation. The primary outcome was prevalence of bruising. Secondary outcomes were prevalence of bruising based on CC and frequency of abuse evaluation. Point estimates of bruise prevalence and differences in bruise prevalence between patient subgroups were calculated with 95% confidence intervals (CI).
Results
Bruising was identified in 88 of 2488 infants (3.5%, 95% CI: [2.9%, 4.4%]). Rates of bruising for infants ≤5 and >5 months old were 1.3% and 6.4%, respectively (difference 5.1%, 95% CI: [3.6%, 6.8%]). For infants ≤5 months old, 83% of bruising was associated with a trauma CC and only 0.2% of infants presenting with a medical CC had bruising. PEM clinicians obtained abuse evaluations on 23% of infants with bruising and that rate increased to 50% for infants ≤ 5 months of age.
Conclusions
Bruising prevalence in children ≤ 12 months of age evaluated in PEDs was low, increased within age strata, and was most often associated with a trauma CC. Most bruised infants did not undergo an abuse evaluation.
BACKGROUND
Bruising in infancy is a red flag for physical abuse, leading to recommendations to evaluate young infants with unexplained bruising for abuse.1-7 This cautious approach is necessary because physical child abuse is a major cause of morbidity and mortality in the first year of life. Bruising is the most common initial injury from physical abuse but is often overlooked.1,8,9
Importance
Before a finding such as infant bruising can serve as a marker for serious disease or as a trigger for further evaluation, knowledge of its prevalence in the targeted population is critical. To our knowledge, no prior study has reported the prevalence of bruising among infants in the Pediatric Emergency Department (PED) setting or the rate of abuse evaluations for infants with bruising. Current published prevalence data come from well-child care clinics, general emergency department (ED) visits that excluded trauma and suspected abuse patients, and from abuse clinics.2,3,10,11 These data may not apply to PED settings where patients with a full spectrum of medical, surgical, traumatic, and social complaints are examined.
Goals
Our primary objective was to determine the prevalence of bruising in the first year of life in previously healthy infants presenting to PEDs. We also sought to determine the prevalence of bruising by age and chief complaint (CC) and the frequency of child abuse evaluations of infants with bruising. Our goal was to establish normative data to inform future guidelines for the evaluation of abuse in infants with bruising.
METHODS
Study design and setting
We conducted this prospective observational study of bruise prevalence among infants ≤12 months of age in the PEDs of three free-standing, tertiary care children's hospitals designated as Level I trauma centers with Child Abuse Pediatricians on staff. These three PEDs collectively evaluate approximately 31,000 patients ≤12 months of age each year. We gathered prevalence data as part of a larger ongoing study to validate a previously derived bruising clinical decision rule (BCDR).12 We obtained the prevalence data in order to determine expected frequency of bruising in this young age group and to identify consecutive cases of infants with bruises. Each hospital's Institutional Review Board granted a waiver of authorization for collection of bruise prevalence information.
Participant Selection
Patients met inclusion criteria if they were 0-12 months of age, presented to the PED for care during a research shift (defined below), and had none of the following exclusion criteria: specific referral for abuse and neglect concern, known coagulation abnormalities, severe neurological and neuromuscular impairment, or severe extensive skin disorders (e.g. severe eczema). These conditions can impact bruise prevalence or interfere with the interpretation of skin findings.
Research shifts
We used a structured sampling approach with research shifts as a feasible proxy to consecutive enrollment. 13 Cost and labor prohibited consecutive and overnight (1 AM to 7 AM) enrollment. We chose research shifts, with start and end times, to minimize potential bias in data collection and increase accuracy of the prevalence estimates. Shifts represented all days of the week between the hours of 7 AM and 1 AM in 4-, 6-, or 8-hour intervals. We investigated post hoc the lack of overnight enrollment utilizing three approaches: PED arrival times for all infants per hospital census, PED arrival times of an abuse population from our BCDR validation study, and surveillance of infants during 9 overnight shifts. These data, collected outside of the study enrollment timeframe, do not appear among the main study results but provide information on the overnight infant population.
Study investigators and skin screening examiners
The study investigator team performed data collection and included PEM-based research assistants and PEM attending physicians, PEM fellows, and social workers who did not provide clinical care during the research shift. The principal investigator conducted training sessions on the study protocol with all study investigators. Skin screening examiners were the treating PEM clinicians who performed complete skin examinations to screen for bruising. This group included PEM attendings, PEM fellows, clinical staff physicians, nurse practitioners, and residents – all familiar with the appearance and diagnosis of a bruise. During each research shift, a study investigator identified all age-appropriate patients from the patient tracking board, confirmed with the screening examiner that the patient met inclusion criteria, and reminded the screening examiner that the patient required a complete skin examination. Skin screening examinations occurred during the course of clinical care.
Methods and measurements
We defined bruises as bleeding beneath intact skin and included hues of red, blue, yellow, green and brown.14 Infants were placed in gowns or undressed for examination. The study investigators verified if the screening examiner had performed a complete skin examination and collected the following data: presence of bruising, date of visit, patient's age in months, CC, and occurrence of abuse evaluation. We defined abuse evaluation as PEM clinician obtaining consultation from the hospital's Child Protection Team or hospital-based social worker to evaluate for possible abuse or submission of a report of suspected child abuse or neglect to a child protection agency.
Only skin findings from patients with a confirmed complete skin assessment were included in the study. Patients discharged prior to complete skin assessments were categorized as having “incomplete skin assessments” and were excluded from analysis. We conducted a sensitivity analysis of the effect of data missing because of “incomplete skin assessments” on estimates of prevalence.
For data analysis, patients were divided into age groups corresponding to mobility stages: 0-2 months (non-mobile); 3-5 months (able to roll and transitioning to sitting without support), 6-8 months (starting to crawl, pulling to stand), and 9-12 months (transitioning from cruising to ambulation).15 We enrolled patients from all age groups until we reached a minimum of 400 patients in each age group. This sample size achieved a 95% confidence interval width of 3% (0.9% - 4.0%) around a published prevalence of 2% for infants in the well-child care setting.3 We defined pre-mobile as inability to crawl, cruise, or walk corresponding to infants aged 0 through 5 months.
We categorized patients by presenting CC: 1) trauma, if the purpose of the PED visit was for the evaluation of an injury occurrence such as a fall from a bed or caregiver's arms; 2) medical, if the visit was related to a sign or symptom of illness such as cough, fever, or vomiting; or 3) abuse and neglect referral, if a patient presented with a specific referral or request for evaluation for possible abuse or neglect.
Outcomes
Our primary outcome was the prevalence of bruising among infants presenting to the PED. Secondary outcomes included the associated CC and frequency of abuse evaluations among bruised infants presenting with trauma and medical CCs.
Analysis
We calculated point estimates of bruise prevalence with 95% confidence intervals (CI) calculated by the Wilson score method in the entire study population, age groups, CC categories, and patients evaluated for abuse.16 We used the Wilson-Newcombe method to calculate 95% CI for differences in prevalence between groups.17 We compared the median age of children with and without bruising with the Wilcoxon rank sum test. We analyzed the data in the open source R software environment (R Core Team (2014). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/).
RESULTS
Characteristics of subjects
From December 2011 to February 2013, we conducted 396 research shifts providing approximately 2200 enrollment hours. Fifty-eight percent of enrollment hours occurred between 7 AM and 3 PM, 42% between 3 PM and 11 PM, and <1% between 11 PM and 1 AM. Most shifts (85%) occurred between Monday 7 AM and Friday 3 PM, and 15% occurred between Friday 3 PM and Monday 7 AM. During research shifts, 2773 infants 0-12 months of age presented to the PEDs. Of these, 127 met exclusion criteria, 147 had incomplete skin assessments, and 11 presented with abuse and neglect referral CCs. The remaining 2488 patients constituted the study sample.
Main results
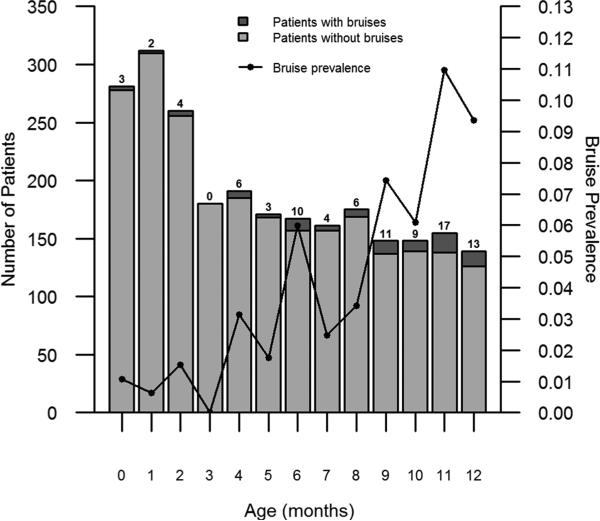
Bruising was present in 88 of the 2488 infants (3.5%, 95% CI: [2.9%, 4.4%]) and prevalence increased with age (Figure 1). The median age of the study population was 5 months (interquartile range 2-8 months). The median age of infants with bruising was more than double the age of those without bruising (9 vs. 4 months). The prevalence of bruising for infants ≤ 5 months and > 5 months of age was 1.3% and 6.4%, respectively (difference 5.1%, 95% CI: [3.6%, 6.8%]). Bruise prevalence varied by study site (6.2% at Rady Children's, 4.4% at Lurie Children's, and 2.6% at Cincinnati Children's).
Figure 1.
Number of patients with and without bruises and bruise prevalence by patient's age (in months)
Most CCs were medical (90%), followed by trauma (8%), and not documented (2%) (Table 1). Among the 88 infants with bruising, the majority (67%) presented with a trauma CC. However, 69% of infants with a trauma CC lacked bruising. Pre-mobile infants rarely had bruises (18/1395; 1.3%), and the majority (15/18; 83%) of those with bruises had a trauma CC (Table 1). Pre-mobile infants with medical CCs were rarely bruised (3/1294; 0.2%). The exclusion of the 11 patients with abuse and neglect referral CCs, two of whom had bruises, did not substantially change the bruise prevalence rate, which would have been 90 of 2499 infants (3.6%, 95% CI: [2.9%, 4.4%]).
Table 1.
Presence of bruising by age group and chief complaint.
| Patient Group | 0-2 mo | 3-5 mo | 6-8 mo | 9-12 mo | Total |
|---|---|---|---|---|---|
| Total patients |
1.0% [0.6%, 2.0%]
(9/853) |
1.8% [1.0%, 3.4%]
9/542 |
4.2% [2.7%, 6.3%]
20/503 |
8.4% [6.4%, 11.0%]
50/590 |
3.5% [2.9%, 4.4%]
(88/2488) |
| Trauma CCs | 18.2% (8/44) |
23.3% (7/30) |
26.0% (13/50) |
44.9% (31/69) |
30.6% [24.5%, 37.4%] (59/193) |
| Medical CCs | 0.0% (1/788) |
0.0% (2/506) |
1.6% (7/438) |
3.7% (19/512) |
1.3% [0.9%, 1.8%] (29/2244) |
| Not documented CC | 0.0% (0/21) |
0.0% (0/6) |
0.0% (0/15) |
0.0% (0/9) |
0% [0.0%, 7.0%] (0/51) |
Values are estimated prevalence [95% CI] (number bruised/number enrolled)
The 147 excluded patients due to incomplete skin assessments were similar in age to patients with documented skin examinations (median, 5 months for each group). They were less likely to have been from Rady Children's (0.7% vs. 6.5%; 95% CI for difference: [2.6%, 9.0%]) and to have had a trauma CC (2.0% vs. 7.7%; 95% CI for difference: [1.7%, 9.6%]).
Abuse evaluations occurred in 38 infants (1.5%) and were more frequent when bruising was present: 23% (20/88) of bruised vs. 0.8% (18/2400) of unbruised infants (difference 22%, 95% CI: [12-32%]). The abuse evaluation rate was highest (50%; [9/18]) among pre-mobile bruised infants. Fourteen (70%) of the 20 CCs of bruised children evaluated for abuse were trauma and six (30%) were medical. These numbers exclude patients referred explicitly for abuse and neglect CC concerns.
Post hoc analysis of overnight hours
By PED census, only 11.5% (6707/58171, 95% CI: [11.2%, 11.8%]) of infant visits occurred overnight, despite these hours occupying 29% of the 24-hour interval. The proportion of trauma CCs during the overnight hours (189/6707; 2.8%, 95% CI: [2.4%, 3.2%]) was slightly lower than during the day/evening hours (1801/51,470; 3.5%, 95% CI: [3.3%, 3.7%]; 95% CI for the difference: [0.2%, 1.1%]). Per the BCDR validation study, the proportion of bruised infants evaluated for abuse who presented to the PED during the overnight hours was lower (14/232; 6.0%, 95% CI: [3.5% - 10.0%]) than the proportion who presented during day/evening enrollment hours. Per overnight surveillance, among the 45 infants 0-12 months of age, none had bruising. The one patient with a trauma CC was the only patient who underwent an evaluation for abuse. Infants in this small overnight sample were less likely to have bruising or be evaluated for abuse as compared to the enrollment day/evening hours.
LIMITATIONS
We enrolled patients in three tertiary center PEDs, excluding patients with severe neurological disabilities and bleeding disorders. Therefore, our results cannot be used to predict the prevalence of bruising among patients presenting to primary care clinics or inpatient services or among those with special health care needs. Data from this study are applicable in general EDs because the infant population of PEDs is likely similar, with the exception of patients with highly specialized needs.
The 147 patients excluded from analysis due to “incomplete skin assessments” may have had characteristics different from those of the study population, and their exclusion may have altered our estimate of prevalence. A sensitivity analysis revealed that bruise prevalence would have ranged from 3.4% if none of the cases with incomplete skin assessments exhibited bruising to 9.0% if all 147 cases had exhibited bruising. If the 147 patients with incomplete skin assessments had exhibited site- and CC- specific bruising consistent with the 2488 patients with complete skin examinations, our prevalence estimate would not have been appreciably different (3.5%, 95% CI: [2.8%, 4.2%]).
The screening examiner may have missed bruises on skin exam, or non-traumatic lesions may have been misidentified as bruises. However, all study sites were Level 1 Pediatric Trauma Centers with examiners experienced in the differentiation of pediatric bruising from other lesions such as birthmarks. We neither measured agreement among screening examiners or study investigators nor provided specific training to standardize recognition of lesions. A second screening examiner did not confirm negative skin exams due to resource and IRB limitations. A study investigator approached all patients identified with bruising by screening examiners for entry into the larger BCDR validation study. All consented patients underwent confirmatory exams by study investigators to confirm the presence of bruising.
We did not record the gender, race, or ethnicity of all screened patients. This limited dataset collected for the prevalence study did not allow us to analyze the effect of gender, race, or ethnicity on bruising prevalence. Previous studies have reported no difference in bruising by gender, while at least one study reported a difference in bruise detection by race.3,10,11 Further research is required to assess the effect race, ethnicity, and skin tone likely have on bruise appearance and prevalence.
The clinical characteristics and legal outcomes of the 88 infants with bruising (with and without evaluations for physical abuse as per PEM clinician discretion) and the two infants with bruising referred specifically for an abuse evaluation were beyond the scope of this study. This strictly observational study reports expected rates of bruising in infants and frequency of abuse evaluations in infants with bruising and does not identify predictors of abuse status.
The structured sampling approach used to simulate consecutive enrollment can potentially introduce distortion in the population being sampled. However, inclusion of all days of the week and different time intervals helped to mitigate distortions. Lack of enrollment during the overnight hours may have introduced bias into the results. We found that infant census was lower during the overnight hours as were trauma CCs and abuse evaluation frequencies as compared to day/evening hours. Since bruises were almost always associated with a trauma CC in this young age group and bruise prevalence is highest among abuse victims, it is possible that our day/evening prevalence slightly overestimated the true bruise prevalence. Therefore, the prevalence rate results likely represent a maximum rate.
DISCUSSION
To our knowledge, this is the first study of bruising prevalence and abuse evaluations among infants in the PED setting, and the largest (n=2488) to investigate bruising prevalence among infants in any clinical setting. We determined that bruising was uncommon, especially in the first 5 months of life (<2%) and, when present, was most often associated with a trauma CC. Abuse evaluations occurred in less than one-quarter of infants with bruising.
Bruise prevalence rates
Published bruise prevalence rates in the first year of life vary widely with rates of 0.6% to 72% depending on the population studied and the inclusion and exclusion criteria applied (Table 2).2,3,9-11 A clinic-based study that excluded suspected abuse patients identified a 0.6% rate of bruising among infants 0-5 months of age.3 A clinic and ED medical visit based study that excluded trauma patients and those with abuse concerns, reported a bruise prevalence of 1.2% among infants 0-8 months of age.10 Our bruise prevalence rates for both these age ranges were approximately double those reported and likely reflect differences in setting and inclusion criteria. 3, 10 Our study was conducted at PEDs designated as Level 1 trauma centers and included trauma patients and patients evaluated for abuse at the discretion of the PEM clinician.
Table 2.
Comparison of our results with published studies
| Age groups (months) | Author | Total patients | Total patients with bruises | Prevalence (%) |
|---|---|---|---|---|
| 0-5 | Pierce/Magana | 1395 | 18 | 1.3 |
| Sugar | 366 | 2 | 0.6 | |
| Harper | 980 | 254 | 25.9 | |
| 0-8 | Pierce/Magana | 1898 | 38 | 2.0 |
| Sugar | 473 | 8 | 1.7 | |
| Labbe | 246 | 3 | 1.2 | |
| 0-11 | Pierce/Magana | 2349 | 75 | 3.2 |
| Sugar | 592 | 31 | 5.2 | |
| Atwal | 18 | 13 | 72 | |
| 6-11 | Pierce/Magana | 954 | 57 | 6.0 |
| Sugar | 226 | 29 | 12.8 | |
| 6-12 | Pierce/Magana | 1093 | 70 | 6.4 |
| Carpenter | 177 | 22 | 12 | |
| Populations | Pierce/Magana | 3 Level I trauma center PEDs | ||
| Sugar | 7 primary care pediatric offices – well child visits | |||
| Harper | 20 child abuse teams – physical abuse consults | |||
| Labbe | Outpatient clinic and medical section of the ED | |||
| Atwal | Forensic pathology – fatal abusive head trauma victims | |||
| Carpenter | Hearing test clinics and child health surveillance clinics | |||
Once infants begin to cruise, they are more likely to bruise. 3 Studies of clinic patients aged 6-12 months yielded prevalences of 12-13%, with increased mobility associated with increased bruising.3,11 Our prevalence rate also increased within age strata but was only half that reported for the 6-12 month olds. The reason for the higher rate of infant bruising in a well-child clinic population compared to a PED population is not clear. However, our oldest patients (11 and 12 months) exhibited a more comparable prevalence rate of 10% (Figure 1).
Studies of high risk and/or abuse populations yielded the highest bruising prevalence rates ranging from 25.9% for children referred to child abuse teams for possible physical abuse to 72% for children who died from abusive head trauma.2,9 The relatively low prevalence of bruising in healthy well-child care and ED visits in the first year of life compared to that among populations referred for or dying from abuse underscores the importance of this seemingly innocuous physical examination finding – the bruise – and indicates such a simple finding can be ominous and requires clinical due diligence.
Bruising and frequency of child abuse evaluations
Bruising often precedes abuse fatalities and near-fatalities in infants and are initially missed as abusive injuries in over one-third of these cases.1,6,9,18,19 Accordingly, child abuse experts and professional organizations recommend strong consideration of abuse evaluations in young pre-mobile infants with bruising not caused by a medical condition. 1-7,20-22 Neither the levels of compliance with these abuse evaluation recommendations nor the rates of abuse evaluations among infants with bruising presenting to the PED setting are known. Our observational study allowed us to assess, but not influence clinical practice, and our results revealed bruising was associated with an increased proportion of patients undergoing an abuse evaluation. Although half of bruised pre-mobile infants were evaluated for abuse, overall, three- quarters of bruised infants were not evaluated. The relatively low rates of abuse evaluations among bruised infants was unexpected given that literature reports bruising in this young age group is a red flag for abuse that warrants further evaluation.1-5,20,21 However, the factors influencing the decision to evaluate for abuse and the outcomes of those evaluations were beyond the scope of this study and will require future study in order to better align clinical practice with recommendations and to implement evidence-driven guidelines specific to the PED setting.
Bruising, age, and associated CC
The prevalence of bruising has been reported to vary by developmental ability in healthy children. Our results were consistent with others who reported higher bruise prevalence in older infants starting to sit on their own or pull to stand.3,10,11,15 Our study found a significant difference in bruise rates for infants ≤5 months as compared to > 5 months of age. After 5 months, the proportion of patients with bruising associated with medical CCs increased 10-fold. These findings further suggest that normal activity should not cause incidental bruising before the infant is mobile.
To our knowledge, prior investigators have not studied the association of CC with bruising. Our study found that bruising prevalence varied significantly by CC category. Trauma CCs represented fewer than 8% of infant PED visits and only 5.3% in the first 5 months of life. However, trauma CC were 8 times more common among bruised infants and 15 times more common among bruised infants ≤5 months of age. The low rates of bruising associated with medical CC visits (1.3% of all visits and only 0.2% of visits in the first 5 months of life) support the notion that bruising on a pre-mobile infant should be considered an exception, especially in the absence of an adequate injury mechanism. These findings highlight the importance of a complete skin examination and context (injury findings and accompanying history) for seemingly minor injuries such as bruises on young infants.
In our experience, both medical and legal professionals commonly believe that an impact such as from a fall off of the bed should cause bruising. In the legal system, it is often opined that if a bruise is not present, no trauma or impact occurred. The unexpectedly low frequency of bruising among infants presenting with trauma CCs (less than one-third) in our study contradicts this commonly held belief. Our finding further highlights the importance of bruising in the first year of life and refutes the notion that infants “bruise easily.”
Bruising prevalence and study site
Prevalence of bruising varied significantly among the three study sites and may be attributable to the percentage of African-American patients presenting to each PED. One study reported African-American children had a bruise prevalence rate that was nearly three times lower than Caucasian children.3 Although we did not document race or ethnicity during data collection, the proportion of African-American patients at each institution was known from PED census data. The sites with the highest and lowest proportions of African-American patients had the lowest and highest prevalence rates of bruising, respectively. Further study will be required to determine the impact of skin tone on bruise recognition.
The prevalence of bruising among previously healthy infants evaluated in the PED is low and increases through the first year of life. Bruising is especially uncommon among infants with medical CCs and not expected as an incidental finding before infants are mobile. Therefore, clinicians should regard the bruise as a notable clinical finding worthy of clinical vigilance to elucidate its etiology. Bruising is associated with an increased use of abuse evaluations. The next step in investigation is to study the specific bruise characteristics resulting from abusive and accidental injury as well as the outcomes of the abuse evaluations in the bruised infants to inform future guidelines and practice.
Acknowledgment
The authors acknowledge and thank the research enrollment team at Lurie Children's – Janet Flores, BS; Shelia Hickey, MSW, MJ; Suzanne M. Schmidt, MD; Laura Turner Martinez, BS; and Tara Shenoy, BA – for their efforts in collecting data.
Grant: The research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) of the National Institutes of Health. (R01HD060997; PI: Pierce)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting: This data was presented as a poster at the Ray E. Helfer Society Annual Meeting April 15, 2013, Sonoma, CA.
Conflict of Interest: The authors have no conflicts of interest to disclose.
Author's Contributions Statement: MCP and JNM share joint first authorship. MCP obtained funding. MCP, JNM, KK, DJL, BB, GM designed the study. MCP, KK, BB, JTK supervised the conduct of the study and data was collected by JNM, GM. MCP, JNM, KK, DJL, JTK analyzed and interpreted the data. DJL was responsible for the statistical analysis. MCP and JNM worked on the initial manuscript draft, and all authors contributed to the revisions for the final version. All authors made critical intellectual contributions and approved the final manuscript as submitted. MCP takes responsibility for the paper as a whole.
REFERENCES
- 1.Sheets LK, Leach ME, Koszewski IJ, et al. Sentinel injuries in infants evaluated for child physical abuse. Pediatrics. 2013;131(4):701–707. doi: 10.1542/peds.2012-2780. [DOI] [PubMed] [Google Scholar]
- 2.Harper N, Feldman KW, Sugar NF, et al. Additional Injuries in Young Infants with Concern for Abuse and Apparently Isolated Bruises. J Pediatr. 2013;165(2):383–388. doi: 10.1016/j.jpeds.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Sugar NF, Taylor JA, Feldman KW. Bruises in infants and toddlers: those who don't cruise rarely bruise. Arch Pediatr Adolesc Med. 1999;153(4):399–403. doi: 10.1001/archpedi.153.4.399. [DOI] [PubMed] [Google Scholar]
- 4.Maguire S, Mann M. Systematic reviews of bruising in relation to child abuse – what have we learnt: an overview of review updates. Evid Based Child Health. 2013;8(2):255–263. doi: 10.1002/ebch.1909. [DOI] [PubMed] [Google Scholar]
- 5.Feldman KW. The bruised premobile infant: should you evaluate further? Pediatr Emerg Care. 2009;25(1):37–39. doi: 10.1097/PEC.0b013e318191db15. [DOI] [PubMed] [Google Scholar]
- 6.Pierce MC, Smith S, Kaczor K. Bruising in infants: those with a bruise may be abused. Pediatr Emerg Care. 2009;25:845–847. doi: 10.1097/PEC.0b013e3181c06217. [DOI] [PubMed] [Google Scholar]
- 7.Anderst JD, Carpenter SL, Abshire TC, et al. Evaluation for bleeding disorders in suspected child abuse. Pediatrics. 2013;131(4):e1314–e1322. doi: 10.1542/peds.2013-0195. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children's Bureau [August 18, 2014];Child Maltreatment 2012. 2014 Available at: http://www.acf.hhs.gov/programs/cb/resource/child-maltreatment-2012.
- 9.Atwal GS, Rutty GN, Carter N, et al. Bruising in non-accidental head injured children; a respective study of the prevalence, distribution and pathological associations in 24 cases. Forensic Sci Int. 1998;96:215–230. doi: 10.1016/s0379-0738(98)00126-1. [DOI] [PubMed] [Google Scholar]
- 10.Labbe J, Caouette G. Recent skin injuries in normal children. Pediatrics. 2001;108:271–276. doi: 10.1542/peds.108.2.271. [DOI] [PubMed] [Google Scholar]
- 11.Carpenter RF. The prevalence and distribution of bruising in babies. Arch Dis Child. 1999;80:363–366. doi: 10.1136/adc.80.4.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pierce MC, Kaczor K, Aldridge S, O'Flynn J, Lorenz D. Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics. 2010;125:64–71. doi: 10.1542/peds.2008-3632. [DOI] [PubMed] [Google Scholar]
- 13.Valley MA, Heard KJ, Ginde AA, et al. Observational studies of patients in the emergency department: a comparison of four sampling methods. Ann Emerg Med. 2012;60(2):139–145. doi: 10.1016/j.annemergmed.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaczor K, Pierce MC, Makoroff K, Corey TS. Bruising and physical child abuse. Clin Ped Emerg Med. 2006;7:153–160. [Google Scholar]
- 15.Frankenburg WK, Dodds J, Archer P, et al. The Denver II: a major revision and restandardization of the Denver Developmental Screening Test. Pediatrics. 1992;89(1):91–97. [PubMed] [Google Scholar]
- 16.Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc. 1927;22:209–212. [Google Scholar]
- 17.Newcombe RG. Interval estimation for the difference between independent proportions: comparison of eleven methods. Statist Med. 1998;17:873–890. doi: 10.1002/(sici)1097-0258(19980430)17:8<873::aid-sim779>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 18.Ellaway BA, Payne EH, Rolfe K, et al. Are abused babies protected from further abuse? Arch Dis Child. 2004;89(9):845–846. doi: 10.1136/adc.2003.035493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ingham AI, Langlois NE, Byard RW. The significance of bruising of infants – a forensic postmortem study. Arch Dis Child. 2011;96:218–220. doi: 10.1136/adc.2009.177469. [DOI] [PubMed] [Google Scholar]
- 20.Kemp AM, Maguire SA, Nuttall D, et al. Bruising in children who are assessed for suspected physical abuse. Arch Dis Child. 2014;99:108–113. doi: 10.1136/archdischild-2013-304339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Christian CW. Committee on Child Abuse and Neglect. The evaluation of suspected child physical abuse. Pediatrics. 2015;135(5):e1337–54. doi: 10.1542/peds.2015-0356. [DOI] [PubMed] [Google Scholar]
- 22.Maguire S, Mann M, Sibert J, et al. Are there patterns of bruising in childhood which are diagnostic or suggestive of abuse? A systematic review. Arch Dis Child. 2005;90:182–186. doi: 10.1136/adc.2003.044065. [DOI] [PMC free article] [PubMed] [Google Scholar]