Abstract
Background:
A higher risk of preterm birth among black women than among white women is well established in the United States. We compared differences in preterm birth between non-Hispanic black and white women in Canada and the US, hypothesizing that disparities would be less extreme in Canada given the different historical experiences of black populations and Canada’s universal health care system.
Methods:
Using data on singleton live births in Canada and the US for 2004–2006, we estimated crude and adjusted risk ratios and risk differences in preterm birth (< 37 wk) and very preterm birth (< 32 wk) among non-Hispanic black versus non-Hispanic white women in each country. Adjusted models for the US were standardized to the covariate distribution of the Canadian cohort.
Results:
In Canada, 8.9% and 5.9% of infants born to black and white mothers, respectively, were preterm; the corresponding figures in the US were 12.7% and 8.0%. Crude risk ratios for preterm birth among black women relative to white women were 1.49 (95% confidence interval [CI] 1.32 to 1.66) in Canada and 1.57 (95% CI 1.56 to 1.58) in the US (p value for heterogeneity [pH] = 0.3). The crude risk differences for preterm birth were 2.94 (95% CI 1.91 to 3.96) in Canada and 4.63 (95% CI 4.56 to 4.70) in the US (pH = 0.003). Adjusted risk ratios for preterm birth (pH = 0.1) were slightly higher in Canada than in the US, whereas adjusted risk differences were similar in both countries. Similar patterns were observed for racial disparities in very preterm birth.
Interpretation:
Relative disparities in preterm birth and very preterm birth between non-Hispanic black and white women were similar in magnitude in Canada and the US. Absolute disparities were smaller in Canada, which reflects a lower overall risk of preterm birth in Canada than in the US in both black and white populations.
In the United States, a higher risk of preterm birth among black women than among white women is well established.1–3 This racial disparity is of great concern because preterm birth is a leading cause of perinatal mortality and is predictive of developmental problems and adverse health outcomes later in life.4 The underlying causes of the racial disparity in preterm birth in the US are not well understood, although research has suggested contributing roles for a wide range of factors, including socioeconomic disadvantage,5 poor neighbourhood conditions (e.g., poverty, crime),5,6 lack of access to health care,7 psychosocial stress,8 racial discrimination9 and adverse health behaviours.10
Rates of preterm birth have consistently been lower in Canada than in the US.11,12 However, in contrast to the US, little is known about differences in rates by race or ethnicity in Canada. There is evidence that African-born and Caribbean-born women in the provinces of Quebec and Ontario have higher rates of preterm birth than Canadian-born women.13–15 Although the magnitude of these differences is smaller than the disparity in preterm births between black and white women in the US,16 foreign-born black women in the US have been found to be at lower risk of preterm birth than US-born black women.17,18
In both Canada and the US, socioeconomic conditions at both individual and neighbourhood levels are important predictors of preterm birth.19–21 Although the income gap between black and white people is markedly smaller in Canada than in the US,22 black populations in both countries have lower education levels, higher unemployment rates and a greater likelihood of living in low-quality neighbourhoods compared with white populations.23 Canada and the US share similar social and economic influences, yet the historical experiences of black populations and the social welfare systems (e.g., universal health care) are quite different in the 2 countries. Black people constitute about 13% of the total US population, but only about 3% of the Canadian population.24,25 The overwhelming majority of Canada’s black population are immigrants who entered the country after 1960 and their descendants, whereas more than 85% of black Americans can trace their ancestry 3 or more generations in the US, with most being descendants of slaves.22
The objectives of our study are twofold. First, using data from a new cohort linking birth registrations with information from the 2006 Canadian long-form census, we present Canada-wide estimates of differences in preterm birth rates between black and white populations. Second, we use comparable methodology to compare racial differences in preterm birth rates between Canada and the US. Given different historical experiences of black populations in the 2 countries, as well as Canada’s commitment to universal health care and its general perception as a more egalitarian society than the US,22 we hypothesized that we would observe smaller racial disparities in the rates in Canada than in the US.
Methods
Study design
We included data on singleton live births in Canada and the US between May 2004 and May 2006. The Canadian data were collected from a linked cohort combining the Canadian Live Birth, Infant Death and Stillbirth Database with 2006 Canadian census data. Approval for this linkage was granted by Statistics Canada’s Executive Management Board, and ethics approval for the study was obtained from the Pediatric Research Ethics Board of the Research Institute of the McGill University Health Centre.
Study cohort
Linkage of the Canadian data was based on the child’s date of birth and sex, the mother’s date of birth, the father’s date of birth and the postal code of the mother’s residence at the time of birth. Completion of the 2006 census was mandatory for all Canadian residents, and 90.5% of births were linked to a census record. In addition to the mandatory short-form census questionnaire, a long-form questionnaire was distributed randomly to 1 in 5 private households (with oversampling in remote northern areas and Indian reserves). For our study cohort, we included births from all Canadian provinces and territories that could be linked to a long-form census questionnaire. As such, we used an approximate 20% sample of births in Canada over the 2-year study period. Data for US births were obtained from the National Center for Health Statistics linked birth–infant death cohort data files.
Gestational age for Canada is based on a clinical estimate of gestational duration, supplied by the physician responsible for delivery. The US data files contain 2 estimates of gestational age: a clinical/obstetric estimate and an estimate based on the date of the mother’s last menstrual period. Although the menstrual-based estimate is frequently used for official US statistics and research, it tends to overestimate preterm birth rates compared with the clinical/obstetric estimates.26 To be comparable with the Canadian data, we restricted the US analysis to the 93.2% of births in our sample with a clinical/obstetric estimate of gestational age. We excluded births with a weight of less than 500 g or a gestational age of less than 20 weeks,27 as well as those with biologically implausible combinations of birth weight and gestational age.28 Infants were categorized as very preterm (< 32 wk), preterm (< 37 wk) or term (37–41 wk).
We restricted our sample to births to non-Hispanic black and non-Hispanic white women. For Canada, these women were identified from the census question on visible minority status, which identifies “persons, other than Aboriginal peoples, who are non-Caucasian in race or non-white in color.” The question asks: “Is this person: White, Chinese, South Asian, Black, Filipino, Latin American, Southeast Asian, Arab, West Asian, Japanese, Korean, other (specify)?” Given the separate category for Latin American, the white and black categories refer primarily to non-Hispanic individuals. People who reported both “black” and “white” were also included in the “black” category. US birth certificates include information on maternal race and Hispanic origin. We included infants born to black or white women who did not report being of Hispanic origin.
Statistical analysis
We used logistic regression to estimate black–white differences in the risk of preterm birth (< 37 wk v. 37–41 wk) and very preterm birth (< 32 wk v. 33–41 wk), separately for each country. To facilitate interpretation and report effects on the absolute probability scale, we calculated average marginal effects estimated from the regression coefficients.29 We estimated crude and adjusted risk differences and risk ratios for preterm birth and very preterm birth for infants born to black versus white women.
We present 2 sets of covariate-adjusted estimates. In the first multivariable model, we adjusted for maternal age (< 20, 20–34 or ≥ 35 yr), marital status (legally married v. not legally married), maternal education (< 12, 12–15 or ≥ 16 yr), birth order (first-born, second, or third or later), infant sex, and paternal information (nonmissing v. missing on birth registration). In the US, missing paternal information on birth registration is associated with an increased risk of preterm birth and other adverse birth outcomes.30 In addition to the aforementioned list of covariates, the second model included maternal nativity (native born v. foreign born) and was estimated for the entire Canadian sample and for US births that occurred in 2004 (29.5% of the total US sample). As of 2005, the National Center for Health Statistics no longer releases maternal birthplace in the publicly available files.
To facilitate comparability, we standardized adjusted models for the US to the covariate distribution of the Canadian study population.29 Specifically, we estimated risk ratios and risk differences for preterm birth between black and white women in each country under a hypothetical scenario in which both populations had Canada’s distribution of measured covariates (e.g., maternal age, education, nativity). For example, although 9.7% of women were less than 20 years of age in the US cohort, we estimated adjusted risk ratios and risk differences for the US for the scenario where just 3.5% of the women were less than 20 (i.e., Canada’s age distribution). As a sensitivity analysis, we also generated estimates for both countries standardized to the covariate distribution of the US black study population.
We used the χ2 test for formal statistical comparison of homogeneity of the estimated risk ratios and risk differences between Canada and the US.31 We applied a cohort weight for analyses using the Canadian data, and we used bootstrap weights to estimate variance. These weights were developed from the census household weight, which adjusts for the census sampling design and nonresponse, and they were calibrated to adjust for missed linkages.
We performed all analyses using Stata version 14.1 (StataCorp).
Results
The Canadian sample comprised 91 045 births, of which 4.2% were to women who reported “black” visible minority status. The US sample included just over 5 million births, with 20.5% born to non-Hispanic black women. Overall, preterm birth rates were 6.0% in Canada and 9.0% in the US; very preterm birth rates were 0.7% and 1.3%, respectively. In Canada, 8.9% of infants born to black women were preterm, as compared with 5.9% of infants born to white women. Corresponding figures in the US were markedly higher, at 12.7% and 8.0%, respectively.
The distribution of selected characteristics of the births to black and white women in each country are presented in Table 1. The US had a higher proportion of births to women less than 20 years of age (9.7% v. 3.5% in Canada). An even starker contrast was observed between the proportion of black women less than 20 in the US and Canada (17.6% v. 4.8%, respectively). Black women in Canada were more likely to be married than black women in the US (52.3% v. 29.7%) and had slightly higher education levels. Finally, we observed large differences in maternal nativity in the black populations between both countries: in the US, 87.2% of the black women were native born, as compared with 24.6% of black women in Canada.
Table 1:
Characteristics of singleton live births to non-Hispanic black and non-Hispanic white women in Canada and the United States, 2004–2006
| Characteristic | Canada*; no. (%) of live births | United States; no. (%) of live births | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Black n = 3 811 |
White n = 87 234 |
Total n = 91 045 |
Black n = 1 039 642 |
White n = 4 029 625 |
Total n = 5 069 267 |
|
| Gestational age, wk | ||||||
|
| ||||||
| 20–28 | 29 (0.8) | 182 (0.2) | 211 (0.2) | 11 224 (1.1) | 12 347 (0.3) | 23 571 (0.5) |
|
| ||||||
| 28–31 | 39 (1.1) | 390 (0.5) | 429 (0.5) | 15 046 (1.5) | 23 379 (0.6) | 38 425 (0.8) |
|
| ||||||
| 32–33 | 43 (1.2) | 529 (0.6) | 572 (0.6) | 15 654 (1.5) | 32 207 (0.8) | 47 861 (0.9) |
|
| ||||||
| 34–36 | 212 (5.8) | 3 962 (4.6) | 4 174 (4.7) | 89 114 (8.6) | 254 587 (6.3) | 343 701 (6.8) |
|
| ||||||
| 37–41 | 3 462 (90.5) | 81 622 (93.4) | 85 084 (93.3) | 902 220 (86.8) | 3 682 951 (91.4) | 4 585 171 (90.4) |
|
| ||||||
| ≥ 42 | 26 (0.6) | 549 (0.6) | 575 (0.6) | 6 384 (0.6) | 24 154 (0.6) | 30 538 (0.6) |
|
| ||||||
| Maternal age, yr | ||||||
|
| ||||||
| < 20 | 161 (4.8) | 2 442 (3.4) | 2 603 (3.5) | 182 477 (17.6) | 309 780 (7.7) | 492 257 (9.7) |
|
| ||||||
| 20–24 | 590 (16.4) | 12 900 (15.8) | 13 490 (15.8) | 341 018 (32.8) | 942 409 (23.4) | 1 283 427 (25.3) |
|
| ||||||
| 25–29 | 1 046 (27.7) | 28 290 (32.2) | 29 336 (32.0) | 251 820 (24.2) | 1 146 411 (28.4) | 1 398 231 (27.6) |
|
| ||||||
| 30–34 | 1 141 (29.5) | 28 706 (32.1) | 29 847 (32.0) | 161 107 (15.5) | 1 011 299 (25.1) | 1 172 406 (23.1) |
|
| ||||||
| 35–39 | 710 (17.4) | 12 518 (13.8) | 13 228 (13.9) | 81 486 (7.8) | 509 839 (12.6) | 591 325 (11.7) |
|
| ||||||
| ≥ 40 | 163 (4.2) | 2 378 (2.7) | 2 541 (2.8) | 21 734 (2.1) | 109 887 (2.7) | 131 621 (2.6) |
|
| ||||||
| Live birth order | ||||||
|
| ||||||
| First-born | 1 508 (41.3) | 40 085 (47.4) | 41 593 (47.1) | 407 178 (39.2) | 1 687 801 (41.9) | 2 094 979 (41.3) |
|
| ||||||
| Second | 1 191 (30.7) | 31 548 (35.7) | 32 739 (35.5) | 300 115 (28.9) | 1 343 462 (33.3) | 1 643 577 (32.4) |
|
| ||||||
| Third or later | 1 112 (28.0) | 15 601 (17.0) | 16 713 (17.4) | 332 349 (32.0) | 998 362 (24.8) | 1 330 711 (26.2) |
|
| ||||||
| Maternal education, yr | ||||||
|
| ||||||
| < 12 | 617 (16.3) | 10 323 (11.4) | 10 940 (11.6) | 249 862 (24.0) | 471 337 (11.7) | 721 199 (14.2) |
|
| ||||||
| 12–15 | 2 507 (65.8) | 50 759 (59.1) | 53 266 (59.4) | 655 150 (63.0) | 2 162 146 (53.7) | 2 817 296 (55.6) |
|
| ||||||
| ≥ 16 | 687 (18.0) | 26 152 (29.5) | 26 839 (29.0) | 134 630 (13.0) | 1 396 142 (34.6) | 1 530 772 (30.2) |
|
| ||||||
| Marital status | ||||||
|
| ||||||
| Unmarried | 1 797 (47.7) | 30 794 (36.6) | 32 591 (37.1) | 730 454 (70.3) | 1 041 893 (25.9) | 1 772 347 (35.0) |
|
| ||||||
| Married | 2 014 (52.3) | 56 440 (63.4) | 58 454 (62.9) | 309 188 (29.7) | 2 987 732 (74.1) | 3 296 920 (65.0) |
|
| ||||||
| Paternal information | ||||||
|
| ||||||
| Not missing | 3 467 (90.7) | 84 940 (97.2) | 88 407 (97.0) | 666 140 (64.1) | 3 667 329 (91.0) | 4 333 469 (85.5) |
|
| ||||||
| Missing | 344 (9.3) | 2 294 (2.8) | 2 638 (3.0) | 373 502 (35.9) | 362 296 (9.0) | 735 798 (14.5) |
|
| ||||||
| Maternal nativity† | ||||||
|
| ||||||
| Native born | 923 (24.6) | 79 232 (90.8) | 80 155 (87.9) | 266 654 (87.2) | 1 123 481 (94.6) | 1 390 126 (93.1) |
|
| ||||||
| Foreign born | 2 888 (75.4) | 8 002 (9.2) | 10 890 (12.1) | 39 206 (12.8) | 63 927 (5.4) | 103 133 (6.9) |
For Canada, frequency counts are unweighted and percentages are weighted. Percentages may not sum to 100 due to rounding.
For US, maternal nativity available only for births in 2004 (n = 1 493 259).
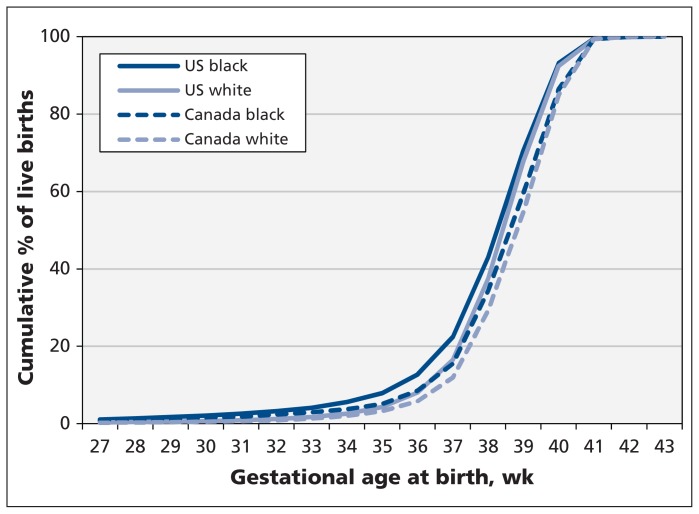
The cumulative proportions of births by gestational age in the black and white cohorts in each country are shown in Figure 1. The proportion of preterm births (< 37 weeks’ gestation) was consistently highest among US black women and lowest among Canadian white women. The crude rates of preterm birth by maternal and paternal sociodemographic characteristics are presented in Table 2. The same information for very preterm birth rates is shown in Table A of Appendix 1 (available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.150464/-/DC1). In both countries, black women had higher rates of preterm birth than white women across nearly all covariate categories, although in Canada no significant racial disparity was observed among women less than 25 years of age or with less than 12 years of education. In general, expected patterns emerged for known maternal risk factors for preterm birth, including younger and older age, being unmarried and low education level. Lower rates of preterm birth were observed among foreign-born than among native-born women in both countries, with the exception of foreign-born black women in Canada, who displayed no preterm birth advantage compared with native-born black women.
Figure 1:
Cumulative proportion of singleton live births, by gestational age, to non-Hispanic black and non-Hispanic white women in Canada and the United States, 2004–2006. The graph is truncated at 27 weeks because the small number of births before 27 weeks among black women in Canada could not be released for confidentiality reasons.
Table 2:
Crude rates of preterm birth among singleton live births to non-Hispanic black and non-Hispanic white women in Canada and the United States, 2004–2006
| Characteristic | Crude rate in Canada, % (95% CI) | Crude rate in US, % (95% CI) | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Black | White | Black–white difference | Black | White | Black–white difference | |
| Maternal age, yr | ||||||
|
| ||||||
| < 20 | 9.6 (5.0 to 14.2) | 8.1 (7.0 to 9.3) | 1.5 (−3.4 to 6.3) | 12.8 (12.6 to 13.0) | 9.8 (9.7 to 9.9) | 3.0 (2.8 to 3.2) |
|
| ||||||
| 20–24 | 6.3 (4.2 to 8.4) | 6.3 (5.8 to 6.7) | 0.0 (−2.0 to 2.2) | 12.1 (12.0 to 12.2) | 8.5 (8.4 to 8.5) | 3.6 (3.5 to 3.8) |
|
| ||||||
| 25–29 | 8.0 (6.2 to 9.8) | 5.7 (5.4 to 6.0) | 2.3 (0.4 to 4.1) | 12.1 (12.0 to 12.2) | 7.7 (7.6 to 7.7) | 4.4 (4.3 to 4.6) |
|
| ||||||
| 30–34 | 8.8 (7.1 to 10.6) | 5.8 (5.5 to 6.1) | 3.1 (1.3 to 4.8) | 13.0 (12.9 to 13.2) | 7.5 (7.4 to 7.5) | 5.6 (5.4 to 5.8) |
|
| ||||||
| 35–39 | 11.2 (8.4 to 14.1) | 5.9 (5.4 to 6.3) | 5.4 (2.6 to 8.2) | 15.1 (14.9 to 15.4) | 8.2 (8.1 to 8.2) | 7.0 (6.7 to 7.2) |
|
| ||||||
| ≥ 40 | 16.0 (10.1 to 21.9) | 8.6 (7.3 to 9.9) | 7.4 (1.3 to 13.4) | 17.6 (17.1 to 18.1) | 9.6 (9.5 to 9.8) | 7.9 (7.4 to 8.5) |
|
| ||||||
| Live birth order | ||||||
|
| ||||||
| First-born | 10.1 (8.5 to 11.8) | 7.2 (7.0 to 7.4) | 2.9 (1.3 to 4.6) | 12.3 (12.2 to 12.4) | 8.8 (8.7 to 8.8) | 3.6 (3.4 to 3.7) |
|
| ||||||
| Second | 8.0 (6.2 to 9.9) | 4.7 (4.4 to 5.0) | 3.3 (1.5 to 5.2) | 11.8 (11.7 to 11.9) | 7.1 (7.1 to 7.2) | 4.7 (4.6 to 4.8) |
|
| ||||||
| Third or later | 8.2 (6.5 to 10.0) | 5.4 (5.1 to 5.8) | 2.8 (1.0 to 4.5) | 14.0 (13.9 to 14.2) | 8.2 (8.2 to 8.3) | 5.8 (5.7 to 6.0) |
|
| ||||||
| Sex of infant | ||||||
|
| ||||||
| Female | 9.9 (8.3 to 11.4) | 5.5 (5.3 to 5.8) | 4.3 (2.8 to 5.9) | 12.7 (12.6 to 12.8) | 7.6 (7.6 to 7.7) | 5.1 (5.0 to 5.2) |
|
| ||||||
| Male | 8.1 (6.7 to 9.4) | 6.4 (6.2 to 6.7) | 1.6 (0.3 to 2.9) | 12.8 (12.7 to 12.8) | 8.5 (8.5 to 8.6) | 4.2 (4.1 to 4.3) |
|
| ||||||
| Maternal education, no. of years | ||||||
|
| ||||||
| < 12 | 7.7 (5.5 to 10.0) | 7.0 (6.4 to 7.5) | 0.8 (−1.5 to 3.1) | 14.1 (13.9 to 14.2) | 10.2 (10.1 to 10.3) | 3.9 (3.7 to 4.0) |
|
| ||||||
| 12–15 | 9.3 (8.1 to 10.6) | 6.1 (5.9 to 6.4) | 3.2 (1.9 to 4.5) | 12.6 (12.5 to 12.7) | 8.5 (8.4 to 8.5) | 4.1 (4.0 to 4.2) |
|
| ||||||
| ≥ 16 | 8.6 (6.3 to 10.8) | 5.4 (5.1 to 5.7) | 3.2 (1.0 to 5.4) | 10.8 (10.7 to 11.0) | 6.8 (6.7 to 6.8) | 4.1 (3.9 to 4.2) |
|
| ||||||
| Marital status | ||||||
|
| ||||||
| Unmarried | 9.5 (8.0 to 11.0) | 6.6 (6.3 to 6.9) | 2.9 (1.4 to 4.5) | 13.2 (13.2 to 13.3) | 9.6 (9.5 to 9.6) | 3.7 (3.6 to 3.8) |
|
| ||||||
| Married | 8.4 (7.1 to 9.8) | 5.7 (5.5 to 5.9) | 2.8 (1.4 to 4.1) | 11.5 (11.4 to 11.6) | 7.6 (7.5 to 7.6) | 4.0 (3.8 to 4.1) |
|
| ||||||
| Paternal information | ||||||
|
| ||||||
| Not missing | 8.8 (7.7 to 9.9) | 6.0 (5.8 to 6.1) | 2.8 (1.7 to 3.9) | 10.8 (10.5 to 11.1) | 7.8 (7.7 to 7.8) | 3.0 (2.7 to 3.4) |
|
| ||||||
| Missing | 10.4 (7.1 to 13.8) | 7.7 (6.4 to 8.9) | 2.8 (−0.9 to 6.4) | 12.0 (11.9 to 12.1) | 8.9 (8.7 to 9.1) | 3.1 (2.9 to 3.3) |
|
| ||||||
| Maternal nativity* | ||||||
|
| ||||||
| Native born | 8.3 (6.3 to 10.2) | 6.1 (5.9 to 6.3) | 2.2 (0.2 to 4.1) | 13.1 (13.0 to 13.2) | 8.1 (8.1 to 8.2) | 5.0 (4.9 to 5.1) |
|
| ||||||
| Foreign born | 9.2 (8.0 to 10.4) | 4.9 (4.4 to 5.4) | 4.2 (2.9 to 5.6) | 9.6 (9.3 to 9.9) | 6.1 (5.9 to 6.3) | 3.5 (3.1 to 3.8) |
Note: CI = confidence interval.
For US, maternal nativity available only for births in 2004 (n = 1 493 259).
Crude and adjusted risk ratios and risk differences for preterm birth and very preterm birth between non-Hispanic black and non-Hispanic white women are shown in Table 3. Crude risk ratios for preterm birth were similar between the 2 countries, with ratios among black women relative to white women of 1.49 (95% confidence interval [CI] 1.32 to 1.66) in Canada and 1.57 (95% CI 1.56 to 1.58) in the US (p value for heterogeneity [pH] = 0.3). Risk ratios were substantially higher for very preterm birth and were again similar between the 2 countries: 2.70 (95% CI 1.95 to 3.44) in Canada and 2.81 (95% CI 2.77 to 2.86) in the US (pH = 0.8). The 2 adjusted models — the first without and the second including maternal nativity — produced similar estimates. Adjustment (with US estimates standardized to the covariate distribution of the Canadian sample) tended to reduce relative disparities for preterm birth in the US. Adjusted risk ratios for preterm birth from the model that included maternal nativity were slightly higher in Canada than in the US (pH = 0.1).
Table 3:
Relative and absolute differences in preterm and very preterm births among non-Hispanic black women relative to non-Hispanic white women in Canada and the United States, 2004–2006
| Measure; outcome | Crude | Adjusted* | Adjusted† | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Canada | US | pH value‡ | Canada | US§ | pH value‡ | Canada | US§ | pH value‡ | |
| Risk ratio (95% CI) | |||||||||
|
| |||||||||
| Preterm birth (< 37 v. 37–41 wk) | 1.49 (1.32 to 1.66) | 1.57 (1.56 to 1.58) | 0.3 | 1.46 (1.29 to 1.63) | 1.41 (1.40 to 1.42) | 0.5 | 1.60 (1.39 to 1.81) | 1.45 (1.44 to 1.47) | 0.1 |
|
| |||||||||
| Very preterm birth (< 32 v. 32–41 wk) | 2.70 (1.95 to 3.44) | 2.81 (2.77 to 2.86) | 0.8 | 2.61 (1.88 to 3.35) | 2.36 (2.31 to 2.40) | 0.5 | 2.62 (1.83 to 3.41) | 2.43 (2.36 to 2.52) | 0.6 |
|
| |||||||||
| Risk difference (95% CI) | |||||||||
|
| |||||||||
| Preterm birth (< 37 v. 37–41 wk) | 2.94 (1.91 to 3.96) | 4.63 (4.56 to 4.70) | 0.003 | 2.76 (1.74 to 3.78) | 3.41 (3.33 to 3.48) | 0.2 | 3.59 (2.32 to 4.85) | 3.57 (3.43 to 3.70) | 1.0 |
|
| |||||||||
| Very preterm birth (< 32 v. 32–41 wk) | 1.22 (0.71 to 1.73) | 1.67 (1.64 to 1.70) | 0.08 | 1.16 (0.66 to 1.67) | 1.31 (1.28 to 1.35) | 0.6 | 1.17 (0.62 to 1.71) | 1.32 (1.25 to 1.38) | 0.6 |
Note: CI = confidence interval.
Term birth = 37–41 wk, preterm = < 37 wk, very preterm = < 32 wk.
Adjusted for maternal age, maternal education, marital status, birth order, sex of child and missing paternal information.
Adjusted for maternal age, maternal education, marital status, birth order, sex of child, missing paternal information and maternal nativity. For the US sample, the estimates include only births in 2004 (n = 1 493 259).
pH = p value for χ2 test for heterogeneity of the risk ratios or risk differences.
Adjusted US estimates are standardized to the covariate distribution of the Canadian study population.
The risk differences show a somewhat different picture of racial disparities between the 2 countries than the risk ratios. Crude risk differences for preterm birth were 2.94 (95% CI 1.91 to 3.96) in Canada and 4.63 (95% CI 4.56 to 4.70) in the US (pH = 0.003), whereas crude risk differences for very preterm birth were 1.22 (95% CI 0.71 to 1.73) in Canada and 1.67 (95% CI 1.64 to 1.70) in the US (pH = 0.08). Adjusted risk differences in the US were substantially reduced from the crude estimates and were similar in magnitude to the adjusted Canadian estimates.
All of the estimates in Table 3 were unchanged when we imputed the 6.8% of the US sample missing a clinical/obstetric estimate for gestational age with the menstrual-based estimate (available for 85% of the missing observations) (see Table B in Appendix 1).
To facilitate comparability of estimates between the 2 countries, we chose to standardize the US estimates to the covariate distribution of the Canadian study population. However, as a sensitivity analysis, we also generated estimates for both countries standardized to the covariate distribution of the US black population (see Table C in Appendix 1). The risk ratios were nearly identical regardless of whether the estimates were standardized to the Canadian population or to the US black population. However, the risk differences in both countries increased in magnitude when the US black population was used as the standard population.
Unweighted risk ratios and risk differences in Canada were similar to the weighted estimates (see Table D in Appendix 1).
Interpretation
We found that relative differences in preterm and very preterm birth rates between black and white women in Canada were similar in magnitude to the racial disparities observed in the US study cohort. The absolute difference in preterm birth was narrower in Canada than in the US, which reflects the lower overall preterm birth rates in Canada among black and white women. In both countries, the racial disparity in preterm birth persisted after we controlled for available sociodemographic variables.
Although the published evidence is limited on racial differences in preterm birth outside the US, studies from the United Kingdom and the Netherlands found narrower gaps in preterm birth rates between black and white women than were evident in our Canadian and US estimates.32–34 Research conducted outside the US has tended to focus more on differences by maternal country of birth as opposed to race or ethnicity, with consistently higher preterm birth risks reported among women born in sub-Saharan Africa and the Caribbean than among women born in France, Canada or the Netherlands.13,15,35
In the US, foreign-born black women have considerably lower preterm birth risk than native-born black women,17,36 but it is not known whether this pattern holds in other countries. We detected no advantage in preterm birth risk among foreign-born versus native-born black women in Canada, with our results instead suggesting higher preterm and very preterm birth risk among foreign-born black women than among native-born black women in Canada (preterm birth rate 9.2% v. 8.3%; very preterm birth 2.1% v. 1.4%). These estimates, however, are not statistically different from each other, owing at least in part to the relatively small number of Canadian-born black women in our study. Still, it appears that foreign-born black women in Canada and the US have similar absolute risks of preterm birth (9.2% and 9.6%, respectively), whereas the risk among native-born black women is considerably lower in Canada than in the US (8.3% v. 13.1%). The explanation for why we did not observe a “healthy immigrant effect” in terms of preterm birth among black women in Canada is not clear. One possibility is that black immigrants in Canada may be a more disadvantaged population than black immigrants in the US — for example, a higher proportion of Africans have come to Canada as refugee claimants compared with the proportion in the US.23
Limitations
We linked birth registry data to a random 20% sample of households that completed the long-form component of the mandatory 2006 census. As such, our results are representative of the Canadian national population, with the only limitation being the reduced sample size that decreased the precision of our estimates. With the birth–census cohort, were were able to link more than 90% of the births to a census record, and preterm birth rates estimated for the cohort were consistent with those calculated for all Canadian births over the same period.37 However, births to women less than 25 years of age and to women not born in Canada were less likely to be linked to census data. As such, the linkage rate may have been lower for births to black women, who were considerably more likely to be foreign born than the white women in the study cohort. Because foreign-born black women appeared to have a slightly higher risk of preterm birth than native-born black women in Canada, the lower linkage rate among foreign-born women may have resulted in slightly underestimated risk ratios and risk differences between the black and white study populations.
Another important limitation of our study is the documented poor quality of birth registration data from Ontario, Canada’s most populous province. Fees for obtaining birth certificates in Ontario led to underregistration of live births, especially for infants who died, compared with other provinces.11 Given that more than half of Canada’s black population lives in Ontario, we conducted our main analyses for the national population (including Ontario) and performed a sensitivity analysis to assess the effect of excluding Ontario on our results (see Table E in Appendix 1). It is reassuring that both the crude and adjusted risk ratios and risk differences for preterm birth were similar whether Ontario data were included or excluded. The crude estimates for very preterm birth also did not differ significantly, although slightly larger adjusted risk ratios and risk differences for very preterm birth were observed when Ontario data were excluded. This suggests that we may have missed some infants born very preterm (likely some unlinked infant deaths).
Further limitations include the slight differences in race and ethnicity categories used to identify black and white women between the 2 countries, and the lack of comparable information for both countries on parental socioeconomic position and other potentially important covariates (e.g., quality of prenatal care).
Finally, the data we used were from a decade ago. Although we cannot rule out changes in racial disparities in preterm birth and very perterm birth in Canada over the past decade, evidence from the US suggests that disparities have been stable over this period.12
Conclusion
Relative disparities in preterm birth and very preterm birth between non-Hispanic black and white women in Canada mirrored those in the US. This observation was contrary to our hypothesis, which was based on the different historical experiences of black populations in the 2 countries and evidence that socioeconomic and racial disparity in health and access to health care tend to be less extreme in Canada. Absolute disparities were smaller in Canada than in the US, which reflects the lower overall risk of preterm birth in Canada in both black and white populations.
Our findings do not provide insight into the specific mechanisms underlying the racial differences in preterm birth, nor whether those mechanisms are likely to be similar or different in the 2 countries. The limited evidence available has not identified genetic differences that explain the racial disparities in preterm birth.38 Previous studies have suggested complex roles for a range of socioeconomic factors at the individual-, household- and neighbourhood-levels.5,39 Stress and adverse experiences throughout life, including racial discrimination, are also biologically plausible factors that may contribute to the observed social patterning of racial disparities in preterm birth in the US.38 Although we hypothesized that the different historical and social context in Canada would mitigate racial disparities in preterm birth, our findings suggest a possible etiologic role for socioeconomic disadvantage and racial discrimination in Canada as well.
Further research is needed to understand the biological and social determinants of differences in preterm birth risk between black and white women in both Canada and the US, as well as the mechanisms by which 2 different national contexts gave rise to similar patterns of relative disparity in preterm birth. Given the large racial disparity in preterm birth rates that we observed in Canada, further research should examine potential determinants (e.g., socioeconomic disadvantage, discrimination, residential segregation, health behaviours) of this disparity, as well as the association between racial disparity and other perinatal outcomes in Canada.
Acknowledgments
The authors thank Russell Wilkins (Statistics Canada and the Department of Epidemiology and Community Medicine, University of Ottawa) for his input on the analysis and interpretation of findings; Statistics Canada employees Martin Lessard, James Brennan and Patrick Gallifa for carrying out the data linkage; Wei Qian for developing a cohort weight; Lauren Pinault, Jessica Pembroke, Raymond Reaume, and Zimei Zhang for manual review and verification; and Michael Tjepkema and Julie Bernier for managerial oversight and support.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributions: Britt McKinnon, Jay Kaufman, Michael Kramer and Seungmi Yang contributed to the study concept and design. All of the authors were involved in the analysis and interpretation of data and the critical revision of the manuscript for important intellectual content. Britt McKinnon conducted the statistical analyses and wrote the first draft. All of the authors approved the final version to be published and agree to act as guarantors of the work.
Funding: Major funding for this study was provided by the Canadian Institutes of Health Research (CIHR grant no. MOP-111122), with additional support from Health Canada (Air Health Effects Research, Population Studies Division). Jay Kaufman was supported by the Canada Research Chairs program. Analysis of the Canadian data was conducted at the Quebec Inter-University Centre for Social Statistics (QICSS), which is part of the Canadian Research Data Centre Network. The services and activities provided by the QICSS are made possible by the financial or in-kind support of the Social Sciences and Humanities Research Council, the CIHR, the Canadian Foundation for Innovation, Statistics Canada, the Fonds de Recherche sur la Société et la Culture, and the Quebec universities. The funding sources had no role in the design and conduct of the study, in the collection, analysis and interpretation of the data, or in the preparation, review or approval of the manuscript.
References
- 1.Culhane JF, Goldenberg RL. Racial disparities in preterm birth. Semin Perinatol 2011;35:234–9. [DOI] [PubMed] [Google Scholar]
- 2.Demissie K, Rhoads GG, Ananth CV, et al. Trends in preterm birth and neonatal mortality among blacks and whites in the United States from 1989 to 1997. Am J Epidemiol 2001;154:307–15. [DOI] [PubMed] [Google Scholar]
- 3.MacDorman MF. Race and ethnic disparities in fetal mortality, preterm birth, and infant mortality in the United States: an overview. Semin Perinatol 2011;35:200–8. [DOI] [PubMed] [Google Scholar]
- 4.Goldenberg RL, Culhane JF, Iams JD, et al. Epidemiology and causes of preterm birth. Lancet 2008;371:75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braveman PA, Heck K, Egerter S, et al. The role of socioeconomic factors in black–white disparities in preterm birth. Am J Public Health 2015;105:694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Messer LC, Kaufman JS, Dole N, et al. Neighborhood crime, deprivation, and preterm birth. Ann Epidemiol 2006;16:455–62. [DOI] [PubMed] [Google Scholar]
- 7.Lu MC, Kotelchuck M, Hogan V, et al. Closing the black–white gap in birth outcomes: a life-course approach. Ethn Dis 2010;20(1 Suppl 2):S2–62–76. [PMC free article] [PubMed] [Google Scholar]
- 8.Witt WP, Cheng ER, Wisk LE, et al. Preterm birth in the United States: the impact of stressful life events prior to conception and maternal age. Am J Public Health 2014;104(Suppl 1):S73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins JW, David RJ, Handler A, et al. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health 2004;94:2132–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elo IT, Culhane JF. Variations in health and health behaviors by nativity among pregnant black women in Philadelphia. Am J Public Health 2010;100:2185–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Canadian perinatal health report, 2008 edition. Ottawa: Public Health Agency of Canada; 2008. Available: www.phac-aspc.gc.ca/publicat/2008/cphr-rspc/index-eng.php (accessed 2014 Oct. 2). [Google Scholar]
- 12.Martin JA, Hamilton BE, Ventura SJ, et al. Births: Final data for 2011. Hyattsville (MD): National Center for Health Statistics; 2013:62. [PubMed] [Google Scholar]
- 13.Auger N, Chery M, Daniel M. Rising disparities in severe adverse birth outcomes among Haitians in Québec, Canada, 1981–2006. J Immigr Minor Health 2012;14:198–208. [DOI] [PubMed] [Google Scholar]
- 14.Moore S, Daniel M, Auger N. Socioeconomic disparities in low birth weight outcomes according to maternal birthplace in Québec, Canada. Ethn Health 2009;14:61–74. [DOI] [PubMed] [Google Scholar]
- 15.Urquia ML, Berger H, Ray JGCanadian Curves Consortium. Risk of adverse outcomes among infants of immigrant women according to birth-weight curves tailored to maternal world region of origin. CMAJ 2015;187:E32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ananth CV, Joseph KS, Oyelese Y, et al. Trends in preterm birth and perinatal mortality among singletons: United States, 1989 through 2000. Obstet Gynecol 2005;105:1084–91. [DOI] [PubMed] [Google Scholar]
- 17.Elo IT, Vang Z, Culhane JF. Variation in birth outcomes by mother’s country of birth among non-Hispanic black women in the United States. Matern Child Health J 2014;18:2371–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mason SM, Kaufman JS, Emch ME, et al. Ethnic density and preterm birth in African-, Caribbean-, and US-born non-Hispanic black populations in New York City. Am J Epidemiol 2010;172:800–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Too early, too small: a profile of small babies across Canada. Ottawa: Canadian Institute for Health Information; 2009. Available: https://secure.cihi.ca/free_products/too_early_too_small_en.pdf (accessed 2014 Oct. 2). [Google Scholar]
- 20.Luo ZC, Wilkins R, Kramer MSFetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. CMAJ 2006;174:1415–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parker JD, Schoendorf KC, Kiely JL. Associations between measures of socioeconomic status and low birth weight, small for gestational age, and premature delivery in the United States. Ann Epidemiol 1994;4:271–8. [DOI] [PubMed] [Google Scholar]
- 22.Attewell P, Kasinitz P, Dunn K. Black Canadians and black Americans: racial income inequality in comparative perspective. Ethn Racial Stud 2010;33:473–95. [Google Scholar]
- 23.Frazier JW, Darden JT, Henry NF. The African diaspora in the United States and Canada at the dawn of the 21st century. Albany (NY): State University of New York Press; 2010. [Google Scholar]
- 24.Rastogi S, Johnson TD, Hoeffel EM, et al. The black population: 2010. Washington (DC): US Census Bureau; 2011. Available: www.census.gov/prod/cen2010/briefs/c2010br-06.pdf (accessed 2014 Nov. 21). [Google Scholar]
- 25.National Household Survey (NHS) Profile, 2011. Ottawa: Statistics Canada; 2011. Available: www12.statcan.gc.ca/nhs-enm/2011/dp-pd/prof/index.cfm?Lang=E (accessed 2015 Feb. 10). [Google Scholar]
- 26.Joseph KS, Huang L, Liu S, et al. Reconciling the high rates of preterm and postterm birth in the United States. Obstet Gynecol 2007;109:813–22. [DOI] [PubMed] [Google Scholar]
- 27.Sepkowitz S. International rankings of infant mortality and the United States’ vital statistics natality data collecting system — failure and success. Int J Epidemiol 1995;24:583–8. [DOI] [PubMed] [Google Scholar]
- 28.Alexander GR, Himes JH, Kaufman RB, et al. A United States national reference for fetal growth. Obstet Gynecol 1996;87:163–8. [DOI] [PubMed] [Google Scholar]
- 29.Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol 2014;43:962–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tan H, Wen SW, Walker M, et al. Missing paternal demographics: a novel indicator for identifying high risk population of adverse pregnancy outcomes. BMC Preg Childbirth 2004;4:21–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaufman JS, MacLehose RF. Which of these things is not like the others? Cancer 2013;119:4216–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bansal N, Chalmers JWT, Fischbacher CM, et al. Scottish Health and Ethnicity Linkage Study. Ethnicity and first birth: age, smoking, delivery, gestation, weight and feeding: Scottish Health and Ethnicity Linkage Study. Eur J Public Health 2014;24:911–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ravelli ACJ, Tromp M, Eskes M, et al. Ethnic differences in stillbirth and early neonatal mortality in The Netherlands. J Epidemiol Community Health 2011;65:696–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patel RR, Steer P, Doyle P, et al. Does gestation vary by ethnic group? A London-based study of over 122 000 pregnancies with spontaneous onset of labour. Int J Epidemiol 2004;33:107–13. [DOI] [PubMed] [Google Scholar]
- 35.Zeitlin J, Bucourt M, Rivera L, et al. Preterm birth and maternal country of birth in a French district with a multiethnic population. BJOG 2004;111:849–55. [DOI] [PubMed] [Google Scholar]
- 36.Kramer MS, Ananth CV, Platt RW, et al. US black vs white disparities in foetal growth: Physiological or pathological? Int J Epidemiol 2006;35:1187–95. [DOI] [PubMed] [Google Scholar]
- 37.Bushnik T, Yang S, Kramer MS, et al. The 2006 Canadian birth–census cohort. Health Rep In press. [PubMed] [Google Scholar]
- 38.Kramer MR, Hogue CR. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiol Rev 2009;31:84–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blumenshine P, Egerter S, Barclay CJ, et al. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med 2010;39:263–72. [DOI] [PubMed] [Google Scholar]