Abstract
Objective
Test changes in (a) coping efficacy and (b) anxious self-talk as potential mediators of treatment gains at 3-month follow-up in the Child/Adolescent Anxiety Multimodal Treatment Study (CAMS).
Method
Participants were 488 youth (ages 7-17; 50.4% male) randomized to cognitive-behavioral therapy (CBT; Coping cat program), pharmacotherapy (sertraline), their combination, or pill placebo. Participants met DSM-IV criteria for generalized anxiety disorder, social phobia, and/or separation anxiety disorder. Coping efficacy (reported ability to manage anxiety provoking situations) was measured by youth and parent reports on the Coping Questionnaire, and anxious self-talk was measured by youth report on the Negative Affectivity Self-Statement Questionnaire. Outcome was measured using the Pediatric Anxiety Rating Scale (completed by Independent Evaluators blind to condition). For temporal precedence, residualized treatment gains were assessed at 3-month follow-up.
Results
Residualized gains in coping efficacy mediated gains in the CBT, sertraline, and combination conditions. In the combination condition, some unique effect of treatment remained. Treatment assignment was not associated with a reduction in anxious self-talk, nor did anxious self-talk predict changes in anxiety symptoms.
Conclusions
The findings suggest that improvements in coping efficacy are a mediator of treatment gains. Anxious self-talk did not emerge as a mediator.
Keywords: anxiety, youth, anxious self-talk, coping, mediators, CBT, pharmacotherapy
Youth with anxiety disorders evidence considerable functional impairment (e.g., Kendall et al., 2010) and are at risk for poor outcomes if left untreated (Angold, Costello, & Erkanli, 1999; Lopez, Turner, & Saavedra, 2005). Fortunately, there are efficacious treatments for youth anxiety, including cognitive-behavioral therapy (CBT; see Hollon & Beck, 2013; e.g., Kendall et al., 2008; Wood, Piacentini, Southam-Gerow, Chu, & Sigman, 2006) and pharmacotherapy using selective serotonin-reuptake inhibitors (SSRIs; e.g., Birmaher et al., 2003; Rynn, Siqueland, & Rickels, 2001). The combination of CBT and the SSRI sertraline has been found to be particularly effective for anxiety in youth (Walkup et al., 2008). Despite these advances, little is known about the operative mechanisms/mediators of change. Yet, the identification of mediators can inform efforts to refine therapeutic approaches (e.g., make them more potent or efficient) and can inform training efforts (Barrett, Farrell, Pina, Peris, & Piacentini, 2008; Chu & Harrison, 2007; Kendall, Comer, Chow, 2013). Conceptual models of anxiety disorders and their treatment (e.g., Albano & Kendall, 2002; Barlow, 2002; Kendall, 2012) and previous empirical work (Muris et al., 2009; Treadwell & Kendall, 2007) suggest that youth show gains in outcomes through both coping and cognitive mechanisms.
The examination of treatment mediators in the youth anxiety literature is surprisingly rare. One step in this process is to pinpoint candidate mediators by determining which change mechanisms are impacted by theoretically distinct therapeutic approaches (Prins & Ollendick, 2003). Meta-analyses suggest potential treatment mediators for anxious youth. For example, Davis and Ollendick (2005) reviewed available empirically supported treatments (ESTs) for pediatric specific phobias, focusing on physiology, behavior, subjective fear, and cognition as underlying principles of change (e.g., Lang, 1979; Lang, Cuthbert, & Bradley, 1998). Although they did not encounter any formal studies of mediation, their review suggests that CBT probably achieved benefit through the reduction of subjective fear, behavioral avoidance, and cognitive factors.
Chu and Harrison (2007) reviewed 14 randomized trials that included at least one theory-based candidate mediator. The potential mediators were behavioral, physiological, cognitive, or coping variables. CBT resulted in a large mean effect size for behavioral variables and moderate mean effect sizes for physiological, cognitive, and coping variables. However, we noted that very few of these studies included formal tests of mediation and/or assessed potential mediators at time points other than pre- and post-treatment. Cognitive outcomes were reported relatively frequently, but few studies examined coping. .
Anxious cognition is a component of distressing anxiety, and age and gender can influence the impact of cognition on anxiety (Cannon & Weems, 2010). Anxious children report more anxious self-talk than non-anxious children, and compared to non-anxious counterparts, anxious youth report more negative than positive self-talk (Sood & Kendall, 2007). These findings are consistent with the notion that beneficial change is not in the power of positive thinking, but in the “power of non-negative thinking” (Kendall, 1984). The content of the negative self-talk in anxious youth tends to include future-oriented thinking associated with danger, harm, and threat (Schniering & Rapee, 2002; 2004). Anxious youth often overestimate the chance of a negative outcome and the consequences of such an outcome, evaluate themselves negatively, and can be preoccupied with their thoughts (Fox, Houston, & Pittner, 1983; Prins & Hanewald, 1997; Szabo & Loviband, 2004). However, the causal and temporal nature of negative self-talk and anxiety in children requires further examination (Sood & Kendall, 2007).
CBT helps youth identify their anxious thoughts and both accept them and challenge their accuracy through cognitive skills training and behavioral experiments (e.g., exposure tasks). Are improvements in anxiety achieved through changes in cognitive processes? Muris, Mayer, den Adel, Roos, and van Wamelen (2009) found that changes in anxiety symptoms were associated with changes in negative automatic thoughts and perceived control over anxiety-related events (Heard, Dadds, & Rapee, 1991). In the Child/Adolescent Anxiety Multimodal Treatment Study (CAMS), the introduction of cognitive restructuring was found to accelerate improvements in CBT among anxious youth (Peris et al., in press). Four studies evaluated cognitive factors as potential treatment mediators for anxious youth. Treadwell and Kendall (1996) examined several cognitive variables as mediators of the Coping cat program (Kendall & Hedtke, 2006) among 151 children with an anxiety disorder randomized to treatment or waitlist. Cognitive variables were measured by the Negative Affectivity Self-Statement Questionnaire for Children (NASSQ; Ronan, Kendall, & Rowe, 1994). Negative self-talk and the ratio of negative to positive self-talk were found to be mediators of change in anxiety, but positive self-talk and depressive self-talk were not. Kendall and Treadwell (2007) followed with a second study of 145 children with an anxiety disorder randomized to CBT (i.e., Coping cat) or waitlist. Changes in both anxious and negative self-talk (on the NASSQ) mediated treatment outcome (changes in depressive and positive self-talk did not; for review of anxiety and depression in youth, see Cummings, Caporino & Kendall, 2014). In a third study, Lau, Chan, Li, and Au (2010) examined the effectiveness of the Coping cat program with Chinese youth (N = 45) in community clinics. Within a multiple mediator model, anxious self-talk (NASSQ) mediated outcome when measured by youth-report on the Spence Children’s Anxiety Scale (SCAS; Spence, 1998). Of note, temporal precedence of the mediators was not established in these studies, so it cannot be concluded with confidence that anxious self-talk is a causal agent rather than a covariate of change (MacKinnon, Fairchild, & Fritz, 2007).
In a study that did assess temporality in 145 anxious Dutch youth, Hogendoorn and colleagues (2013) found that an increase in positive thoughts (on the Children’s Automatic Thoughts Scale- Negative/Positive; CATS-N/P; Hogendoorn et al., 2010) mediated the effect of CBT (the Dutch Coping Cat protocol; Nauta & Scholing, 2007). Contrary to Kendall and Treadwell’s (2007) findings, changes in negative thoughts did not precede change in anxiety symptoms. To their credit, Hogendoorn and colleagues (2013) analyses included temporal precedence.
Behavioral change is another candidate mediator of treatment for anxiety disorders. Avoidance behavior is associated with anxiety (Mineka & Zinbarg, 2006) and, though avoidance may alleviate anxiety in the short-term, it is ineffective in the long-term. Given that avoidance is a core feature in pathological anxiety, exposure tasks are regarded as an important therapeutic ingredient (Bouchard, Mendlowitz, Coles, & Franklin, 2004; Kazdin & Weisz, 1998; Kendall et al., 2005), and some evidence suggests that treatment gains do not occur until the exposure part of treatment (Kendall et al., 1997). In CAMS, the introduction of exposure tasks significantly accelerated treatment outcome (Peris et al., 2015). Variations in procedures for implementing exposure tasks (e.g., the amount of preparation, execution, and processing of the experience) have been examined (Tiwari, Kendall, Hoff, Harrison, & Fizur, 2013) and post-exposure processing significantly predicted lower clinician-rated anxiety severity at posttreatment.
Why might exposure tasks be critical to a positive treatment outcome? Through behavioral exposure, youth work their way through a hierarchy of feared situations, thus learning to face and experience rather than avoid anxiety. Exposure tasks are theorized to, in part, facilitate the development of coping skills (Kendall et al., 2005), Such skills include a range of physiological, cognitive, and behavioral strategies used to manage emotions and the environment in response to stress (Compas et al., 2001). Coping may have some overlap with cognitive variables, but it can be more broadly understood as moving from inactive, passive strategies (e.g., escape or avoidance) to more active strategies (e.g., problem-solving) to address stressful situations (Chu & Harrison, 2007). By participating in exposure tasks, youth practice their coping skills in anxiety-provoking situations. These successive experiences of actively coping with previously avoided situations present youth with the opportunity to build their overall sense of coping efficacy. Coping efficacy, the reported ability to manage anxiety provoking situations, is a candidate mediator in CBT for anxiety disorders because a child with greater coping efficacy is less likely to avoid an anxiety-provoking situation. Evidence suggests that perceived coping is particularly salient for older children (Creswell, Murray & Cooper, 2014). Decreased avoidance results in confronting feared stimuli which in turn can result in respondent extinction and/or new skills and thus decreased overall anxiety.
Coping variables have been tested as a candidate mediator. Lau and colleagues (2010) examined coping efficacy, measured by the Coping-Questionnaire-Child/youth report (CQ-C; Kendall, 1994) and the Coping Questionnaire- Parent report (CQ-P; Kendall, 1994) in the aforementioned effectiveness trial of CBT for anxious Chinese youth. In a multiple mediator model, changes in CQ-C and CQ-P scores mediated treatment outcome. Further testing of specific contributions revealed that the CQ-C mediated outcome as measured by the Spence Children’s Anxiety Scale (SCAS; Spence, 1998) and Spence Children’s Anxiety Scale-Parent (PSCAS; Spence, 1998) although the CQ-P did not. Among the studies that tested for mediation, temporal precedence of the mediator was typically not established, limiting the ability to draw firm conclusions and make causal inferences (MacKinnon et al., 2007). Given the emphasis that CBT places on the acquisition of coping skills, studies examining coping variables as potential treatment mediators are warranted.
The present study evaluated (a) anxious self-talk and (b) coping efficacy as potential mediators in CAMS (Walkup et al., 2008). Through use of CAMS data, we tested mediation across four treatment conditions (CBT only, sertraline only, their combination, and pill placebo). Primary findings from the CAMS revealed that combination therapy (80% improved) outperformed both CBT (60% improved) and sertraline (55% improved), and that all therapies were superior to placebo (24% improved; Walkup et al., 2008). Although our focus is on the CBT conditions, investigation of psychological mediators in the medication literature is virtually unexplored (see Walkup et al., 2003) so we also examined mediation in the medication conditions. To have true temporal precedence, we tested the mediation of gains assessed 3 months after treatment. Thus, CBT participants had time to integrate their therapy experiences. Some participants continued their treatment (e.g., medications) or had other professional contacts. Placebo participants received some services (resulting in a more conservative test). We hypothesized that: (1) reductions in anxious self-talk would mediate treatment gains; and (2) increases in perceived coping efficacy would mediate treatment gains. These hypotheses were tested across acute treatment and initial follow-up and across all four conditions, although their examination in the medication conditions was exploratory. Coping efficacy and anxious self-talk were examined in separate models.
Method
Participants
The current study included 488 youth with principal diagnoses of separation anxiety disorder (SAD), generalized anxiety disorder (GAD), or social phobia (SoP) (data from CAMS; Walkup et al., 2008). Youth were 50.4% male and ranged in age from 7 to 17 years (M = 10.72, SD = 2.80). The majority of the sample identified as White (78.9%, n = 385), followed by African American (9.0%, n = 44), Asian (2.5%, n = 12), American Indian (1.2%, n = 6), Native Hawaiian/Other Pacific Islander (0.4%, n = 2), and other (8.0%, n = 39). Around 12% of the sample identified their ethnicity as Hispanic. Approximately one fourth of the sample (n = 124) was of low socioeconomic status, as defined by a score of 3 or less on the Hollingshead Two-Factor Scale (range 0 to 5; Hollingshead, 1971). In terms of targeted anxiety disorders, 263 youth (53.9%) met criteria for SAD, 399 (81.8%) met criteria for SoP, and 382 (78.3%) met criteria for GAD. Comorbidity was common, as 55.33% participants were diagnosed with at least one other Diagnostic and Statistical Manual of Mental Disorders- 4th edition, text revision (DSM-IV-TR; American Psychiatric Association, 2000) Axis I disorder at baseline. Outside of comorbidity among the targeted anxiety disorders (GAD, SAD, SoP), the most common comorbidities were attention-deficit/hyperactivity disorder (ADHD; 10.04%, n = 49), oppositional defiant disorder (9.43%, n = 46), and obsessive-compulsive disorder (8.61%, n = 42). Sample characteristics are detailed in Kendall et al. (2010).
Recruitment occurred at six university/medical outpatient clinics. Inclusion criteria were: (1) principal diagnosis of SAD, SoP, or GAD (DSM-IV-TR criteria and Clinical Severity Rating [CSR] ≥ 4 on the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions [ADIS-IV-C/P; Silverman & Albano, 1996]); (2) IQ estimate of greater than 80; (3) no use of anti-anxiety medications prior to baseline assessment; 4) appropriateness for outpatient (versus inpatient) services. Exclusion criteria were: (1) any Axis I disorder with ADIS-IV-C/P CSR > the CSR for at least one of the disorders of interest; (2) presence of comorbid major depressive disorder, bipolar disorder, psychotic disorder, pervasive developmental disorder, unmanaged ADHD, eating disorder, or substance use disorder; (3) a concerning risk of dangerousness to self or others; (4) two failed trials of a selective-serotonin reuptake inhibitor (SSRI) or one failed trial of an adequate course of CBT; (5) school refusal behavior that involves missing more than 25% of school days in most recent term; (6) pregnancy, history of intolerance to sertraline, or a confounding medical condition; and (7) lack of fluency with English language. Youth were randomly assigned to: CBT (Coping cat; n = 139), medication (sertraline, n = 133), their combination (n = 140), or pill placebo (n = 76). Study measures were administered by independent evaluators (IEs) who were blind to treatment condition. Overall, study attrition was considered low (see Walkup et al., 2008).
Measures
Negative Affectivity Self-Statement Questionnaire (NASSQ; Ronan, Kendall, & Rowe, 1994)
The full NASSQ consists of 70 anxious and depressive self-statements. Youth rate the frequency of the thought within the past week on a scale ranging from 1 (not at all) to 5 (all the time). Items on the NASSQ are empirically derived (Ronan et al., 1994; Lerner et al., 1999). Sood and Kendall (2007) identified an anxiety subscale which was found to be valid across different age groups and a recent study (Villabø et al., 2013) found that high overall scores on the NASSQ were related to anxiety symptom severity, and that anxious but not depressive self-statements were related to anxiety. The anxiety subscale identified by Sood and Kendall was examined as a potential mediator using baseline and posttreatment scores. In the current study, Cronbach's alpha was .95 at pretreatment and .94 at posttreatment.
Coping Questionnaire, Parent and Child/Youth Versions (CQ-C/P; Kendall, 1994)
The CQ-C measures the youth’s perceptions of their abilities to cope with anxiety-provoking situations (coping efficacy). Similarly, the CQ-P measures the parent’s perceptions of their child’s ability to cope with these same situations. The CQ-C/P documents changes over time in youth’s perceived coping efficacy. Before completing the CQ, the examiner explains the task and offers a sample item. For instance, here is the example used for the CQ-C.
“Let’s be sure you know how to use the scale (from 1 to 7). Practice: You go to a restaurant with your parents, and you want to order your favorite meal, but you find out they don’t have it. Are you able to help yourself feel less upset?
Suppose you were really upset a half hour later after finishing dinner, when everyone else had forgotten about it. That would be a 1. But suppose you could quickly change your mind and find something else to order that you would like. Then that’s a 7. Or suppose you would be upset when you found out you couldn’t have what you wanted, but could enjoy your new choice once it arrived. That would be a 4.”
The examiner, based on information from the prior interview, enters the three situations that the youth finds most anxiety provoking and the CQ/measure assesses their perception of their ability to cope in such situations. In the CQ-C, youth are asked to rate their ability to cope (i.e., Are you able to help yourself feel less upset?) with the three anxiety-provoking situations that were identified during the ADIS on a scale of 1 (not at all able to help myself) to 7 (completely able to help myself). On the CQ-P, parents are asked to rate their child’s ability to cope with the same three situations, also on a scale of 1 (not at all able to help himself/herself) to 7 (completely able to help himself/herself feel comfortable). The CQ-C/P has evidenced sensitivity to treatment effects (Kendall, 1994) and retest reliability and internal consistency (Lau et al., 2010). In the current study, parent and youth reports on the CQ correlated significantly with bivariate correlation coefficients of mean scores ranging from .73 to .98 at different time points. In the present analyses, parent and youth reports at baseline and posttreatment were included as indicator variables for the same latent variable (combined).
Anxiety Disorders Interview Schedule-Child/Parent Versions (ADIS-IV-C/P; Silverman & Albano, 1996)
The ADIS-IV-C/P is a semi-structured diagnostic interview that evaluates DSM-IV-TR anxiety disorders and associated psychopathology (e.g., disruptive behavior disorders, eating disorders) in children and adolescents. Composite diagnoses are determined using information gathered from parent and youth interviews, and are based on the presence of symptom criteria and a clinical severity rating (CSR) of greater than 4, on a scale that ranges from 0-8. The psychometric properties of the ADIS-IV-C/P are documented (e.g., Silverman, Savedra, & Pina, 2001; Wood et al., 2002). CAMS IE reliability (10% of the assessments), using intraclass correlation coefficients, ranged from 0.82 to 0.88. For the current study, the ADIS-IV-C/P was administered at baseline to determine anxiety diagnoses and study eligibility.
Pediatric Anxiety Rating Scale (PARS; RUPP, 2002)
The PARS is a clinician-rated measure of anxiety in youth consisting of a checklist of 50 anxiety symptoms relating to diagnoses of SAD, SoP, and GAD. It includes seven global items that are administered to the youth and parent together. Severity ratings are made on a 6-point scale ranging from 0 (none) to 5 (extreme) based on the number and frequency of symptoms, and the extent of distress, interference with functioning, avoidance and accompanying physical symptoms. Six of the seven items were summed (the item that is not scored asks for the overall number of anxiety symptoms--which shouldn’t go into the total score because it is not independent of that score) to produce a total score with a possible range of 0 to 30. Reliability and validity of the PARS has been reported (RUPP, 2002). In the CAMS, baseline scores on the PARS ranged from 7 to 29 and inter-rater reliability among the IEs was >0.97. The current study used data from PARS administered at baseline and 3-month follow-up.
Procedures
Procedures were approved by the Institutional Review Boards at all six sites. Participants were recruited through flyers, television, radio, and internet advertisements. After eligibility was determined and informed consent/assent was provided by parents and youth, a baseline assessment determined parent and youth ratings of anxiety, comorbid problems, and youth and family functioning before randomization to treatment condition. Full assessments using parent-, youth-, and IE-rated measures were completed at baseline, posttreatment, and 3-month follow-up. Partial assessments occurred at weeks 4, 8, and 24. Measures were administered by IEs blind to treatment condition who were trained to a pre-specified reliability criterion and monitored for drift (details in Compton et al., 2010). Randomly-selected, videotaped therapy sessions were reviewed for treatment fidelity and found to have excellent correspondence with the treatment protocol.
Cognitive-behavioral therapy (CBT)
Following the Coping cat program (Kendall & Hedtke, 2006), CBT participants received 14, 60-min sessions delivered over 12 weeks. Teens received the C.A.T. Project (Kendall, Choudhury, Hudson, & Webb, 2002). Coping cat and C.A.T. Project include training in skills for managing anxiety (e.g., psychoeducation, changing views of anxiety-provoking situations, problem solving) followed by exposure tasks for anxiety-provoking situations. Parents participated in brief, weekly check-ins with the therapist plus two sessions without the youth present. Youth were assigned treatment-related homework to do between sessions. Supervision was provided weekly to therapists, both on-site and cross-sites. CBT providers were 38 doctoral candidates, social workers, psychologists, and psychiatrists. The majority were Caucasian (92%) and female (84%). Most identified their theoretical orientation as cognitive-behavioral and therapists had, on average, 5.59 years of prior clinical experience. Fifty-eight percent had a Ph.D. and 37% had a master’s degree in psychology; one had a PsyD and one was a licensed clinical social worker (see Podell et al., 2012).
Pharmacotherapy
Pharmacotherapy consisted of eight 30-60-minute sessions (weeks 1-4, 6, 8, 12) that involved discussing anxiety symptoms, overall functioning, treatment response, and adverse events in the context of supportive clinical care. Providers checked in with participants by phone during weeks when there was no in-person session. Sertraline was administered on a fixed-flexible schedule beginning with 25 mg per day and adjusted up to 200 mg per day by week 8. Adherence was assessed using pill counts and medication diaries. Providers consisted of psychiatrists and psychiatric nurses, experienced in administering pharmacotherapy to anxious youth. They received cross-site supervision every other week as well as on-site supervision each month.
Combination therapy
Combination therapy consisted of all components of the CBT and the pharmacotherapy conditions. Sessions occurred on the same day when possible, with the participants typically meeting with the pharmacotherapist first. Dose increases could be informed by input from the CBT therapist.
Statistical Analyses
Analyses were conducted using structural equation modeling (SEM) in Mplus (Muthen & Muthen, 1998 - 2010). Results are based on latent variables for coping efficacy, negative anxious self-talk, and anxiety symptoms. Parameter estimation was achieved through WLSMV, the standard weight least square parameter estimate when using categorical indicator variables for latent variables in Mplus. Missing data ranged from 1% to 23% on single variables. In contrast to other ML estimators in Mplus, WLSMV does not run a full-information-maximum-likelihood (FIML) but rather a limited-information-approach for accounting for missing data (Graham & Coffman, 2012). To ensure that the estimates in the current paper were not biased due to this missing data approach, results on all single path analyses were compared with an approach using Multiple Imputation (with 10 imputations in Mplus) before running WLSMV. Regression coefficients and standard errors did not differ significantly. All indirect effects were tested using the Model indirect command IND in Mplus.
Separate models were run for the different treatment conditions: the categorical variable (treatment condition) was recoded into three dichotomous variables: youth receiving Placebo compared to (a) CBT, (b) sertraline, and (c) their combination (COMB). Placebo was coded as 0 and the active treatment as 1. Bootstrapping with 500 replications was applied in all mediator models to derive more accurate standard errors and correct for skewness in some of the categorical indicator variables. For the current study, measurements of the hypothesized mediators immediately posttreatment and gains at 3-month follow-up were used. This both established temporal precedence of the mediator over outcome, and allowed time for an integration of the participants treatment experiences, given that improvements occur after exposure tasks.
The present results evaluated the two mediators in separate models. Testing both mediators within the same model had high inter-correlations and cross-loadings between the mediator indicator variables resulted in impaired model fit for CBT and sertraline conditions, precluding further interpretation of model estimates. For the combined condition, the main results remained the same whether mediators were examined separately or simultaneously. Thus, results are presented for models evaluating each mediator separately.
Results
Table 1 presents the means and standard deviations for coping efficacy as per youth and parent reports (CQ-C/P), anxious self-talk (NASSQ), and clinician-rated anxiety symptoms (PARS) by treatment condition. There were no significant differences between the treatment groups at baseline for anxious self-talk, coping efficacy, or anxiety symptoms. All active treatment conditions evidenced an improvement in anxiety symptoms from baseline to 3-month follow-up compared to placebo (see Table 2).
Table 1.
Descriptive statistics for measures at different time points, by reporter, per treatment condition.
| Measure | Time Point | COMB | CBT | SRT | Placebo | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |||
| NASSQ | Baseline | Y | 66.35 | 23.79 | 68.30 | 24.32 | 66.08 | 23.00 | 63.82 | 22.19 |
| NASSQ | Week 12 | Y | 43.56 | 13.77 | 45.31 | 14.10 | 43.04 | 12.71 | 45.25 | 17.39 |
| Coping efficacy | Baseline | Y | 3.07 | 1.41 | 3.25 | 1.45 | 3.32 | 1.36 | 3.15 | 1.39 |
| Coping efficacy | Week 12 | Y | 5.72 | 1.19 | 5.24 | 1.22 | 5.33 | 1.44 | 4.81 | 1.38 |
| Coping efficacy | Baseline | P | 2.39 | 0.97 | 2.56 | 1.18 | 2.66 | 1.10 | 2.73 | 1.28 |
| Coping efficacy | Week 12 | P | 5.57 | 1.07 | 4.91 | 1.21 | 4.98 | 1.45 | 4.24 | 1.26 |
| Anxiety symptoms | Baseline | IE | 19.54 | 3.86 | 19.01 | 4.27 | 18.76 | 4.34 | 19.43 | 4.39 |
| Anxiety symptoms | Week 24 | IE | 6.22 | 5.14 | 8.38 | 6.18 | 8.03 | 6.63 | 11.63 | 6.70 |
Note: NASSQ = Negative Affectivity Self-Statements Questionnaire; Coping efficacy = Coping Questionnaire; COMB = combined treatment; SRT = sertraline; CBT = cognitive-behavioral therapy; Y = Youth; P = Parent; IE = Independent Evaluator; Baseline = Pretreatment; Week 12 = Posttreatment; Week 24 = 3-month follow-up.
Table 2.
Unstandardized regression coefficients,standard errors, and 95% confidence intervals (CI) for mediator models.
| Mediator variable (M) = |
Coping efficacy at 12 weeks | Anxious self-talk at 12 weeks | ||||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | P | 95% CI | Estimate | SE | p | 95% CI | |
| Independent variable = Placebo vs. CBT, Dependent variable = PARS | ||||||||
|
| ||||||||
| Model without mediator |
||||||||
| CBT → PARS (c) | −.44 | .18 | .02 | [−.79, −.08] | −.44 | .18 | .02 | [−.79, −.08] |
| R2Y | .21 | .21 | ||||||
|
| ||||||||
| Model with mediator | ||||||||
| CBT → M (a) | .36 | .12 | .003 | [.13, .60] | .14 | .10 | .16 | [−.06, .34] |
| M → PARS (b) | −.49 | .16 | .002 | [−.81, −.17] | −.19 | .14 | .17 | [−.45, .08] |
| CBT → PARS (c′) | −.26 | .19 | .16 | [−.62, .10] | −.42 | .16 | .01 | [−.74, −.09] |
| Indirect effect (a×b) |
−.18 | .08 | .03 | [−.34, −.02] | −.03 | .03 | .32 | [−.08, .03] |
| R2y | .42 | .24 | ||||||
|
| ||||||||
| Independent variable = Placebo vs. SRT, Dependent variable = PARS | ||||||||
|
| ||||||||
| Model without mediator |
||||||||
| SRT → PARS (c) | −.49 | .16 | .002 | [−.81, −.17] | −.49 | .16 | .002 | [−.81, −.17] |
| R2Y | .25 | .25 | ||||||
|
| ||||||||
| Model with mediator | ||||||||
| SRT → M (a) | .39 | .12 | .001 | [.16, .61] | .10 | .11 | .36 | [−.11, .30] |
| M → PARS (b) | −.65 | .14 | .000 | [−.92, −.38] | −.21 | .14 | .13 | [−.48, .06] |
| SRT → PARS (c′) | −.24 | .15 | .12 | [−.54, .06] | −.48 | .17 | .004 | [−.81, −.15] |
| Indirect effect (a×b) |
−.25 | .09 | .005 | [−.43, −.08] | −.02 | .03 | .43 | [−.07, .03] |
| R2y | .45 | .29 | ||||||
|
| ||||||||
| Independent variable = Placebo vs. COMB, Dependent variable = PARS | ||||||||
|
| ||||||||
| Model without mediator |
||||||||
| COMB → PARS (c) |
−.81 | .20 | .000 | [-1.20, −.42] | −.81 | .20 | .000 | [−1.20, −.42] |
| R2y | .25 | .25 | ||||||
|
| ||||||||
| Model with mediator | ||||||||
| COMB → M (a) | .88 | .13 | .000 | [.64, 1.13] | .09 | .11 | .39 | [−.12, .30] |
| M → PARS (b) | −.37 | .10 | .000 | [−.56, −.18] | −.13 | .11 | .26 | [−.34, .09] |
| COMB → PARS (c′) |
−.48 | .20 | .02 | [−.87, −.09] | −.80 | .17 | .000 | [−1.13, −.47] |
| Indirect effect (a×b) |
−.33 | .09 | .000 | [−.50, −.16] | −.01 | .02 | .51 | [−.05, .02] |
| R2y | .35 | .28 | ||||||
Note: Child gender and age were included as covariates in all models. COMB = combined treatment; SRT = sertraline; CBT = cognitive-behavioral therapy; PARS = Pediatric Anxiety Rating Scale; Baseline = Pretreatment; Week 12 = posttreatment; Week 24 = 3-month follow-up.
Measurement Model
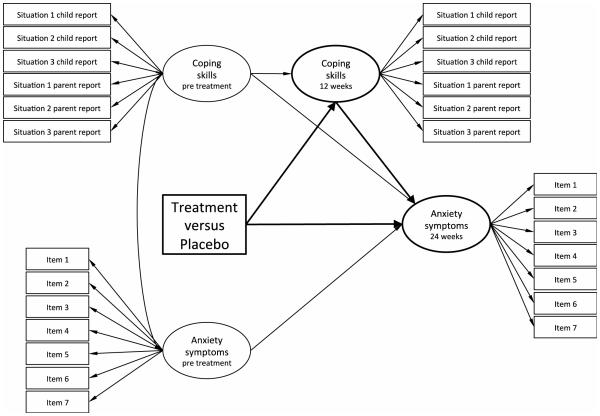
Figure 1 illustrates the measurement model that forms the basis of the mediator models run to examine coping efficacy as a potential mediator. Latent variables for youth baseline coping efficacy and posttreatment coping efficacy were created with six categorical indicator variables each, including all three items from the parent report and all three items from the youth report on the CQ. All factor loadings were significant ranging from .45 to .78, with two factor loadings < .50. Latent variables for youth anxiety symptoms at baseline and at 3-month follow-up were created with seven categorical indicator variables each, all items from the PARS. All factor loadings were significant ranging from .44 to .91, with two factor loading < .50. Relevant model fit indices indicated good model fit (RMSEA =.05; CFI = .95 - .97).
Figure 1.
Exemplified illustration of measurement model and regression paths for all mediator models including coping efficacy as mediator. Baseline = Pretreatment; Week 12 = posttreatment; Week 24 = 3-month follow-up.
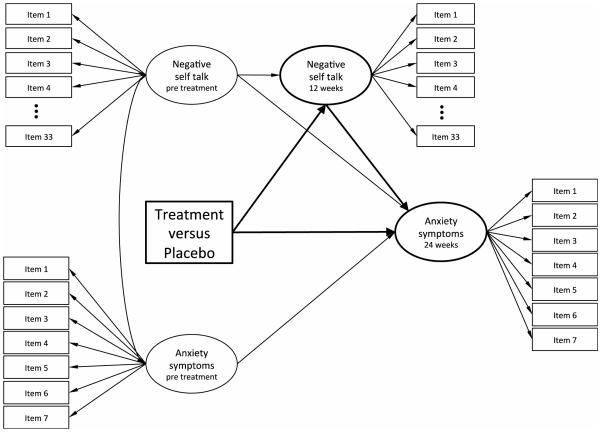
In similar but separate analyses, anxious self-talk was tested as a mediator on youth anxiety symptoms (see Figure 2; measurement model for all mediator models). Latent variables for anxious self-talk at baseline and at posttreatment were constructed using the 33 indicator items on the NASSQ that form the Anxiety scale (Sood & Kendall, 2007). All factor loadings were significant ranging from .47 to .90, with only one factor loading < .50. Relevant model fit indices indicated good model fit (RMSEA =.03; CFI = .95 - .97).
Figure 2.
Exemplified illustration of measurement model and regression paths for all mediator models including anxious self-talk as mediator. Baseline = Pretreatment; Week 12 = posttreatment; Week 24 = 3-month follow-up.
Mediation Analyses of Coping Efficacy
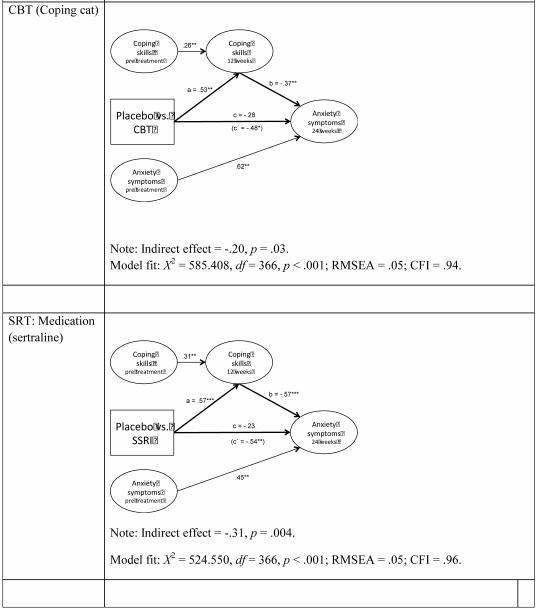
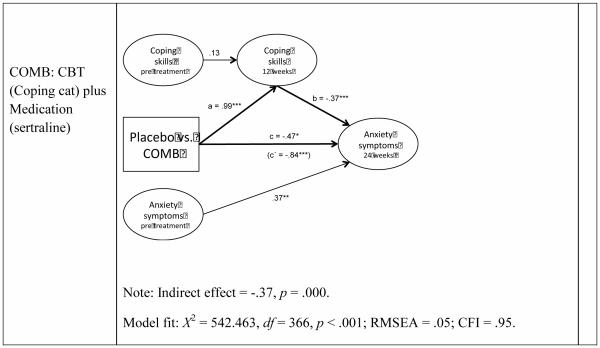
Figure 1 shows all regression paths that were included in the mediation models (youth gender and age were covariates in all models). By regressing anxiety (PARS) at 3-month follow-up (24 weeks) on anxiety symptoms at baseline (pretreatment), the outcome variable is interpreted as the residualized change (change) in anxiety between these two time points. Figure 3 displays simplified versions of mediation models testing whether coping efficacy at posttreatment mediates residualized gains on the PARS at 3-month follow-up. Figures include partially standardized regression coefficients and indirect effects (standardized for latent variables only) as well as model fit. Table 2 (left column) shows unstandardized regression coefficients, standard errors, and confidence intervals for mediation models including coping efficacy as mediator. .
Figure 3.
Mediator models testing the effect of treatment on anxiety symptoms via change in coping efficacy
Note: The illustrations are simplified. For the complete mediator models, including indicator variables and regression paths, see Figure 1. Regression coefficients are partially standardized (standardized on latent variables only). Numbers in parentheses represent regression coefficients for treatment effects before including the mediator. Youth gender and age were included as covariates in all models. Baseline = Pretreatment; Week 12 = posttreatment; Week 24 = 3-month follow-up.
CBT condition
The model tested whether changes in coping efficacy at posttreatment mediated the effects of CBT on change in anxiety symptoms (see Figure 3). This model showed an acceptable fit. The indirect path from treatment condition to coping efficacy to anxiety symptoms was significant, implying that the effect of treatment condition on change in anxiety symptoms was mediated by increased coping efficacy. In addition, Table 2 demonstrates that the treatment condition significantly predicted change in coping efficacy, indicating that youth in the CBT treatment showed greater improvement in coping efficacy compared to youth in the placebo condition (Path a). An increase in coping efficacy predicted a significant reduction in anxiety symptoms, indicating that increased coping efficacy were associated with greater reduction in anxiety symptoms at 3-month follow-up (Path b). CBT had a significant effect on the reduction of anxiety symptoms before including coping efficacy as a mediator in the model (Path c). When controlling for the change in coping efficacy in the mediator model, the treatment no longer had a significant effect on anxiety symptoms (Path c’), suggesting that the mediator, coping efficacy, accounted for the previously found treatment gains.
Sertraline condition
Model 2 tested whether change in coping efficacy mediated the effects of sertraline on change in anxiety symptoms (see Figure 3). This model showed an acceptable fit. The indirect path from treatment condition to anxiety symptoms via coping efficacy was significant, suggesting that the effect of treatment condition on anxiety symptoms was mediated by increased coping efficacy. In addition, Table 2 shows that the treatment condition predicted change in coping efficacy at posttreatment (Path a), indicating that youth in the sertraline condition showed greater improvement in coping efficacy compared to youth in the placebo condition. An increase in coping efficacy predicted a significant reduction in anxiety symptoms (Path b). Youth who showed better coping efficacy were reported as having fewer anxiety symptoms at 3-month follow-up. Sertraline had a significant effect on the reduction of anxiety symptoms before including coping efficacy as a mediator in the model (Path c). When controlling for the change in coping efficacy in the mediator model, the treatment no longer had a significant effect on anxiety symptoms (Path c’), suggesting that the mediator, coping efficacy, accounted for the previously found treatment gains.
Combined treatment
The third model tested whether changes in coping efficacy mediated the effects of the combined treatment on change in anxiety symptoms (Figure 3). The model showed an acceptable fit. The indirect path from treatment condition to anxiety symptoms via coping efficacy was significant, suggesting that coping efficacy is a significant mediator of treatment gains. In addition, Table 2 shows that the combined treatment predicted change in coping efficacy at posttreatment (Path a), indicating that youth who received the combined treatment showed greater improvement in coping efficacy compared to youth in the placebo condition. Again, increase in coping efficacy predicted a significant reduction in anxiety symptoms (Path b), indicating that greater coping efficacy was associated with greater reduction in anxiety symptoms. The combined treatment had a significant effect on the reduction of anxiety symptoms before including coping efficacy as a mediator in the model (Path c). This time, when controlling for the change in coping efficacy in the mediator model, treatment effects on anxiety symptoms remained significant though significantly reduced (Path c’). This suggests that the mediator, coping efficacy, accounted for only some variation in the previously found treatment gains, but that some variation is still attributable to a unique effect of treatment condition.
Mediation Analyses of Anxious Self-Talk
Table 2 (right column) shows unstandardized regression coefficients, standard errors, and 95% confidence intervals for all mediation models including anxious self-talk as mediator. The coefficients in Figure 3 are partially standardized (standardized on latent variables only). Youth age and gender were included as covariates in all mediation models.
For all three treatment conditions, the indirect path from treatment condition to anxiety symptoms via anxious self-talk was not significant, indicating that anxious self-talk is not a mediator of residualized treatment gains. None of the treatment conditions predicted a significant reduction in anxious self-talk (see Table 2, path a). Further, change in anxious self-talk throughout the treatment did not predict any significant changes in anxiety symptoms (path b). Treatment effects on the youth's anxiety symptoms were not significantly reduced when including anxious self-talk as a mediator in the model (compare paths c and c’).
Discussion
The current study examined two variables, residualized changes in coping efficacy and anxious self-talk, as potential mediators of residualized treatment gains for anxiety disorders in youth. Given that data from 3-months posttreatment were included, the gains being referred to can be viewed as “change following treatment.” Findings indicated that improvements in residualized change in coping efficacy mediated gains seen at 3-month follow-up in both the CBT and the sertraline conditions. Similarly measured coping efficacy also mediated treatment gains in the combined condition, but unique effects of the treatment remained. Contrary to hypotheses and in contrast to previous findings (e.g., Kendall & Treadwell, 2007), residualized changes in anxious self-talk did not mediate change in anxiety symptoms in the present study. These findings suggest that improvement in coping efficacy is one active mechanism within both CBT and medication treatments for anxiety disorders in youth.
Residualized changes in coping efficacy were found to mediate change in the combined, CBT, and sertraline conditions when compared with placebo. These findings are consistent with those of Lau et al. (2010) and Hogendoorn et al. (2013). Lau et al. (2010) also found that youth and parent responses on the same measure of coping efficacy (i.e., Coping Questionnaire) mediated treatment outcome for CBT. Similarly, Hogendoorn and colleagues (2013) reported that coping mechanisms including problem-solving and distraction were potential treatment mediators. The current study builds upon these findings by both establishing temporal precedence and using a control condition. Although coping as mediator has been a relatively understudied area when compared to cognitive mediators (see Chu & Harrison, 2007), the present findings buttress the potentially important role of an individual’s perception of their coping ability as an active mechanism of change. As youth come to see themselves as being able to cope with (rather than avoid) challenging situations, their symptoms are reduced. Prins and Ollendick (2003) found that coping, when examined as a CBT outcome, demonstrated a higher effect size than cognitive change and they highlighted the importance of learning active coping strategies in CBT. Exposure tasks are considered among the most important components of CBT for anxiety disorders--in part because youth learn and practice strategies to cope with their anxiety. Our findings are consistent with the notion that improved coping efficacy is one process in effective treatment of anxiety in youth.
Interestingly, residualized change in coping efficacy also mediated gains that were found in both conditions that included medication (i.e., the sertraline and combined conditions). In what ways could the notion of improved coping efficacy mediate pharmacotherapy? It’s possible that, as a youth’s anxiety symptoms are reduced through pharmacotherapy, he or she is more likely to actively engage in previously avoided situations. Once he/she gains experience with these formerly anxiety-provoking situations, his/her coping efficacy improves, and his/her overall anxiety reduces. In this way, improvements in one’s sense of coping efficacy could be an important process in pharmacotherapy. For the combined condition, some unique effect of treatment remained, in sync with the CAMS finding that the combined treatment was stronger than either of the monotherapies (Walkup et al., 2008). Consistent with the current findings, other treatment processes beyond coping efficacy might account for the added effect of the combined treatment (e.g., the synergistic effect of pharmacologic and psychosocial treatments; physiological changes). These processes warrant exploration.
In contrast, residualized change in anxious self-talk was not associated with reduction in anxiety symptoms. These findings suggest that, in the present sample, reduction in anxious self-talk was not a mechanism of change. This finding was surprising, given the emphasis that CBT places on cognitive change (see also Dozois & Quilty, 2014), including identifying anxious thoughts and the use of coping thoughts. Indeed, previous research had found that (a) anxious self-talk differentiated between anxious and non-anxious youth (Sood & Kendall, 2007), (b) reductions in anxiogenic cognitions were related to improvements in anxiety symptoms (Muris et al., 2009), and (c) changes in cognition were mediators of symptom change (Chu & Harrison; Davis & Ollendick; Hogendoorn et al., 2013; Peris et al., in press; Prins & Ollendick, 2003). In three previous studies, anxious self-talk measured by the NASSQ was found to mediate change associated with CBT (Treadwell & Kendall, 1996; Kendall & Treadwell, 2007; Lau et al., 2010). Hogendoorn et al. (2013) reported that increases in positive thoughts, but not decreases in negative thoughts, were potential mediators of CBT treatment for anxious youth. There are possible explanations related to the timing of the measurement of the mediator and the outcome variables. Previous studies that supported anxious self-talk as a potential treatment mediator did not establish temporal precedence, such that changes in anxious self-talk were measured simultaneously with treatment outcome. The present study measured treatment gains 3 months after treatment. Therefore, it is possible that in previous studies, reductions in NASSQ were associated with reductions in anxiety symptoms, but that this was not a causal relationship. In other words, reductions in anxious self-talk may have been associated with reductions in anxiety because anxious self-talk is a symptom of anxiety, but not necessarily a mediator of treatment. Also, the present outcome measure was the PARS, a clinician/IE-administered semi-structured interview. Previous studies used primarily child- and parent-report measures as outcome variables. Given that cognition is an internal experience, changes in anxious self-talk may be more apparent on a self-report measure than an interview such as the PARS. It is also possible that prior findings indicating that changes in self-talk mediate pre-post treatment changes are accurate but, as in the present case, such mediation does not hold for residualized changes assessed at 3-month follow-up. Additional research is needed with an emphasis on the timing of the potential mediators of therapeutic change.
Potential limitations merit consideration. First, coping efficacy was measured combining parent and youth report, whereas anxious self-talk relied on youth-report. That said, self-talk is an internal experience, so parents could not be expected to accurately report on their child’s self-talk. Still, whether anxious self-talk was confounded with anxiety symptoms must be considered (Prins & Ollendick, 2003; Rietveld, Prins, & van Beest, 2002). Also, although some psychometric properties of the Coping Questionnaire have been reported (Kendall, 1994; Lau et al., 2010), additional psychometric analyses (e.g., predictive criterion-related validity) are needed. For example, the Coping Questionnaire assesses youth- and parent-reported coping efficacy, whereas the development of observational measures to assess actual coping behaviors would provide valuable data. Second, the construct of anxious elf-talk overlaps to some degree with definitions of anxiety, and this overlap could detract from examining its role as a moderator. Third, additional services or medication during the follow-up period was not controlled. Fourth, the manual-based CBT was delivered by trained/supervised therapists and was found to be efficacious. Some have noted differences between services delivered in research settings compared to those provided in community practice settings (McLeod et al, 2014; Weisz, Donenberg, Weiss, & Han, 1995), and it is possible that mediators of change could differ across settings. Such a possibility is consistent with findings that the observer-rated therapeutic alliance was higher in a research setting than in practice settings (McLeod, Jensen-Doss, Tully, Southam-Gerow, Weisz, & Kendall, 2014). CAMS consisted of mostly white therapists and youth from middle class families with moderate to severe anxiety, so the findings cannot be generalized to other groups. On balance, relevant therapist variables (e.g., experience, treatment adherence, and collaborative style) varied among CAMS therapists (Podell et al., 2013).
Considering that therapeutic procedures and processes may differ from the research clinic to the community practice setting, studies of mechanisms of action in the real world are needed (Weersing & Weisz, 2002). Mediational pathways can be bidirectional, multi-causal, reciprocal, and complex (Kazdin & Nock, 2003) such that, once a mediator is identified, a next step may be to test a treatment that is enhanced by an emphasis on the mediator against the original treatment (Chu & Harrison, 2007). Such a comparison would offer experimental evidence regarding active mechanisms of change. Further, there is the need to include well-timed assessments that allow for the exploration of mediators during the course of treatment and to consider treatment mediators among minority populations (e.g., Silverman, Pina, & Viswesvaran, 2008), across varying modes of treatment delivery and formats (Chu et al., 2004), and when therapy is combined with medication.
Clinical Implications
CAMS offered a promising take home message: CBT (Coping cat), pharmacotherapy with SSRIs (sertraline), and their combination are effective treatments for anxiety in youth (e.g., Walkup et al, 2008). The current study used data from CAMS (a large, multi-site trial) that included multiple time points to measure mediators. Improvements in coping efficacy appear to be an important mechanism of change, where change in self-talk may not be as important as previously thought. It appears that children and adolescents benefit from a treatment that focuses on active coping strategies to managing anxiety, a strategy that enhances coping self-efficacy. Exposure tasks are an essential component of CBT for youth anxiety (e.g., Kendall et al., 2005), and this may be, in part, because they can lead to the realization that coping skills are available. Our findings suggest that therapists may want to emphasize available coping skills with the child, prior to, during, and after exposure tasks, to influence the child’s coping self-efficacy. Future research can examine the components of exposure that are most potent in terms of a child’s coping efficacy. For instance, post-event processing of an exposure task, during which a child’s ability to cope with the feared stimulus is discussed, has been found to predict a positive treatment outcome, whereas preparation for the exposure task did not (Tiwari et al., 2013).
Although there is a valued emphasis on the dissemination of evidence-based treatments (EBTs) in the community, there remains the need to ensure fidelity to the essential “ingredients” of EBTs. Exposure tasks may be underutilized (Becker, Zayfert, & Anderson, 2004), with research showing that they are the least frequently implemented component of the Coping Cat protocol by community-based therapists (Chu, Crocco, Arnold, Brown, Southam-Gerow, & Weisz, 2014). The present findings underscore the need for continued dialogue regarding the implementation of essential EBT components, such as exposure tasks, in the community.
Public Health Significance.
These findings suggest that, within empirically supported treatments for anxiety in youth, the youth’s self-perceived ability to manage anxiety provoking situations plays a role in beneficial change.
Acknowledgments
This research was supported by an NIMH grants (MH063747 to Kendall; MH64003 to Birmaher; MH64003 to Compton; MH 64088 to Piacentini; MH64089 to Walkup; MH64092 to Albano). The authors thank David Kenny for his contributions.
Dr. Kendall receives royalties from sales of treatment materials related to anxiety in youth. He publishes and distributes the program that was included in the study.
Dr. Birmhaer receives royalties from American Psychiatric Association, Random House, UpToDate.
Dr. Piacentini receives research support from Pfizer Pharmaceuticals, Pettit Foundation, Tourette Association of America; publication royalties from Oxford University Press and Guilford Press; travel support and speaking honoraria from Tourette Association, International OCD Foundation; speaking honoraria from Trichtillomania Learning Center.
Dr. Walkup has received free drug/placebo from the following pharmaceutical companies for National Institute of Mental Health funded studies Eli Lilly (2003), Pfizer (2007), Abbott (2005). Dr. Walkup was paid for a one time consultation with Shire (2011). Dr. Walkup is a paid speaker for the Tourette Syndrome – Center for Disease Control and Prevention outreach educational programs; American Academy of Child and Adolescent Psychiatry, American Psychiatric Association. Dr. Walkup receives royalties for books on Tourette syndrome from Guilford Press and Oxford Press. Dr. Walkup receives grant funding from the Hartwell Foundation and the Tourette Syndrome Association, and is an unpaid advisor to Anxiety Disorders Association of America, Consumer Reports, and Trichtillomania Learning Center.
Footnotes
Views expressed within this article represent those of the authors and are not intended to represent the position of NIMH, NIH, or DHHS.
References
- Albano AM, Kendall PC. Cognitive behavioral therapy for children and adolescents with anxiety disorders: Clinical research advances. International Review of Psychiatry. 2002;14:129–124. doi:10.1080/09540260220132644. [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 4th. Author; Washington, D.C.: 2000. text rev. [Google Scholar]
- Angold A, Costello E, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. doi:10.1111/1469-7610.00424. [PubMed] [Google Scholar]
- Barlow DH. Anxiety and its disorders. 2nd Guilford Press; New York: 2002. [Google Scholar]
- Barrett P, Farrell L, Pina A, Peris T, Piacentini J. Evidence-based psychosocial treatments for child and adolescent obsessive-compulsive disorder. Journal of Clinical Child and Adolescent Psychology. 2008;37:131–155. doi: 10.1080/15374410701817956. doi: 10.1080/15374410701817956. [DOI] [PubMed] [Google Scholar]
- Becker CB, Zayfert C, Anderson E. A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behavior Research & Therapy. 2004;42:277–92. doi: 10.1016/S0005-7967(03)00138-4. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Monk K, Kalas C, Clark D, Ehmann, Brent B. Fluoxetine for the treatment of childhood anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:415–23. doi: 10.1097/01.CHI.0000037049.04952.9F. doi:10.1097/01.CHI.0000037049.04952.9F. [DOI] [PubMed] [Google Scholar]
- Bouchard S, Mendlowitz S, Coles M, Franklin M. Considerations in the use of exposure with children. Cognitive and Behavioral Practice. 2004;11:56–65. doi: 10.1016/S1077-7229(04)80007-5. [Google Scholar]
- Cannon MF, Weems CF. Cognitive biases in childhood anxiety disorders: Do interpretive and judgment biases distinguish anxious youth from their non-anxious peers? Journal of Anxiety Disorders. 2010;24:751–758. doi: 10.1016/j.janxdis.2010.05.008. Doi: 10.1016/j.janxdis.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavira D, Stein M, Bailey K, Stein M. Comorbidity of generalized social anxiety disorder and depression in a pediatric primary care sample. Journal of Affective Disorders. 2004;80:163–171. doi: 10.1016/S0165-0327(03)00103-4. doi:10.1016/S0165-0327(03)00103-4. [DOI] [PubMed] [Google Scholar]
- Chu BC, Choudhury MS, Shortt A, Pincus D, Creed T, Kendall PC. Alliance, technology, and outcome in the treatment of anxious youth. Cognitive and Behavioral Practice. 2004;11:44–55. [Google Scholar]
- Chu BC, Harrison T. Disorder-specific effects of CBT for anxious and depression youth: A meta-analysis of candidate mediators of change. Clinical Child and Family Psychological Review. 2007;10:352–372. doi: 10.1007/s10567-007-0028-2. doi: 10.1007/s10567-007-0028-2. [DOI] [PubMed] [Google Scholar]
- Chu BC, Crocco S, Arnold C, Brown R, Southam-Gerow M, Weisz J. Sustained implementation of cognitive-behavioral therapy for youth anxiety and depression: Long-term effects of structured training and consultation on therapist practice in the field. Professional Psychology: Research & Practice. 2014 doi: 10.1037/a0038000. Online first publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen A, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127:87–127. doi:10.1037/0033-2909.127.1.87. [PubMed] [Google Scholar]
- Compton S, Walkup J, Albano AM, Piacentini J, Birmaher B, Sherrill J, March J. Child/Adolescent Anxiety Multimodal Treatment Study (CAMS): Rationale, design, and methods. Child and Adolescent Psychiatry and Mental Health. 2010;4:1. doi: 10.1186/1753-2000-4-1. doi:10.1186/1753-2000-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello E, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and Development of Psychiatric Disorders in Childhood and Adolescence. Archives of General Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. doi:10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Creswell C, Murray L, Cooper P. Interpretation and expectation in childhood anxiety disorders: Age effects and social specificity. Journal of Abnormal Child Psychology. 2014;42:453–465. doi: 10.1007/s10802-013-9795-z. doi: 10.1007/s10802-013-9795-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings C, Caporino N, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological Bulletin. 2014;140:816–845. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis T, Ollendick TH. Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response? Clinical Psychology: Science and Practice. 2005;12:144–160. doi: 10.1093/dipsy/bpi018. [Google Scholar]
- Dozois DJA, Quilty LC. Cognitive mechanisms of change in the treatment of depression. International Journal of Cognitive Therapy. 2014;7:211–216. [Google Scholar]
- Fox J, Houston B, Pittner M. Trait anxiety and children's cognitive behaviors in an evaluative situation. Cognitive Therapy and Research. 1983;7:149–154. doi:10.1007/BF01190068. [Google Scholar]
- Graham JW, Coffman DL. Structural equation modeling with missing data. In: Hoyle RH, editor. Handbook of structural equation modeling. Guilford Press; New York: 2012. pp. 277–295. [Google Scholar]
- Heard P, Dadds M, Rapee R. Modified Australian version of Kendall’s treatment program for anxious children. University of Queensland; Brisbane, Australia: 1991. The Coping Koala workbook. [Google Scholar]
- Hogendoorn S, Prins P, Boer F, Vervoort L, Wolters L, Moorlag H, Nauta M, de Haan E. Mediators of cognitive behavioral therapy for anxiety-disordered children and adolescents: Cognitive, perceived control, and coping. Journal of Clinical Child and Adolescent Psychology. 2013 doi: 10.1080/15374416.2013.807736. doi: 10.1080/15374416.2013.807736. [DOI] [PubMed] [Google Scholar]
- Hogendoorn S, Wolters L, Vervoot L, Prins P, Boer F, Kooij E, De Haan E. Measuring negative and positive thoughts in children: An adaptation of the Children’s Automatic Thoughts Scale (CATS) Cognitive Therapy and Research. 2010;34:467–478. doi: 10.1007/s10608-010-9306-2. doi: 10.1007/s10608-010-9306-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Commentary on the indiscriminate state of social class measurement. Social Forces. 1971;49:563–567. doi: 10.2307/2576737. [Google Scholar]
- Hollon S, Beck AT. Cognitive and cognitive-behavioral therapies. In: Lambert M, editor. Handbook of Psychotherapy and Behavior Change. Wiley; New York: 2013. pp. 393–442. [Google Scholar]
- Kazdin A, Nock M. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. doi:10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kazdin A, Weisz J. Identifying and developing empirically supported child and adolescent treatments. Journal of Consulting and Clinical Psychology. 1998;66:100–110. doi: 10.1037//0022-006x.66.1.19. doi:10.1037=0022-006X.66.1.19. [DOI] [PubMed] [Google Scholar]
- Kearney CA. Social anxiety and social phobia in youth: Characteristics, assessment, and psychological treatment. Springer; New York: 2005. [Google Scholar]
- Kendall PC. Behavioral assessment and methodology. In: Wilson GT, Franks CM, Braswell KD, Kendall PC, editors. Annual review of behavior therapy: Theory and practice. Vol. 9. Guilford Press; New York: 1984. pp. 39–94. [Google Scholar]
- Kendall PC. Treating anxiety disorders in children: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 1994;62:100–110. doi: 10.1037//0022-006x.62.1.100. doi:10.1037/0022-006X.62.1.100. [DOI] [PubMed] [Google Scholar]
- Kendall PC. Treating anxiety disorders in youth. In: Kendall PK, editor. Child and adolescent therapy: Cognitive-behavioral procedures. 4th Guilford Press; New York: 2012. [Google Scholar]
- Kendall PC, Choudhury M, Hudson J, Webb A. The C.A.T. project therapist manual. Workbook Publishing; Ardmore, PA: 2002. [Google Scholar]
- Kendall PC, Comer JS, Chow C. The randomized controlled trial: Basics and beyond. In: Comer JS, Kendall PC, editors. The Oxford handbook of research strategies for clinical psychology. Oxford University Press; New York: 2013. pp. 40–61. [Google Scholar]
- Kendall PC, Compton S, Walkup J, Birmaher B, Albano AM, Sherrill J, Piacentini J. Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders. 2010;24:360–5. doi: 10.1016/j.janxdis.2010.01.009. doi:10.1016/j.janxdis.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel S, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:366–380. doi: 10.1037//0022-006x.65.3.366. doi:10.1037/0022-006X.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hedtke K. Cognitive-behavioral therapy for anxious children: Therapist manual. 3rd Workbook Publishing; Ardmore, PA: 2006. [Google Scholar]
- Kendall PC, Hudson J, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. doi:10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Robin J, Hedtke K, Suveg C, Flannery-Schroeder E, Gosch E. Considering CBT with anxious youth? Think exposures. Cognitive and Behavioral Practice. 2005;12:136–150. doi:10.1016/S1077-7229(05)80048-3. [Google Scholar]
- Kendall PC, Treadwell KRH. The role of self-statements as a mediator in treatment for youth with anxiety disorders. Journal of Consulting and Clinical Psychology. 2007;75:380–389. doi: 10.1037/0022-006X.75.3.380. doi: 10.1037/0022-006X.75.3.380. [DOI] [PubMed] [Google Scholar]
- Lang PJ. A bio-informational theory of emotional imagery. Psychophysiology. 1979;16:495–512. doi: 10.1111/j.1469-8986.1979.tb01511.x. doi:10.1111/j.1469-8986.1979.tb01511.x. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Cuthbert BN, Bradley MM. Measuring emotion in therapy: Imagery, activation, and feeling. Behavior Therapy. 1998;29:655–674. doi:10.1016/S0005-7894(98)80024-5. [Google Scholar]
- Lau W, Chan C, Li JC, Au T. Effectiveness of group cognitive-behavioral treatment for childhood anxiety in community clinics. Behaviour Research and Therapy. 2010;48:1067–1077. doi: 10.1016/j.brat.2010.07.007. [DOI] [PubMed] [Google Scholar]
- Lerner J, Safren S, Henin A, Warman M, Heimberg R, Kendall PC. Differentiating anxious and depressive self-statements in youth: factor structure of the Negative Affect Self-Statement Questionnaire among youth referred to an anxiety disorders clinic. Journal of Clinical Child Psychology. 1999;28:82–93. doi: 10.1207/s15374424jccp2801_7. [DOI] [PubMed] [Google Scholar]
- Lopez B, Turner R, Saavedra L. Anxiety and risk for substance dependence among late adolescents/young adults. Journal of Anxiety Disorders. 2005;19:275–294. doi: 10.1016/j.janxdis.2004.03.001. doi:10.1016/j.janxdis.2004.03.001. [DOI] [PubMed] [Google Scholar]
- MacKinnon D, Fairchild A, Fritz M. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. doi:10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod BD, Jensen-Doss A, Tully C, Southam-Gerow M, Weisz j., Kendall PC. The role of setting and treatment modality on the therapeutic alliance in treatment of youth anxiety. 2014 Manuscript submitted for publication. [Google Scholar]
- Mineka S, Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: It's not what you thought it was. American Psychologist. 2006;61:10–26. doi: 10.1037/0003-066X.61.1.10. doi:10.1037/0003-066X.61.1.10. [DOI] [PubMed] [Google Scholar]
- Muris P, Mayer B, den Adel M, Roos T, van Wamelen J. Predictors of change following cognitive-behavioral treatment of children with anxiety problems: A preliminary investigation on negative automatic thoughts and anxiety control. Child Psychiatry and Human Development. 2009;40:139–151. doi: 10.1007/s10578-008-0116-7. doi: 10.1007/s10578-008-0116-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus. Statistical Analyses with Latent Variables. User's Guide. Muthen & Muthen; Los Angeles: 1998 – 2010. [Google Scholar]
- Nauta M, Scholing A. Dappere Kat: Cognitieve gedragstherapie bij kinderen en jongere: een protocol van 12 sessies [Adaption of the Coping Cat: Cognitive Behavioral Therapy with children and adolescents] University of Groningen; Groningen, the Netherlands: 2007. [Google Scholar]
- Peris T, Compton S, Kendall P, Birmaher B, Sherrill J, March J, Gosch E, Ginsburg G, Rynn M, McCracken J, Keeton C, Sakolsky D, Suveg C, Aschenbrand S, Almirall D, Iyengar S, Walkup J, Albano AM, Piacentini J. Trajectories of change in youth anxiety during cognitive behavior therapy. Journal of Consulting and Clinical Psychology. 2015;83:239–252. doi: 10.1037/a0038402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podell JL, Kendall PC, Gosch E, Compton S, March J, Albano A, Piacentini JC. Therapist factors and outcomes in CBT for anxiety in youth. Professional Psychology: Research and Practice. 2013;44:89–98. doi: 10.1037/a0031700. doi:10.1037/a0031700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins P, Hanewald G. Self-statements of test-anxious children: Thought-listing and questionnaire approaches. Journal of Consulting and Clinical Psychology. 1997;65:440–447. doi: 10.1037//0022-006x.65.3.440. doi:10.1037/0022-006X.65.3.440. [DOI] [PubMed] [Google Scholar]
- Prins P, Ollendick TH. Cognitive change and enhanced coping: Missing mediational links in cognitive behavior therapy with anxiety-disordered child. Clinical Child and Family Psychology Review. 2003;6:87–105. doi: 10.1023/a:1023730526716. [DOI] [PubMed] [Google Scholar]
- The Research Units on Pediatric Psychopharmacology Anxiety Study Group The Pediatric Anxiety Rating Scale (PARS): Development and psychometric properties. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:1061–1069. doi: 10.1097/00004583-200209000-00006. doi: 10.1097/00004583-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Rietveld S, Prins PM, van Beest I. Negative thoughts in children with symptoms of anxiety and depression. Journal of Psychopathology and Behavioral Assessment. 2002;24:107–113. doi:10.1023/A:1015340808609. [Google Scholar]
- Ronan KR, Kendall PC, Rowe M. Negative affectivity in children: Development and validation of a self-statement questionnaire. Cognitive Therapy and Research. 1994;18:509–528. [Google Scholar]
- Schniering C, Rapee R. Development and validation of a measure of children's automatic thoughts: The Children's Automatic Thoughts Scale. Behaviour Research and Therapy. 2002;40:1091–1109. doi: 10.1016/s0005-7967(02)00022-0. doi:10.1016/S0005-7967(02)00022-0. [DOI] [PubMed] [Google Scholar]
- Schniering C, Rapee R. The relationship between automatic thoughts and negative emotions in children and adolescents: A test of the cognitive content-specificity hypothesis. Journal of Abnormal Psychology. 2004;113:464–470. doi: 10.1037/0021-843X.113.3.464. doi:10.1037/0021-843X.113.3.464. [DOI] [PubMed] [Google Scholar]
- Rynn M, Siqueland L, Rickels L. Placebo controlled trial of sertraline in the treatment of children with generalized anxiety disorder. American Journal of Psychiatry. 2001;158:2008–2014. doi: 10.1176/appi.ajp.158.12.2008. doi: 10.1176/appi.ajp.158.12.2008. [DOI] [PubMed] [Google Scholar]
- Silverman W, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Silverman W, Pina A, Viswesvaran C. Evidence-based psychosocial treatments for phobia and anxiety disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2008;37:105–130. doi: 10.1080/15374410701817907. doi: 10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- Silverman W, Saavedra L, Pina A. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:937–44. doi: 10.1097/00004583-200108000-00016. doi:10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Sood E, Kendall PC. Assessing anxious self-talk in youth: The Negative Affectivity Self-Statement Questionnaire--Anxiety Scale. Cognitive Therapy and Research. 2007;31:603–618. doi:10.1007/s10608-006-9043-8. [Google Scholar]
- Spence S. A measure of anxiety symptoms among children. Behaviour Research and Therapy. 1998;36:545–566. doi: 10.1016/s0005-7967(98)00034-5. doi:10.1016/S0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- Szabó M, Lovibond PF. The cognitive content of thought-listed worry episodes in clinic-referred anxious and nonreferred children. Journal Of Clinical Child And Adolescent Psychology. 2004;33:613–622. doi: 10.1207/s15374424jccp3303_18. doi:10.1207/s15374424jccp3303_18. [DOI] [PubMed] [Google Scholar]
- Tiwari S, Kendall PC, Hoff A, Harrison J, Fizur P. Characteristics of exposure sessions as predictors of treatment response in anxious youth. Journal of Clinical Child and Adolescent Psychology. 2013;42:34–43. doi: 10.1080/15374416.2012.738454. DOI: 10.1080/15374416.2012.738454. [DOI] [PubMed] [Google Scholar]
- Treadwell KRH, Kendall PC. Self-talk in youth with anxiety disorders: States of mind, content specificity, and treatment outcome. Journal of Consulting and Clinical Psychology. 1996;64:941–950. doi: 10.1037//0022-006x.64.5.941. [DOI] [PubMed] [Google Scholar]
- Villabø M, Gere M, Torgersen S, Arnberg K, Neumer S, Kendall PC. Anxious self-statements in clinic-referred U. S. and Norwegian anxiety-disordered youth. Cognitive Therapy And Research. 2013;37:840–850. doi:10.1007/s10608-013-9530-7. [Google Scholar]
- Walkup J, Albano A, Piacentini J, Birmaher B, Compton S, Sherrill J, Kendall PC. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. The New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup J, Labellarte M, Riddle M, Pine D, Greenhill L, Klein R, Roper M. Searching for moderators and mediators of pharmacological treatment effects in children and adolescents with anxiety disorders. Journal of the American Academy Of Child and Adolescent Psychiatry. 2003;42:13–21. doi: 10.1097/00004583-200301000-00006. doi:10.1097/00004583-200301000-00006. [DOI] [PubMed] [Google Scholar]
- Weersing VR, Weisz JR. Mechanisms of action in youth psychotherapy. Journal of Child Psychology and Psychiatry. 2002;43:3–29. doi: 10.1111/1469-7610.00002. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Donenberg GR, Han SS, Weiss B. Bridging the gap between laboratory and clinic in child and adolescent psychotherapy. Journal of Consulting And Clinical Psychology. 1995;63:688–701. doi: 10.1037//0022-006x.63.5.688. doi:10.1037/0022-006X.63.5.688. [DOI] [PubMed] [Google Scholar]
- Wood J, Piacentini J, Bergman L, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. Journal of Clinical Child and Adolescent Psychology. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- Wood J, Piacentini J, Southam-Gerow M, Chu BC, Sigman M. Family cognitive behavioral therapy for child anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:314–321. doi: 10.1097/01.chi.0000196425.88341.b0. doi: 10.1097/01.chi.0000196425.88341.b0. [DOI] [PubMed] [Google Scholar]