Abstract
Similarities and differences in parenting practices of children (Mage = 10; range 8-13 years) with traumatic brain injury (TBI) and socially-typical controls were examined. In addition, parenting practices were examined as moderators between injury group status (TBI or socially-typical) and social adjustment in the peer group. Mothers completed assessments of parenting practices; children's peers reported about children's social adjustment. The mothers of children with TBI reported significantly lower levels of nurturance and significantly higher levels of restrictiveness than mothers of socially-typical children. In addition, mothers’ nurturance moderated the relation between injury group and peer rejection, such that children with TBI were more rejected by classmates compared to their socially-typical peers at low levels of maternal nurturance. The findings are interpreted as supporting the important role parents play in the development of children with a history of TBI, as well as the implications for family-level interventions.
Keywords: traumatic brain injury, parenting, social adjustment, peer rejection
Parents are arguably the most significant influence on children's and adolescents’ socialization (see Grusec & Davidov, 2007; Steinberg & Silk, 2002). The extant literature suggests that parents who are warm, sensitive, and responsive in interactions with their children also form a trusting, supportive bond with them. This loving, trusting bond fosters children's beliefs that: (1) they are worthy of healthy, loving relationships with others and (2) potential social others (i.e., friends, peers) are trustworthy and the social world is safe to explore (Bowlby, 1969). Empirical work has documented that a positive, nurturing relationship with a primary caregiver is associated with successful functioning in the peer group in early (Brophy-Herb et al., 2011) and middle childhood (Booth-LaForce, Oh, Kim, Rubin, Rose-Krasnor, & Burgess, 2006), as well as during adolescence (Swanson, Valiente, Lemery-Chalfant, & O'Brien, 2011). However, children who have an insecure relationship with their parents are more likely to have difficulties both intra- and interpersonally (e.g., Booth-LaForce et al., 2012; Fearon, Bakermans-Kranenburg, Van IJzendoorn, Lapsley & Roisman, 2010). In addition, children whose parents are intrusive, unresponsive, and harsh develop a negative view of themselves (e.g., unworthy of love) and a perception that the social world is unsafe to explore (and social others are not trustworthy). Indeed, harsh, insensitive parenting is associated with a host of difficulties in the peer group from early childhood through adolescence, including peer victimization (Ladd & Kochenderfer Ladd, 1998); aggression (Park et al., 2005); unsupportive friendships (Cook, Buehler, & Fletcher, 2012); and anxious withdrawal (McShane & Hastings, 2009).
While much is known about general patterns in parenting, many factors affect parenting and moderate the relation between parenting and social competence, including child characteristics (e.g., Kochanska, Aksan, & Joy, 2007). This body of work includes investigations of parenting with respect to children's gender (e.g., Schuster, Mermelstein, & Wakschalg, 2013), temperament (e.g., van der Voort, Linting, Juffer, Bakersman-Kranenburg, & van Ijzendoorn, 2013), ordinal position (e.g., Bumpus, Crouter, & McHale, 2001), and health status (Hullmann et al., 2010), as well as moderating effects of parenting on the relation between child characteristics and later adjustment (e.g., Lewis-Morrarty, et al., 2012; Rubin, Burgess, Dwyer, & Hastings, 2003). One emerging area of study is focused on the relations between parenting and adjustment in children who have experienced a traumatic brain injury (TBI).
Approximately 30% of children will sustain a TBI by the age of 25 years (McKinlay et al., 2008), often resulting in long-term physical, cognitive, and socio-emotional difficulties (Taylor et al., 2002). The effects of TBI on children's development has been of considerable interest to researchers, with much focus on health and cognitive outcomes (see Yeates et al., 2007). Findings from this research indicate that children with TBI, and especially those with more severe injuries, are more likely to develop behavioral problems of both an externalizing (Chapman, Wade, Walz, Taylor, & Stancin, 2010) and internalizing (Karver et al., 2012) nature when compared to control children with a history of orthopedic injuries (Yeates et al., 2013; 2014). Moderators of injury outcomes, in addition to TBI severity, include the quality of their family relationships and the types of parenting they experience.
Most researchers who have examined the parenting styles of children with TBI have focused on preschool- and school-aged children. To control for the effects of hospitalization and behavioral predisposition to injury, many studies have compared the parents of these children to parents of children with orthopedic injuries (OI). Findings from these investigations indicate that mothers of children with TBI are less warm and responsive and more directive in their interactions with their children than mothers of children with OI. For instance, Wade and colleagues (2008) observed parent-child interactions during free play and a teaching task in a sample of families with preschool-aged children with TBI and OI in the weeks following injury. They found that the parents of children with moderate and complicated mild TBI displayed lower levels of warmth and responsiveness compared to parents of children with OI, and that the parents of children with severe TBI were more directive than the control parents. Other studies have failed to report differences in parenting, including subsequent research by Wade and colleagues (Kurowski et al., 2011). Studies of adolescents have also failed to demonstrate significant differences in parent-adolescent interactions or conflicts between parents of youth with TBI and parents of youth with OI (Wade et al., 2003).
While the effects of TBI on parent-child interactions across childhood are unclear, there is consistent evidence that parenting characteristics are associated with children's adjustment post-injury. Potter and colleagues (2011) reported that children with moderate TBI whose parents reported high levels of harsh, punitive parenting had significantly higher ratings of behavioral and cognitive dysregulation than children with OI whose parents reported the highest levels of authoritarian parenting. Other researchers have reported that permissive parenting is associated with poor functioning for children with TBI. In a study of young children (3-7 years), Yeates and colleagues (2010) found that parenting practices moderated the relation between injury status (severe-TBI, moderate TBI, and OI) and adjustment 18 months post-injury. Specifically, children with severe TBI who had highly permissive or highly restrictive parents had the highest levels of parent-reported behavioral difficulties. Wade et al. (2011) also reported that children with severe TBI whose parents were responsive and displayed low levels of negative interactions during free-play had fewer externalizing difficulties 6 months post injury than children with severe TBI whose parents were relatively unresponsive and highly negative.
In sum, it seems clear that children with TBI are at risk for the development of maladaptive outcomes, and that parents can influence their adjustment. While several studies have examined the moderating effects of parenting on behavioral outcomes following TBI, the majority of these investigations have utilized global ratings of socio-emotional well-being, such as ratings on the Child Behavior Checklist (CBCL). Few researchers have examined whether parental behavior is associated specifically with peer group functioning in children with TBI. Examination of peer-related functioning is critical as difficulties in peer interactions may serve as a precursor to the development of interpersonal and intrapersonal maladaptation (e.g., Ladd, 2006; Pedersen, Vitaro, Barker, & Borge, 2007; Sentse, Lindenberg, Omvlee, Ormel, & Veenstra, 2010). In support of the relevance of peer group interactions, peer-rated and teacher-rated maladaptive behaviors within the peer group are associated with problems of an internalizing and externalizing nature, and children's behavioral characteristics (e.g., aggression; social withdrawal) predict rejection, exclusion, and victimization by peers (Rubin, Bowker, McDonald, & Menzer, 2013). Recent work has indicated that children with TBI are more likely to be rejected by peers than OI children (Yeates et al., 2013).
Moreover, peer processes may be particularly important to study during the middle childhood period. Indeed, from a developmental perspective, middle childhood provides a critical window on social relationships, because of the growing importance of peer relationships and friendship at that age (Grusec, Chaparro, Johnston, & Sherman, 2013; Parker & Gottman, 1987). A recent study indicated that social relationships in middle childhood were associated with self-esteem and well-being (Guhn et al., 2013). In view of the importance of social adjustment with peers, we focused our investigation on the middle childhood period.
Although children with OI frequently serve as a comparison group in examining the effects of pediatric TBI, these children may be predisposed to behavioral characteristics that affect their social relationships, including relationships with their parents, and for this reason may be less appropriate in examining the effects of TBI on peer relationships. Brehaut et al. (2003) reported that children with behavioral difficulties were at an increased risk for orthopedic injuries and other studies indicate that children with OI are at higher risk for behavior problems than children from the general child population or those without physical injuries (Goldstrohm & Arffa, 2005; Uslu & Uslu, 2008). Thus, it would be fruitful to examine how parents of children with TBI compare in their parenting practices to parents of socially-typical controls, as well as how parenting moderates the relation between injury group (TBI or socially-typical) and peer social adjustment in the school context.
The primary aim of the current investigation was to compare the parenting practices of children with TBI and socially-typical controls. The second aim was to examine parenting style as a moderator between injury group and social adjustment within the peer group. Data were drawn from two larger studies: a study of the social outcomes of children with TBI (citation removed) and a study of friendship across the transition from elementary-to-middle school (citation removed). Importantly, we used peer-informants as raters of children's behaviors in order to assess children's behaviors in the school environment. Thus, we obtained assessments of children's functioning outside of the family unit, something that has rarely been done in this area of study. We hypothesized that: (1) the parents of socially-typical controls would report higher levels of nurturing and lower levels of restrictive parenting than parents of children with TBI; and (2) parenting practices would moderate the relation between injury group and behavior in the peer group. More specifically, we expected that relative to socially typical controls, TBI would be more strongly associated with poor peer outcomes in the context of restrictive parenting, and less strongly associated with poor peer outcomes in the context of more supportive, warm parenting.
Method
Participants
Data were drawn from two samples. The first was a sample of children with TBI who participated in a larger study on the social outcomes of TBI. The participants with TBI were recruited from children's hospitals at three metropolitan sites, including the Hospital for Sick Children in Toronto (Canada), Nationwide Children's Hospital in Columbus (US), and Rainbow Babies and Children's Hospital and MetroHealth Medical Center in Cleveland (US). Eligible participants included children hospitalized for a TBI who were 8 to 13 years of age at the time of their participation and injured between 12 and 63 months before participation. All children were injured after 3 years of age, and the vast majority after 4 years. The TBI group was restricted to children with complicated mild to severe TBI. The severity of TBI was determined by the Glasgow Coma Scale (GCS; Teasdale & Jennett,1974). The GCS is the most common method used to determine the level of consciousness after a TBI. The scale is typically administered at the time of injury and measures the following: eye opening, verbal response, and motor impairment scores range from 3-15. Consistent with established conventions (Sternbach, 2000), severe TBI was defined based on a lowest post-resuscitation GCS score of 8 or less, moderate TBI on GCS scores 9-12, and complicated mild TBI on a GCS score 13-15 in association with trauma-related abnormalities on neuroimaging at the time of hospitalization. A depressed skull fracture was sufficient to warrant inclusion in the complicated mild TBI group although only 3 children were eligible on this basis alone.
All children were subject to the following exclusion criteria: (a) history of more than one serious injury requiring medical treatment; (b) premorbid neurological disorder or mental retardation; (c) any injury determined to be a result of child abuse or assault; (d) a history of severe psychiatric disorder requiring hospitalization before the injury; (e) any sensory or motor impairment that prevented valid administration of study measures; (f) not fluent in English; and (g) any medical contraindication to MRI. Children in fulltime special education classrooms were excluded because the reliability and validity of classroom data for such classrooms; children with learning or attention problems were not excluded from the study.
Among children with TBI eligible to participate and approached about the study, 82 (47%) agreed to enroll. Those who agreed to participate did not differ from those who did not participate in age at injury, age at initial contact about the study, gender, race, or census tract measures of socioeconomic status (SES) that included mean family income, percentage of minority heads of household, and percentage of households below the poverty line. Participants and non-participants also did not differ on measures of injury severity (i.e., mean length of stay, median GCS score for children with TBI).
The current sample was restricted to the 67 children with TBI whose mothers completed ratings of parenting or for whom classroom data were obtained. Because the sample size for the severe group was small (n = 20), children in the complicated mild, moderate, and severe TBI groups were combined into a single TBI group. Importantly, the three severity groups were compared on all variables of interest and no significant differences emerged between the groups on mothers’ ratings of parenting or peer-rated social outcomes. The TBI group consisted of 43 males and 24 females with a mean age of 10.36 years (SD = 1.49). Sixty-two percent of the parents reported that they had completed at least some college and the majority of the sample (78%) self-identified as Caucasian. Measures were collected from the TBI group over several sessions (laboratory and classroom); therefore, forty -seven participants had peer-reported data.
The control group data were drawn from a separate study of fifth grade students from eight public elementary schools in the Washington D.C. metropolitan area. The aim of the study was to examine the longitudinal relations between parenting, peer relationships, and psychosocial outcomes across school transition periods. In the present report, a sub-sample of 93 children who were rated as socially-typical (i.e., did not demonstrate high behavioral problems in the school (below the 60th percentile on aggression and social withdrawal) on the Extended Class Play (ECP) served as a comparison group for children with TBI (ECP; Wojslawowicz Bowker, Rubin, Burgess, Booth-LaForce, & Rose-Krasnor, 2006). The socially typical control group consisted of 46 males and 47 females; the mean age of the control group was 10.35 years (SD = .52; range 9-12 years). Of the available demographic data for the socially-typical group, 85% reported that they had completed some college and 63% self-identified as Caucasian.
Measures
Child-Rearing Practices Report Questionnaire (CRPR-Q; Rickel & Biasatti, 1982)
The mothers of participating children were asked to complete the CRPR to assess their parenting behaviors. This Likert scale questionnaire assessed the primary caregiver's child-rearing practices, yielding the following two factors: nurturant parenting [14 items; e.g., “I respect my child's opinion and encourage him/her to express it”; α = .77 (TBI) and .70 (controls)] parenting, and restrictive parenting [12 items; e.g., “I control my child by warning him/her bad things might happen”; α = .79 (TBI) and .81 (controls)].
Extended Class Play (ECP; Wojslawowicz Bowker, Rubin, Burgess, Booth-LaForce, & Rose-Krasnor, 2006)
The participants completed an extended version of the Revised Class Play (RCP, Masten, Morison, & Pelligrini, 1985). The children were instructed to pretend to be the directors of an imaginary class play and to nominate their classmates for various roles. Children were instructed to nominate one boy and one girl within their classroom for each role and only nominations for participating children were considered. To eliminate possible gender-stereotyping, only same-gender nominations were utilized (Zeller, Vannatta, Schafer, & Noll, 2003). All item scores were standardized within gender and within classroom to adjust for the number of nominations received and the number of nominators.
Of interest in the current study were the subscales of aggression (7 items; e.g., “A person who gets into a lot of fights.”), rejection/victimization (8 items; e.g., “Someone who has mean things said to them”), popularity/sociability (6 items; e.g., “Someone who makes new friends easily”), prosociality (5 items; e.g., “Someone who helps other people when they need it”), and social withdrawal (4 items; e.g., “Someone who would rather play or hang out alone than with others”). Internal consistency alpha values for each construct were: aggression: α = .90 (TBI) and .89 (control), rejection/victimization: α = .93 (TBI) and .89 (control), popularity/sociability: α = .90 (TBI) and .92 (control), prosocial: α = .89 (TBI) and .90 (control), and social withdrawal: α = .87 (TBI) and .82 (control).
Analysis
Multivariate analysis of variance (MANOVA) was used to compare the groups on the parenting measures of nurturance and restrictiveness from the CRPR-Q. Examination of the predictors of peer-based social adjustment was conducted using multiple linear regression. Injury group was entered on the first step (TBI or socially-typical control, coded “0” and “1,” respectively), nurturance and restrictiveness were entered on the second step, and the two interaction terms to examine the interaction between group and parenting (nurturance, restrictiveness) were entered on the third step. Neither injury severity nor time since injury was significantly associated with CRPR-Q nurturance or restrictiveness nor with ECP aggression, social withdrawal, rejection victimization, popularity/sociability, or prosociality; thus, we did not control for these variables in the analyses.
Results
Group Differences in Parenting Measures of Nurturance and Restrictiveness
Tables 1 and 2 present the correlations, means, and standard deviations for all measures for the TBI group and socially typical group, respectively. The TBI group and socially typical group differed on maternal education, χ2 (9, N = 157) = 42.52, p = .001, and maternal race, χ2 (4, N = 155) = 22.77, p = .001; therefore, maternal education and maternal race were controlled for in the MANOVAs. The MANOVA revealed a significant group difference on the parenting measures, Pillai's Trace =.21 F(2, 147) = 19.951, p = .001. Follow-up ANOVAs indicated that the two groups differed significantly on restrictiveness, F(1, 151) = 7.60, p = .007, η2 = .05, with the mothers of children with TBI reporting more restrictiveness than mothers of socially typical children. In addition, the two groups differed on nurturance, F(1, 151) = 35.05, p = .001, η2 = .19, with the mothers of children with TBI reporting less nurturance than mothers of socially typical children.
Table 1.
Correlations, Means, and Standard Deviations for all Measures: TBI
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | M | SD | n | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. CRPR-Restrictive | -- | 3.49 | .63 | 67 | ||||||
| 2. CRPR-Nurturance | −.13 | -- | 5.33 | .44 | 67 | |||||
| 3. ECP-Aggression | .13 | −.08 | -- | .05 | .95 | 47 | ||||
| 4. ECP-Shy/Withdrawn | −.20 | −.01 | −.27t | -- | −.01 | .79 | 47 | |||
| 5. ECP-Rejection/Victimization | .19 | −.31* | .24 | .26t | -- | .21 | .94 | 47 | ||
| 6. ECP-Prosocial | −.03 | .16 | −.42** | −.05 | −.43** | -- | .03 | .86 | 47 | |
| 7 ECP-Popular/Sociable | −.22 | .10 | −.01 | −.33* | −.48** | .45** | -- | .07 | .89 | 47 |
Note.
p < .05, two-tailed
p < .01
*** p < .001
p < .10
Table 2.
Correlations, Means, and Standard Deviations for all Measures: Socially-Typical
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | M | SD | n | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. CRPR-Restrictive | -- | 3.23 | .72 | 93 | ||||||
| 2. CRPR-Nurturance | −.20t | -- | 5.63 | .26 | 93 | |||||
| 3. ECP-Aggression | −.28** | −.07 | -- | −.45 | .16 | 93 | ||||
| 4. ECP-Shy/Withdrawn | −.06 | .02 | −.11 | -- | −.45 | .17 | 93 | |||
| 5. ECP-Rejection/Victimization | .05 | −.009 | .20t | .18t | -- | −.39 | .27 | 93 | ||
| 6. ECP-Prosocial | .12 | .07 | −.11 | .06 | −.09 | -- | .12 | .61 | 93 | |
| 7 ECP-Popular/Sociable | .11 | −.009 | .16 | −.22* | −.23* | .43** | .17 | .79 | 93 |
Note.
p < .05, two-tailed
p < .01
p < .10
Peer-reported Adjustment
To examine the moderating effects of parenting on the relation between injury group and child outcomes as reported by peers, regression analyses were conducted (Table 3). The results for each of the measures of children's peer-based social adjustment are presented in Table 3 and summarized below.
Table 3.
Predictions of Peer-reported School Behavior
| Aggressive | Shy/Withdrawn | Rejection/Victimization | Prosocial | Popular/Sociable | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | δR2 | β | t | ΔR2 | β | t | ΔR2 | β | t | ΔR2 | β | t | ΔR2 | β | t | |
| Step 1 | ||||||||||||||||
| Injury Group1 | .20*** | −.45 | −5.86*** | .16*** | −.40 | −5.11*** | .19*** | −.43 | −5.60 | .003 | .05 | .62 | .002 | .05 | .56 | |
| Step 2 | ||||||||||||||||
| Nurturance | .004 | −.07 | −.81 | .001 | −.004 | −.05 | .04** | −.22 | −2.57 | .01 | .13 | 1.35 | .002 | .05 | .49 | |
| Restrictive | .001 | −.005 | −.07 | .01 | .10 | −1.26 | .009 | .09 | 1.20 | .004 | .06 | .76 | .001 | .005 | .06 | |
| Step 3 | ||||||||||||||||
| Injury × Nurturance | .001 | .05 | .44 | .001 | .02 | −.14 | .03* | .24 | 2.29 | .002 | −.05 | −.47 | .002 | −.07 | −.55 | |
| Injury × Restrictive | .02t | −.26 | −1.68t | .02t | .29 | 1.84t | .02t | −.26 | −1.66t | .004 | .13 | .72 | .03t | .33 | 1.91t | |
Note.
p < .05, two-tailed
p < .10; injury group
0 = TBI; 1 = socially-typical
Aggression
Injury group significantly predicted peer-reported aggression, adjR2= .20, Δ F(1, 137) = 34.33, p = .001; β = −.45. The presence of a negative beta weight indicates that children with TBI had peers who rated them as more aggressive in the classroom. No other main effects or interaction effects were found as predictors of peer-reported aggression.
Shy/withdrawn
Injury group significantly predicted peer-reported shyness/social withdrawal, adjR2= .15, Δ F(1, 137) = 26.15, p = .001; β = −.40, such that children with TBI had peers who rated them as more highly withdrawn in the classroom. No other main effects or interaction effects were found as predictors of peer-reported social withdrawal.
Rejection/victimization
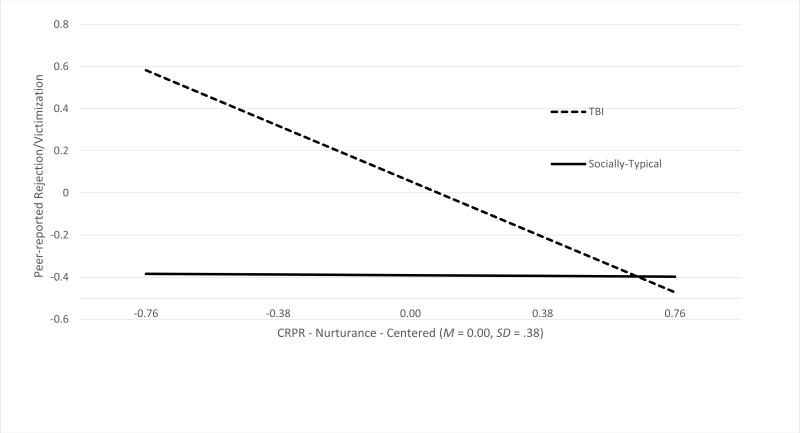
Injury group was also negatively predictive of rejection/victimization, adjR2= .18, Δ F(1, 137) = 31.30, p = .001; β = −.43, such that children with TBI had peers who rated them as more highly rejected in the classroom. Results also indicated that CRPR-Q nurturance was negatively predictive of peer-reported rejection/victimization, adjR2= .21, Δ F(1, 135) = 3.53, p = .03; β = −.20; the presence of a negative beta weight indicated that mothers who were lower in nurturance had children who were more highly rejected/victimized. This effect was subsumed under a significant interaction between injury group and nurturance, adjR2= .26 Δ F(1, 133) = 3.20, p = .04; β = .22. The interaction was modeled separately for the TBI and socially-typical groups (see Figure 1). For the TBI group, peer-reported rejection/victimization was significantly and negatively associated with CRPR-Q nurturance, β = −.31, p = .04, while the association was not significant for the socially-typical controls, β = −.009, ns (Figure 1).
Figure 1.
Interaction between group type and maternal nurturance in the prediction of peer-rated rejection/victimization
Discussion
The purpose of the current study was to examine parenting in a sample of children with TBI and socially-typical children. We found that mothers of socially-typical children reported significantly higher levels of warm, nurturing parenting and lower levels of restrictiveness than mothers of TBI children. Research on families of children with TBI has yielded inconsistent findings with regard to differences between children with TBI and those with other injuries on parenting practices and parent-child relationships (Kurowski et al., 2011; Wade et al., 2008). Our findings underscore the importance of incorporating a socially-typical group when examining the social relationships of children with TBI and suggest that, in comparison to parents of socially typical children, parents of children with TBI are less nurturant and more restrictive. One possible explanation for the lower level of nurturance and higher restrictiveness among parents of children with TBI is that these parents may view their children as more vulnerable, and may be less likely to consider reasoning with their child after misbehavior as a part of their parenting philosophy. Specifically, parents of children with TBI may focus more on keeping their children injury free and placing less value on nurturance. Consistent with this possibility, parents of children with TBI (Hawley, Ward, Magnay, & Long, 2003), as well as parents of children with critical or terminal illnesses, report increased levels of stress (Rodriquez, Dunn, Zuckerman, Vannatta, Gerhardt, & Compas, 2012), with increased stress in turn negatively associated with maternal warmth and responsiveness (Gelfand, Teti, & Fox, 1992).
The small sample size, combined with variability in how parents adapt to their children's TBI, may help account for the lack of association between TBI severity and parenting characteristics. These negative findings run contrary to previous studies that have reported differences in parenting practices when comparing TBI severity groups and orthopedic injury controls (Wade et al., 2008). A further consideration is that the measures used in this study were exclusively questionnaire-based assessments, whereas studies that have included direct observations of parent-child interactions have reported that TBI severity moderates the relation between parenting and behavioral difficulties in early childhood (Wade et al., 2011). Thus, it may be important for future researchers in this area to examine associations of parenting characteristics with TBI severity using alternative methods of data collection.
The findings indicating that peers rated children with TBI as more aggressive, socially withdrawn, and rejected compared to socially typical controls are consistent with previous research comparing the social outcomes of children with TBI and children with OI (Yeates et al., 2013; 2014). However, unlike previous work, the present findings represent peers’ ratings of children with TBI. Therefore, our findings broaden our understanding of the adjustment of children with TBI by providing evidence for their adjustment with the peers (rather than parents’ global ratings of adjustment).
When we examined parenting as a moderator of the relation between TBI and social outcomes, the results largely supported previous work on the role of parents in the development of children with TBI (Wade et al., 2011; Yeates et al., 2010). When children with TBI had mothers who were low in nurturance, they were rated by their peers as higher in rejection by their peers (see Figure 1). Importantly, when mothers of children with TBI reported high levels of nurturance, their children were rated as having the lowest levels of rejection by peers. This same pattern of results did not emerge when examining the moderating role of parenting on the relation between injury status and other forms of social adjustment in the peer group. It may be that mothers who are sensitive and responsive to their children's needs provide their children with the self-confidence that helps them to stand up for themselves in certain situations (e.g., when being bullied), which protects them from peer rejection. The same type of parenting may not be relevant for peers’ ratings of specific behaviors (e.g., aggression and social withdrawal) that may be influenced by more specific socialization practices, such as emotion socialization. It seems plausible that children with TBI's display of both aggression and withdrawal may be attenuated by the way that their parents respond to their emotions and teach them how to regulate their affect. This may be an important line for future work in this area.
Regardless, nurturant parenting appears to be an important protective factor in the social adjustment of children with TBI. Given that restrictive parenting did not moderate the relation between injury group and social adjustment, it may be that the most critical focus of interventions for families of children with TBI should be on cultivating supportive, warm, and responsive caregiving in order to foster social adjustment among children with TBI post-injury.
Notably, it is possible that the social difficulties of children with TBI are a result of the bidirectional nature of the relation between a child's injury and parenting. Children's social behaviors may be the result of the reciprocal relation between injury and parenting. Previous longitudinal work has indicated that such relations exist in the prediction of internalizing and externalizing difficulties (Taylor et al., 2001). Thus, future researchers should consider examining these variables longitudinally. This would allow for the examination of the dynamic nature of parent-child relationships in a study of children with TBI's adjustment in the peer group.
These findings extend the literature on the social outcomes of TBI by examining difficulties specific to the peer group. To our knowledge, this is one of few studies to examine parenting as a moderator of adjustment specific to the peer group in children with TBI. By examining peer-level variables (as opposed to parent ratings of adjustment), we are able to confirm that the behavioral difficulties reported by parents in previous studies are evidenced in other contexts (e.g., school). This is particularly important given the pivotal role that peers play during the middle childhood period (e.g., Collins & van Dulmen, 2006; Rubin, Bukowski, & Bowker, 2015). Indeed, some studies have linked difficulties with peers during middle childhood to socio-emotional difficulties and psychopathology concurrently (Guhn et al., 2013) and longitudinally (Hoglund, Lalonde, & Leadbeater, 2008).
These findings also have implications for interventions with children with TBI. Previous work has indicated that interventions focused on parents of children with TBI result in improvements both in parenting and child behavior (e.g., Antonini et al., 2014). Moreover, a recent review of parenting interventions for TBI indicated that interventions that target parents ameliorate child adjustment (behavioral, cognitive) after TBI (Brown, Whittingham, Boyd, & Sofronoff, 2013). The findings of this study provide evidence suggesting that teaching parents to be more affectionate, flexible, and supportive of their children may support children's social development.
It is also important to note that we compared children with TBI to socially-typical children, rather than children with OI. This seems important given that there is evidence to suggest that some children with OI are not socially typical (Uslu & Uslu, 2008). Thus, the findings of the present study, while they require replication, provide evidence that the parenting and peer experiences of children with TBI differs from those who are socially typical.
Limitations and Future Directions
While the present study had many notable strengths, there were also several limitations. The measures used herein were exclusively questionnaire-based assessments. Although the data were drawn from multiple informants, future researchers in this area will need to integrate other methods of data collection. For instance, the inclusion of observations of parent-child interactions would provide powerful information regarding the similarities and differences between TBI and socially-typical children. Previous work (Wade et al., 2008; 2011) using observations of mothers and their children has indicated that differences exist between mothers of TBI and OI children in their interactions with their children in the laboratory.
The current study requires replication given that only a single test of moderation was significant. In addition, the effect sizes ranged from small to medium, and there are certainly other processes that affect the relation between TBI and social adjustment other than maternal parenting practices. For instance, it may be important to examine how children's relationships with their fathers impact adjustment post-injury. Few studies have examined how, or if the relationship between TBI children and their fathers is associated with children's later adjustment. Given that the literature on typically-developing children has documented the unique role that fathers play in children's socio-emotional development (Brand & Klimes-Dougan, 2010), it seems critical to understand how fathers can help or hinder the development of TBI.
Parenting is also known to be affected by factors intrinsic to the parent, including parental stress and personality (Belsky, 1984). Examination of these parent characteristics would likely shed light on factors contributing to the group differences. Previous investigations on the family life of children with TBI has indicated that parents of children with TBI report higher levels of stress than those with OI (e.g., Hawley et al., 2003). This stress is almost certain to further impact (1) how parents interact with their children and (2) how TBI children fare in the peer group. This line of research may prove especially important for targeting interventions to those at the highest risk as it would provide a comprehensive picture of which families (presumably those children with TBI who have parents reporting the highest levels of stress) are in the greatest need for parent training. Of course, it would also be fruitful to examine how these children fare over time. An important “next step” in this line of research is to see how children with TBI fare beyond the middle childhood years.
In sum, the findings presented herein provide insight into the similarities and differences in the parenting experiences of children with TBI and socially-typical children. These findings bolster the work of others (e.g., Wade et al., 2008, 2011) and by revealing effects of TBI on parenting relative to a socially-typical comparison group. The findings also provide new evidence of moderating effects of maternal parenting practices on peer-related social outcomes of childhood TBI. By understanding how parents can help their children with TBI successfully navigate the peer world post-injury, it may be possible to develop targeted interventions that will shield children from the detrimental outcomes commonly associated with TBI. The findings reinforce the relevance of parenting characteristics to outcomes of pediatric TBI by indicating that children with TBI who have parents low in nurturance are at heightened risk for peer social problems.
Highlights.
Mothers of children with TBI report less nurturing and more restrictive parenting.
TBI significantly predicted social difficulties within the peer group.
Children with TBI were highly rejected when mothers were low in nurturance.
Acknowledgements
This research was supported by the National Institute of Child Health and Human Development (Grant # 5R01HD048946) and the National Institute of Mental Health (Grant # MH58116).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Antonini TN, Raj SP, Oberjohn KS, Cassedy A, Makoroff KL, Fouladi M, Wade SL. A pilot randomized trial of an online parenting skills program for pediatric traumatic brain injury: Improvements in parenting and child behavior. Behavior Therapy. 2014;45:455–48. doi: 10.1016/j.beth.2014.02.003. [DOI] [PubMed] [Google Scholar]
- Belsky J. The determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Booth La Force CB, Oh W, Kennedy AE, Rubin KH, Rose-Krasnor L, Laursen B. Parent and peer links to trajectories of anxious withdrawal from grades 5 – 8. Journal of Clinical Child and Adolescent Psychology. 2012;41:138–149. doi: 10.1080/15374416.2012.651995. doi:10.1080/15374416.2012.651995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth-LaForce CL, Oh W, Kim A, Rubin KH, Rose-Krasnor L, Burgess KB. Attachment, Self-Worth, and Peer-Group Functioning in Middle Childhood. Attachment and Human Development. 2006;8:309–325. doi: 10.1080/14616730601048209. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment. Basic Books; NY: 1969. [Google Scholar]
- Brand A, Klimes-Dougan B. Emotion socialization in adolescence: The roles of mothers and fathers. New Directions for Child and Adolescent Development. 2010;128:85–100. doi: 10.1002/cd.270. doi:10.1002/cd.270. [DOI] [PubMed] [Google Scholar]
- Brehaut JC, Miller A, Raina P, McGrail KM. Childhood behavior disorders and injuries among children and youth: A population-based study. Pediatrics. 2003;11:262–269. doi: 10.1542/peds.111.2.262. [DOI] [PubMed] [Google Scholar]
- Brophy-Herb HE, Schiffman RF, Dupuis SB, Fitzgerald HE, Horodynski M, Onaga E, Hillaker B. Toddlers' social-emotional competence in the contexts of maternal emotion socialization and contingent responsiveness in a low-income sample. Social Development. 2011;20:73–92. doi:10.1111/j.1467-9507.2009.00570.x. [Google Scholar]
- Brown FL, Whittingham K, Boyd R, Sofronoff K. A systematic review of parenting interventions fo traumatic brain injury: Child and parent outcomes. Journal of Head Trauma Rehabilitation. 2013;28:349–360. doi: 10.1097/HTR.0b013e318245fed5. [DOI] [PubMed] [Google Scholar]
- Bumpas MF, Crouter AC, McHale SM. Parental autonomy granting during adolescence: Exploring gender differences in context. Developmental Psychology. 2001;37:163–173. doi: 10.1037/0012-1649.37.2.163. doi:10.1037/0012-1649.37.2.163. [DOI] [PubMed] [Google Scholar]
- Chapman LA, Wade SL, Walz NC, Taylor HG, Stancin T, Yeates KO. Clinically significant behavior problems during the initial 18 months following early childhood traumatic brain injury. Rehabilitation Psychology. 2010;55:48–57. doi: 10.1037/a0018418. doi:10.1037/a0018418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins WA, van Dulmen M. The significance of middle childhood peer competence for work and relationships in early adulthood. In: Huston AC, Ripke MN, editors. Developmental contexts in middle childhood: Bridges to adolescence and adulthood. Cambridge University Press; New York, NY, US: 2013. pp. 23–40. [Google Scholar]
- Cook EC, Buehler C, Fletcher AC. A process model of parenting and adolescents' friendship competence. Social Development. 2012;21:461–481. doi: 10.1111/j.1467-9507.2011.00642.x. doi:10.1111/j.1467-9507.2011.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fearon RP, Bakermans-Kranenburg MJ, van IJzendoorn MH, Lapsley A, Roisman GI. The significance of insecure attachment and disorganization in the development of children's externalizing behavior: A meta-analytic study. Child Development. 2010;81:435–456. doi: 10.1111/j.1467-8624.2009.01405.x. doi:10.1111/j.1467-8624.2009.01405.x. [DOI] [PubMed] [Google Scholar]
- Gelfand DM, Teti DM, Fox C. Sources of parenting stress for depressed and nondepressed mothers of infants. Journal of Clinical Child Psychology. 1992;21:262–272. [Google Scholar]
- Goldstrohm SL, Arffa S. Preschool children with mild to moderate traumatic brain injury: An exploration of immediate and post-acute morbidity. Archives of Clinical Neuropsychology. 2005;20:675–695. doi: 10.1016/j.acn.2005.02.005. [DOI] [PubMed] [Google Scholar]
- Grusec JE, Chaparro MP, Johnston M, Sherman A. Social development and social relationships in middle childhood. In: Lerner RM, Easterbrooks MA, Mistry J, Weiner IB, editors. Handbook of psychology, Vol. 6: Developmental psychology. Wiley; Hoboken, NJ: 2013. pp. 243–264. [Google Scholar]
- Grusec JE, Davidov M. Socialization in the family: The role of parents. In: Grusec JE, Hastings PD, editors. Handbook of Socialization: Theory and Research. Guilford; New York: 2007. pp. 284–304. [Google Scholar]
- Guhn M, Schonert-Reichl KA, Gadermann AM, Hymel S, Herzman C. A population study of victimization, relationships, and well-being in middle childhood. Journal of Happiness Studies. 2013;14:1529–1541. doi:10.1007/s10902-012-9393-8. [Google Scholar]
- Hawley CA, Ward AB, Magnay AR, Long J. Parental stress and burden following traumatic brain injury amongst children and adolescents. Brain Injury. 2003;17:1–23. doi: 10.1080/0269905021000010096. [DOI] [PubMed] [Google Scholar]
- Hoglund WLG, Lalonde CE, Leadbeater BJ. Social cognitive competence, peer rejection and neglect, and behavioral and emotional problems in middle childhood. Social Development. 2008;17:528–553. doi:10.1111/j.1467-9507.2007.00449.x. [Google Scholar]
- Hullmann SE, Wolfe-Christensen C, Ryan J, Fedele DA, Rambo PL, Chaney JM, Mullins LL. Parental overprotection, perceived child vulnerability, and parenting stress: A cross-illness comparison. Journal of Clinical Psychology in Medical Settings. 2010;17:357–365. doi: 10.1007/s10880-010-9213-4. doi:10.1007/s10880-010-9213-4. [DOI] [PubMed] [Google Scholar]
- Karver CL, Wade SL, Cassedy A, Taylor HG, Stancin T, Yeates KO, Walz NC. Age at injury and long-term behavior problems after traumatic brain injury in young children. Rehabilitation Psychology. 2012;57:256–265. doi: 10.1037/a0029522. doi: 10.1037/a0029522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, Aksan N, Joy ME. Children's fearfulness as a moderator of parenting in early socialization: Two longitudinal studies. Developmental Psychology. 2007;43(1):222–237. doi: 10.1037/0012-1649.43.1.222. doi:10.1037/0012-1649.43.1.222. [DOI] [PubMed] [Google Scholar]
- Kurkowski BG, Taylor HG, Yeates KO, Walz NC, Stancin T, Wade SL. Caregiver ratings of long-term executive dysfunction and attention problems after early childhood traumatic brain injury: Family functioning is important. PM&R. 2011;3:836–845. doi: 10.1016/j.pmrj.2011.05.016. doi:10.1016/j.pmrj.2011.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladd GW. Peer rejection, aggression or withdrawn behavior, and psychological maladjustment from ages 5 to 12: An examination of four predictive models. Child Development. 2006;77:822–846. doi: 10.1111/j.1467-8624.2006.00905.x. doi:10.1111/j.1467-8624.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- Ladd GW, Kochenderfer-Ladd B. Parenting behavior and parent-child relationships: Correlates of peer victimization in kindergarten? Developmental Psychology. 1998;34:1450–1458. doi: 10.1037//0012-1649.34.6.1450. doi:10.1037/0012-1649.34.6.1450. [DOI] [PubMed] [Google Scholar]
- Lansford JE, Laird RD, Pettit GS, Bates JE, Dodge KA. Mothers' and fathers' autonomy-relevant parenting: Longitudinal links with adolescents' externalizing and internalizing behavior. Journal of Youth and Adolescence. 2014;43:1877–1889. doi: 10.1007/s10964-013-0079-2. doi:10.1007/s10964-013-0079-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Morrarty E, Degnan K, Chronis-Tuscano A, Rubin KH, Cheah CSL, Pine D, Fox NA. Maternal over-control moderates the association between early childhood behavioral inhibition and adolescent social anxiety symptoms. Journal of Abnormal Child Psychology. 2012;40:363–1373. doi: 10.1007/s10802-012-9663-2. doi:10.1007/s10802-012-9663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loder RT, Warschausky S, Schwartz EM, Hensigner RN, Greenfield ML. The psychosocial characteristics of children with fractures. Journal of Pediatric Orthopaedics. 1995;15:41–46. doi: 10.1097/01241398-199501000-00010. [DOI] [PubMed] [Google Scholar]
- Masten AS, Morison P, Pellegrini DS. A revised class play method of peer assessment. Developmental Psychology. 1985;21:523–533. doi:10.1037/0012-1649.21.3.523. [Google Scholar]
- McKinlay A, Grace LJ, Horwood LJ, Fergusson DM, Ridder EM, MacFarlane MR. Prevalence of traumatic brain injury among children, adolescents and young adults: Prospective evidence from a birth cohort. Brain Injury. 2008;22:175–181. doi: 10.1080/02699050801888824. doi:10.1080/02699050801888824. [DOI] [PubMed] [Google Scholar]
- McShane KE, Hastings PD. The new friends vignettes: Measuring parental psychological control that confers risk for anxious adjustment in preschoolers. International Journal of Behavioral Development. 2009;33:481–495. doi:10.1177/0165025409103874. [Google Scholar]
- Park J, Essex MJ, Zahn-Waxler C, Armstrong JM, Klein MH, Goldsmith HH. Relational and overt aggression in middle childhood: Early child and family risk factors. Early Education and Development. 2005;16:233–256. doi:10.1080/10409289.2005.10472869. [Google Scholar]
- Pedersen S, Vitaro F, Barker ED, Borge AIH. The timing of middle-childhood peer rejection and friendship: Linking early behavior to early-adolescent adjustment. Child Development. 2007;78:1037–1051. doi: 10.1111/j.1467-8624.2007.01051.x. doi:10.1111/j.1467-8624.2007.01051.x. [DOI] [PubMed] [Google Scholar]
- Potter JL, Wade SL, Walz NC, Cassedy A, Stevens MH, Yeates KO, Taylor HG. Parenting style is related to executive dysfunction after brain injury in children. Rehabilitation Psychology. 2011;56:351–358. doi: 10.1037/a0025445. doi:10.1037/a0025445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickel AU, Biasatti LL. Modification of the Block child rearing practices report. Journal of Clinical Psychology. 1982;38:129–134. [Google Scholar]
- Rodriguez EM, Dunn MJ, Zuckerman T, Vannatta K, Gerhardt CA, Compas BE. Cancer-related sources of stress for children and their parents. Journal of Pediatric Psychology. 2012;37:185–197. doi: 10.1093/jpepsy/jsr054. doi:10.1093/jpepsy/jsr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin KH, Bower JC, McDonald K, Menzer M. Peer relationships in childhood. In: Zelazo PD, editor. The Oxford Handbook of Developmental Psychology. Vol. 2. Oxford; United Kingdom: 2013. pp. 242–275. [Google Scholar]
- Rubin KH, Bukowski W. Children in peer groups. In: Bornstein M, Leventhal T, Lerner RM, editors. Handbook of Child Psychology and Developmental Science. Seventh Edition. Wiley; New York: 2015. pp. 175–222. formerly The Handbook of Child Psychology Volume Four: Ecological Settings and Processes. [Google Scholar]
- Rubin KH, Burgess KB, Dwyer KM, Hastings PD. Predicting preschoolers’ externalizing behaviors from toddler temperament, conflict, and maternal negativity. Developmental Psychology. 2003;39:164–176. doi:10.1037/0012-1649.39.1.164. [PubMed] [Google Scholar]
- Schuster RM, Mermelstein R, Wakschlag L. Gender-specific relationships between depressive symptoms, marijuana use, parental communication and risky sexual behavior in adolescence. Journal of Youth and Adolescence. 2013;42:1194–1209. doi: 10.1007/s10964-012-9809-0. doi:10.1007/s10964-012-9809-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sentse M, Lindenberg S, Omvlee A, Veenstra R. Rejection and acceptance across contexts: Parents and peers as risks and buffers for early adolescent psychopathology. The TRAILS study. Journal of Abnormal Child Psychology. 2010;38:119–130. doi: 10.1007/s10802-009-9351-z. doi:10.1007/s10802-009-9351-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Silk JS. Parenting adolescents. In: Bornstein M, editor. Handbook of Parenting: Vol. 1: Children and parenting. 2nd ed. Erlbaum; Mahwah, NJ: 2002. pp. 103–133. [Google Scholar]
- Sternbach GL. The Glasgow Coma Scale. Journal of Emergency Medicine. 2000;19:67–71. doi: 10.1016/s0736-4679(00)00182-7. [DOI] [PubMed] [Google Scholar]
- Swanson J, Valiente C, Lemery-Chalfant K, O'Brien TC. Predicting early adolescents' academic achievement, social competence, and physical health from parenting, ego resilience, and engagement coping. The Journal of Early Adolescence. 2011;31:548–576. doi:10.1177/0272431610366249. [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Burant C. Bidirectional child-family influences on outcomes of traumatic brain injury. Journal of the International Neuropsychological Society. 2001;7:755–767. doi: 10.1017/s1355617701766118. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. doi:10.1037/0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Uslu MM, Uslu R. Extremity fracture characteristics in children with impulsivity/hyperactive behavior. Archives of Orthopedic and Traumatic Surgery. 2008;128:417–421. doi: 10.1007/s00402-007-0393-9. doi:10.1007/s00402-007-0393-9. [DOI] [PubMed] [Google Scholar]
- Van der Voort A, Linting M, Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH. Delinquent and aggressive behaviors in early-adopted adolescents: Longitudinal predictions from child temperament and maternal sensitivity. Children and Youth Services Review. 2013;35:439–446. doi:10.1016/j.childyouth.2012.12.008. [Google Scholar]
- Wade SL, Cassedy A, Wade NC, Taylor HG, Stancin T, Yeates KO. The relationship of parental warmth responsiveness and negativity to emerging behavior problems following traumatic brain injury in young children. Developmental Psychology. 2011;47:119–133. doi: 10.1037/a0021028. doi:10.1037/a0021028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade SL, Taylor HG, Chertkoff NC, Salisbury S, Stancin T, Bernard LA, Oberjohn K, Yeates KO. Parent-child interactions during the initial weeks following brain injury in young children. Rehabilitation Psychology. 2008;53:180–190. doi: 10.1037/0090-5550.53.2.180. doi:10.1037/0090-5550.53.2180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade SL, Taylor HG, Drotar D, Stancin T, Yeates KO, Minich NM. Parent-adolescent interactions after traumatic brain injury: Their relationship to family adaptation and adolescent adjustment. Journal of Head Trauma Rehabilitation. 2003;18:164–176. doi: 10.1097/00001199-200303000-00007. [DOI] [PubMed] [Google Scholar]
- Wojslawowicz Bowker J, Rubin KH, Burgess KB, Booth-LaForce C, Rose-Krasnor L. Behavioral characteristics associated with stable and fluid best friendship patterns in middle childhood. Merrill-Palmer Quarterly. 2006;52:671–693. doi:10.1353/mpq.2006.0000. [Google Scholar]
- Yeates KO, Bigler ED, Dennis M, Gerhardt CA, Rubin KH, Stancin T, Vannatta K. Social outcomes in childhood brain disorder: A heuristic integration of social neuroscience and developmental psychology. Psychological Inquiry. 2007;133:535–556. doi: 10.1037/0033-2909.133.3.535. doi:10.1037/0033-2909.133.3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeates KO, Bigler ED, Abildskov T, Dennis M, Gerhardt CA, Vannatta K, Taylor HG. Social competence in pediatric traumatic brain injury: From brain to behavior. Clinical Psychological Science. 2014;2:97–207. doi:10.1177/2167702613499734. [Google Scholar]
- Yeates KO, Gerhardt CA, Bigler ED, Abildskov T, Dennis M, Rubin KH, Vannatta K. Peer relationships of children with traumatic brain injury. Journal of the International Neuropsychological Society. 2013;19:518–527. doi: 10.1017/S1355617712001531. doi:10.1017/S1355617712001531. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Walz NC, Stancin T, Wade SL. The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology. 2010;24:345–356. doi: 10.1037/a0018387. doi:10.1037-a001838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller MH, Vannatta K, Schaefer J, Noll RB. Behavioral reputation: A cross-age perspective. Developmental Psychology. 2003;39:129–139. doi: 10.1037//0012-1649.39.1.129. [DOI] [PubMed] [Google Scholar]