Dear Editor:
Melasma is a symmetrically acquired hypermelanosis of the malar, mandible, and forehead that more commonly affects women than men. The pathogenesis of melasma is multifactorial, including factors such as sun exposure, genetics, cosmetics, photosensitive drugs, and thyroid dysfunction. Whereas melasma in female patients has been found to have an etiological relation with female hormones, such as in cases of oral contraceptive use, hormone replacement therapy, and pregnancy, a few cases of melasma in male patients have been identified in the literature.
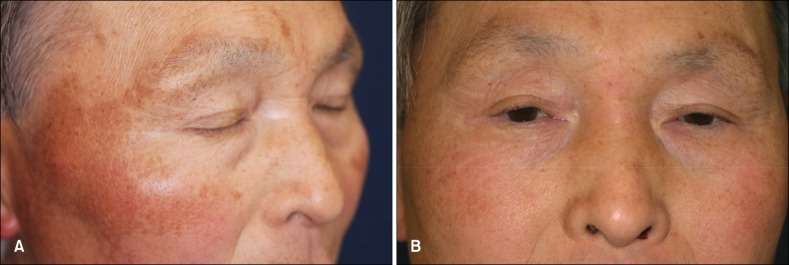
A 68-year-old Japanese man, who had episodic sun exposure for 2~3 h per day, visited our clinic for the evaluation of hyperpigmentation on his face. He had been given docetaxel hydrate (Taxotere; Sanofi Aventis, Paris, France) and ethinyl estradiol (Prosexol; Aska Pharmaceutical Co., Ltd., Tokyo, Japan) for prostate cancer 14 months and 3 months before the appearance of hyperpigmentation, respectively. He had no habit of scrubbing his face and no family history of melasma. A physical examination revealed symmetric, well-circumscribed light to dark-brown macule on the malar, nose, and upper part of his eyebrows (Fig. 1A). The diagnosis of melasma (malar type) was made clinically. During the administration of ethinyl estradiol, 1.5 g tranexamic acid (Transamin; Daiichi Sankyo Co., Ltd., Tokyo, Japan) had been administered. The macules on his face were mostly diminished by the 6-month administration of 1.5 g tranexamic acid (Fig. 1B). After 14 months, both tranexamic acid and ethinyl estradiol were discontinued, and melasma showed no recurrence. Hormonal investigation revealed low levels of testosterone, estradiol (E2), luteinizing hormone (LH), and follicle-stimulating hormone (FSH) (Table 1).
Fig. 1. (A) Symmetric, light to dark brown macules on the malar, nose, and upper part of the eyebrows with sharply demarcated margins. (B) The macules on his face mostly disappeared by 6 months after the administration of 1.5 g tranexamic acid.
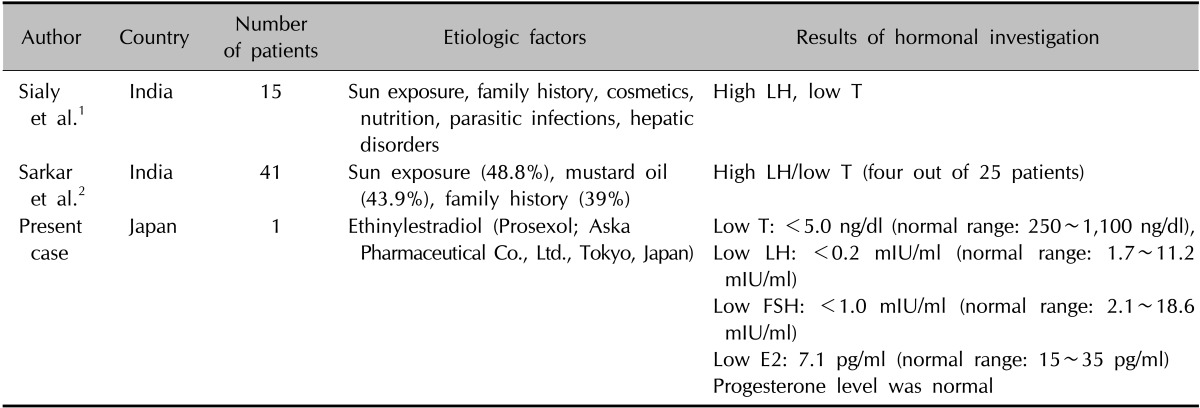
Table 1. The reports of male melasma in which hormonal evaluations were conducted.
LH: luteinizing hormone, T: testosterone, FSH: follicule stimulating hormone, E2: estradiol.
Sun exposure and genetics appear to be the most significant etiological factors of melasma in male patients (Table 1); however, hormonal imbalance between estrogen and testosterone might be one of the etiological factors. Ethinyl estradiol is known to lower blood testosterone and suppress the secretion of LH and FSH, which affects the suppression of E2. Also, increased levels of ethinyl estradiol would be expected with ethinyl estradiol treatment. The two studies noted low testosterone levels in Indian men with melasma (Table 1)1,2. Furthermore, Tadokoro et al. indicated that testosterone affects human melanocytes by reducing the level of intracellular cyclic adenosine monophosphate and tyrosinase activity3. Moreover, there were three reports of melasma in male patients due to hormone therapy4,5 6: one case due to fosfestrol tetrasodium4, one case due to an androgenic agent, Andro-6 (EAS Inc., Golden, Colorado, USA)5, and another case due to finasteride6. The authors reported that finasteride induces increased testosterone level, which is available for aromatization to estradiol, resulting in the subsequent induction of melasma because finasteride inhibits the conversion of testosterone to dihydrotestosterone6. Docetaxel is also known to cause nail pigmentation and persistent serpentine supravenous hyperpigmented eruption; however, only one possible case of melasma due to docetaxel was found in an online search and no reports have been indexed in PubMed. In conclusion, we hypothesize that a shift in the balance of these two hormones may increase the risk for the development of melasma in male patients. It is true that not all subjects who have hormonal imbalance develop melasma; however, hormonal imbalance between estrogen and androgen might be one of the etiological factors in some patients.
References
- 1.Sialy R, Hassan I, Kaur I, Dash RJ. Melasma in men: a hormonal profile. J Dermatol. 2000;27:64–65. doi: 10.1111/j.1346-8138.2000.tb02122.x. [DOI] [PubMed] [Google Scholar]
- 2.Sarkar R, Puri P, Jain RK, Singh A, Desai A. Melasma in men: a clinical, aetiological and histological study. J Eur Acad Dermatol Venereol. 2010;24:768–772. doi: 10.1111/j.1468-3083.2009.03524.x. [DOI] [PubMed] [Google Scholar]
- 3.Tadokoro T, Rouzaud F, Itami S, Hearing VJ, Yoshikawa K. The inhibitory effect of androgen and sex-hormone-binding globulin on the intracellular cAMP level and tyrosinase activity of normal human melanocytes. Pigment Cell Res. 2003;16:190–197. doi: 10.1034/j.1600-0749.2003.00019.x. [DOI] [PubMed] [Google Scholar]
- 4.O'Brien TJ, Dyall-Smith D, Hall AP. Melasma of the forearms. Australas J Dermatol. 1997;38:35–37. doi: 10.1111/j.1440-0960.1997.tb01097.x. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart CG. Chloasma in a man due to oral hormone replacement. Skinmed. 2006;5:46–47. doi: 10.1111/j.1540-9740.2006.04323.x. [DOI] [PubMed] [Google Scholar]
- 6.Famenini S, Gharavi NM, Beynet DP. Finasteride associated melasma in a Caucasian male. J Drugs Dermatol. 2014;13:484–486. [PubMed] [Google Scholar]