Abstract
Endometrial hyperplasia (EH) comprises a spectrum of changes in the endometrium ranging from a slightly disordered pattern that exaggerates the alterations seen in the late proliferative phase of the menstrual cycle to irregular, hyperchromatic lesions that are similar to endometrioid adenocarcinoma. Generally, EH is caused by continuous exposure of estrogen unopposed by progesterone, polycystic ovary syndrome, tamoxifen, or hormone replacement therapy. Since it can progress, or often occur coincidentally with endometrial carcinoma, EH is of clinical importance, and the reversion of hyperplasia to normal endometrium represents the key conservative treatment for prevention of the development of adenocarcinoma. Presently, cyclic progestin or hysterectomy constitutes the major treatment option for EH without or with atypia, respectively. However, clinical trials of hormonal therapies and definitive standard treatments remain to be established for the management of EH. Moreover, therapeutic options for EH patients who wish to preserve fertility are challenging and require nonsurgical management. Therefore, future studies should focus on evaluation of new treatment strategies and novel compounds that could simultaneously target pathways involved in the pathogenesis of estradiol-induced EH. Novel therapeutic agents precisely targeting the inhibition of estrogen receptor, growth factor receptors, and signal transduction pathways are likely to constitute an optimal approach for treatment of EH.
Keywords: Endometrial Hyperplasia; Progestins; Receptors, Estrogen; Therapy
INTRODUCTION
The endometrium, the innermost glandular layer of the uterus, is a dynamic tissue that goes through a series of alterations (proliferation, secretion and menstruation/shedding) during the menstrual cycle in a woman’s reproductive years [1]. This cyclic phase involves a complex interaction between the two female sex hormones, estradiol, and progesterone (Fig. 1). Estrogen promotes epithelial cell proliferation resulting in thickening of the uterus, while progesterone encourages epithelial cell differentiation and the secretory phase of the endometrial cycle [2,3]. The fine equilibrium between endometrial proliferation and apoptosis is maintained by an intricate process involving a number of factors including hormonal balance, molecular mechanisms, environment, age, and so forth; accordingly, it is prone to various disturbances leading to several endometrial abnormalities [4].
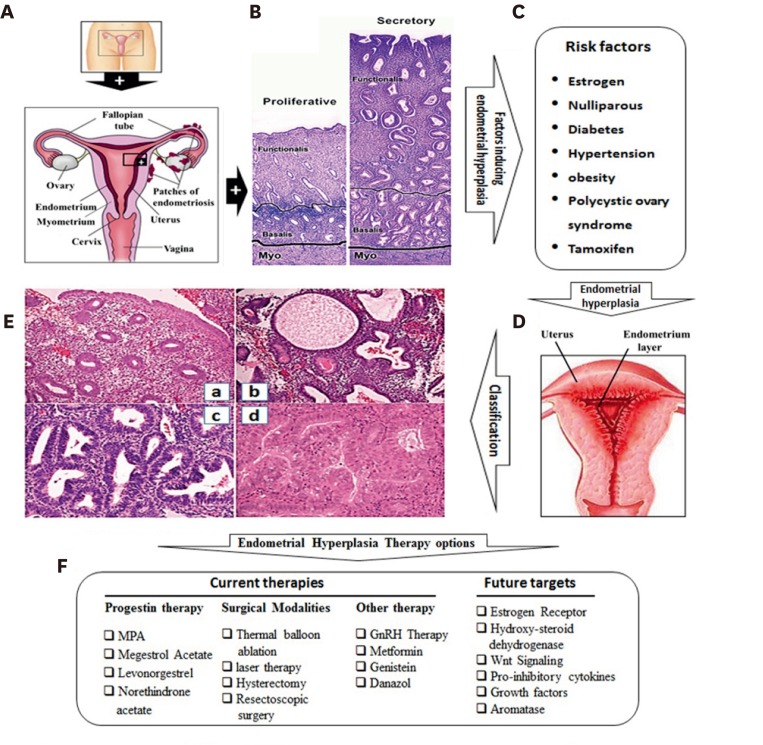
Fig. 1.
Overview of endometrial hyperplasia, risk factors, classification and treatment options. (A) The cross-sectional view of uterus showing endometrium. (B) H&E staining of endometrium at proliferative and secretory phase of endometrium. Adapted from Horne et al. [3], with permission from Oxford University Press. (C) Risk factors associated with endometrial hyperplasia. (D) The cross-sectional view of uterus showing proliferative endometrium and the H&E staining of endometrium hyperplasia showing abnormal increase of endometrial glands. (E) H&E stained section of endometrial: (a) proliferative endometrium; (b) simple hyperplasia; (c) complex hyperplasia; and (d) complex atypical hyperplasia. Adapted from Palmer et al. [15], with permission from John Wiley and Sons. (F) Different therapeutic options of endometrial hyperplasia. MPA, medroxy-progesterone acetate.
Endometrial hyperplasia (EH) is a pre-cancerous, non-physiological, non-invasive proliferation of the endometrium that results in increased volume of endometrial tissue with alterations of glandular architecture (shape and size) and endometrial gland to stroma ratio of greater than 1:1 [5,6]. Currently, the incidence of EH is indistinctly reported to be around 200,000 new EH cases per year in Western countries [7]. The majority of cases of EH arise in the presence of chronic exposure to estrogen unopposed by progesterone such as in earlier forms of hormone replacement therapy [6]. Overproduction of estrogen by fat cells also contributes to the higher risk of EH and endometrial cancer (EC) in obese women [8,9]. In addition to inducing proliferation of the uterus [10], estrogen induces morphometric alterations in the uterus that include changes in the type of luminal and glandular epithelia, the number and shape of glands, the gland to stroma ratio, and the morphology of epithelial cells [11,12].
EH also occurs after menopause, when ovulation stops and progesterone is no longer produced, as well as during perimenopause when women experience irregular ovulation. The most common symptom of EH is abnormal uterine bleeding including, menorrhagia, intermenstrual bleeding, postmenopausal bleeding, and irregular bleeding when on hormone replacement therapy or tamoxifen [13,14,15]. Currently, the treatment approaches for EH are limited, such as hysterectomy or hormone therapy [16]. EH without atypia is generally treated with progestins [17,18,19], while hysterectomy is the best treatment option for EH with atypia [20].
Since EH with atypia may progress to or coexist with EC [21], it is of clinical importance and should not be ignored. Moreover, conservative treatment with progestins is designed to regress hyperplasia to normal endometrium to prevent subsequent development of adenocarcinoma [22]. However, hormonal management of women with EH has largely been based on case studies, the efficacy of which has not been well assessed. The lack of standard and conservative treatment options emphasizes the need for new therapies. In this review, we discuss the etiology and risk factors for EH and the related advancement or existing therapies.
CLASSIFICATION OF ENDOMETRIAL HYPERPLASIA
Two different systems are commonly used to classify EH, the World Health Organization (WHO) schema [13] and the endometrial intraepithelial neoplasia (EIN) (Table 1) [13,15,23,24,25,26,27,28,29,30,31,32]. The WHO classification system, which is the most commonly recognized system, use cellular complexity, crowding of the endometrial gland and the presence of cytological atypia to categorize pathologies as simple or complex hyperplasia, with or without atypia (Table 1, Fig. 1) [15,33,34].
Table 1. Different classification systems of endometrial hyperplasia.
| Classifying year | Classifying type | Source | |||
|---|---|---|---|---|---|
| 1961 | Benign hyperplasia | Atypical hyperplasia type I | Atypical hyperplasia type II | Atypical hyperplasia type III | [25] |
| 1963 | Mild adenomatous hyperplasia | Moderate adenomatous hyperplasia | Marked adenomatous hyperplasia | [26] | |
| 1966 | Cystic hyperplasia | Adenomatous hyperplasia | Anaplasia | Carcinoma in situ | [27] |
| 1972 | Cystic hyperplasia | Adenomatous hyperplasia | Atypical hyperplasia | Carcinoma in situ | [28] |
| 1978 | Cystic hyperplasia | Adenomatous hyperplasia | Atypical hyperplasia | [29] | |
| 1979 | Hyperplasia without atypia | Hyperplasia with mild atypia | Hyperplasia with mild atypia | Hyperplasia with severe atypia | [30] |
| 1985 | Simple, nonatypical | Complex, nonatypical | Simple atypical | Complex atypical | [13] |
| WHO (1994) | Simple hyperplasia | Complex hyperplasia | Simple hyperplasia with atypia | Complex hyperplasia with atypia | [31] |
| WHO (2003) (revised) | Proliferative endometrium ● Tubular and regularly spaced gland ● Glands are lined with pseudostratified nuclei ● Abundant stroma ● Mitotic figures are easily found both in glands and stroma |
Simple hyperplasia ● Irregular shape and size glands ● Cystic appearance ● Abundant stroma, ● Nuclear pseudostratified glands but no nuclear atypia ● No back to back crowding |
Complex hyperplasia ● Closely packed glands ● Stroma is relatively sparse ● Gland to stroma ratio is more than 2:1 ● Nuclei are uniform, oval and pseudostratified ● Nucleoli are indistinct |
Complex atypical hyperplasia ● Tightly packed glands ● Very little intervening stroma ● Larger and vascular nuclei with chromatin clumped along the nuclear membrane ● Prominent nucleoli |
[15] |
| EIN | Benign or endometrial hyperplasia | EIN | Carcinoma | [23,24] | |
Adapted from Trimble et al. [32], with permission from Wolters Kluwer Health, Inc.
EIN, endometrial intraepithelial neoplasia.
The complexity of the WHO classification system has prompted improvement of an alternative system, the EIN. The EIN classifies EH as either benign or hyperplasia, and includes additional EIN and cancer classifications [35]. Cases are categorized as EIN based on architectural gland crowding, altered cytology and maximum linear dimension of the lesion exceeding 1 mm, while excluding cancer and mimics [35,36,37]. The EIN classification system can easily be applied to routine H&E stained sections and is more reproducible, helping clinicians to select treatment options [36,37]. This system efficiently classifies samples into high and low cancer risk categories. Various other old classifications are summarized in Table 1.
RISK OF PROGRESSION
EH represents a continuum of histologically distinct processes, starting from simple EH without atypia and then progress to complex EH with atypia, followed by well-differentiated endometrial carcinoma (Fig. 1) [38]. The presence and severity of cytological atypia and architectural crowding are key factors defining the risk for progression to carcinoma. Simple hyperplasia shows the lowest risk of cancer progression, and most cases (80%) of this naturally regress [13,39]. Among patients with atypical hyperplasia, postmenopausal status is associated with the highest risk of progression to adenocarcinoma [16]. Simple hyperplasia is associated with 3% and 8% rates of progression to complex hyperplasia and simple atypical hyperplasia, respectively. Complex hyperplasia has an intermediate risk of progression, which has been shown to regress in most of cases, while EH with cytological atypia is characterized as direct precancerous lesions and may carry a higher risk of progression to carcinoma [40]. Another study reported progression to EC in 1% of patients with simple hyperplasia, 3% of patients with complex hyperplasia, 8% of patients with simple atypical hyperplasia, and 29% of patients with complex atypical hyperplasia [13]. A recent study reported that 2% of the cases with complex hyperplasia (8/390) progressed to EC and 10.5% into atypical hyperplasia, while 52% of the atypical hyperplasia progressed into EC [41].
RISK FACTORS
Since EH is a precursor to cancer, all risk-factors of EC could be related to EH (Table 2). Postmenopausal, nulliparous, and infertile women are at greater risk of developing EH [42,43]. Diabetes, hypertension, and obesity are also associated with increased EH risk [13,44]. In addition to elevated estrogen levels, obesity causes chronic inflammation that can promote hyperplasia and cancer development [8]. When compared with non-obese ones, obese women (body mass index [BMI] >30 kg/m2) exhibited a nearly 4-fold increase in the incidence of atypical EH. Furthermore, women with a BMI of 40 kg/m2 showed a 13-fold increased risk of EH with atypia and a 23-fold increased risk of EH without atypia [45].
Table 2. Risk factors for endometrial hyperplasia.
| Risk factor | Factor inducing endometrial hyperplasia |
|---|---|
| Menstrual and parity status | Postmenopausal, null parity, late menopause or early menarche, chronic anovulation |
| Pre-existing disease | Obesity/overweight/high body mass index, diabetes mellitus, infertility, hypertension, polycystic ovarian syndrome, androgen-secreting tumors, hereditary non-polyposis colonic cancer (Lynch syndrome) |
| Hormone therapy | Prolonged exogenous estrogen exposure, tamoxifen, estrogen replacement therapy |
| Genetic factors | SNPs (CYP2D6, CYP17, COMT, APOE, and HFE), PTEN, K-ras, β-catenin, PIK3CA mutations, deletions on the short arm of chr-8, MSI |
| Inflammatory markers and cytokines | TNF-α, PCNA, EGF, Fas, TNF-R1, IGF-1, NF-κB, IL-22 |
APOE, apolipoprotein E; chr-8, chromosome 8; COMT, catechol-O-methyltransferase; CYP17, cytochrome P450 17A1; CYP2D6, cytochrome P450 2D6; EGF, epithelial growth factor; HFE, hemochromatosis; IGF-1, insulin-like growth factor 1; IL-22, interleukin 22; NF-κB, nuclear factor-κB; MSI, microsatellite instability; PCNA, proliferating cell nuclear antigen; PIK3CA, phosphatidylinositol 4,5-bisphosphate 3-kinase catalytic subunit alpha isoform; PTEN, phosphatase and tensin homolog; SNP, single nucleotide polymorphism; TNF-α, tumor necrosis factor-α; TNF-R1, tumor necrosis factor receptor 1.
Postmenopausal women taking estrogen supplements have long been known to be at increased risk of EH if a progestin is not used to oppose estrogen-activity [14]. The risk of developing EH also increases with increasing dose and length of estrogen treatment [46,47,48]. In a randomized placebo-controlled PEPI (postmenopausal-estrogen/progestin-interventions) trial, women receiving conjugated equine estrogen alone were more likely to develop simple EH (28% vs. 1%), complex EH (23% vs. 1%), and EH with atypia (11.8% vs. 0%), whereas combining the conjugated equine estrogen with cyclic or continuous progestins protected the endometrium from hyperplastic changes associated with estrogen-only therapy [49].
Several conditions associated with steroid hormone imbalances cause increased risk of EH and EC. Chronic anovulation, early menarche, late onset of menopause and other conditions associated with increased estrogen levels are also risk factors for EH. Polycystic ovary syndrome (PCOS) associated with anovulation leads to unopposed estrogenic activity on the endometrium [13]. Women with hereditary non-polyposis colonic cancer (Lynch syndrome) may have complex atypical EH at an earlier age [50] and altered estrogen levels which affects expression of DNA repair genes [51]. Androgen-secreting tumors of the adrenal cortex may induce the peripheral conversion of androgens to estrogens and is a rare cause of EH [14].
The endometrium is reported to have a balanced cytokine system with numerous correlations at the proliferative and secretary stages of the menstrual cycle. Though inflammation is the most important factor in most hyperplasia conditions, only a few studies have focused on the role of various pro- and anti-inflammatory cytokines in EH pathogenesis. Zhdanov et al. [52] reported in 2003 prominent imbalance in the cytokine system in atypical hyperplasia. EH was associated with reduced production of tumor necrosis factor-α (TNF-α), proliferating cell nuclear antigen, and epithelial growth factor mRNA and enhanced production of Fas mRNA. The expression of tumor necrosis factor receptor 1, interleukin-1β (IL-1β), and IL-12 genes was found to decrease only in glandular cystic hyperplasia while the expression of the insulin-like growth factor-1 (IGF-1) gene decreased only in adenomatous hyperplasia [53]. Production of IGF-1 is induced by estradiol and implicated in the estrogen effects on uterine growth [54]. The IGF-1 receptor (IGF-1R) was found to be expressed at higher levels in EH and EC in comparison to proliferative endometrium [55]. Furthermore, TNF-α was demonstrated to be expressed in normal endometrium and in simple and complex hyperplasia, but it was downregulated in atypical hyperplasia and endometrial carcinoma. The transcription factor nuclear factor-κB was also expressed in proliferating endometrium and in EH, but its expression was lower in carcinoma [56].
The most common genetic alterations in endometrial lesions (atypical EH or endometrioid endometrial carcinomas) are microsatellite instability (MSI) [57], PTEN mutations [58], K-ras mutation [59], beta-catenin mutation [60] and PIK3CA mutation [61]. PTEN, is involved in the pathogenesis of endometrial lesions and may precede the development of the MSI [57]. An immunohistochemical study revealed an important role of mismatch repair genes (hMLH1 and hMSH2) in the development of MSI in EC and atypical EH [62]. Patients with diagnosed hyperplasia were reported to have significant genome imbalance [63] and frequent deletions on the short arm of chromosome 8 [64]. Dysregulation of CTNNB1/β-catenin has been observed in atypical EH, complex EH with atypia, and in EIN [65]. Further mutant alleles of rs1800716 CYP2D6 polymorphisms were associated with increased chance of having double endometrial thickness of ≥5 mm in postmenopausal women on tamoxifen [66]. CYP17 polymorphism had correlation with endometrial atypia and cancer. Significant increase of A1/A1 and a decrease of A1/A2 genotype frequencies have been determined in patients with atypical EH [67]. A recent study showed a role of functional single nucleotide polymorphisms (SNPs) in the catechol-O-methyltransferase, apolipoprotein E, and hemochromatosis genes in EH and EC [68].
TAMOXIFEN AND ENDOMETRIAL HYPERPLASIA RISK
Among selective estrogen receptor (ER) modulators (SERMs), tamoxifen is the primary endocrine agent used to treat ERα-positive primary and advanced breast cancers [69,70,71]. Tamoxifen has been shown to improve the overall survival for both pre- and postmenopausal patients [72]. The first cases of endometrial carcinoma related to tamoxifen use were reported in 1985 [73]. Since then, many authors have confirmed the association of tamoxifen use with development of endometrial polyps, EH, and abnormal vaginal bleeding [74]. Multiple studies have evaluated the EH and EC risk in tamoxifen treated breast cancer patients [74,75]. In a randomized, double-blind trial, tamoxifen-treatment was shown to develop abnormal endometrial histology, proliferation, polyps, or mitotic cells in 39% of women, while 16% women showed atypical hyperplastic conditions [76]. Tamoxifen-treatment may result in endometrial thickness and polyps, leading to irregular endometrial linings that are associated with endometrial neoplasia [14,77].
The development of EC due to tamoxifen is a leading cause of concern. One of the molecular theories being investigated is that tamoxifen-induced genotoxicity (e.g., induction of micronucleus formation and cytochrome P450s) causes unscheduled DNA-synthesis and mitotic-spindle disruption [78,79]. The mechanism of tamoxifen action involves suppression of ER-dependent gene regulation in breast tissue and stimulation of ER-dependent gene regulation in the uterus [80,81]. In endometrial cells, the tamoxifen-ERα complex is able to recruit co-activator proteins and initiate gene transcription, and this differential recruitment of a co-activator contributes to the tissue specificity of the function of the tamoxifen-ERα complex, which may ultimately result in EC [81,82]. Tamoxifen was shown to up-regulate cancer markers in the endometrium, which are responsible for induction of EH and EC, such as ERα, progesterone receptor (PR), vascular endothelial growth factor, epidermal growth factor receptor (EGFR), mechanistic target of rapamycin (mTOR), human epidermal growth factor receptor 2 (HER-2/neu), IGF-1R, and c-Myc [83,84].
TREATMENT OPTIONS FOR ENDOMETRIAL HYPERPLASIA
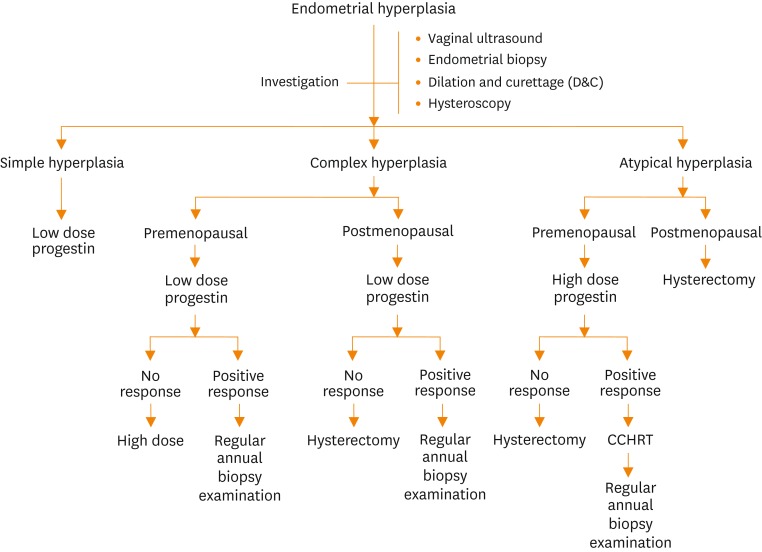
Although there is no bona fide treatment for EH, most current guidelines recommend hormone therapies (including use of progestin, gonadotropin-releasing hormone (GnRH) or its analogues or their combination) or surgical treatment (Fig. 1). The selection criteria for treatment options are based on patient age, health, the presence of cytologic-atypia and fertility status (Fig. 2). EH without atypia responds well to progestins. Hormone therapy is also recommended for women whose general health prevents them from tolerating surgery due to coexisting medical conditions. However, women with atypical EH or persistent EH without atypia that are symptomatic (abnormal uterine bleeding) are treated with hysterectomy. Among women hoping for childbirth, EH treatment is challenging, demanding conservative treatment regardless of whether the hyperplasia is with or without atypia.
Fig. 2.
The investigations and management schemes for endometrial hyperplasia. CCHRT, continuous-combined hormone replacement therapy.
PROGESTIN THERAPY
Progestins synthetic progestogens with similar effects as progesterone are most frequently employed to induce EH regression in women with EH without atypia or those who wish to retain fertility. Progestins can provide hormonal contraception either alone or with estrogen, and prevent EH development associated with unopposed estrogen. In addition, progestins have been found to decrease glandular cellularity by inducing apoptosis [85] and to inhibit angiogenesis in the myometrium immediately underlying the complex EH [86]. Progestins can be given to patients via oral, intramuscular, micronized vaginal cream, or intrauterine devices [16,87]. This treatment has been highly successful in reversing EH with or without atypia in patients on estrogen-alone replacement therapy [88], and was found to reduce EH in 61% of patients with atypical hyperplasia [5].
The mode and duration of progestin treatment is essential to its success. EH usually shows a response after 10-week of dosing, but significant responses are commonly observed after 3-months of progestin therapy [89,90], with the median time to resolution being 6 months [91]. Progestin therapy may be continued or hysterectomy performed in cases of no response. Different types of progestins and their doses in clinical use for the treatment of EH are shown in Tables 3, 4, respectively.
Table 3. Common therapies for endometrial hyperplasia.
| Therapy type | Origin and formula | Routes of administration |
|---|---|---|
| Progestin therapy | ||
| Medroxy progesterone acetate | Steroidal progestin (C24H34O4) | Oral; intramuscular |
| Megestrol acetate | Steroidal progestin (C24H32O4) | Oral |
| Levonorgestrel | Synthetic progestogen (C21H28O2) | Implant; insert (extended-release); oral |
| Norethisterone acetate | Steroidal progestin (C22H28O3) | Oral |
| Megestrol acetate+metformin | - | Oral |
| Levonorgestrel-IUD+metformin | - | Oral or implant; insert (extended-release) |
| Other than progestin therapy | ||
| Danazol | Synthetic steroid ethisterone (C22H27NO2) | Oral |
| Genistein | Isoflavones (C15H10O5) | Oral |
| Metformin | Biguanide class (C4H11N5) | Oral |
| GnRH therapy | ||
| Histrelin | D-His(B21)6, Pro9-Net-GnRH (C66H86N18O12) | Subcutaneous implant |
| Nafarelin | D-Nal(2)6-GnRH (C66H83N17O13)s | Nasal spray |
IUD, intrauterine device; His, histidine; GnRH, gonadotropin-releasing hormone; NH2, amino group; Pro, proline.
Table 4. Common doses of various progestins for treatment of endometrial hyperplasia.
| Progestin type | Common name | Common dose (endometrial type) | Source | |
|---|---|---|---|---|
| Benign or simple hyperplasia | Atypical hyperplasia or EIN | |||
| Progesterone | Progestasert, Crinone, Endometrin | 300 mg PO × 14 day/mo | 300 mg/day PO | [32,87] |
| Medroxy progesterone acetate | Depo-provera (injection), Provera (oral) | 10 mg PO × 14 day/mo | 100 mg PO or 1,000 mg/wk IM | |
| Megestrol acetate | Megace | 80 mg PO × 14 day/mo | 160 mg/day PO | |
| Levonorgestrol-IUD | Mirena, Orplant | 20 µg/day × 6 mo to 2 yr | ||
EIN, endometrial intraepithelial neoplasia; IM, intramuscularly; IUD, intrauterine device; PO, orally.
MEDROXYPROGESTERONE ACETATE
Medroxyprogesterone acetate (MPA) is a synthetic steroidal progestin (synthetic steroid hormone progesterone) that is usually used to treat cases with absent or irregular menstrual periods, or abnormal uterine bleeding. MPA prevents overgrowth in the uterine lining in postmenopausal women receiving estrogen hormone and decreases the risk of EH progression. Cyclic MPA has been shown to be a safer and more acceptable therapy than continuous MPA [92]. A multicenter trial by Ushijima et al. [93] showed 82% complete and 18% partial response rates in EH patients receiving an MPA regimen with a 25- to 73-month follow-up. Another study reported 54.8% remission by MPA [94]. MPA is commonly administered at 10 mg per day, orally and continuously for 6 weeks, or cyclically for 3 months (2 weeks of each month) [88]. In patients having only partial response, MPA may be continued for another 3 months orally at a dose of 10 mg, four times per day.
MEGESTROL ACETATE
Megestrol acetate (MA) is a steroidal progestin (specifically, 17-hydroxylated progesterone) with predominantly progestational and antigonadotropic effects that has been shown to have the potential to inhibit proliferation in the uterus and treat EH. MA at doses ranging from 160 to 320 mg/day has been reported to be an effective method of treatment for endometrial pathologies without causing marked harmful effects on serum lipid profiles or glucose levels [95]. Other studies also reported complete remissions of hyperplasia in more than 90% of patients [95,96]. A phase-II trial study of 31 patients with atypical EH and well- to moderately-differentiated endometrial carcinoma receiving MA at a dose of 80 mg (2 tablets) orally at breakfast and dinner for at least 12-week showed a positive response within 4 weeks, which was confirmed by endometrial biopsy or dilatation and curettage/hysteroscopy (https://clinicaltrials.gov/ct2/show/record/NCT00483327).
LEVONORGESTREL
Levonorgestrel (LNG) is a second generation progestin (synthetic progestogen) commonly used as an active component in some hormonal contraceptives. The LNG-impregnated intrauterine device (LNG-IUD) is currently a very common treatment option for EH. This device releases a constant amount of LNG inside the uterus and effectively opposes the estrogenic effect [97].
A multicenter randomized trial of 170 women with low- or medium-risk EH was recently conducted to investigate the safety and effectiveness of LNG-IUD, Mirena (Bayer, Leverkusen, Germany) [98]. Women treated with the LNG-IUD showed histologically normal endometrium after 6-months of therapy for EH. Moreover, cyclic progestogens were found to be less effective than continuous oral therapy and LNG-IUD [98]. Perimenopausal women (n=59) with non-atypical EH treated with LNG-IUD showed an 88.1% success rate (56/59) after 12-months of treatment [99]. A study in the United Kingdom showed histological regression in 90% of patients with EH (n=105) after 2-years of LNG-IUD treatment [100]. Another study reported 100% remission of EH by intrauterine-LNG [94].
NORETHINDRONE ACETATE OR NORETHISTERONE ACETATE
Norethisterone (or norethindrone) is a synthetic, orally active steroidal progestin with antiandrogen and antiestrogen effects [101]. It is commonly used as oral contraceptive pills and to treat premenstrual syndrome, irregular intense bleeding, irregular and painful periods, menopausal syndrome in combination with estrogen, or to postpone a period [102].
Various studies have validated use of norethisterone as an agent to reduce the incidence of EH in postmenopausal women treated with estradiol [74,103]. A phase-III double-blind, randomized, multi-center study of norethisterone in 662 postmenopausal women was conducted from 2007 to 2009. The results showed 56% improvement in menopausal symptoms (ClinicalTrials.gov Identifier: NCT00522873 [104]). Several other clinical trials have investigated application of norethindrone with a combination of LNG-IUD (ClinicalTrials.gov Identifier: NCT01499602) or with genistein (ClinicalTrials.gov Identifier: NCT00453960). However, no final results have been posted to date.
Although various studies and randomized trials have shown that progestin is a potent therapeutic option for EH, there are some common side effects including dizziness, headache, nausea, abdominal pain, uterine pain, delay of menstruation, heavy menstruation, uterine bleeding, fatigue, diarrhea, vomiting, and painful menstruation. However, these symptoms commonly disappeared within 48 hours. Further, although the progestins have been widely used as nonsurgical management of EH, about 12% to 53% resistance rates were reported after progestin therapy [105]. Failure of progestin treatment may depend on various details such as a patient’s age, health, other diseases, and hyperplasia grade or type. Resistance may be due to inadequate/low level of progestin receptors, particularly PR-B, before treatment or alterations in PR regulatory function, co-activators and co-repressors [106]. Other molecular mechanisms for progestin resistance are dysregulation of TGF-α and EGFR in endometrial glandular cells, Fas/FasL and survivin expression, as well as insulin resistance [107,108]. Hence, precautions such as routine checkups and biopsies are recommended for patients while on progestin therapy.
THERAPIES OTHER THAN PROGESTINS
1. Danazol
Danazol, a synthetic androgen, is a derivative of 17α-ethinyltestosterone that is usually used as a treatment option for endometriosis [109]. Danazol can induce a hypoestrogenic, as well as, a hypoandrogenic state in the uterus, resulting in atrophy of the endometrium [110,111]. Various studies have shown the significant effects of danazol against EH [112,113,114,115,116]. Moreover, it has been suggested as an effective and safe alternative to progesterone for treatment of EH [114]. Danazol containing IUDs (D-IUDs) might also be a novel and effective method for the treatment of EH [117]. However, some studies have suggested that danazol can increase the risk of ovarian cancer among women with endometriosis [118]. Other side effects of danazol include weight gain, muscle cramps, acne, seborrhea, decreased breast size, hirsutism, and deepening of the voice, which are all strongly related to androgenic action [119].
2. Genistein
Genistein is an isoflavonoid extracted from soy products that is a well-known inhibitor of protein-tyrosine kinases and topoisomerase-II [120,121]. Genistein has been shown to suppress estrogen-induced genes such as c-fos and c-jun, as well as the internal cytokines IL-1α and TNF-α through cytokine- and ER-mediated pathways [122]. Treatment with genistein aglycone (54 mg/day, n=19) for 6 months caused a 42% positive response rate in premenopausal women with non-atypical EH [123]. A randomized double-blind, placebo and progesterone-controlled clinical trial also showed that after 6 months, 42% of genistein aglycone treated subjects showed significant improvement of symptoms, significantly reduced staining for ER-α and PR, and enhanced ER-β1 staining with complete regression of bleeding [124]. In a phase-II clinical trial (January 2007 to December 2008), genistein (54 mg/day daily for 6 months) was administered as a dietary supplement with norethisterone acetate and patients were found to recover from EH (ClinicalTrials.gov Identifier: NCT00453960). These results prompted use of genistein aglycone for EH management, particularly in patients without atypia. However, more studies and clinical trials are needed to establish genistein as a potent drug for the treatment of EH.
3. Metformin
Metformin (N,N-dimethylbiguanide) belonging to a class biguanides is commonly used for the treatment of type 2 diabetes mellitus [125] and PCOS, especially in over-weight and obese individuals [126], or in cases when insulin resistance may be an important factor [127]. Since insulin resistance is associated with the occurrence of atypical EH [128] and metformin was shown to have anti-proliferative, anti-invasive, and anti-metastatic effects in multiple cancers, use of metformin is a logical approach for the treatment of EH [127,128,129,130,131,132]. Interestingly, metformin was shown to induce PR expression in EC cells [133], which may enhance progestin therapy efficiency or overcome the progestin resistance caused by PR depletion in long term progestin therapy.
Erdemoglu et al. [134] demonstrated the anti-proliferative effects of metformin on the endometrium in estradiol- or tamoxifen- treated mice. Several studies have established metformin as an effective anti-estrogenic agent in the control of abnormal endometrial proliferative disorders or atypical EH [127,128,135]. Tas et al. [136] verified that, similar to progesterone, metformin attenuates estrogen-induced EH in oopherectomized rats. Metformin is now being studied in multiple cancer clinical trials (ClinicalTrials.gov identifier: NCT01685762), as well as in combination with LNG-IUD (clinical trial.gov identifier: NCT02035787; NCT01686126) and MA (ClinicalTrials.gov Identifier: NCT01968317) [137].
GONADOTROPIN-RELEASING HORMONE THERAPY
The endometrium contains GnRH receptors and GnRH agonists can down-regulate GnRH receptors upon prolonged exposure. GnRH analogues suppress the hypothalamic pituitary-ovarian axis, thereby inhibiting estrogen production. Thus, GnRH analogues appear to have a direct anti-proliferative effect on endometrial cells [138]. This has led to exciting and promising new avenues for EH therapy [139]. GnRH has been applied at a dose of 1 ampule/3.75 mg intramuscularly every 28 days for 6 months to treat women with EH, with or without atypia. However, 25% of patients showed hyperplasia recurrence within 16-months of the completion of therapy [139]. A study, in which GnRH and tibolone (a synthetic steroid with both estrogenic and progestagenic effects) were used to treat EH, achieved complete remission in all patients, but with 19% recurrence within 2 years after cessation of therapy [140]. Accordingly, further study is needed to determine the usefulness of GnRH analogues before it can be recommended for clinical use in patients with atypical hyperplasia [141]. Different types of GnRH and its analogues evaluated for treatment of EH are shown in Table 3. Various clinical trials for treatment of EH are summarized in Table 5.
Table 5. Clinical trials for endometrial hyperplasia.
| ClinicalTrials.gov Identifier (study type) | Hyperplasia grade | Drug | No. of patients (age range, yr) | Phase trial | Study duration | Outcome |
|---|---|---|---|---|---|---|
| NCT01499602 (interventional) | Simple or complex EH without atypia | Levonorgestrel and norethisterone acetate | 120 (40-50) | May 2009-Nov 2011 | Achieve complete regression | |
| NCT00453960 (interventional) | Non atypical EH | Genistein and norethisterone acetate | 59 | II | Jan 2007-Nov 2008 | Recovery from endometrial hyperplasia |
| NCT01234818 (interventional) | EH | LNG-IUD | 80 | II | Nov 2010-Nov 2012 | Endometrial aspiration biopsy shows exacerbation, treatment with LNG-IUD must be stopped and other specific treatment should be initiated. |
| NCT01685762 (interventional) | Asymptomatic EH | Metformin | ~15 (18-75) | 0 | Jul 2012-Apr 2014 | No study results posted on clinicaltrials.gov yet |
| NCT01074892 (interventional) | EH | MPA and levonorgestrel | 170 (30-70) | IV | May 2005-May 2012 | Regression of hyperplasia after 6 months of therapy but recurrence and side effects during 2 year fallow-up treatment |
| NCT00483327 (interventional) | Atypical EH | Megestrol acetate | 31 (>18) | II | Jun 2007-Nov 2013 | Best pathologic response rates |
| NCT01686126 (interventional) | Complex atypia EH | Levonorgestrel and metformin | 165 (>18) | II | Sep 2012-Dec 2014 | Pathological complete response |
| NCT00490087 (interventional) | Atypical endometrial polyps and atypical EH | LNG-IUD | 21 (25-50) | III | Jun 2007-Sep 2011 | Recurrence of polyp in the two groups |
| NCT00883662 (observational) | EH | Levonorgestrel | 2,680 (>18) | - | Jun 2009-Apr 2015 | Patient distribution per indication |
| NCT00919919 (interventional) | EH and EC | progesterone | 60 (45-60) | II | Jun 2009-Nov 2010 | Comparing the proportion of women with endometrial thickness not exceeding 8mm and change not exceeding 3 mm between the two groups. |
| NCT01968317 (interventional) | Atypical EH | Megestrol acetate and metformin | ~150 (18-45) | II | Oct 2013-Apr 2015 | Got pathological response rate |
| NCT00788671 (interventional) | Complex atypical EH | LNG-IUD | ~50 (>18) | II | Nov 2008-Mar 2015 | Complete regression of disease |
| NCT02035787 (interventional) | Complex atypical EH and EC in non-surgical patients | Metformin with LNG-IUD | ~30 (>18) | - | Jan 2014-Jul 2 014 | Percent of individuals achieving complete disease regression as defined by no evidence of microscopic viable hyperplasia or carcinoma on endometrial biopsy after 6 months of treatment compared to a base rate of 50% |
EC, endometrial cancer; EH, endometrial hyperplasia; LNG-IUD, levonorgestrel-impregnated intrauterine device; LNG-IUD, levonorgestrel-impregnated intrauterine system; MPA, medroxy-progesterone acetate.
SURGICAL MODALITIES
Since EH can progress to endometrial carcinoma, surgery is favored in most women with complex EH with atypia if they have completed childbearing, do not desire preservation of their fertility or did not respond to hormone therapy [142]. Several surgical options have been widely reported as common treatments of atypical EH, such as thermal balloon ablation, laser therapy or resectoscopic surgery. Thermal balloon endometrial ablation or resectoscopic endometrial ablation therapy is a feasible, safe, and effective treatment option for simple and complex non-atypical EH [143]; however, hysterectomy might be considered a first-choice treatment for EH [144,145]. Resectoscopic surgery is an effective treatment for EH without atypia, especially for those at high risk for medical therapy or hysterectomy [146]. It is also recommended that postmenopausal women with atypical EH undergo hysterectomy with concomitant bilateral salpingo-oophorectomy rather than hysterectomy alone [147].
Women who undergo hysterectomies are at higher risk of developing stress incontinence. Although surgical modulations are well developed, studies with larger numbers of participants are still required to define their safety and efficiency before they can be recommended for all EH patients.
LIMITATIONS OF EXISTING THERAPIES, NEED FOR FURTHER RESEARCH, AND FUTURE PROSPECTS FOR DRUG DEVELOPMENT
Currently, the recommended treatment approach for EH includes; cyclic progestin therapy, GnRH therapy, and hysterectomy. The main limitations of the surgical methods (hysterectomy, hysteroscopic endometrial resection/ablation) are that they lead to the removal or disruption of the endometrium and can cause infertility and significant side effects. Progestins continue to be an effective option, especially for patients with low-grade ER and/or PR positive disease, some of whom achieve prolonged remission [148,149]. Regrettably, progestin treatment contributes to reduction of PRs thereby causing response failure in adjuvant settings [148,150,151]. The disadvantages of GnRH therapy includes high cost, menopausal symptoms and bone demineralization associated with prolonged therapy [152]. Moreover, pre-operative use of GnRH has been accounted as a risk factor for recurrence of fibroids. Hence, further research to identify new compounds and treatment strategies for this disease are warranted.
EH is a complex disease that may require simultaneously attacking more than one target or a systems approach for effective treatment. With the increased understanding of the molecular basis and the pathways related to particular disease progression, the era of molecularly targeted therapies has emerged as a most promising direction of research. For the development of personalized therapy agents in EH, pathways relevant to EH and EC may be targeted necessitating the careful research on molecular modulations in EH and endometrial tumors. Since EH is basically a hormone-dependent problem having high ER and/or PR expression, targeting ER may be a viable approach toward the development of novel treatment strategies for such disease.
Towards such an approach, pure antiestrogens represent endocrine-targeted therapy whose mechanism of action involves competition with the ER ligands and ER down regulation. Fulvestrant (ICI 182,780) is used to treat hormone receptor-positive metastatic breast cancer in postmenopausal women by enhancing ER degradation [153]. Acolbifene (EM-652) and EM-800, are nonsteroidal anti-estrogens that have been found to reduce uterine weight and uterine/vaginal ER expression [154]. In vivo, acolbifene was devoid of any agonist activity in an immature rat uterotrophic assay and in mouse endometrial tissues [155,156]. Additionally, acolbifene was more effective than Fulvestrant in inhibiting estradiol-induced EC and cell proliferation [157,158,159]. Taken together, these findings suggest that these antiestrogens may be beneficial to treat EH by reducing ER expression and acting as anti-proliferative agents.
The 2-[piperidinoethoxyphenyl]-3-[4-hydroxyphenyl]-2H-benzo(b) pyran, identified as an anti-estrogenic agent, is a nonsteroidal, triaryethylene and triarylpropenone compound which was found to inhibit uterine growth [148,160,161,162]. The ability of this compound to inhibit uterine growth is attributed to its ability to antagonize estrogen action and apoptosis-inducing activities [162]. The activity of this compound has also been validated in primary cell culture of human atypical EH cells suggesting its potential use as a new targeted therapy for EH via inhibition of Wnt signaling, as well as inhibition of cell survival pathway [163].
Apart from the ovaries, fat tissues are the most common site for conversion of androgen to estrogen [164]. This locally produced estrogen results from over-expression of P450 aromatase in endometriotic tissue and increases the risk of endometrial hyperproliferation, EH, and EC [165]. Aromatase inhibitors can inhibit estrogen production and thus reduce estrogen levels [166]. Examples of aromatase inhibitors include letrozole (Femara, Novartis, Basel, Switzerland), anastrozole (Arimidex, AstraZeneca, London, UK), and exemestane (Aromasin, Pfizer, New York, NY, USA), which are commonly used to treat breast cancer, and also thought to be helpful in the treatment of EC [167,168]. Anastrozole or letrozole were shown to reduce endometrial thickness in patients with EH [169]. Recent studies have established letrozole as good therapeutic option for simple EH without atypia [170,171]. Anastrozole was also found to be an interesting new modality for the treatment of EH in obese postmenopausal women [172]. Side effects of aromatase inhibitor treatment may include joint and muscle pain as well as hot flashes, bones weakening and occasionally osteoporosis.
Further, although tamoxifen is a well known inducer of endometrial proliferation, it is a major therapeutic option for breast cancer. Thus we cannot ignore its importance as a potent therapeutic agent. Till now, various studies have been carried out to overcome the side effects of tamoxifen on the uterus [173,174,175]. Since tissue specific actions of SERMs are based on various molecular components in specific cellular environments including the ERα to ERβ ratio and of co-activators and co-repressors [176], an approach to modulate tissue specific tamoxifen action in the uterus could also be a fascinating area of research involving development of new drugs that prevent the uterine estrogenic activity in a combination therapy with tamoxifen in breast cancer treatment. Combination with progestin or cyclic therapy of tamoxifen for breast cancer treatment needs more attention to prevent tamoxifen induced hyperplasia of endometrium.
Therapies targeted at immune cytokines that are elevated in EH and EC are also a promising avenue of investigation. A neutralizing antibody to human IL-22, was shown to inhibit proliferation of EC cells [177]. Multiple neutralizing antibodies and small chemical inhibitors of IGF-R1 are being studied in EC and could have applicability to treat EH if their toxicity profiles prove acceptability for a cancer prevention application [54]. Similarly, a chemokine (C-C motif) ligand 2 neutralizing antibody and a CCR2 antagonist, which have been shown to inhibit endometrial stromal cell proliferation could potentially be studied for treatment of EH given appropriate safety profiles [178]. There is a wide variety of pharmaceuticals in clinical use and trial for treatment of a variety of diseases including cancer, which also might have applicability for targeting the imbalance of cytokines involved in the development of EH and progression to cancer.
CONCLUSIONS
EH, being a precursor of EC, is of clinical importance. Available therapeutic options for EH, such as progestin, danazol, genistein, metformin and GnRH therapy or surgery have restricted efficacy due to high cost, side effects and drug resistance. Further, EH treatment is still challenging in patients who wish to retain their fertility. As a novel approach, the antiestrogens, aromatase inhibitors and cytokines might give optimistic outcome for EH; however, clinical trials are needed to prove their efficacy. Various mutations and SNP in pathobiology of EH should be also targeted to achieve better therapeutic response. Future investigations and clinical trials with these novel compounds in combination with known established EH therapies are required to achieve precise management of EH. Further research on the cellular signaling pathways that control endometrial cell proliferation and development of EH, as well as targeting various mutations and SNP in pathobiology of EH will help to identify novel targeted therapeutic agents to improve the management of EH.
ACKNOWLEDGMENTS
A. D. wants to thank ICMR, India for their support. CDRI communication number-9037.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Jabbour HN, Kelly RW, Fraser HM, Critchley HO. Endocrine regulation of menstruation. Endocr Rev. 2006;27:17–46. doi: 10.1210/er.2004-0021. [DOI] [PubMed] [Google Scholar]
- 2.Medh RD, Thompson EB. Hormonal regulation of physiological cell turnover and apoptosis. Cell Tissue Res. 2000;301:101–124. doi: 10.1007/s004419900159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horne FM, Blithe DL. Progesterone receptor modulators and the endometrium: changes and consequences. Hum Reprod Update. 2007;13:567–580. doi: 10.1093/humupd/dmm023. [DOI] [PubMed] [Google Scholar]
- 4.Kaaks R, Lukanova A, Kurzer MS. Obesity, endogenous hormones, and endometrial cancer risk: a synthetic review. Cancer Epidemiol Biomarkers Prev. 2002;11:1531–1543. [PubMed] [Google Scholar]
- 5.Horn LC, Schnurrbusch U, Bilek K, Hentschel B, Einenkel J. Risk of progression in complex and atypical endometrial hyperplasia: clinicopathologic analysis in cases with and without progestogen treatment. Int J Gynecol Cancer. 2004;14:348–353. doi: 10.1111/j.1048-891x.2004.014220.x. [DOI] [PubMed] [Google Scholar]
- 6.Daud S, Jalil SS, Griffin M, Ewies AA. Endometrial hyperplasia - the dilemma of management remains: a retrospective observational study of 280 women. Eur J Obstet Gynecol Reprod Biol. 2011;159:172–175. doi: 10.1016/j.ejogrb.2011.06.023. [DOI] [PubMed] [Google Scholar]
- 7.Ozdegirmenci O, Kayikcioglu F, Bozkurt U, Akgul MA, Haberal A. Comparison of the efficacy of three progestins in the treatment of simple endometrial hyperplasia without atypia. Gynecol Obstet Invest. 2011;72:10–14. doi: 10.1159/000321390. [DOI] [PubMed] [Google Scholar]
- 8.Nieman KM, Romero IL, Van Houten B, Lengyel E. Adipose tissue and adipocytes support tumorigenesis and metastasis. Biochim Biophys Acta. 2013;1831:1533–1541. doi: 10.1016/j.bbalip.2013.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Q, Shen Q, Celestino J, Milam MR, Westin SN, Lacour RA, et al. Enhanced estrogen-induced proliferation in obese rat endometrium. Am J Obstet Gynecol. 2009;200:186.e1–186.e8. doi: 10.1016/j.ajog.2008.08.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gunin AG, Mashin IN, Zakharov DA. Proliferation, mitosis orientation and morphogenetic changes in the uterus of mice following chronic treatment with both estrogen and glucocorticoid hormones. J Endocrinol. 2001;169:23–31. doi: 10.1677/joe.0.1690023. [DOI] [PubMed] [Google Scholar]
- 11.Deligdisch L. Hormonal pathology of the endometrium. Mod Pathol. 2000;13:285–294. doi: 10.1038/modpathol.3880050. [DOI] [PubMed] [Google Scholar]
- 12.Silverberg SG. Problems in the differential diagnosis of endometrial hyperplasia and carcinoma. Mod Pathol. 2000;13:309–327. doi: 10.1038/modpathol.3880053. [DOI] [PubMed] [Google Scholar]
- 13.Kurman RJ, Kaminski PF, Norris HJ. The behavior of endometrial hyperplasia. A long-term study of “untreated” hyperplasia in 170 patients. Cancer. 1985;56:403–412. doi: 10.1002/1097-0142(19850715)56:2<403::aid-cncr2820560233>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 14.Montgomery BE, Daum GS, Dunton CJ. Endometrial hyperplasia: a review. Obstet Gynecol Surv. 2004;59:368–378. doi: 10.1097/00006254-200405000-00025. [DOI] [PubMed] [Google Scholar]
- 15.Palmer JE, Perunovic B, Tidy JA. Endometrial hyperplasia. Obstet Gynaecol. 2008;10:211–216. [Google Scholar]
- 16.Reed SD, Newton KM, Garcia RL, Allison KH, Voigt LF, Jordan CD, et al. Complex hyperplasia with and without atypia: clinical outcomes and implications of progestin therapy. Obstet Gynecol. 2010;116(2 Pt 1):365–373. doi: 10.1097/AOG.0b013e3181e93330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bese T, Vural A, Ozturk M, Dagistanli F, Demirkiran F, Tuncdemir M, et al. The effect of long-term use of progesterone therapy on proliferation and apoptosis in simple endometrial hyperplasia without atypia. Int J Gynecol Cancer. 2006;16:809–813. doi: 10.1111/j.1525-1438.2006.00533.x. [DOI] [PubMed] [Google Scholar]
- 18.Haimovich S, Checa MA, Mancebo G, Fusté P, Carreras R. Treatment of endometrial hyperplasia without atypia in peri- and postmenopausal women with a levonorgestrel intrauterine device. Menopause. 2008;15:1002–1004. doi: 10.1097/gme.0b013e3181659837. [DOI] [PubMed] [Google Scholar]
- 19.Anastasiadis PG, Skaphida PG, Koutlaki NG, Galazios GC, Tsikouras PN, Liberis VA. Descriptive epidemiology of endometrial hyperplasia in patients with abnormal uterine bleeding. Eur J Gynaecol Oncol. 2000;21:131–134. [PubMed] [Google Scholar]
- 20.Kim MK, Seong SJ. Conservative treatment for atypical endometrial hyperplasia: what is the most effective therapeutic method? J Gynecol Oncol. 2014;25:164–165. doi: 10.3802/jgo.2014.25.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cormio A, Guerra F, Cormio G, Pesce V, Fracasso F, Loizzi V, et al. Mitochondrial DNA content and mass increase in progression from normal to hyperplastic to cancer endometrium. BMC Res Notes. 2012;5:279. doi: 10.1186/1756-0500-5-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wheeler DT, Bristow RE, Kurman RJ. Histologic alterations in endometrial hyperplasia and well-differentiated carcinoma treated with progestins. Am J Surg Pathol. 2007;31:988–998. doi: 10.1097/PAS.0b013e31802d68ce. [DOI] [PubMed] [Google Scholar]
- 23.Mutter GL. Endometrial intraepithelial neoplasia (EIN): will it bring order to chaos? The Endometrial Collaborative Group. Gynecol Oncol. 2000;76:287–290. doi: 10.1006/gyno.1999.5580. [DOI] [PubMed] [Google Scholar]
- 24.Baak JP, Mutter GL. EIN and WHO94. J Clin Pathol. 2005;58:1–6. doi: 10.1136/jcp.2004.021071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campbell PE, Barter RA. The significance of a typical endometrial hyperplasia. J Obstet Gynaecol Br Commonw. 1961;68:668–672. doi: 10.1111/j.1471-0528.1961.tb02789.x. [DOI] [PubMed] [Google Scholar]
- 26.Gusberg SB, Kaplan AL. Precursors of corpus cancer. iv. adenomatous hyperplasia as stage o carcinoma of the endometrium. Am J Obstet Gynecol. 1963;87:662–678. [PubMed] [Google Scholar]
- 27.Gore H, Hertig AT. Carcinoma in situ of the endometrium. Am J Obstet Gynecol. 1966;94:134–155. doi: 10.1016/0002-9378(66)90391-7. [DOI] [PubMed] [Google Scholar]
- 28.Vellios F. Endometrial hyperplasias, precursors of endometrial carcinoma. Pathol Annu. 1972;7:201–229. [PubMed] [Google Scholar]
- 29.Tavassoli F, Kraus FT. Endometrial lesions in uteri resected for atypical endometrial hyperplasia. Am J Clin Pathol. 1978;70:770–779. doi: 10.1093/ajcp/70.5.770. [DOI] [PubMed] [Google Scholar]
- 30.Hendrickson MR, Kempson RL. Surgical pathology of the uterine corpus. Major Probl Pathol. 1979;12:1–580. [PubMed] [Google Scholar]
- 31.Bergeron C, Nogales FF, Masseroli M, Abeler V, Duvillard P, Müller-Holzner E, et al. A multicentric European study testing the reproducibility of the WHO classification of endometrial hyperplasia with a proposal of a simplified working classification for biopsy and curettage specimens. Am J Surg Pathol. 1999;23:1102–1108. doi: 10.1097/00000478-199909000-00014. [DOI] [PubMed] [Google Scholar]
- 32.Trimble CL, Method M, Leitao M, Lu K, Ioffe O, Hampton M, et al. Management of endometrial precancers. Obstet Gynecol. 2012;120:1160–1175. doi: 10.1097/aog.0b013e31826bb121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oza AM, Eisenhauer EA, Elit L, Cutz JC, Sakurada A, Tsao MS, et al. Phase II study of erlotinib in recurrent or metastatic endometrial cancer: NCIC IND-148. J Clin Oncol. 2008;26:4319–4325. doi: 10.1200/JCO.2007.15.8808. [DOI] [PubMed] [Google Scholar]
- 34.Scully RE, Bonfiglio TA, Kurman RJ, Silverberg SG, Wilkinson EJ. 2nd ed. New York: Springer-Verlag; 1994. Histological typing of female genital tract tumours. [Google Scholar]
- 35.Lacey JV, Jr, Mutter GL, Nucci MR, Ronnett BM, Ioffe OB, Rush BB, et al. Risk of subsequent endometrial carcinoma associated with endometrial intraepithelial neoplasia classification of endometrial biopsies. Cancer. 2008;113:2073–2081. doi: 10.1002/cncr.23808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Owings RA, Quick CM. Endometrial intraepithelial neoplasia. Arch Pathol Lab Med. 2014;138:484–491. doi: 10.5858/arpa.2012-0709-RA. [DOI] [PubMed] [Google Scholar]
- 37.Salman MC, Usubutun A, Boynukalin K, Yuce K. Comparison of WHO and endometrial intraepithelial neoplasia classifications in predicting the presence of coexistent malignancy in endometrial hyperplasia. J Gynecol Oncol. 2010;21:97–101. doi: 10.3802/jgo.2010.21.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kleebkaow P, Maneetab S, Somboonporn W, Seejornj K, Thinkhamrop J, Kamwilaisak R. Preoperative and postoperative agreement of histopathological findings in cases of endometrial hyperplasia. Asian Pac J Cancer Prev. 2008;9:89–91. [PubMed] [Google Scholar]
- 39.Terakawa N, Kigawa J, Taketani Y, Yoshikawa H, Yajima A, Noda K, et al. The behavior of endometrial hyperplasia: a prospective study. J Obstet Gynaecol Res. 1997;23:223–230. doi: 10.1111/j.1447-0756.1997.tb00836.x. [DOI] [PubMed] [Google Scholar]
- 40.Widra EA, Dunton CJ, McHugh M, Palazzo JP. Endometrial hyperplasia and the risk of carcinoma. Int J Gynecol Cancer. 1995;5:233–235. doi: 10.1046/j.1525-1438.1995.05030233.x. [DOI] [PubMed] [Google Scholar]
- 41.Bernstein L. The risk of breast, endometrial and ovarian cancer in users of hormonal preparations. Basic Clin Pharmacol Toxicol. 2006;98:288–296. doi: 10.1111/j.1742-7843.2006.pto_277.x. [DOI] [PubMed] [Google Scholar]
- 42.Farquhar CM, Lethaby A, Sowter M, Verry J, Baranyai J. An evaluation of risk factors for endometrial hyperplasia in premenopausal women with abnormal menstrual bleeding. Am J Obstet Gynecol. 1999;181:525–529. doi: 10.1016/s0002-9378(99)70487-4. [DOI] [PubMed] [Google Scholar]
- 43.Ricci E, Moroni S, Parazzini F, Surace M, Benzi G, Salerio B, et al. Risk factors for endometrial hyperplasia: results from a case-control study. Int J Gynecol Cancer. 2002;12:257–260. doi: 10.1046/j.1525-1438.2002.01105.x. [DOI] [PubMed] [Google Scholar]
- 44.Fu YS, Gambone JC, Berek JS. Pathophysiology and management of endometrial hyperplasia and carcinoma. West J Med. 1990;153:50–61. [PMC free article] [PubMed] [Google Scholar]
- 45.Epplein M, Reed SD, Voigt LF, Newton KM, Holt VL, Weiss NS. Risk of complex and atypical endometrial hyperplasia in relation to anthropometric measures and reproductive history. Am J Epidemiol. 2008;168:563–570. doi: 10.1093/aje/kwn168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baskin GB, Smith SM, Marx PA. Endometrial hyperplasia, polyps, and adenomyosis associated with unopposed estrogen in rhesus monkeys (Macaca mulatta) Vet Pathol. 2002;39:572–575. doi: 10.1354/vp.39-5-572. [DOI] [PubMed] [Google Scholar]
- 47.Grady D, Gebretsadik T, Kerlikowske K, Ernster V, Petitti D. Hormone replacement therapy and endometrial cancer risk: a meta-analysis. Obstet Gynecol. 1995;85:304–313. doi: 10.1016/0029-7844(94)00383-O. [DOI] [PubMed] [Google Scholar]
- 48.Sherman ME. Theories of endometrial carcinogenesis: a multidisciplinary approach. Mod Pathol. 2000;13:295–308. doi: 10.1038/modpathol.3880051. [DOI] [PubMed] [Google Scholar]
- 49.The Writing Group for the PEPI Trial. Effects of hormone replacement therapy on endometrial histology in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. JAMA. 1996;275:370–375. doi: 10.1001/jama.1996.03530290040035. [DOI] [PubMed] [Google Scholar]
- 50.Hannemann MM, Alexander HM, Cope NJ, Acheson N. Endometrial hyperplasia: a clinician’s review. Obstet Gynaecol Reprod Med. 2007;17:169–172. [Google Scholar]
- 51.Ferreira AM, Westers H, Albergaria A, Seruca R, Hofstra RM. Estrogens, MSI and Lynch syndrome-associated tumors. Biochim Biophys Acta. 2009;1796:194–200. doi: 10.1016/j.bbcan.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 52.Zhdanov AV, Sukhikh GT, Davydova MP, Slukina TV, Chernukha GE, Samoilova TE, et al. Correlations in the cytokine system in endometrial hyperplasia. Bull Exp Biol Med. 2003;136:270–272. doi: 10.1023/b:bebm.0000008980.25653.1b. [DOI] [PubMed] [Google Scholar]
- 53.Sukhikh GT, Zhdanov AV, Davydova MP, Slukina TV, Chernukha GE, Samoilova TE, et al. Disorders in cytokine gene expression in endometrial hyperplasia and effect of hormone therapy. Bull Exp Biol Med. 2005;139:235–237. doi: 10.1007/s10517-005-0257-7. [DOI] [PubMed] [Google Scholar]
- 54.Bruchim I, Sarfstein R, Werner H. The IGF Hormonal Network in Endometrial Cancer: Functions, Regulation, and Targeting Approaches. Front Endocrinol (Lausanne) 2014;5:76. doi: 10.3389/fendo.2014.00076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McCampbell AS, Broaddus RR, Loose DS, Davies PJ. Overexpression of the insulin-like growth factor I receptor and activation of the AKT pathway in hyperplastic endometrium. Clin Cancer Res. 2006;12:6373–6378. doi: 10.1158/1078-0432.CCR-06-0912. [DOI] [PubMed] [Google Scholar]
- 56.Vaskivuo TE, Stenbäck F, Tapanainen JS. Apoptosis and apoptosis-related factors Bcl-2, Bax, tumor necrosis factor-alpha, and NF-kappaB in human endometrial hyperplasia and carcinoma. Cancer. 2002;95:1463–1471. doi: 10.1002/cncr.10876. [DOI] [PubMed] [Google Scholar]
- 57.Levine RL, Cargile CB, Blazes MS, van Rees B, Kurman RJ, Ellenson LH. PTEN mutations and microsatellite instability in complex atypical hyperplasia, a precursor lesion to uterine endometrioid carcinoma. Cancer Res. 1998;58:3254–3258. [PubMed] [Google Scholar]
- 58.Maxwell GL, Risinger JI, Gumbs C, Shaw H, Bentley RC, Barrett JC, et al. Mutation of the PTEN tumor suppressor gene in endometrial hyperplasias. Cancer Res. 1998;58:2500–2503. [PubMed] [Google Scholar]
- 59.Dobrzycka B, Terlikowski SJ, Mazurek A, Kowalczuk O, Niklińska W, Chyczewski L, et al. Mutations of the KRAS oncogene in endometrial hyperplasia and carcinoma. Folia Histochem Cytobiol. 2009;47:65–68. doi: 10.2478/v10042-009-0014-2. [DOI] [PubMed] [Google Scholar]
- 60.Saegusa M, Hashimura M, Yoshida T, Okayasu I. beta-Catenin mutations and aberrant nuclear expression during endometrial tumorigenesis. Br J Cancer. 2001;84:209–217. doi: 10.1054/bjoc.2000.1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hayes MP, Wang H, Espinal-Witter R, Douglas W, Solomon GJ, Baker SJ, et al. PIK3CA and PTEN mutations in uterine endometrioid carcinoma and complex atypical hyperplasia. Clin Cancer Res. 2006;12(20 Pt 1):5932–5935. doi: 10.1158/1078-0432.CCR-06-1375. [DOI] [PubMed] [Google Scholar]
- 62.Hardisson D, Moreno-Bueno G, Sánchez L, Sarrió D, Suárez A, Calero F, et al. Tissue microarray immunohistochemical expression analysis of mismatch repair (hMLH1 and hMSH2 genes) in endometrial carcinoma and atypical endometrial hyperplasia: relationship with microsatellite instability. Mod Pathol. 2003;16:1148–1158. doi: 10.1097/01.MP.0000095646.70007.6A. [DOI] [PubMed] [Google Scholar]
- 63.Bednarek M, Constantinou M, Kqpczyfiskil L, Shiar Kassassir A, Sobczuk A, Wieszczycka M, et al. Evaluation of genomic imbalance in endometrial hyperplasia and carcinoma. Ginekol Pol. 2014;85:828–832. doi: 10.17772/gp/1908. [DOI] [PubMed] [Google Scholar]
- 64.Fabjani G, Kucera E, Schuster E, Minai-Pour M, Czerwenka K, Sliutz G, et al. Genetic alterations in endometrial hyperplasia and cancer. Cancer Lett. 2002;175:205–211. doi: 10.1016/s0304-3835(01)00714-5. [DOI] [PubMed] [Google Scholar]
- 65.O’Hara AJ, Bell DW. The genomics and genetics of endometrial cancer. Adv Genomics Genet. 2012;2012:33–47. doi: 10.2147/AGG.S28953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dieudonné AS, Lambrechts D, Smeets D, Belmans A, Wildiers H, Paridaens R, et al. The rs1800716 variant in CYP2D6 is associated with an increased double endometrial thickness in postmenopausal women on tamoxifen. Ann Oncol. 2014;25:90–95. doi: 10.1093/annonc/mdt399. [DOI] [PubMed] [Google Scholar]
- 67.Aban M, Arslan M, Tok E, Tekes S, Budak T, Altintas A. CYP17 genetic polymorphism in patients with endometrial hyperplasia and cancer. Int J Gynecol Cancer. 2006;16(Suppl 1):448–451. doi: 10.1111/j.1525-1438.2006.00417.x. [DOI] [PubMed] [Google Scholar]
- 68.Ivanova TI, Krikunova LI, Ryabchenko NI, Mkrtchyan LS, Khorokhorina VA, Salnikova LE. Association of the apolipoprotein E 2 allele with concurrent occurrence of endometrial hyperplasia and endometrial carcinoma. Oxid Med Cell Longev. 2015;2015:593658. doi: 10.1155/2015/593658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jordan VC. Tamoxifen: the herald of a new era of preventive therapeutics. J Natl Cancer Inst. 1997;89:747–749. doi: 10.1093/jnci/89.11.747. [DOI] [PubMed] [Google Scholar]
- 70.Lee WL, Cheng MH, Chao HT, Wang PH. The role of selective estrogen receptor modulators on breast cancer: from tamoxifen to raloxifene. Taiwan J Obstet Gynecol. 2008;47:24–31. doi: 10.1016/S1028-4559(08)60051-0. [DOI] [PubMed] [Google Scholar]
- 71.Gradishar WJ. Tamoxifen--what next? Oncologist. 2004;9:378–384. doi: 10.1634/theoncologist.9-4-378. [DOI] [PubMed] [Google Scholar]
- 72.Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687–1717. doi: 10.1016/S0140-6736(05)66544-0. [DOI] [PubMed] [Google Scholar]
- 73.Killackey MA, Hakes TB, Pierce VK. Endometrial adenocarcinoma in breast cancer patients receiving antiestrogens. Cancer Treat Rep. 1985;69:237–238. [PubMed] [Google Scholar]
- 74.Vollmer G. Endometrial cancer: experimental models useful for studies on molecular aspects of endometrial cancer and carcinogenesis. Endocr Relat Cancer. 2003;10:23–42. doi: 10.1677/erc.0.0100023. [DOI] [PubMed] [Google Scholar]
- 75.Berlière M, Charles A, Galant C, Donnez J. Uterine side effects of tamoxifen: a need for systematic pretreatment screening. Obstet Gynecol. 1998;91:40–44. doi: 10.1016/s0029-7844(97)00591-7. [DOI] [PubMed] [Google Scholar]
- 76.Kedar RP, Bourne TH, Powles TJ, Collins WP, Ashley SE, Cosgrove DO, et al. Effects of tamoxifen on uterus and ovaries of postmenopausal women in a randomised breast cancer prevention trial. Lancet. 1994;343:1318–1321. doi: 10.1016/s0140-6736(94)92466-x. [DOI] [PubMed] [Google Scholar]
- 77.Hann LE, Giess CS, Bach AM, Tao Y, Baum HJ, Barakat RR. Endometrial thickness in tamoxifen-treated patients: correlation with clinical and pathologic findings. AJR Am J Roentgenol. 1997;168:657–661. doi: 10.2214/ajr.168.3.9057510. [DOI] [PubMed] [Google Scholar]
- 78.Sargent LM, Dragan YP, Bahnub N, Wiley JE, Sattler CA, Schroeder P, et al. Tamoxifen induces hepatic aneuploidy and mitotic spindle disruption after a single in vivo administration to female Sprague-Dawley rats. Cancer Res. 1994;54:3357–3360. [PubMed] [Google Scholar]
- 79.Brown K. Is tamoxifen a genotoxic carcinogen in women? Mutagenesis. 2009;24:391–404. doi: 10.1093/mutage/gep022. [DOI] [PubMed] [Google Scholar]
- 80.Shang Y. Molecular mechanisms of oestrogen and SERMs in endometrial carcinogenesis. Nat Rev Cancer. 2006;6:360–368. doi: 10.1038/nrc1879. [DOI] [PubMed] [Google Scholar]
- 81.Shang Y. Hormones and cancer. Cell Res. 2007;17:277–279. doi: 10.1038/cr.2007.26. [DOI] [PubMed] [Google Scholar]
- 82.Shang Y, Brown M. Molecular determinants for the tissue specificity of SERMs. Science. 2002;295:2465–2468. doi: 10.1126/science.1068537. [DOI] [PubMed] [Google Scholar]
- 83.Bai JX, Yan B, Zhao ZN, Xiao X, Qin WW, Zhang R, et al. Tamoxifen represses miR-200 microRNAs and promotes epithelial-to-mesenchymal transition by up-regulating c-Myc in endometrial carcinoma cell lines. Endocrinology. 2013;154:635–645. doi: 10.1210/en.2012-1607. [DOI] [PubMed] [Google Scholar]
- 84.Tergas AI, Buell-Gutbrod R, Gwin K, Kocherginsky M, Temkin SM, Fefferman A, et al. Clinico-pathologic comparison of type II endometrial cancers based on tamoxifen exposure. Gynecol Oncol. 2012;127:316–320. doi: 10.1016/j.ygyno.2012.07.105. [DOI] [PubMed] [Google Scholar]
- 85.Amezcua CA, Lu JJ, Felix JC, Stanczyk FZ, Zheng W. Apoptosis may be an early event of progestin therapy for endometrial hyperplasia. Gynecol Oncol. 2000;79:169–176. doi: 10.1006/gyno.2000.5955. [DOI] [PubMed] [Google Scholar]
- 86.Abulafia O, Triest WE, Adcock JT, Sherer DM. The effect of medroxyprogesterone acetate on angiogenesis in complex endometrial hyperplasia. Gynecol Oncol. 1999;72:193–198. doi: 10.1006/gyno.1998.5106. [DOI] [PubMed] [Google Scholar]
- 87.Reed SD, Voigt LF, Newton KM, Garcia RH, Allison HK, Epplein M, et al. Progestin therapy of complex endometrial hyperplasia with and without atypia. Obstet Gynecol. 2009;113:655–662. doi: 10.1097/AOG.0b013e318198a10a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Figueroa-Casas PR, Ettinger B, Delgado E, Javkin A, Vieder C. Reversal by medical treatment of endometrial hyperplasia caused by estrogen replacement therapy. Menopause. 2001;8:420–423. doi: 10.1097/00042192-200111000-00006. [DOI] [PubMed] [Google Scholar]
- 89.Reifenstein EC., Jr The treatment of advanced endometrial cancer with hydroxyprogesterone caproate. Gynecol Oncol. 1974;2:377–414. doi: 10.1016/0090-8258(74)90029-8. [DOI] [PubMed] [Google Scholar]
- 90.Saegusa M, Okayasu I. Progesterone therapy for endometrial carcinoma reduces cell proliferation but does not alter apoptosis. Cancer. 1998;83:111–121. doi: 10.1002/(sici)1097-0142(19980701)83:1<111::aid-cncr15>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 91.Gunderson CC, Fader AN, Carson KA, Bristow RE. Oncologic and reproductive outcomes with progestin therapy in women with endometrial hyperplasia and grade 1 adenocarcinoma: a systematic review. Gynecol Oncol. 2012;125:477–482. doi: 10.1016/j.ygyno.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 92.Emarh M. Cyclic versus continuous medroxyprogesterone acetate for treatment of endometrial hyperplasia without atypia: a 2-year observational study. Arch Gynecol Obstet. 2015;292:1339–1343. doi: 10.1007/s00404-015-3749-3. [DOI] [PubMed] [Google Scholar]
- 93.Ushijima K, Yahata H, Yoshikawa H, Konishi I, Yasugi T, Saito T, et al. Multicenter phase II study of fertility-sparing treatment with medroxyprogesterone acetate for endometrial carcinoma and atypical hyperplasia in young women. J Clin Oncol. 2007;25:2798–2803. doi: 10.1200/JCO.2006.08.8344. [DOI] [PubMed] [Google Scholar]
- 94.Vereide AB, Arnes M, Straume B, Maltau JM, Ørbo A. Nuclear morphometric changes and therapy monitoring in patients with endometrial hyperplasia: a study comparing effects of intrauterine levonorgestrel and systemic medroxyprogesterone. Gynecol Oncol. 2003;91:526–533. doi: 10.1016/j.ygyno.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 95.Güven M, Dikmen Y, Terek MC, Ozsaran AA, Itil IM, Erhan Y. Metabolic effects associated with high-dose continuous megestrol acetate administration in the treatment of endometrial pathology. Arch Gynecol Obstet. 2001;265:183–186. doi: 10.1007/s004040000154. [DOI] [PubMed] [Google Scholar]
- 96.Gal D, Edman CD, Vellios F, Forney JP. Long-term effect of megestrol acetate in the treatment of endometrial hyperplasia. Am J Obstet Gynecol. 1983;146:316–322. doi: 10.1016/0002-9378(83)90754-8. [DOI] [PubMed] [Google Scholar]
- 97.Wildemeersch D, Pylyser K, De Wever N, Pauwels P, Tjalma W. Endometrial safety after 5 years of continuous combined transdermal estrogen and intrauterine levonorgestrel delivery for postmenopausal hormone substitution. Maturitas. 2007;57:205–209. doi: 10.1016/j.maturitas.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 98.Orbo A, Vereide A, Arnes M, Pettersen I, Straume B. Levonorgestrel-impregnated intrauterine device as treatment for endometrial hyperplasia: a national multicentre randomised trial. BJOG. 2014;121:477–486. doi: 10.1111/1471-0528.12499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Abu Hashim H, Zayed A, Ghayaty E, El Rakhawy M. LNG-IUS treatment of non-atypical endometrial hyperplasia in perimenopausal women: a randomized controlled trial. J Gynecol Oncol. 2013;24:128–134. doi: 10.3802/jgo.2013.24.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Varma R, Soneja H, Bhatia K, Ganesan R, Rollason T, Clark TJ, et al. The effectiveness of a levonorgestrel-releasing intrauterine system (LNG-IUS) in the treatment of endometrial hyperplasia--a long-term follow-up study. Eur J Obstet Gynecol Reprod Biol. 2008;139:169–175. doi: 10.1016/j.ejogrb.2008.02.022. [DOI] [PubMed] [Google Scholar]
- 101.Garza-Flores J, Menjívar M, Cardenas M, Reynoso M, García GA, Pérez Palacios G. Further studies on the antigonadotropic mechanism of action of norethisterone. J Steroid Biochem Mol Biol. 1991;38:89–93. doi: 10.1016/0960-0760(91)90406-u. [DOI] [PubMed] [Google Scholar]
- 102.Gong Z, Chandler K, Webster S, Kerley R, Buist S, McCort-Tipton M. Simple and rapid determination of norethindrone in human plasma by supported liquid extraction and ultra performance liquid chromatography with tandem mass spectrometry. Talanta. 2012;91:77–82. doi: 10.1016/j.talanta.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 103.Portman DJ, Symons JP, Wilborn W, Kempfert NJ. A randomized, double-blind, placebo-controlled, multicenter study that assessed the endometrial effects of norethindrone acetate plus ethinyl estradiol versus ethinyl estradiol alone. Am J Obstet Gynecol. 2003;188:334–342. doi: 10.1067/mob.2003.91. [DOI] [PubMed] [Google Scholar]
- 104.Genazzani AR, Schmelter T, Schaefers M, Gerlinger C, Gude K. One-year randomized study of the endometrial safety and bleeding pattern of 0.25 mg drospirenone/0.5 mg 17β-estradiol in postmenopausal women. Climacteric. 2013;16:490–498. doi: 10.3109/13697137.2013.783797. [DOI] [PubMed] [Google Scholar]
- 105.Brun JL, Belaisch J, Rivel J, Hocké C. Endometrial hyperplasias resistant to progestins: alternatives to traditional treatments. Gynecol Obstet Fertil. 2002;30:244–251. doi: 10.1016/s1297-9589(02)00301-6. [DOI] [PubMed] [Google Scholar]
- 106.Upson K, Allison KH, Reed SD, Jordan CD, Newton KM, Swisher EM, et al. Biomarkers of progestin therapy resistance and endometrial hyperplasia progression. Am J Obstet Gynecol. 2012;207:36.e1–36.e8. doi: 10.1016/j.ajog.2012.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang S, Pudney J, Song J, Mor G, Schwartz PE, Zheng W. Mechanisms involved in the evolution of progestin resistance in human endometrial hyperplasia--precursor of endometrial cancer. Gynecol Oncol. 2003;88:108–117. doi: 10.1016/s0090-8258(02)00008-2. [DOI] [PubMed] [Google Scholar]
- 108.Chen X, Zhang Z, Feng Y, Fadare O, Wang J, Ai Z, et al. Aberrant survivin expression in endometrial hyperplasia: another mechanism of progestin resistance. Mod Pathol. 2009;22:699–708. doi: 10.1038/modpathol.2009.25. [DOI] [PubMed] [Google Scholar]
- 109.Greenblatt RB, Dmowski WP, Mahesh VB, Scholer HF. Clinical studies with an antigonadotropin-Danazol. Fertil Steril. 1971;22:102–112. doi: 10.1016/s0015-0282(16)38045-1. [DOI] [PubMed] [Google Scholar]
- 110.Fedele L, Marchini M, Bianchi S, Baglioni A, Bocciolone L, Nava S. Endometrial patterns during danazol and buserelin therapy for endometriosis: comparative structural and ultrastructural study. Obstet Gynecol. 1990;76:79–84. [PubMed] [Google Scholar]
- 111.Crosignani P, Olive D, Bergqvist A, Luciano A. Advances in the management of endometriosis: an update for clinicians. Hum Reprod Update. 2006;12:179–189. doi: 10.1093/humupd/dmi049. [DOI] [PubMed] [Google Scholar]
- 112.Sedati A, Mariani L, Giovinazzi R, Yacoub M, Atlante G. The effectiveness of danazol therapy in postmenopausal women affected by endometrial hyperplasia. Clin Exp Obstet Gynecol. 1992;19:161–165. [PubMed] [Google Scholar]
- 113.Mariani L, Sedati A, Giovinazzi R, Sindico R, Atlante G. Postmenopausal endometrial hyperplasia: role of danazol therapy. Int J Gynaecol Obstet. 1994;44:155–159. doi: 10.1016/0020-7292(94)90071-x. [DOI] [PubMed] [Google Scholar]
- 114.Soh E, Sato K. Clinical effects of danazol on endometrial hyperplasia in menopausal and postmenopausal women. Cancer. 1990;66:983–988. doi: 10.1002/1097-0142(19900901)66:5<983::aid-cncr2820660530>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 115.Grio R, Piacentino R, Marchino GL, Bocci A, Navone R. Danazol in the treatment of endometrial hyperplasia. Panminerva Med. 1993;35:231–233. [PubMed] [Google Scholar]
- 116.Harada T, Momoeda M, Taketani Y, Aso T, Fukunaga M, Hagino H, et al. Dienogest is as effective as intranasal buserelin acetate for the relief of pain symptoms associated with endometriosis--a randomized, double-blind, multicenter, controlled trial. Fertil Steril. 2009;91:675–681. doi: 10.1016/j.fertnstert.2007.12.080. [DOI] [PubMed] [Google Scholar]
- 117.Tamaoka Y, Orikasa H, Sumi Y, Sakakura K, Kamei K, Nagatani M, et al. Treatment of endometrial hyperplasia with a danazol-releasing intrauterine device: a prospective study. Gynecol Obstet Invest. 2004;58:42–48. doi: 10.1159/000077882. [DOI] [PubMed] [Google Scholar]
- 118.Cottreau CM, Ness RB, Modugno F, Allen GO, Goodman MT. Endometriosis and its treatment with danazol or lupron in relation to ovarian cancer. Clin Cancer Res. 2003;9:5142–5144. [PubMed] [Google Scholar]
- 119.Vercellini P, Somigliana E, Viganò P, Abbiati A, Barbara G, Crosignani PG. Endometriosis: current therapies and new pharmacological developments. Drugs. 2009;69:649–675. doi: 10.2165/00003495-200969060-00002. [DOI] [PubMed] [Google Scholar]
- 120.Akiyama T, Ishida J, Nakagawa S, Ogawara H, Watanabe S, Itoh N, et al. Genistein, a specific inhibitor of tyrosine-specific protein kinases. J Biol Chem. 1987;262:5592–5595. [PubMed] [Google Scholar]
- 121.Yamashita Y, Kawada S, Nakano H. Induction of mammalian topoisomerase II dependent DNA cleavage by nonintercalative flavonoids, genistein and orobol. Biochem Pharmacol. 1990;39:737–744. doi: 10.1016/0006-2952(90)90153-c. [DOI] [PubMed] [Google Scholar]
- 122.Lian Z, Niwa K, Tagami K, Hashimoto M, Gao J, Yokoyama Y, et al. Preventive effects of isoflavones, genistein and daidzein, on estradiol-17beta-related endometrial carcinogenesis in mice. Jpn J Cancer Res. 2001;92:726–734. doi: 10.1111/j.1349-7006.2001.tb01154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Granese R, Bitto A, Polito F, Triolo O, Giordano D, Santamaria A, et al. Genistein reduces angiogenesis and apoptosis in women with endometrial hyperplasia. Botanics. 2015;5:27–32. [Google Scholar]
- 124.Bitto A, Granese R, Triolo O, Villari D, Maisano D, Giordano D, et al. Genistein aglycone: a new therapeutic approach to reduce endometrial hyperplasia. Phytomedicine. 2010;17:844–850. doi: 10.1016/j.phymed.2010.03.024. [DOI] [PubMed] [Google Scholar]
- 125.Pernicova I, Korbonits M. Metformin--mode of action and clinical implications for diabetes and cancer. Nat Rev Endocrinol. 2014;10:143–156. doi: 10.1038/nrendo.2013.256. [DOI] [PubMed] [Google Scholar]
- 126.Nestler JE. Metformin for the treatment of the polycystic ovary syndrome. N Engl J Med. 2008;358:47–54. doi: 10.1056/NEJMct0707092. [DOI] [PubMed] [Google Scholar]
- 127.Shao R, Li X, Feng Y, Lin JF, Billig H. Direct effects of metformin in the endometrium: a hypothetical mechanism for the treatment of women with PCOS and endometrial carcinoma. J Exp Clin Cancer Res. 2014;33:41. doi: 10.1186/1756-9966-33-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Shen ZQ, Zhu HT, Lin JF. Reverse of progestin-resistant atypical endometrial hyperplasia by metformin and oral contraceptives. Obstet Gynecol. 2008;112:465–467. doi: 10.1097/AOG.0b013e3181719b92. [DOI] [PubMed] [Google Scholar]
- 129.Cantrell LA, Zhou C, Mendivil A, Malloy KM, Gehrig PA, Bae-Jump VL. Metformin is a potent inhibitor of endometrial cancer cell proliferation--implications for a novel treatment strategy. Gynecol Oncol. 2010;116:92–98. doi: 10.1016/j.ygyno.2009.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Dowling RJ, Niraula S, Stambolic V, Goodwin PJ. Metformin in cancer: translational challenges. J Mol Endocrinol. 2012;48:R31–R43. doi: 10.1530/JME-12-0007. [DOI] [PubMed] [Google Scholar]
- 131.Ko EM, Walter P, Jackson A, Clark L, Franasiak J, Bolac C, et al. Metformin is associated with improved survival in endometrial cancer. Gynecol Oncol. 2014;132:438–442. doi: 10.1016/j.ygyno.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 132.Nevadunsky NS, Van Arsdale A, Strickler HD, Moadel A, Kaur G, Frimer M, et al. Metformin use and endometrial cancer survival. Gynecol Oncol. 2014;132:236–240. doi: 10.1016/j.ygyno.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Xie Y, Wang YL, Yu L, Hu Q, Ji L, Zhang Y, et al. Metformin promotes progesterone receptor expression via inhibition of mammalian target of rapamycin (mTOR) in endometrial cancer cells. J Steroid Biochem Mol Biol. 2011;126:113–120. doi: 10.1016/j.jsbmb.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 134.Erdemoglu E, Güney M, Giray SG, Take G, Mungan T. Effects of metformin on mammalian target of rapamycin in a mouse model of endometrial hyperplasia. Eur J Obstet Gynecol Reprod Biol. 2009;145:195–199. doi: 10.1016/j.ejogrb.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 135.Session DR, Kalli KR, Tummon IS, Damario MA, Dumesic DA. Treatment of atypical endometrial hyperplasia with an insulin-sensitizing agent. Gynecol Endocrinol. 2003;17:405–407. doi: 10.1080/09513590312331290298. [DOI] [PubMed] [Google Scholar]
- 136.Tas M, Kutuk MS, Serin IS, Ozgun MT, Oner G, Ozturk F. Comparison of antiproliferative effects of metformine and progesterone on estrogen-induced endometrial hyperplasia in rats. Gynecol Endocrinol. 2013;29:311–314. doi: 10.3109/09513590.2012.743010. [DOI] [PubMed] [Google Scholar]
- 137.Shan W, Wang C, Zhang Z, Gu C, Ning C, Luo X, et al. Conservative therapy with metformin plus megestrol acetate for endometrial atypical hyperplasia. J Gynecol Oncol. 2014;25:214–220. doi: 10.3802/jgo.2014.25.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Meresman GF, Bilotas MA, Lombardi E, Tesone M, Sueldo C, Barañao RI. Effect of GnRH analogues on apoptosis and release of interleukin-1beta and vascular endothelial growth factor in endometrial cell cultures from patients with endometriosis. Hum Reprod. 2003;18:1767–1771. doi: 10.1093/humrep/deg356. [DOI] [PubMed] [Google Scholar]
- 139.Agorastos T, Bontis J, Vakiani A, Vavilis D, Constantinidis T. Treatment of endometrial hyperplasias with gonadotropin-releasing hormone agonists: pathological, clinical, morphometric, and DNA-cytometric data. Gynecol Oncol. 1997;65:102–114. doi: 10.1006/gyno.1997.4639. [DOI] [PubMed] [Google Scholar]
- 140.Agorastos T, Vaitsi V, Paschopoulos M, Vakiani A, Zournatzi-Koiou V, Saravelos H, et al. Prolonged use of gonadotropin-releasing hormone agonist and tibolone as add-back therapy for the treatment of endometrial hyperplasia. Maturitas. 2004;48:125–132. doi: 10.1016/j.maturitas.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 141.Fister S, Günthert AR, Emons G, Gründker C. Gonadotropin-releasing hormone type II antagonists induce apoptotic cell death in human endometrial and ovarian cancer cells in vitro and in vivo. Cancer Res. 2007;67:1750–1756. doi: 10.1158/0008-5472.CAN-06-3222. [DOI] [PubMed] [Google Scholar]
- 142.Sirimusika N, Peeyananjarassri K, Suphasynth Y, Wootipoom V, Kanjanapradit K, Geater A. Management and clinical outcomes of endometrial hyperplasia during a 13-year period in Songklanagarind Hospital. J Med Assoc Thai. 2014;97:260–266. [PubMed] [Google Scholar]
- 143.Järvelä I, Tekay A, Santala M, Jouppila P. Thermal balloon endometrial ablation therapy induces a rise in uterine blood flow impedance: a randomized prospective color Doppler study. Ultrasound Obstet Gynecol. 2001;17:65–70. doi: 10.1046/j.1469-0705.2001.00317.x. [DOI] [PubMed] [Google Scholar]
- 144.Järvelä IY, Santala M. Treatment of non-atypic endometrial hyperplasia using thermal balloon endometrial ablation therapy. Gynecol Obstet Invest. 2005;59:202–206. doi: 10.1159/000084142. [DOI] [PubMed] [Google Scholar]
- 145.Vilos GA, Oraif A, Vilos AG, Ettler H, Edris F, Abu-Rafea B. Long-term clinical outcomes following resectoscopic endometrial ablation of non-atypical endometrial hyperplasia in women with abnormal uterine bleeding. J Minim Invasive Gynecol. 2015;22:66–77. doi: 10.1016/j.jmig.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 146.Vilos GA, Harding PG, Ettler HC. Resectoscopic surgery in women with abnormal uterine bleeding and nonatypical endometrial hyperplasia. J Am Assoc Gynecol Laparosc. 2002;9:131–137. doi: 10.1016/s1074-3804(05)60120-x. [DOI] [PubMed] [Google Scholar]
- 147.Mutter GL, Ferenczy A. Endometrial hyperplasia and neoplasia: definition, diagnosis, and management principles. Glob Libr Womens Med. 2008 doi: 10.3843/GLOWM.10235. [DOI] [Google Scholar]
- 148.Fatima I, Chandra V, Saxena R, Manohar M, Sanghani Y, Hajela K, et al. 2,3-Diaryl-2H-1-benzopyran derivatives interfere with classical and non-classical estrogen receptor signaling pathways, inhibit Akt activation and induce apoptosis in human endometrial cancer cells. Mol Cell Endocrinol. 2012;348:198–210. doi: 10.1016/j.mce.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 149.Zagouri F, Bozas G, Kafantari E, Tsiatas M, Nikitas N, Dimopoulos MA, et al. Endometrial cancer: what is new in adjuvant and molecularly targeted therapy? Obstet Gynecol Int. 2010;2010:749579. doi: 10.1155/2010/749579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Satyaswaroop PG, Clarke CL, Zaino RJ, Mortel R. Apparent resistance in human endometrial carcinoma during combination treatment with tamoxifen and progestin may result from desensitization following downregulation of tumor progesterone receptor. Cancer Lett. 1992;62:107–114. doi: 10.1016/0304-3835(92)90180-4. [DOI] [PubMed] [Google Scholar]
- 151.Neijt JP. Advances in the chemotherapy of gynecologic cancer. Curr Opin Oncol. 1994;6:531–538. doi: 10.1097/00001622-199409000-00015. [DOI] [PubMed] [Google Scholar]
- 152.Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health. 2014;6:95–114. doi: 10.2147/IJWH.S51083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Scott SM, Brown M, Come SE. Emerging data on the efficacy and safety of fulvestrant, a unique antiestrogen therapy for advanced breast cancer. Expert Opin Drug Saf. 2011;10:819–826. doi: 10.1517/14740338.2011.595560. [DOI] [PubMed] [Google Scholar]
- 154.Sourla A, Luo S, Labrie C, Bélanger A, Labrie F. Morphological changes induced by 6-month treatment of intact and ovariectomized mice with tamoxifen and the pure antiestrogen EM-800. Endocrinology. 1997;138:5605–5617. doi: 10.1210/endo.138.12.5560. [DOI] [PubMed] [Google Scholar]
- 155.Labrie F, Labrie C, Bélanger A, Simard J, Giguère V, Tremblay A, et al. EM-652 (SCH57068), a pure SERM having complete antiestrogenic activity in the mammary gland and endometrium. J Steroid Biochem Mol Biol. 2001;79:213–225. doi: 10.1016/s0960-0760(01)00139-x. [DOI] [PubMed] [Google Scholar]
- 156.Labrie F, Labrie C, Bélanger A, Simard J, Gauthier S, Luu-The V, et al. EM-652 (SCH 57068), a third generation SERM acting as pure antiestrogen in the mammary gland and endometrium. J Steroid Biochem Mol Biol. 1999;69:51–84. doi: 10.1016/s0960-0760(99)00065-5. [DOI] [PubMed] [Google Scholar]
- 157.Gauthier S, Cloutier J, Dory YL, Favre A, Mailhot J, Ouellet C, et al. Synthesis and structure-activity relationships of analogs of EM-652 (acolbifene), a pure selective estrogen receptor modulator. Study of nitrogen substitution. J Enzyme Inhib Med Chem. 2005;20:165–177. doi: 10.1080/14756360500043448. [DOI] [PubMed] [Google Scholar]
- 158.Elkak AE, Mokbel K. Pure antiestrogens and breast cancer. Curr Med Res Opin. 2001;17:282–289. [PubMed] [Google Scholar]
- 159.Tremblay A, Tremblay GB, Labrie C, Labrie F, Giguère V. EM-800, a novel antiestrogen, acts as a pure antagonist of the transcriptional functions of estrogen receptors alpha and beta. Endocrinology. 1998;139:111–118. doi: 10.1210/endo.139.1.5702. [DOI] [PubMed] [Google Scholar]
- 160.Sharma AP, Saeed A, Durani S, Kapil RS. Structure-activity relationship of antiestrogens. Effect of the side chain and its position on the activity of 2,3-diaryl-2H-1-benzopyrans. J Med Chem. 1990;33:3216–3222. doi: 10.1021/jm00174a019. [DOI] [PubMed] [Google Scholar]
- 161.Kharkwal G, Fatima I, Kitchlu S, Singh B, Hajela K, Dwivedi A. Anti-implantation effect of 2-[piperidinoethoxyphenyl]-3-[4-hydroxyphenyl]-2H-benzo(b)pyran, a potent antiestrogenic agent in rats. Fertil Steril. 2011;95:1322–1327. doi: 10.1016/j.fertnstert.2010.06.066. [DOI] [PubMed] [Google Scholar]
- 162.Chandra V, Fatima I, Saxena R, Kitchlu S, Sharma S, Hussain MK, et al. Apoptosis induction and inhibition of hyperplasia formation by 2-[piperidinoethoxyphenyl]-3-[4-hydroxyphenyl]-2H-benzo(b)pyran in rat uterus. Am J Obstet Gynecol. 2011;205:362.e1–362.e11. doi: 10.1016/j.ajog.2011.05.024. [DOI] [PubMed] [Google Scholar]
- 163.Chandra V, Fatima I, Manohar M, Popli P, Sirohi VK, Hussain MK, et al. Inhibitory effect of 2-(piperidinoethoxyphenyl)-3-(4-hydroxyphenyl)-2H-benzo(b)pyran (K-1) on human primary endometrial hyperplasial cells mediated via combined suppression of Wnt/β-catenin signaling and PI3K/Akt survival pathway. Cell Death Dis. 2014;5:e1380. doi: 10.1038/cddis.2014.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Siiteri PK. Adipose tissue as a source of hormones. Am J Clin Nutr. 1987;45(1 Suppl):277–282. doi: 10.1093/ajcn/45.1.277. [DOI] [PubMed] [Google Scholar]
- 165.Yu HC, Lin CY, Chang WC, Shen BJ, Chang WP, Chuang CM, et al. Increased association between endometriosis and endometrial cancer: a nationwide population-based retrospective cohort study. Int J Gynecol Cancer. 2015;25:447–452. doi: 10.1097/IGC.0000000000000384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Fabian CJ. The what, why and how of aromatase inhibitors: hormonal agents for treatment and prevention of breast cancer. Int J Clin Pract. 2007;61:2051–2063. doi: 10.1111/j.1742-1241.2007.01587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Bershteĭn LM, Maksimov SI, Danilova MA, Gershfel’d ED, Boiarkina MP, Khadzhimba AS, et al. Effectiveness of aromatase inhibitors in comparison with metformin for neoadjuvant treatment in patients with endometrial cancer. Vopr Onkol. 2011;57:737–741. [PubMed] [Google Scholar]
- 168.Lai CH, Huang HJ. The role of hormones for the treatment of endometrial hyperplasia and endometrial cancer. Curr Opin Obstet Gynecol. 2006;18:29–34. doi: 10.1097/01.gco.0000192994.37965.c6. [DOI] [PubMed] [Google Scholar]
- 169.Barker LC, Brand IR, Crawford SM. Sustained effect of the aromatase inhibitors anastrozole and letrozole on endometrial thickness in patients with endometrial hyperplasia and endometrial carcinoma. Curr Med Res Opin. 2009;25:1105–1109. doi: 10.1185/03007990902860549. [DOI] [PubMed] [Google Scholar]
- 170.Tabatabaie A, Karimi Zarchi M, Dehghani-Tafti M, Miratashi-Yazdi A, Teimoori S, Dehghani A. Comparing letrozole with medroxyprogesterone acetate (MPA) as hormonal therapy for simple endometrial hyperplasia without atypia in adult and middle-aged women. Eur J Gynaecol Oncol. 2013;34:552–555. [PubMed] [Google Scholar]
- 171.El-shamy M, Gibreel A, Refai E, Sadek E, Ragab A. Aromatase inhibitor “letrozole” versus progestin “norethisterone” in women with simple endometrial hyperplasia without atypia: a prospective cohort trial. Middle East Fertil Soc J. 2012;17:111–115. [Google Scholar]
- 172.Agorastos T, Vaitsi V, Pantazis K, Efstathiadis E, Vavilis D, Bontis JN. Aromatase inhibitor anastrozole for treating endometrial hyperplasia in obese postmenopausal women. Eur J Obstet Gynecol Reprod Biol. 2005;118:239–240. doi: 10.1016/j.ejogrb.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 173.Greenberger LM, Annable T, Collins KI, Komm BS, Lyttle CR, Miller CP, et al. A new antiestrogen, 2-(4-hydroxy-phenyl)-3-methyl-1-[4-(2-piperidin-1-yl-ethoxy)-benzyl]-1H-indol-5-ol hydrochloride (ERA-923), inhibits the growth of tamoxifen-sensitive and -resistant tumors and is devoid of uterotropic effects in mice and rats. Clin Cancer Res. 2001;7:3166–3177. [PubMed] [Google Scholar]
- 174.Morales L, Timmerman D, Neven P, Konstantinovic ML, Carbonez A, Van Huffel S, et al. Third generation aromatase inhibitors may prevent endometrial growth and reverse tamoxifen-induced uterine changes in postmenopausal breast cancer patients. Ann Oncol. 2005;16:70–74. doi: 10.1093/annonc/mdi021. [DOI] [PubMed] [Google Scholar]
- 175.Menendez JA, Oza BP, Atlas E, Verma VA, Mehmi I, Lupu R. Inhibition of tumor-associated fatty acid synthase activity antagonizes estradiol- and tamoxifen-induced agonist transactivation of estrogen receptor (ER) in human endometrial adenocarcinoma cells. Oncogene. 2004;23:4945–4958. doi: 10.1038/sj.onc.1207476. [DOI] [PubMed] [Google Scholar]
- 176.Dutertre M, Smith CL. Molecular mechanisms of selective estrogen receptor modulator (SERM) action. J Pharmacol Exp Ther. 2000;295:431–437. [PubMed] [Google Scholar]
- 177.Guo Y, Chen Y, Liu LB, Chang KK, Li H, Li MQ, et al. IL-22 in the endometriotic milieu promotes the proliferation of endometrial stromal cells via stimulating the secretion of CCL2 and IL-8. Int J Clin Exp Pathol. 2013;6:2011–2020. [PMC free article] [PubMed] [Google Scholar]
- 178.Li MQ, Li HP, Meng YH, Wang XQ, Zhu XY, Mei J, et al. Chemokine CCL2 enhances survival and invasiveness of endometrial stromal cells in an autocrine manner by activating Akt and MAPK/Erk1/2 signal pathway. Fertil Steril. 2012;97:919–929. doi: 10.1016/j.fertnstert.2011.12.049. [DOI] [PubMed] [Google Scholar]