Abstract
Background
The surrounding environment influences the constitution of illness perceptions. Therefore, local research is needed to examine how Libyan diabetes patients perceive diabetes and how their perceptions influence their medication adherence.
Methods
A cross-sectional study was conducted at the National Centre for Diabetes and Endocrinology in Tripoli, Libya, between October and December 2013. A total of 523 patients with type 2 diabetes participated in this study. A self-administered questionnaire was used for data collection; this included the Revised Illness Perception Questionnaire and the eight-item Morisky Medication Adherence Scale.
Results
The respondents showed moderately high personal control and treatment control perceptions and a moderate consequences perception. They reported a high perception of diabetes timeline as chronic and a moderate perception of the diabetes course as unstable. The most commonly perceived cause of diabetes was Allah's will. The prevalence of low medication adherence was 36.1%. The identified significant predictors of low medication adherence were the low treatment control perception (p=0.044), high diabetes identity perception (p=0.008), being male (p=0.026), and employed (p=0.008).
Conclusion
Diabetes illness perceptions of type 2 diabetic Libyans play a role in guiding the medication adherence and could be considered in the development of medication adherence promotion plans.
Keywords: diabetes, illness perceptions, medication adherence, Arabs, Libya
Diabetes is a major global health issue. The Middle East and North Africa (MENA) region faces the highest burden of this disease. Compared to the other world regions, this region has the highest comparative prevalence of diabetes (1). Libya is one of the MENA countries, with a comparative prevalence of diabetes of 9.86% (1). Medication adherence is important in diabetes management and studies have supported its relevance in achieving good glycemic control (2, 3). Despite its importance, the reported data on adherence to oral diabetes medications and insulin showed that low medication adherence is prevalent (4). The issue of low therapeutic adherence in chronic diseases is generally greater in developing countries than in developed countries (5). In Libya, a previous study among diabetics at Benghazi Diabetes Centre reported a considerable rate of suboptimal medication adherence (6), and a more recent study in the same center found that non-adherence to diabetes management advice as measured by glycosylated hemoglobin level was considerable (7). Therefore, there is a need to identify the factors that could influence medication adherence among Libyan diabetic patients.
Illness perceptions are among the modifiable factors that have been postulated to influence coping behaviors in illness. Therefore, studying them might help in understanding medication adherence among diabetics. This postulation has been presented by the Common Sense Model (CSM) of illness perceptions (8, 9). The CSM demonstrates the role of cognitive perceptions as well as the emotional representations of the illness in guiding human coping behaviors (8, 9). Several studies have shown that CSM illness perceptions influence coping behaviors in diabetes (10–14) and in other chronic diseases (15). In illness perception research, it is important to consider the context of the study population, because the surrounding atmosphere is one of the important sources of information that influences the constitution of illness perceptions (8, 9). The patient gathers information from several sources and processes them into illness perception constitutions. Among these sources of information is the personal context, like the patient's own memories about a previous illness experience, and also the interpersonal context and the surrounding environment (8). Therefore, different populations might constitute different perceptions about the same illness. Several studies have shown the differences in illness perceptions across different groups, both in diabetes (11, 16, 17) and other diseases (15).
Thus, to have a valid insight on how Libyan diabetics perceive their diabetes and how their perceptions influence their medication adherence, it is important to conduct local research. To the best of our knowledge, there has been no previous study on this topic in Libya. Overall, there is a paucity of research that relates psychological factors to patient behavior in the Libyan diabetes context. We identified one study that related self-efficacy – which is a close concept to one of the CSM illness perceptions, the personal control perception – to non-adherence to diabetes management advice (7). The aim of our paper was to assess diabetes illness perceptions among Libyans with type 2 diabetes mellitus (T2DM) and the influence of their diabetes perceptions on their medication adherence.
Materials and methods
Study settings and participants
This study was part of a larger study that looked at several outcomes, including diabetes coping behaviors and glycemic control status of T2DM patients. The study design was cross-sectional and it was conducted at the National Centre for Diabetes and Endocrinology (NCDE) in Tripoli, Libya, after being approved by Universiti Kebangsaan Malaysia Research and Ethics Committee and the management at the NCDE. The NCDE, although a referral center, provides diabetes follow-up, medications, and laboratory services for diabetes outpatients.
To find out the minimum sample size required for the large study, several calculations were performed. The largest sample size obtained was considered, and it was based on the sample size needed to test the difference in the prevalence of poor glycemic control across males and females using the Fleiss formula (18). The preliminary data used in the calculation included a prevalence of poor glycemic control among males of 45% and among females of 58% (19). A sample size of 498 was needed for a margin of precision (α) of 5% and a power of 80%. To compensate for low response and rejection due to non-eligibility, 30% was added. Thus, the target sample size was 648 respondents.
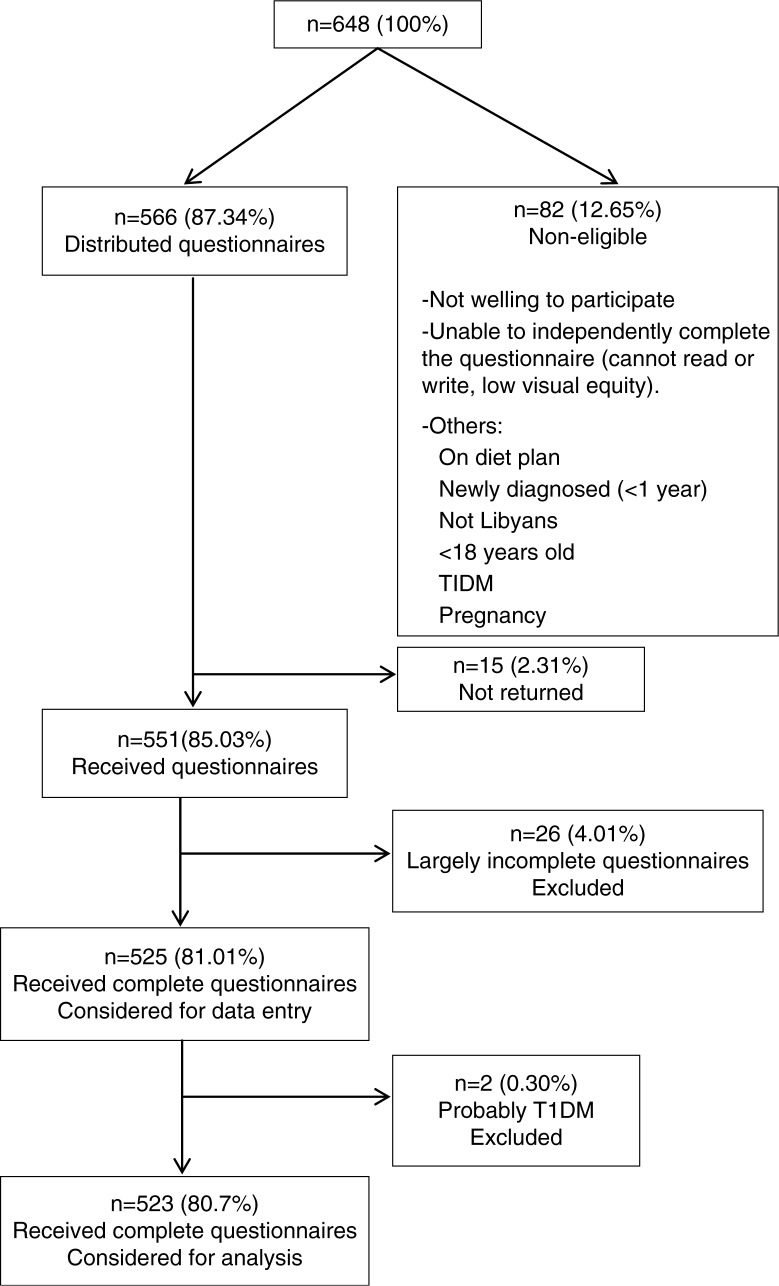
Patients were recruited systematically at the laboratory waiting area between October and December 2013, whereby every fourth patient was approached at their coming sequence. When the patient was not eligible, the immediate next patient was invited. The eligibility criteria included being Libyan, having T2DM for at least 1 year, being 18 years old or above, having no cognitive impairment that could interfere with communication or comprehending the questions, being able to read and write in Arabic, having no visual impairment that interfered with self-reporting, and being willing to participate in the study. Those who were placed on a diet plan only, pregnant women, and very ill patients were not eligible. The type of diabetes was self-reported, and it was verified whenever applicable by checking the medical follow-up card of each respondent. However, as not all the follow-up cards showed the type of diabetes, further verification of diabetes type was done at the stage of analysis. Those who reported being diagnosed before the age of 40, placed on insulin at diagnosis, and on insulin at the time of the study (20) were considered as having type 1 diabetes and were excluded from the analysis. Out of the 648 addressed patients, 523 responses were considered in the data analysis, which gave a response rate of 80.7%. Details on sampling flow are depicted in Fig. 1. Patients were given a briefing about the study, as well as on their participation and withdrawal rights. The study was conducted on a voluntary basis and consent forms were received.
Fig. 1.
Sampling flowchart.
Measures
Data collection was based on a self-reported questionnaire, which gathered information about patients’ sociodemographic characteristics and disease profile, their diabetes illness perceptions based on the Revised Illness Perception Questionnaire (IPQ-R), and medication adherence based on the eight-item Morisky Medication Adherence Scale (MMAS-8).
Data on age, sex, marital status, education level, employment status, income, duration of diabetes, type of diabetes medication, presence of comorbidity, and the number of other medications were gathered from the information sheet.
The Revised Illness Perception Questionnaire
The IPQ-R was used with permission to assess diabetes illness perceptions. A version for diabetes is available at the IPQ website. The IPQ-R is a well-validated instrument (21). It includes three sections. The first section represents the identity perception domain and comprises 14 listed symptoms. Each symptom is attached to a yes or no response. Identity perception refers to how the patient labels the illness. It is related to the number of symptoms the patients have experienced since their diabetes diagnosis and that they attribute to their diabetes. A high score indicates a high diabetes identity perception. The second section comprises 38 items and measures seven illness perception domains (timeline acute/chronic perception, timeline cyclical perception, consequences perception, personal control perception, treatment control perception, illness coherence, emotional representations). Each of the 38 items is attached to a five-level (strongly disagree – strongly agree) Likert-type response. Timeline acute-chronic perception (six items) refers to the perception of the illness duration. A high score indicates a strong perception of diabetes as a chronic (long-term) illness (sample item: ‘My diabetes will last a short time’). Timeline cyclical perception (four items) refers to the perception of the pattern of the course of the illness. A high score indicates a strong perception of diabetes course as a cyclical or unstable illness (sample item: ‘I go through cycles in which my diabetes gets better and worse’). Consequences perception (six items) refers to the perception of the seriousness of the illness and its impact on life. A high score indicates a perception of diabetes as a serious illness with negative impacts on life, social relationships, or economic status (sample item: ‘My diabetes is a serious condition’). Personal control perception (six items) refers to the patient's perception of his or her own ability to manage or control the illness. A high score indicates a high perception of the personal ability to control diabetes (sample item: ‘I have the power to influence my diabetes’). Treatment control perception (five items) refers to the perception of the effectiveness of treatment in controlling the illness. A high score indicates a high perception of the effectiveness of diabetes treatment in controlling diabetes (sample item: ‘My treatment can control my diabetes’). Illness coherence (five items) refers to the patient's perception of his or her own understanding of the illness. A high score indicates a high perception of the personal understanding of diabetes and that diabetes is perceived as a clear or unambiguous illness (sample item: ‘I have a clear picture or understanding of my condition’). Emotional representations (six items) refer to emotional responses to the illness. A high score refers to more emotional responses to diabetes and indicates that diabetes affects the patient emotionally and makes him or her emotionally distressed (sample item: ‘When I think about my diabetes I get upset’). The last section of the IPQ-R is the cause section, and it comprises 18 disparate items (causes). Each item is attached to a five-level (strongly disagree – strongly agree) Likert-type response. We dichotomized the responses to each cause item into yes and no, where yes indicated those who strongly agreed or agreed on the item as a cause for their diabetes (22). Only the eight illness perception domains (identity perception, timeline acute-chronic perception, timeline cyclical perception, consequences perception, personal control perception, treatment control perception, illness coherence, emotional representations) were defined as independent variables and tested for their contribution to medication adherence, whereas the cause section was only included for description. The scale was translated from English into Arabic by two bilingual translators using a forward–backward method. The content validity of the scale was assessed by a group of Libyan experts, and two items were added to the other 14 generic symptoms in the identity subscale –numbness and paresthesia. Another item was added to the 18 disparate items in the cause section – Allah's will or fate. Then, face validity was pretested on 10 diabetic Libyans and the necessary amendments to enhance the clarity were done.
The eight-item Morisky Medication Adherence Scale
The MMAS-8 was used to measure medication adherence. It is a valid (23, 24) single-dimension measure that comprises eight items (sample item: ‘When you travel or leave home, do you sometimes forget to bring along your medications?’). Each item is attached to a yes or no response, except for the last item, which has a five-level Likert-type response (23). The short construct of the MMAS-8 was useful as data were collected in a busy clinical setting (25). The possible total score range is from 0 to 8. A score of 8 indicates high adherence, a score of 6 and above but less than 8 indicates moderate adherence, whereas a score below 6 indicates low adherence (23, 24). An Arabic version was obtained with permission from the scale copyright owner. This version was found to be reliable and valid among Libyans with T2DM (26).
Data analysis
Data analysis was conducted using SPSS (version 22) for Windows. The internal consistency reliability of the IPQ-R and MMAS-8 was assessed using Cronbach's alpha. A chi-square test, independent t-test, and the Mann–Whitney U test were used to explore the bivariate associations between medication adherence and sociodemographic characteristics, disease profile, and illness perceptions. All variables that showed bivariate associations with medication adherence at a p-value of 0.25 or less were included in the multiple regression analysis. A two-step hierarchical binary multiple logistic regression was run to test the contribution of illness perceptions on low medication adherence. A p-value less than 0.05 was considered in the interpretation of the significance of the findings.
Results
Table 1 summarizes the sociodemographic characteristics and disease profile of the respondents. The mean age of the respondents was 54.43 (SD=10.03). The mean diabetes duration was 9.4 (SD=7.3) years, and the number of other long-term medications ranged from zero to seven.
Table 1.
Sociodemographic characteristics and disease profile (n=523)
| Variable | f | % |
|---|---|---|
| Sex | ||
| Male | 215 | 41.1 |
| Female | 308 | 58.9 |
| Marital status | ||
| Not married | 121 | 23.1 |
| Married | 402 | 76.9 |
| Education level | ||
| Primary | 304 | 58.1 |
| Secondary or higher | 219 | 41.9 |
| Employment status | ||
| Employed | 142 | 27.2 |
| Unemployed | 381 | 72.8 |
| Income (LD)a | ||
| Low (600 and less) | 394 | 75.3 |
| Moderate-high (more than 600) | 129 | 24.7 |
| Diabetes medications | ||
| OHGb | 199 | 38.0 |
| Insulin with or without OHGb | 324 | 62.0 |
| Comorbidity | ||
| No | 215 | 41.1 |
| Yes | 308 | 58.9 |
LD, Libyan dinars (conversion rate at the time of the study: 1 LD = 1.32 USD).
OHG, oral hypoglycemic agents.
Table 2 displays the descriptive statistics of diabetes illness perceptions based on the identity and views sections of the IPQ-R. All eight illness perception domains displayed a satisfactory internal consistency, with the alpha coefficient ranging from 0.87 for the emotional representations subscale to 0.76 for the consequences perception subscale. Respondents showed low diabetes identity perception, indicating that they attributed few of the symptoms they experienced to their diabetes (mean=4.55, SD=3.72). They showed a high perception of diabetes timeline as a chronic illness (mean=22.08, SD=5.34) and a moderate perception of diabetes course as a cyclical (unstable) illness (mean=12.42, SD=4.80). Illness coherence was moderate (mean=16.12, SD=6.76). Respondents had a moderately high perception of the treatment controllability of their illness (mean=19.19, SD=4.48) and their personal control over diabetes (mean=18.93, SD=7.06), while demonstrating a moderate diabetes consequences perception (mean=16.24, SD=6.05) and emotional representations (mean=16.99, SD=7.76).
Table 2.
Diabetes illness perceptions based on the Revised Illness Perception Questionnaire (IPQ-R) scale
| IPQ-R | Number of items | Possible score range | Mean±SD | Cronbach's alpha (α) | |
|---|---|---|---|---|---|
| I | Identity | 16 | 0–16 | 4.55±3.72 | 0.841 |
| II | Timeline (acute/chronic) | 6 | 6–30 | 22.08±5.34 | 0.788 |
| III | Timeline (cyclical) | 4 | 4–20 | 12.42±4.80 | 0.772 |
| VI | Consequences | 6 | 6–30 | 16.24±6.05 | 0.763 |
| V | Personal control | 6 | 6–30 | 18.93±7.06 | 0.793 |
| VI | Treatment control | 5 | 5–25 | 19.19±4.48 | 0.780 |
| VII | Emotional | 6 | 6–30 | 16.99±7.76 | 0.877 |
| VIII | Coherence | 5 | 5–25 | 16.12±6.76 | 0.847 |
Table 3 shows the descriptive statistics on the perceptions of the cause of diabetes. The five most commonly indicated causes out of the 19 listed items as causes for diabetes were ‘Allah's will/fate’ (86.6%), ‘hereditary – it runs in my family’ (53.0%), ‘my emotional state’ (44.4%), ‘family problems or worries’ (40.0%), and ‘diet or eating habits’ (35.6%).
Table 3.
Diabetes cause perceptions (n=523)
| Causea | Strongly agree or agree f (%) |
|---|---|
| 1. Allah's will/fate | 86.6 |
| 2. Hereditary – it runs in my family | 53.0 |
| 3. My emotional state | 44.4 |
| 4. Family problems or worries | 40.0 |
| 5. Diet or eating habits | 35.6 |
| 6. My own behavior | 31.9 |
| 7. My mental attitude | 29.1 |
| 8. Chance or bad luck | 23.9 |
| 9. Poor medical care in my past | 23.5 |
| 10. Stress or worry | 21.8 |
| 11. My personality | 14.1 |
| 12. Overwork | 14.0 |
| 13. Accident or injury | 11.5 |
| 14. Aging | 1.3 |
| 15. A germ or virus | 0.8 |
| 16. Pollution in the environment | 0.6 |
| 17. Altered immunity | 0.4 |
| 18. Alcohol | 0.0 |
| 19. Smoking | 0.0 |
The cause section of the IPQ-R consists of disparate items.
Table 4 shows the descriptive statistics on diabetes medication adherence based on the MMAS-8. The scale showed a satisfactory internal consistency reliability (α=0.74). The mean medication adherence score was 6.06 (SD=1.89), and the prevalence of low medication adherence was 36.1%.
Table 4.
Medication adherence based on the MMAS-8©
| Medication adherence level | f | (%) | α |
|---|---|---|---|
| Total score (mean±SD) | 6.06 | ±1.89 | 0.72 |
| Medication adherence groups | |||
| Low (score < 6) | 189 | 36.1 | |
| Moderate and high (score ≥6) | 334 | 63.9 |
Use of the ©MMAS is protected by US copyright laws. Permission for use is required. A license agreement is available from: Donald E. Morisky, ScD, ScM, MSPH, Professor, Department of Community Health Sciences, UCLA School of Public Health, 650 Charles E. Young Drive South, Los Angeles, CA 90095-1772; dmorisky@ucla.edu.
Table 5 shows the results of bivariate analysis. Several sociodemographic variables and disease profile–related factors showed statistically significant associations with medication adherence. The frequency of low medication adherers was significantly higher among males than females (χ2=10.247, p=0.001). Respondents with secondary to high education level reported a significantly higher prevalence of low medication adherers than those with primary education (χ2=5.628, p=0.018). A significantly higher frequency of low adherers was also found among employed respondents compared to the unemployed (χ2=17.921, p<0.001) and among the moderate- to high-income group compared to the low income group (χ2=3.925, p=0.048). Respondents who had no comorbidity showed a significantly higher prevalence of low medication adherers compared to those who had comorbidity (χ2=11.466, p=0.001). In addition, there was a significant difference in the number of other long-term medications between low adherence and moderate-high adherence groups (z=−2.810, p=0.005). Regarding illness perceptions, a significant difference in the mean treatment control perception score (t=−2.366, p=0.018) was found between patients who reported low adherence to their diabetes medications (mean=18.58, SD=4.51) and those who reported moderate-high adherence (mean=19.54, SD=4.44).
Table 5.
Bivariate association between sociodemographic factors, disease profile, and illness perceptions with medication adherence
| Medication adherence | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Moderate-high adherence | Low adherence | |||||
|
|
|
|||||
| Variables | f (%) | f (%) | f (%) | f (%) | χ2 | P |
| (I) Sociodemographic | ||||||
| Age (mean±SD) | 54.84 | ±10.09 | 53.69 | ±9.91 | −1.261a | 0.208 |
| Sex | ||||||
| Male | 120 | (55.8) | 95 | (44.2) | ||
| Female | 214 | (69.5) | 94 | (30.5) | 10.247 | 0.001** |
| Marital status | ||||||
| Unmarried | 84 | (69.4) | 37 | (30.6) | ||
| Married | 250 | (62.2) | 152 | (37.8) | 2.108 | 0.147 |
| Education level | ||||||
| Primary | 207 | (68.1) | 97 | (31.9) | ||
| Secondary or higher | 127 | (58.0) | 92 | (42.0) | 5.628 | 0.018* |
| Employment status | ||||||
| Employed | 70 | (49.3) | 72 | (50.7) | ||
| Unemployed | 264 | (69.3) | 117 | (30.7) | 17.921 | 0.000*** |
| Income (Libyan dinar) | ||||||
| Low (600 or less) | 261 | (66.2) | 133 | (33.8) | ||
| Moderate-high (more than 600) | 73 | (56.6) | 56 | (43.4) | 3.925 | 0.048* |
| (II) Disease profile | ||||||
| Diabetes duration (years) | 9.72 | ±7.56 | 9.04 | ±6.83 | −1.058 | 0.291 |
| Diabetes medications | ||||||
| OHG | 126 | (63.3) | 73 | (36.7) | ||
| Insulin±OHG | 208 | (64.2) | 116 | (35.8) | 0.041 | 0.839 |
| Comorbidity | ||||||
| No | 119 | (55.3) | 96 | (44.7) | ||
| Yes | 215 | (69.8) | 93 | (30.2) | 11.466 | 0.001** |
| Number of other medications (mean±SD) | 0.98 | ±1.15 | 0.72 | ±1.04 | −2.810b | 0.005** |
| (III) Illness perceptions (mean±SD) | ||||||
| Identity | 4.33 | ±3.62 | 4.93 | ±3.86 | 1.772 | 0.077 |
| Timeline (acute/chronic) | 22.19 | ±5.39 | 21.90 | ±5.27 | −0.594 | 0.553 |
| Timeline (cyclic) | 12.19 | ±4.87 | 12.81 | ±4.65 | 1.428 | 0.154 |
| Consequences | 15.99 | ±6.04 | 16.69 | ±6.05 | 1.276 | 0.202 |
| Personal control | 19.05 | ±7.18 | 18.71 | ±6.86 | −0.527 | 0.599 |
| Treatment control | 19.54 | ±4.44 | 18.58 | ±4.51 | −2.366 | 0.018* |
| Emotional | 16.53 | ±7.70 | 17.81 | ±7.84 | 1.825 | 0.069 |
| Coherence | 16.11 | ±6.90 | 16.14 | ±6.52 | 0.052 | 0.959 |
p<0.05,
p<0.01,
p<0.001.
t statistic (independent t-test);
z statistic (Mann–Whitney U test).
Table 6 shows a two-step hierarchical binary logistic regression model. In the first step, all sociodemographic and disease profile–related factors that displayed associations with medication adherence at p≤0.25 in the bivariate analysis were entered into the model. All illness perceptions that displayed crude associations with medication adherence with p≤0.25 were entered in the second step. In the first step, the model showed a good fit of the included variables as indicated by the non-significant Hosmer Lemeshow test (p=0.160). Referring to the block omnibus test, the contribution of the model with these variables to low medication adherence variance compared to the model with the constant alone was significant (Δχ2 (df) =26.997(8), p=0.001). Based on the Nagelkerke R 2, this model contributed to 6.9% of the variance of low medication adherence. In the second step, illness perceptions were added to the model. The model showed a good fit of the included variables as indicated by the non-significant Hosmer–Lemeshow test (p=0.208). The addition of illness perceptions led to a significant improvement in the model's level of predictivity as indicated by a significant chi-square increment (Δχ2 (df) =19.867(5), p=0.001). Referring to the Nagelkerke R 2, the model's level of predictivity was raised to 11.7%. Thus, illness perceptions have a unique contribution to medication adherence above and beyond the control variables alone.
Table 6.
Hierarchical regression model of low medication adherence predictors
| Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Variables | B | Wald | Adjusted OR (95% CI) | B | Wald | Adjusted OR (95% CI) | |
| Step 1 | |||||||
| Sociodemographic and disease profile | |||||||
| Age | 0.000 | 0.001 | 1.00 (0.98–1.02) | 0.004 | 0.155 | 1.00 (0.98–1.02) | |
| Sex | |||||||
| Male (reference) | |||||||
| Female | −0.357 | 2.569 | 0.70 (0.45–1.08) | −0.522 | 4.522 | 0.59 (0.37–0.93)* | |
| Marital status | |||||||
| Unmarried (reference) | |||||||
| Married | 0.054 | 0.049 | 1.05 (0.65–1.69) | 0.087 | 0.123 | 1.09 (0.67–1.77) | |
| Education | |||||||
| Primary (reference) | |||||||
| Secondary or higher | −0.033 | 0.021 | 0.96 (0.62–1.50) | −0.082 | 0.128 | 0.92 (0.58–1.44) | |
| Employment | |||||||
| Employed (reference) | |||||||
| Unemployed | −0.646 | 5.079 | 0.52 (0.29–0.91)* | −0.781 | 6.983 | 0.45 (0.25–0.81)** | |
| Income | |||||||
| Low (reference) | |||||||
| Moderate-high | −0.083 | 0.098 | 0.92 (0.54–1.54) | 0.002 | 0.000 | 1.00 (0.59–1.70) | |
| Presence of comorbidity | |||||||
| No (reference) | |||||||
| Yes | −0.409 | 2.902 | 0.66 (0.41–1.6) | −0.419 | 2.858 | 0.65 (0.40–1.06) | |
| Number of other medications | −0.035 | 0.100 | 0.96 (0.77–1.19) | −0.081 | 0.515 | 0.92 (0.73–1.15) | |
| Constant | 0.327 | 0.230 | 1.38 | ||||
| Step 2 | Illness perceptions | ||||||
| Identity | 0.078 | 7.059 | 1.08 (1.02–1.14)** | ||||
| Timeline (cyclical) | 0.027 | 1.509 | 1.02 (0.98–1.07) | ||||
| Consequences | −0.001 | 0.001 | 0.99 (0.96–1.03) | ||||
| Treatment control | −0.044 | 4.074 | 0.95 (0.91–0.99)* | ||||
| Emotional | 0.010 | 0.420 | 1.01 (0.98–1.04) | ||||
| Constant | 0.298 | 0.110 | 1.34 | ||||
| Model fitness (Hosmer–Lemeshow) | 0.160 | 0.208 | |||||
| Omnibus test | |||||||
| ▵χ2 (df), p | 26.997 (8), 0.001** | 19.867 (5), 0.001** | |||||
| χ2 (df), p | 26.997 (8), 0.001** | 46.865 (13), 0.000*** | |||||
| Model predictivity (Nagelkerke R 2) | 0.069 | 0.117 | |||||
p<0.05,
p<0.01,
p<0.001;
▵χ2, chi-square difference across two subsequent models after adding illness perceptions.
The final model showed that two illness perceptions contributed significantly to low medication adherence; these were treatment control perception and illness identity perception. High treatment control perception contributed slightly yet significantly to medication adherence as a protective factor. The odds of having low adherence to medications decreased with the increase in treatment control perception (p=0.044, OR=0.95, 95% CI=0.91_0.99). On the other hand, high identity perception predicted lower medication adherence, as the odds of having low adherence to medications increased with the increase in identity perception (p=0.008, OR=1.08, 95% CI=1.02=1.14). Two of the control variables also displayed a significant contribution to low medication adherence; these were sex and employment status. Females were 1.5 times less likely than males to be low adherers (p=0.026, OR=0.59, 95% CI=0.37−0.93) and unemployed respondents were half as likely as employed respondents to be low adherers (p=0.008, OR=0.45, 95% CI=0.25−0.81).
Discussion
To the best of our knowledge, this study was the first to explore diabetes perceptions as guided by the CSM in the Libyan context. In our study, the number of female respondents exceeded that of males. Although this might indicate that females were more willing to participate in the study, it may also reflect the sex profile of diabetes in Libya. An early study of the epidemiological pattern of diabetes in Benghazi, Libya, found that the prevalence of T2DM was significantly higher among females than males (27). The predominance of females over males was also reported in a previous study among diabetics in the same center where our study was conducted (28) and in other Libyan diabetes settings (6, 7). The respondents reported a low identity perception, indicating that they attributed few of the symptoms they had experienced after the diagnosis to their diabetes. Regarding personal and treatment control perception domains, the respondents reported a moderately high perception of both their own ability to control their diabetes and the effectiveness of their diabetes treatment. Personal control perception is a close concept to self-efficacy, which is also about the confidence of the patients in their personal ability to control their illness. In line with our finding, a previous study among adult diabetics in Libya reported a moderate level of self-efficacy (7). The respondents perceived diabetes as a chronic illness, and moderately perceived the course of diabetes as unstable or cyclical. The respondents reported moderate coherence perception, which reflects a moderate personal understanding of diabetes. This finding shows that many of them perceived diabetes as an ambiguous illness that they did not understand well. Lack of professional information on diabetes, which in turn affects diabetes knowledge, could be one of the reasons. Several previous studies in the Libyan diabetes context showed a poor level of diabetes knowledge (6, 7). Therefore, empowering our patients’ diabetes knowledge through diabetes educational programs could help in optimizing their diabetes coherence or understanding perception. The respondents perceived that diabetes imposed moderate consequences on their life and health and they displayed moderate negative emotional responses to their illness.
The Islamic religious influences on the constitution of diabetes perceptions were reflected in the perception of the cause of diabetes, where ‘Allah's will/fate’ was the most frequently reported cause for diabetes. We also found that more respondents attributed their diabetes to psychosocial factors like their emotional state and family problems or worries than to their diet or eating habits. Studies in other diabetic populations reported different cause perception patterns. For instance, in a study among Nepali diabetics, pollution and immunity were frequently reported as the causes of diabetes, whereas emotional state was among the least perceived causes (22). Furthermore, a study in the United States reported heredity, diet and eating habits, and own behavior as the top three perceived causes for diabetes (14).
More than one-third of the respondents reported low adherence to their diabetes medications. This is considerable, and it should be taken seriously for its consequences on patients’ health and its ultimate impacts on the health-care system. Our study confirmed the findings of two previous studies in the Libyan diabetes context (6, 7). In a large diabetes care center in Benghazi, Libya, Roaeid and Kablan (6) reported that 27.1% of diabetics were not taking their medications regularly. In a more recent study in the same center in Benghazi, Elkharam et al. (7) assessed adherence to diabetes management advice using HbA1c as a distant adherence measure, and their findings also reflected the problem of low adherence levels. Both of these two studies used different adherence measures to that used in this current study. Compared to some Middle Eastern countries, the reported low medication adherence prevalence in this study is lower than that reported in Palestine among T2DM patients, using the same measure (42.7%) (29), but higher than that reported in Jordan (30).
In this study, we focused on eight illness perception domains in relation to medication adherence. Our findings added to the preexisting research evidence on the role of the CSM illness perceptions in guiding the coping behaviors in illness (10–14). Two illness perceptions were found to contribute significantly to medication adherence; these were identity and treatment control perceptions. The contribution of each of these two perceptions matched the theoretically anticipated directions. Identity perception was a predictor factor. The respondents who attributed many of the symptoms they had experienced to their diabetes were more likely to be low adherers to their medications. Meanwhile, treatment control perception was a protective factor, as those who reported higher perception of the effectiveness of their treatment were less likely to be low adherers. In line with our findings, it was found that the perceived treatment effectiveness in diabetes control contributed to the use of insulin (31). Although treatment control perception was identified among the predictors of medication adherence among Nepali diabetics, unlike in our study, higher perception of treatment effectiveness was associated with lower medication adherence (22).
The final model also identified two personal characteristics as predictors of low medication adherence; these were sex and employment status. Females were less likely than males to have low adherence to their diabetes medications. This was inconsistent with the findings of some studies where no relationship between sex and adherence level was reported (29, 32). Employed respondents were more likely to have low adherence than employed respondents. This could be related to some barriers that employed diabetics face, such as the lack of time or access to medications while away from home. Consistent with our findings, some other studies found that employment status influenced medication adherence in diabetes (22, 33).
Several limitations should be considered in the interpretation of the findings from this study, such as the cross-sectional design, which precludes making causal assumptions, and self-reporting of data, which is subject to recall bias as well as over- and under-reporting bias. Type 2 diabetic Libyans who are unable to read and write should be considered in further research that uses face-to-face interviews. As the study was conducted in a single diabetic center in Tripoli, the findings could not be generalized to all Libyans with T2DM. However, the findings could be generalized to the study population, which is Libyans with T2DM who attended the center during the study period.
Conclusion
This study provided insight into how Libyans with T2DM perceive their diabetes. The findings may inform local diabetic care providers about how their patients perceive their diabetes. Better understanding of the patients could positively influence patient–provider communication. The current study confirmed the suboptimal level of medication adherence reported by some previous studies in the Libyan diabetes context. It also showed how diabetes illness perceptions influence medication adherence. These findings could be used to develop medication adherence promotion approaches, as in the form of psychoeducational interventions. The findings from this study showed that males and employed patients were more likely to be low adherers; therefore, they might represent in-need groups for medication adherence promotion. The predictivity of the medication adherence model was low. Thus, further research is needed to identify what other factors could explain low medication adherence among Libyan diabetics. In addition, as our study was conducted at a single center, in the capital city of Libya, more research in the Libyan diabetes context is warranted to support the generalizability of the findings from our study to all Libyans with T2DM.
Acknowledgements
We acknowledge Universiti Kebangsaan Malaysia Medical Centre (UKMMC) for the grant given under project code FF-2013–298. Use of the ©MMAS is protected by US copyright laws. Permission for use is required. A license agreement is available from: Donald E. Morisky, ScD, ScM, MSPH, Professor, Department of Community Health Sciences, UCLA School of Public Health, 650 Charles E. Young Drive South, Los Angeles, CA 90095-1772; dmorisky@ucla.edu.
Conflict of interest and funding
The authors report no conflict of interest.
References
- 1.International Diabetes Federation (IDF) Diabetes atlas 6th edition 2013. Brussels, Belgium: International Diabetes Federation; 2013. [Google Scholar]
- 2.Aikens JE, Piette JD. Longitudinal association between medication adherence and glycaemic control in Type 2 diabetes. Diabet Med. 2013;30:338–44. doi: 10.1111/dme.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruelas V, Roybal GM, Lu Y, Goldman D, Peters A. Clinical and behavioral correlates of achieving and maintaining glycemic targets in an underserved population with type 2 diabetes. Diabetes Care. 2009;32:54–6. doi: 10.2337/dc08-1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27:1218–24. doi: 10.2337/diacare.27.5.1218. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization (WHO) Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003. [Google Scholar]
- 6.Roaeid RB, Kablan AA. Profile of diabetes health care at Benghazi Diabetes Centre, Libyan Arab Jamahiriya. East Mediterr Health J. 2007;13:168–76. [PubMed] [Google Scholar]
- 7.Elkharam WM, Khatri R, Wallymahmed AH, Gee I, Elhisadi T. Knowledge of and adherence to health advice among adults with diabetes in Libya. Ibnosina J Med BS. 2013;5:140–7. [Google Scholar]
- 8.Diefenbach MA, Leventhal H. The common-sense model of illness representation: Theoretical and practical considerations. J Soc Distress Homeless. 1996;5:11–38. [Google Scholar]
- 9.Leventhal H, Diefenbach M, Leventhal EA. Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cognit Ther Res. 1992;16:143–63. [Google Scholar]
- 10.Abubakari AR, Jones MC, Lauder W, Kirk A, Anderson J, Devendra D. Associations between knowledge, illness perceptions, self-management and metabolic control of type 2 diabetes among African and European-origin patients. J Nurs Healthc Chronic Illn. 2011;3:245–56. [Google Scholar]
- 11.Bean D, Cundy T, Petrie KJ. Ethnic differences in illness perceptions, self-efficacy and diabetes self-care. Psychol Health. 2007;22:787–811. [Google Scholar]
- 12.Broadbent E, Donkin L, Stroh JC. Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care. 2011;34:338–40. doi: 10.2337/dc10-1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Griva K, Myers LB, Newman S. Illness perceptions and self efficacy beliefs in adolescents and young adults with insulin dependent diabetes mellitus. Psychol Health. 2000;15:733–50. [Google Scholar]
- 14.Hart PL, Grindel CG. Illness representations, emotional distress, coping strategies, and coping efficacy as predictors of patient outcomes in type 2 diabetes. J Nurs Healthc Chronic Illn. 2010;2:225–40. [Google Scholar]
- 15.Kim Y, Pavlish C, Evangelista LS, Kopple JD, Phillips LR. Racial/ethnic differences in illness perceptions in minority patients undergoing maintenance hemodialysis. Nephrol Nurs J. 2012;39:39–48. [PMC free article] [PubMed] [Google Scholar]
- 16.Abubakari AR, Jones MC, Lauder W, Kirk A, Anderson J, Devendra D, et al. Ethnic differences and socio-demographic predictors of illness perceptions, self-management, and metabolic control of type 2 diabetes. Int J Gen Med. 2013;6:617–28. doi: 10.2147/IJGM.S46649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barnes L, Moss-Morris R, Kaufusi M. Illness beliefs and adherence in diabetes mellitus: A comparison between Tongan and European patients. N Z Med J. 2004;117:U743. [PubMed] [Google Scholar]
- 18.Fleiss JL. Statistical methods for rates and proportions. New York: Wiley; 1981. [Google Scholar]
- 19.Sasisekhar TVD, Shabana S, Bhargav SY. Gender: Does it have role has role in glycaemic control and diabetic distress in type 2 diabetes? IOSR-JDMS. 2013;4:48–51. [Google Scholar]
- 20.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychological problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitude, Wishes and Needs (DAWN) Study. Diabet Med. 2005;22:1379–85. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 21.Moss-Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, Buick D. The Revised Illness Perception Questionnaire (IPQ-R) Psychol Health. 2002;17:1–16. [Google Scholar]
- 22.Kart CS, Kinney JM, Subedi J, Basnyat KB, Vadakkan MF. Lay explanations and self-management of diabetes in Kathmandu, Nepal. J Aging Health. 2007;19:683–704. doi: 10.1177/0898264307301183. [DOI] [PubMed] [Google Scholar]
- 23.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10:348–54. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Krousel-Wood M, Islam T, Webber LS, Re R, Morisky DE, Muntner P. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15:59–66. [PMC free article] [PubMed] [Google Scholar]
- 25.Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: Final response. J Clin Epidemiol. 2011;64:262–3. doi: 10.1016/j.jclinepi.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ashur ST, Shamsuddin K, Shah SA, Bosseri S, Morisky DE. Reliability and known-group validity of the Arabic version of the 8-item Morisky Medication Adherence Scale among type 2 diabetes mellitus patients. East Mediterr Health J. 2015;21:722–728. doi: 10.26719/2015.21.10.722. [DOI] [PubMed] [Google Scholar]
- 27.Kadiki OA, Roaed RBM. Epidemiological and clinical patterns of diabetes mellitus in Benghazi, Libyan Arab Jamahiriya. East Mediterr Health J. 1999;5:6–13. [PubMed] [Google Scholar]
- 28.Elmiladi SA. Fasting and diabetic care during Ramadan in Libyan people with diabetes in Tripoli diabetes endocrine hospital. Libyan J Med Res. 2014;8:69–75. [Google Scholar]
- 29.Sweileh WM, Zyoud SH, Abu Nab'a RJ, Deleq MI, Enaia MI, Nassar SM, et al. Influence of patients’ disease knowledge and beliefs about medicines on medication adherence: Findings from a cross-sectional survey among patients with type 2 diabetes mellitus in Palestine. BMC Public Health. 2014;14:94. doi: 10.1186/1471-2458-14-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khattab M, Khader YS, Al-Khawaldeh A, Ajlouni K. Factors associated with poor glycemic control among patients with type 2 diabetes. J Diabetes Complications. 2010;24:84–9. doi: 10.1016/j.jdiacomp.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 31.Skinner TC, Hampson SE, Fife-Schaw C. Personality, personal model beliefs, and self-care in adolescents and young adults with Type 1 diabetes. Health Psychol. 2012;21:61–70. [PubMed] [Google Scholar]
- 32.Mahfouz EM, Awadalla HI. Compliance to diabetes self-management in rural El-Minia, Egypt. Cent Eur J Public Health. 2011;19:35–41. doi: 10.21101/cejph.a3573. [DOI] [PubMed] [Google Scholar]
- 33.Raum E, Krämer HU, Rüter G, Rothenbacher D, Rosemann T, Szecsenyi J, et al. Medication non-adherence and poor glycaemic control in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2012;97:377–84. doi: 10.1016/j.diabres.2012.05.026. [DOI] [PubMed] [Google Scholar]