Abstract
Objectives. We assessed the effectiveness of an intervention targeting home food and activity environments to reduce energy intake and increase physical activity among overweight and obese patients from 3 community health centers in rural Georgia.
Methods. We conducted a randomized controlled trial (n = 349) from 2011 to 2013, with follow-up at 6 and 12 months. Health coaches delivered the 16-week intervention by using tailored home environment profiles showing areas in need of improvement and positive aspects of the home environment, behavioral contracts for healthy actions, and mailed support materials.
Results. Participants were mostly African American women (84.8%), with a mean age of 50.2 years and a mean body mass index (weight in kilograms divided by the square of height in meters) of 38.3. Daily energy intake decreased more for the intervention than control group at 6 (–274 vs –69 kcal) and 12 months (–195 vs –76 kcal). We observed no change for either objective or self-reported physical activity. At 12 months, 82.6% of intervention participants had not gained weight compared with 71.4% of control participants.
Conclusions. The intervention was effective in changing home environments and reducing energy intake.
Adults gain about 1 pound per year, which over time can result in increased risk of diabetes and coronary heart disease, and with larger weight gain, increased risk of cancer.1–8 Preventing weight gain requires increased energy expenditure, decreased energy consumption, and ideally both. The home environment provides physical and social cues for eating, exercise, and sedentary activity, and can be structured to encourage both healthy and unhealthy behaviors. More than two thirds of calories for US adults come from home food sources and a significant amount of time is spent at home.9,10 Numerous aspects of the home environment affect dietary behavior, including availability and accessibility of healthy and unhealthy foods, use of nonhome food sources for family meals, and food preparation methods.11–24 Frequency of grocery shopping and family norms around eating with the TV on are also associated with dietary behavior.25–27 Likewise, numerous aspects of the home activity environment influence physical activity (PA) behaviors, including the availability of exercise equipment in the home and the number and location of TVs.16,28–34 Family social support can also influence dietary and PA behaviors, in both positive and negative directions.35–39 The home environment, while shaping behavior, is influenced, in turn, by the broader environment and may be an important mediator between community environments and behavior, especially for dietary practices.14,40
Despite the potential impact of changing the home environment, only a handful of studies have attempted to influence weight-related behaviors by doing so. The majority of these have focused on childhood obesity or attempted to change just 1 or 2 aspects of the home environment.7,41–44 Recent exceptions have targeted changes in both social and physical aspects of the food and PA home environments, with mixed results.45–47 Gorin et al. reported successful weight loss and environmental change at 6 months in an enhanced home environment intervention relative to a standard weight loss program, but no sustained weight loss difference at 18 months and no difference in PA at either time point.45 In a weight-gain-prevention study by French et al., participants were encouraged to make both household and individual-level (e.g., limit eating fast food) behavioral goals.46 The 1-year program led to increased PA, but no change in body mass index (BMI). Both sets of authors concluded that the home environment may be a promising target for intervention programs, but more research is needed to identify intervention strategies that support sustained change.
The purpose of the current study was to test the effectiveness of a weight-gain-prevention intervention delivered by health coaches and targeting the home environments of overweight and obese female patients from 3 community health centers. Health coaches help patients set goals, develop strategies for achieving goals, and anticipate and address challenges.48 Our health coaches can be viewed as a form of community health worker, in that they were local residents not formally trained as health professionals.49 We hypothesized that the Healthy Homes/Healthy Families intervention would reduce energy intake and increase PA at 6 and 12 months after baseline, as well as lead to improved home environments relative to usual care. No studies have rigorously tested the effectiveness of a moderate-intensity intervention delivered by health coaches and focusing on home environment change to influence weight-related behaviors of adults. Use of health coaches may provide a promising alternative to intensive and expensive weight-loss programs for resource-limited safety-net providers such as community health centers.
METHODS
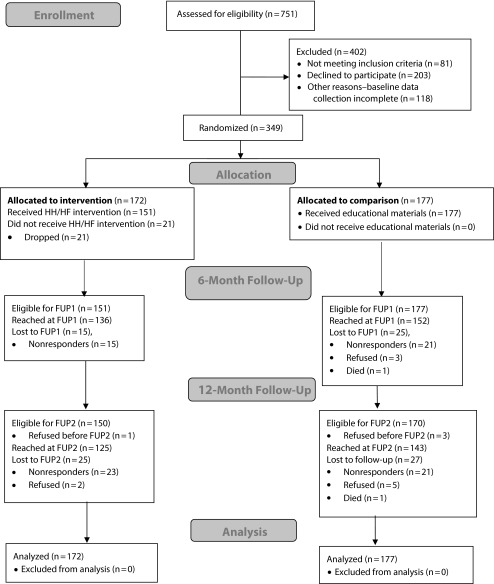
Providers from 3 community health centers (9 clinical sites) in southwest Georgia referred overweight and obese female patients to the study. Only women were recruited because of their potential role as gatekeepers of the home environment. Eligible participants were aged 35 to 65 years at baseline, lived with at least 1 other person, and lived no farther than 30 miles from the referring clinic, the latter to reduce intervention delivery costs. Providers were asked not to refer patients with conditions that could have an impact on their ability to be physically active. Pregnant women were also excluded from the study. From February 2011 to December 2012, a total of 948 women were referred (Figure 1). Of these, 751 were reached by telephone and screened for eligibility, with 81 not meeting inclusion criteria, 203 declining to participate, 118 not completing baseline data collection, and 349 completing baseline data collection and randomized. Verbal consent was obtained before data collection. Our statistician randomized participants into intervention and control in blocks of 4 by clinic, with the RAND function in Excel 2010 (Microsoft Corp, Redmond, WA).
FIGURE 1—
Consolidated Standards of Reporting Trials Statement Diagram Showing Study Flow: Healthy Homes/Healthy Families Study, Southwest Georgia, 2011–2013
Note. FUP = follow-up; HF = Healthy Families; HH = Healthy Homes.
Intervention and Control Conditions
We developed the intervention with a community-based participatory approach. In addition to input on study design, members of the Emory Prevention Research Center’s Community Advisory Board recommended use of a health coach model, decided on the number and types of contacts, and advised on intervention strategies. The intervention was based on social–cognitive theory in that we attempted to leverage the reciprocal nature of social support, physical environments, and individual behavior.50 It consisted of 3 home visits and 4 coaching calls over 16 weeks. Core elements, informed by social–cognitive theory, include a tailored home environment profile, goal setting, and behavioral contracting for 6 healthy actions. Healthy actions were supported by correlational data and experience from our pilot study, and refined by Community Advisory Board members.47 Selected healthy actions included always having a low-calorie beverage available instead of sugar-sweetened soda or sweet tea, cutting back on how often your family eats restaurant food, and creating a place for exercise in your home or yard and committing to using it at least once a week (Table A, available as a supplement to the online version of this article at http://www.ajph.org, shows the full set).
We used baseline data related to the healthy actions to generate a tailored home environment profile showing areas in need of improvement and positive aspects of the home environment. The profile had sections that matched the healthy actions, such as food and exercise equipment inventories. Coaches, hired and supervised by a community partner, used the home environment profile to guide participants in choosing healthy actions. The chosen healthy actions were recorded on a family contract that was signed by the participant and coach. On the basis of the healthy actions chosen, participants received supportive materials via mail (e.g., portion size plate). The intervention delivery schedule is available in Table B (available as a supplement to the online version of this article at http://www.ajph.org).
Control participants received 3 mailings of educational booklets at 6-week intervals. These mailings were government documents encouraging adoption of US dietary and PA guidelines.51–53
Health coaches who resided in southwest Georgia and had at least a high-school education and experience in social or customer service delivered the intervention. Training consisted of 2 days of formal training by university staff that covered the protocol for each contact point, how to use the intervention materials for goal setting, coaching tips, and documentation, followed by practice coaching sessions with extensive feedback. Quality control consisted of recording the first 3 families coached, followed by every 10th throughout intervention delivery. Supervisors gave detailed written individualized feedback, and held monthly group meetings to ensure high-quality delivery of the intervention.
Data Collection
Study participants were asked to complete 3 baseline and two 6- and 12-month follow-up telephone interviews each, and wear an accelerometer at baseline and at 6-month follow-up. Accelerometers were mailed to participants following the first interview with a stamped return envelope at baseline and 6 months. We did not collect accelerometer data at 12 months because of budget constraints. In addition, intervention participants were mailed a process evaluation survey at 6 months. We collected data from February 2011 to July 2013, and subsequently cleaned and analyzed the data from February 2014 to July 2014.
At 6 months, 82.5% completed data collection. At 12 months, 76.8% completed data collection. All data collection staff were blind to group assignment. With the exception of objectively measured PA and process measures, all data were obtained at baseline, 6 months, and 12 months via telephone interview.
Main Outcomes
At each time point, participants completed two 24-hour dietary recalls (1 weekday and 1 weekend day). Two recalls have substantially greater validity than 1 when compared with the doubly labeled water method.54 We calculated energy intake as the average daily kilocalories from the 2 recalls.54 We collected and analyzed data by using Nutrition Data System for Research software version 2010, (University of Minnesota Regents, Minneapolis, MN).55–57 Participants were mailed a copy of a Nutrition Data System for Research Foods Amount Booklet to assist with estimating portion sizes.
We measured PA as hours per week spent in moderate or vigorous PA by using the 7-day PA Recall (PAR).58 The PAR has moderate to high criterion validity (r = 0.54–0.73) for total PA using accelerometers for comparison.59,60 Participants also wore accelerometers for 7 days (ActiGraph 3X+, ActiGraph, Pensacola, FL) at baseline and 6 months after baseline. We used self-reported height and weight (in pounds) to calculate BMI (defined as weight in kilograms divided by the square of height in meters).
Secondary Outcomes
Home food environment.
Measures of the home food environment corresponded to healthy actions (Table A, available as a supplement to the online version of this article at http://www.ajph.org). To assess food inventories, participants were asked about the presence of 3 unhealthy drinks (e.g., soda) and 8 unhealthy foods and snacks (e.g., regular potato chips) in the home in the past week.12,13 Food placement was assessed by asking if participants kept fruits, vegetables, and high-calorie snack foods where they were easy to see and easy to reach.12 Participants were also asked how often they purchased fruit and vegetables when they went grocery shopping in the past month. We assessed TV watching while eating with 3 items asking how often their family ate evening meals, other meals, and snacks in front of the TV.61
We assessed food preparation through 15 items that asked how often, in the past month, participants served healthier food options or prepared foods by using healthy cooking methods.61,62 Meal serving practices focused on 3 strategies with potential to decrease portion size (e.g., use smaller plates). We assessed nonhome food sources by asking the number of days in the past week that family meals were purchased from a fast-food restaurant, full-service restaurant, take out, or delivery.63 Participants also reported how often they told others in their household their weight in the past month. Family support for healthy eating was adapted from Sallis et al. (Cronbach α = 0.70).35
Home activity environment.
We assessed screen time rules by asking about rules that limited time spent watching TV, using a computer or laptop, playing video games, and using any other hand-held device to play games, watch movies or videos, or use the Internet. In addition, we adapted an inventory of 14 items to assess availability and accessibility of exercise equipment in the home.12,32,64
We measured use of community facilities and spaces with 9 items that assessed frequency of using facilities and spaces for exercise in their neighborhood (e.g., public sports fields). Six items assessed family time spent in PA (e.g., playing a sport) in the past month. We also developed a set of items to assess ways in which participants might incorporate PA into their daily routines (e.g., parked far away). Participants were asked about 5 types of exercise space in their home or yards. Lastly, we measured family support for PA by using 9 items (Cronbach α = 0.79).35
Intervention participants were mailed a survey that assessed satisfaction with the coach, the home visits, telephone calls, and the support materials. In addition, coaches documented each contact with the participants in a coaching log, indicating actions selected, corresponding goals, successes, and barriers.
We also assessed education, annual household income, household composition, race/ethnicity, age, general health, and neighborhood type.
Statistical Analysis
We assessed outcome variables for normality and transformed them if assumptions were not met. Assessment of missingness found no significant differences between those reached for follow-up and those who were not. We assessed statistical significance of change between baseline and each follow-up point with appropriate statistical tests (e.g., independent t test, Wilcoxon–Mann–Whitney test). We used growth modeling as the intent-to-treat analysis as it allows for modeling of all available data without the need for imputation.65 The analysis produces results that can be interpreted as if all participants had provided follow-up data under the assumption of data missing at random.66 For each outcome variable, the models included time (calculated as time elapsed between the measurement time point and baseline date) and an interaction effect between time and group assignment. Because intraclass correlations were very low for our primary outcomes (< 1% for moderate to vigorous physical activity and caloric intake), combined with the fact that our intervention was delivered at the household level, we did not adjust for clustering within clinics. We used PROC MIXED for continuous outcome variables and PROC GLIMMIX for binary variables in SAS version 9.4 (SAS Institute Inc, Cary, NC). We excluded several participants who reported unusually high (beyond 3 SDs) weight gain or weight loss from the growth model with weight as the outcome.
The study was powered to detect a difference of 31.5 minutes of moderate to vigorous activity per week between intervention and control, which is equivalent to a medium effect size of 0.35. A sample size of 258 would allow us to detect a difference of this magnitude with power of 0.80 and α of 0.05.
RESULTS
The majority of participants were African American women (84.8%), with an average age of 50.2 years (SD = 8.1) and a mean BMI of 38.3 (SD = 8.4; Table 1). Most were low-income with 68.7% reporting a yearly household income of $25 000 or less. Almost half reported fair or poor general health. About 45% were employed and almost half (49%) were living in a rural area. Most lived with 1 additional adult and half had at least 1 child younger than 18 years in the home.
TABLE 1—
Baseline Characteristics of Participants in the Healthy Homes/Healthy Families Study, Southwest Georgia, 2011–2013
| Characteristic | Intervention (n = 172), Mean ±SD or No. (%) | Control (n = 177), Mean ±SD or No. (%) | P |
| Age, y | 50.5 ±8.0 | 49.8 ±8.2 | .41 |
| Age group, y | |||
| 35–44 | 45 (26.2) | 57 (32.4) | |
| 45–54 | 71 (41.3) | 59 (33.5) | |
| 55–65 | 56 (32.6) | 60 (34.1) | .27 |
| BMI, kg/m2 | 37.6 ±8.5 | 39.0 ±8.4 | .11 |
| Race | |||
| White | 25 (14.6) | 26 (14.7) | |
| African American | 146 (85.4) | 149 (84.2) | |
| Other | 0 (0.0) | 2 (1.1) | .38 |
| Highest education | |||
| ≤ some high school | 37 (21.5) | 34 (19.2) | |
| High school or GED | 65 (38.0) | 62 (35.0) | |
| Some college or technical school | 52 (30.4) | 58 (32.8) | |
| ≥ college graduate | 17 (9.9) | 23 (13.0) | .49 |
| Employment status | |||
| Full time | 61 (35.5) | 58 (32.8) | |
| Part time | 16 (9.3) | 19 (10.7) | |
| Retired | 9 (5.2) | 15 (8.5) | |
| Not working, homemaker, student, or on disability | 86 (50.0) | 85 (48.0) | .62 |
| Household income, $ | |||
| ≤ 10 000 | 56 (33.1) | 58 (33.5) | |
| 10 001–25 000 | 64 (37.9) | 57 (33.0) | |
| 25 001–50 000 | 37 (21.9) | 41 (23.7) | |
| ≥ 50 001 | 12 (7.1) | 17 (9.8) | .69 |
| Marital status | |||
| Married or living with partner | 82 (47.7) | 79 (44.6) | |
| Widowed, separated, or divorced | 58 (33.7) | 48 (27.1) | |
| Not married | 32 (18.6) | 50 (28.3) | .19 |
| Neighborhood | |||
| In town | 86 (50.0) | 92 (52.0) | |
| In rural area | 86 (50.0) | 85 (48.0) | .71 |
| Other adults in the home | |||
| None | 16 (9.3) | 21 (11.9) | |
| 1 | 88 (51.2) | 97 (55.1) | |
| 2 | 49 (28.5) | 35 (19.9) | |
| ≥ 3 | 19 (11.1) | 23 (13.1) | .43 |
| Children aged < 18 y in the home | |||
| None | 82 (47.7) | 92 (52.3) | |
| 1 | 44 (25.6) | 46 (26.1) | |
| 2 | 33 (19.2) | 19 (10.8) | .4 |
| ≥ 3 | 13 (7.6) | 19 (10.8) | |
| General health | |||
| Poor | 13 (7.6) | 20 (11.3) | |
| Fair | 72 (41.9) | 58 (32.8) | |
| Good | 64 (37.2) | 80 (45.2) | |
| Very good | 20 (11.6) | 15 (8.5) | |
| Excellent | 3 (1.7) | 4 (2.3) | .23 |
Note. BMI = body mass index, defined as weight in kilograms divided by the square of height in meters; GED = general equivalency diploma. P values are from independent t test for continuous variables and χ2 test for categorical variables.
Most (74.4%) intervention participants received the entire intervention (Table B, available as a supplement to the online version of this article at http://www.ajph.org). The others either dropped out (n = 21) or exceeded the 6 months allocated for intervention delivery. Only 12.2% of participants had fewer than 4 contacts with a coach. Using a 4-point scale (with 1 = strongly disagree and 4 = strongly agree), intervention participants (n = 121) found the coach easy to understand (mean = 3.72), informative (mean = 3.71), and motivating for themselves (mean = 3.64) and even others in their household (mean = 3.35). They found both the home visits and the phone calls similarly interesting (mean = 3.66 and 3.55, respectively) and relevant (mean = 3.59 and 3.61, respectively). In addition, they reported the support materials to be helpful (mean = 3.56) and motivating (mean = 3.53).
Primary Behavioral Outcomes
Daily energy consumption decreased significantly more for the intervention than control group at 6 months (–274 vs –69 kcal/day) and 12 months (–195 vs –76 kcal/day), and was significantly different in longitudinal intent-to-treat analyses based on growth models (P = .03; Table 2).
TABLE 2—
Baseline Values and Changes Over Time in Weight, Daily Energy Intake, and Home Food Environment Outcomes: Healthy Homes/Healthy Families Study, Southwest Georgia, 2011–2013
| Change Baseline to FUP1 (6 Months; n = 288) |
Change Baseline to FUP2 (12 Months; n = 268) |
|||||
| Variables | Baseline (n = 349), Mean ±SD or No. (%) | Mean ±SD or No. (%) | P | Mean ±SD or No. (%) | P | Intent to Treat, P |
| Primary outcomes | ||||||
| Energy intake, kcal/d | ||||||
| Intervention | 1466 ±644 | –274 ±583 | –195 ±535 | |||
| Control | 1470 ±674 | −69 ±594 | .003 | −76 ±584 | .09 | .03 |
| Weight, poundsa | ||||||
| Intervention | 219.6 ±51.0 | −9.1 ±16.5 | −10.7 ±17.4 | |||
| Control | 232.1 ±49.7 | −5.0 ±13.7 | .03 | −7.1 ±14.6 | .08 | .03 |
| Secondary outcomes | ||||||
| Unhealthy drinks in the home (of 3) | ||||||
| Intervention | 1.78 ±0.97 | −0.65 ±1.04 | −0.48 ±1.00 | |||
| Control | 1.89 ±0.93 | 0.11 ±0.99 | < .001 | 0.21 ±1.11 | .01 | < .001 |
| Unhealthy snacks in the home (of 8) | ||||||
| Intervention | 4.44 ±1.74 | −1.39 ±2.26 | −0.92 ±2.18 | |||
| Control | 4.68 ±1.78 | −0.28 ±1.67 | < .001 | −0.08 ±1.76 | < .001 | < .001 |
| Buying fruits/wk | ||||||
| Intervention | 1.07 ±1.27 | 0.18 ±1.62 | 0.16 ±1.80 | |||
| Control | 0.93 ±0.99 | 0.20 ±0.98 | .07 | 0.22 ±1.21 | .22 | .04 |
| Buying vegetables/wk | ||||||
| Intervention | 1.02 ±1.23 | 0.04 ±1.48 | 0.13 ±1.68 | |||
| Control | 0.85 ±0.78 | 0.20 ±0.87 | .19 | 0.13 ±1.03 | .03 | .004 |
| Family eating and TVb | ||||||
| Intervention | 2.73 ±0.92 | −0.83 ±1.04 | −0.83 ±1.09 | |||
| Control | 2.65 ±1.05 | −0.17 ±0.93 | < .001 | −0.20 ±0.95 | < .001 | < .001 |
| Healthy food preparationb | ||||||
| Intervention | 2.27 ±0.47 | 0.24 ±0.46 | 0.22 ±0.53 | |||
| Control | 2.11 ±0.46 | 0.19 ±0.47 | .005 | 0.14 ±0.46 | .02 | < .001 |
| Healthy food serving practicesb | ||||||
| Intervention | 2.51 ±0.66 | 0.38 ±0.85 | 0.24 ±0.82 | |||
| Control | 2.39 ±0.60 | 0.09 ±0.75 | < .001 | 0.11 ±0.78 | .06 | < .001 |
| Family meals from nonhome sources/wk | ||||||
| Intervention | 2.46 ±2.84 | −0.82 ±2.74 | −0.87 ±3.09 | |||
| Control | 2.78 ±3.32 | −0.67 ±3.27 | .01 | −0.54 ±3.46 | .13 | .04 |
| Family support for healthy eatingb | ||||||
| Intervention | 2.58 ±0.57 | 0.22 ±0.55 | 0.08 ±0.61 | |||
| Control | 2.51 ±0.54 | 0.10 ±0.56 | .01 | 0.18 ±0.59 | .71 | .38 |
| Telling others your weight (yes) | ||||||
| Intervention | 68 (39.5) | 19 (14.96) | 22 (18.5) | |||
| Control | 66 (37.3) | 18 (12.16) | .51 | 19 (13.6) | .48 | .11 |
Note. FUP1 or 2 = follow-up 1 or 2. P values for cross-sectional analyses and change between 2 time points result from independent t test and regression analyses; P values for the intent-to-treat analysis are from unadjusted growth models (which included all participants) testing for intervention effect and refer to the significance of the interaction term of group and time.
Significant difference at baseline (P = .04).
1 = never or rarely; 2 = occasionally; 3 = often; 4 = very often.
We did not find any meaningful change in self-reported moderate to vigorous PA as measured with the 7-day PAR (Table 3). In addition, there was no significant change in PA measured by accelerometers at 6 months compared with baseline (not shown).
TABLE 3—
Baseline Values and Changes Over Time in Moderate to Vigorous Physical Activity and Home Activity Environment Outcomes: Healthy Homes/Healthy Families Study, Southwest Georgia, 2011–2013
| Change Baseline to FUP1 (6 Months; n = 288) |
Change Baseline to FUP2 (12 Months; n = 268) |
|||||
| Variables | Baseline (n = 349), Mean ±SD | Mean ±SD | P | Mean ±SD | P | Intent to Treat, P |
| Primary outcomes | ||||||
| MVPA, h/wk | ||||||
| Intervention | 3.9 ±5.9 | 0.1 ±6.3 | .46 | −1.3 ±4.5 | .26 | .38 |
| Control | 3.5 ±5.8 | −0.8 ±6.3 | −0.9 ±4.2 | |||
| Secondary outcomes | ||||||
| Screen rules (of 4) | ||||||
| Intervention | 1.74 ±1.60 | 0.14 ±1.63 | 0.26 ±1.78 | |||
| Control | 1.51 ±1.67 | 0.16 ±1.46 | .57 | 0.18 ±1.53 | .07 | .053 |
| Visible physical activity equipment (of 12) | ||||||
| Intervention | 2.79 ±1.78 | 1.23 ±1.71 | 1.38 ±2.04 | |||
| Control | 2.95 ±1.87 | 5.77 ±1.61 | .006 | 0.72 ±1.82 | .005 | .01 |
| Use of community facilities or space, frequency/wk | ||||||
| Intervention | 1.56 ±2.49 | 0.54 ±3.16 | 0.96 ±3.48 | |||
| Control | 1.70 ±3.05 | 0.39 ±3.17 | .49 | 0.49 ±4.32 | .21 | .12 |
| Family physical activity, frequency/wk | ||||||
| Intervention | 2.19 ±2.98 | 0.66 ±4.05 | 1.17 ±4.61 | |||
| Control | 1.71 ±3.06 | 0.61 ±2.99 | .46 | 0.83 ±4.24 | .07 | .01 |
| Incorporate physical activity into daily life, frequency/wk | ||||||
| Intervention | 4.24 ±5.67 | 3.12 ±10.84 | 1.64 ±11.11 | |||
| Control | 4.00 ±6.34 | 0.16 ±6.05 | .45 | 0.99 ±8.68 | .08 | .03 |
| Exercise space (of 5) | ||||||
| Intervention | 1.38 ±1.20 | 0.49 ±1.35 | 0.54 ±1.25 | |||
| Control | 1.44 ±1.16 | 1.12 ±1.24 | .03 | 0.06 ±1.29 | .002 | .003 |
| Family support for physical activitya | ||||||
| Intervention | 2.14 ±0.56 | 0.20 ±0.66 | 0.08 ±0.61 | |||
| Control | 2.07 ±0.49 | 0.10 ±0.57 | .055 | 0.10 ±0.59 | .36 | .17 |
Note. FUP1 or 2 = follow-up 1 or 2; MVPA = moderate to vigorous physical activity. P values for cross-sectional analyses and change between 2 time points result from independent t test and regression analyses; P values for the intention-to-treat analysis are from unadjusted growth models (which include all participants) testing for intervention effect and refer to the significance of the interaction term of group and time. P values for MVPA are based on log-transformed values.
1 = never or rarely; 2 = occasionally; 3 = often; 4 = very often.
Secondary Outcomes
Self-reported weight.
Intervention participants had significantly higher self-reported weight loss at 6 months (mean = −9.1 pounds; SD = 16.5 pounds) than control participants (mean = −5.0 pounds; SD = 13.7 pounds; P = .03; Table 3). Differences were slightly less at 12 months, but longitudinal intent-to-treat analyses showed significant differences in weight loss over time (P = .03). In addition, at 12 months after baseline, 82.6% of intervention participants had not gained weight compared with 71.4% of control participants (P = .03).
Home food environment.
Intervention participants made many changes to their home food environments relative to control participants (Table 2). They reduced the number of unhealthy drinks and snacks in the home, increased buying frequency for fruits and vegetables, and reduced the frequency of watching TV while eating meals and snacks. They also improved how they prepared and served meals in the home and reported eating family meals from nonhome sources less frequently. Telling others in the household their weight and family support for healthy eating did not improve in the intervention group relative to the control group.
Home activity environment.
Having exercise equipment in a visible location changed significantly more in the intervention group relative to the control group (Table 3). Intervention participants also incorporated PA more often into their daily lives than those in the control group, and created more exercise space in their homes and yards. Differences between groups in screen rules, use of community facilities and spaces, and family social support for PA were not significant over time.
DISCUSSION
We tested a moderate-intensity, coach-delivered, weight-gain-prevention intervention with an explicit focus on the home environment of adults. Our primary finding was a significant and sustained difference in daily energy intake. In addition, self-reported weight loss was greater among intervention relative to control participants and percentage of participants with no weight gain was higher among intervention participants at 12 months. A recent review of weight-gain-prevention interventions used a difference of 0.5 kilograms (1.1 pounds) to designate meaningful differences by group at 12 months.43 These results, in combination with the large number of home food environment changes, suggest that the nutrition component of the Healthy Homes/Healthy Families intervention was effective.
We observed changes in almost all of the measures that corresponded to the food-related healthy actions, including household food inventories, frequency of purchasing fruits and vegetables, patterns of family eating with the TV on, food preparation, and family meals from nonhome sources. These results suggest that women can be effective change agents in establishing healthier home food environments. Other studies have similarly documented changes in the home food environment, but have not sustained daily caloric differences between groups as documented in our study.45
Despite the encouraging changes in nutrition-related outcomes, our intervention was not effective in changing PA levels. One reason may be the surprisingly low levels of PA at baseline among our primarily obese participants. Although self-reported levels of PA were relatively high, none of the participants met recommended guidelines for PA when we used objective measures and the average level of moderate to vigorous activity at baseline was less than 1 minute per day.67 Poor health status, combined with morbid obesity, was a significant barrier to moderate and vigorous activity as documented in our coaching logs and supported by almost half of our participants indicating poor or fair general health. It is also possible that targeting the home environment is not sufficiently powerful to induce increased PA. Gorin et al. gave participants an exercise machine, asked them to restrict TV viewing, provided cues to exercise (e.g., videos), and observed no change in PA.45 In addition, participants in our study were very poor and half lived in rural areas outside town, thus suggesting limited access to safe, walkable neighborhoods or affordable recreational facilities.
This study has several limitations. With the exception of the accelerometers, all measures were self-reported, with acceptable but modest validity reported in the literature.12,68–70 The 24-hour dietary recall is considered one of the better ways to measure dietary intake54; however, of some concern was the suspected underreporting of daily food intake. Our population of low-income, obese, and African American women is one of the most challenging for accurate dietary intake.71,72 We also collected self-reported height and weight. Fortunately, because of randomization, the potential underreporting of food intake and weight was distributed across groups and does not invalidate our outcomes. It is possible, however, that intervention participants reported more favorable home environment outcomes. A second substantive limitation is related to generalizability of the findings. Because of the extensive baseline data collection (i.e., 3 interviews and wearing an accelerometer), a significant number of those initially enrolled in the study did not complete baseline data collection and were not randomized.
The US Preventive Services Task Force recommends screening all adults for obesity and encourages clinicians to refer obese patients to intensive, multicomponent behavioral interventions.73,74 This recommendation, however, is difficult to implement in safety-net clinics such as community health centers in resource-poor communities.75 Alternative approaches are needed, both in terms of intervention targets and intervention delivery methods. Our intervention integrates public health principles that focus on environmental influences with current health reform attempts to transform the “doctor’s office” into the patient-centered medical home.76–78 Instead of traditional moderate-intensity behavioral counseling, our intervention trains local residents to function as health coaches who help the patient construct a healthier home environment, thus linking the medical home with the patient’s home. This model capitalizes on the ability of residents who essentially work as community health workers to create a bridge between the community and formal health services.49
This approach proved successful in changing one of the most challenging behaviors—excessive food consumption—in a very-high-priority population for obesity prevention. Future research could complement our intervention with mobile messaging and home monitoring of PA, weight, blood pressure, and blood sugars. Future research could also focus on the long-term sustainability of changes to the home food environment and whether booster sessions would be beneficial. Our study offers one model for intervening in a potentially important setting for obesity prevention. Combining effective home-focused interventions with strategies that target individual-level factors and neighborhoods is an important next step in a more comprehensive approach to tackling the obesity epidemic.
ACKNOWLEDGMENTS
This publication was supported by Cooperative Agreement 5U48DP001909 from the Centers for Disease Control and Prevention.
The authors wish to thank members of the Emory Prevention Research Center Community Advisory Board for their guidance in the design and implementation of this research; the Cancer Coalition of South Georgia, including Denise Ballard, for helping to coordinate recruitment and intervention delivery; the 3 community health centers that referred their patients to this study; and the many graduate research assistants and research interviewers who helped with data collection. We also wish to thank Laura Whitaker and Alexandra Gemma for their assistance in data cleaning and study coordination. Finally, we wish to thank our health coaches and study participants for their valuable contributions to this research.
Note. The findings and conclusions in this journal article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
HUMAN PARTICIPANT PROTECTION
This protocol was approved by the Emory University institutional review board.
REFERENCES
- 1.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–2404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.He XZ, Baker DW. Changes in weight among a nationally representative cohort of adults aged 51 to 61, 1992 to 2000. Am J Prev Med. 2004;27(1):8–15. doi: 10.1016/j.amepre.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 3.Colditz GA, Willett WC, Stampfer MJ, London SJ, Segal MR, Speizer FE. Patterns of weight change and their relation to diet in a cohort of healthy women. Am J Clin Nutr. 1990;51(6):1100–1105. doi: 10.1093/ajcn/51.6.1100. [DOI] [PubMed] [Google Scholar]
- 4.Willett WC, Manson JE, Stampfer MJ et al. Weight, weight change, and coronary heart disease in women. Risk within the “normal” weight range. JAMA. 1995;273(6):461–465. doi: 10.1001/jama.1995.03520300035033. [DOI] [PubMed] [Google Scholar]
- 5.Resnick HE, Valsania P, Halter JB, Lin X. Relation of weight gain and weight loss on subsequent diabetes risk in overweight adults. J Epidemiol Community Health. 2000;54(8):596–602. doi: 10.1136/jech.54.8.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Cancer Research Fund, American Institute for Cancer Research. Food, Nutrition, Physical Activity and the Prevention of Cancer: A Global Perspective. Washington, DC: American Institute for Cancer Research; 2007. [Google Scholar]
- 7.Lombard CB, Deeks AA, Teede HJ. A systematic review of interventions aimed at the prevention of weight gain in adults. Public Health Nutr. 2009;12(11):2236–2246. doi: 10.1017/S1368980009990577. [DOI] [PubMed] [Google Scholar]
- 8.Hebden L, Chey T, Allman-Farinelli M. Lifestyle intervention for preventing weight gain in young adults: a systematic review and meta-analysis of RCTs. Obes Rev. 2012;13(8):692–710. doi: 10.1111/j.1467-789X.2012.00990.x. [DOI] [PubMed] [Google Scholar]
- 9.Lin B-H, Guthrie J. Nutritional Quality of Food Prepared at Home and Away From Home, 1977–2008. Washington, DC: US Department of Agriculture, Economic Research Service; 2012. [Google Scholar]
- 10.Bureau of Labor Statistics, US Department of Labor. American Time Use Survey—2014 Results. Available at: http://www.bls.gov/news.release/pdf/atus.pdf. Accessed September 12, 2015.
- 11.Rosenkranz RR, Dzewaltowski DA. Model of the home food environment pertaining to childhood obesity. Nutr Rev. 2008;66(3):123–140. doi: 10.1111/j.1753-4887.2008.00017.x. [DOI] [PubMed] [Google Scholar]
- 12.Gattshall ML, Shoup JA, Marshall JA, Crane LA, Estabrooks PA. Validation of a survey instrument to assess home environments for physical activity and healthy eating in overweight children. Int J Behav Nutr Phys Act. 2008;5:3. doi: 10.1186/1479-5868-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patterson RE, Kristal AR, Shannon J, Hunt JR, White E. Using a brief household food inventory as an environmental indicator of individual dietary practices. Am J Public Health. 1997;87(2):272–275. doi: 10.2105/ajph.87.2.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hermstad AK, Swan DW, Kegler MC, Barnette JK, Glanz K. Individual and environmental correlates of dietary fat intake in rural communities: a structural equation model analysis. Soc Sci Med. 2010;71(1):93–101. doi: 10.1016/j.socscimed.2010.03.028. [DOI] [PubMed] [Google Scholar]
- 15.Larson N, Laska MN, Story M, Neumark-Sztainer D. Predictors of fruit and vegetable intake in young adulthood. J Acad Nutr Diet. 2012;112(8):1216–1222. doi: 10.1016/j.jand.2012.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorin AA, Phelan S, Raynor H, Wing RR. Home food and exercise environments of normal-weight and overweight adults. Am J Health Behav. 2011;35(5):618–626. doi: 10.5993/ajhb.35.5.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fulkerson JA, Farbakhsh K, Lytle L et al. Away-from-home family dinner sources and associations with weight status, body composition, and related biomarkers of chronic disease among adolescents and their parents. J Am Diet Assoc. 2011;111(12):1892–1897. doi: 10.1016/j.jada.2011.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kramer RF, Coutinho AJ, Vaeth E, Christiansen K, Suratkar S, Gittelsohn J. Healthier home food preparation methods and youth and caregiver psychosocial factors are associated with lower BMI in African American youth. J Nutr. 2012;142(5):948–954. doi: 10.3945/jn.111.156380. [DOI] [PubMed] [Google Scholar]
- 19.Champagne CM, Bogle ML, McGee BB et al. Dietary intake in the lower Mississippi Delta region: results from the Foods of our Delta Study. J Am Diet Assoc. 2004;104(2):199–207. doi: 10.1016/j.jada.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 20.Crawford D, Ball K, Mishra G, Salmon J, Timperio A. Which food-related behaviours are associated with healthier intakes of fruits and vegetables among women? Public Health Nutr. 2007;10(3):256–265. doi: 10.1017/S1368980007246798. [DOI] [PubMed] [Google Scholar]
- 21.Neumark-Sztainer D, Hannan PJ, Story M, Croll J, Perry C. Family meal patterns: associations with sociodemographic characteristics and improved dietary intake among adolescents. J Am Diet Assoc. 2003;103(3):317–322. doi: 10.1053/jada.2003.50048. [DOI] [PubMed] [Google Scholar]
- 22.Neumark-Sztainer D. Eating among teens: do family mealtimes make a difference for adolescents’ nutrition? New Dir Child Adolesc Dev. 2006;(111):91–105. doi: 10.1002/cd.157. [DOI] [PubMed] [Google Scholar]
- 23.Rollins BY, Belue RZ, Francis LA. The beneficial effect of family meals on obesity differs by race, sex, and household education: the National Survey of Children’s Health, 2003–2004. J Am Diet Assoc. 2010;110(9):1335–1339. doi: 10.1016/j.jada.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chu YL, Addo OY, Perry CD, Sudo N, Reicks M. Time spent in home meal preparation affects energy and food group intakes among midlife women. Appetite. 2012;58(2):438–443. doi: 10.1016/j.appet.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Bhargava A, Jolliffe D, Howard LL. Socio-economic, behavioural and environmental factors predicted body weights and household food insecurity scores in the Early Childhood Longitudinal Study–Kindergarten. Br J Nutr. 2008;100(2):438–444. doi: 10.1017/S0007114508894366. [DOI] [PubMed] [Google Scholar]
- 26.Blass EM, Anderson DR, Kirkorian HL, Pempek TA, Price I, Koleini MF. On the road to obesity: television viewing increases intake of high-density foods. Physiol Behav. 2006;88(4-5):597–604. doi: 10.1016/j.physbeh.2006.05.035. [DOI] [PubMed] [Google Scholar]
- 27.Huffman FG, Vaccaro JA, Exebio JC, Zarini GG, Katz T, Dixon Z. Television watching, diet quality, and physical activity and diabetes among three ethnicities in the United States. J Environ Public Health. 2012;2012 doi: 10.1155/2012/191465. 191465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297–322. doi: 10.1146/annurev.publhealth.27.021405.102100. [DOI] [PubMed] [Google Scholar]
- 29.Jakicic JM, Wing RR, Butler BA, Jeffery RW. The relationship between presence of exercise equipment in the home and physical activity level. Am J Health Promot. 1997;11(5):363–365. doi: 10.4278/0890-1171-11.5.363. [DOI] [PubMed] [Google Scholar]
- 30.Kerr J, Norman GJ, Sallis JF, Patrick K. Exercise aids, neighborhood safety, and physical activity in adolescents and parents. Med Sci Sports Exerc. 2008;40(7):1244–1248. doi: 10.1249/MSS.0b013e31816b8797. [DOI] [PubMed] [Google Scholar]
- 31.Reed JA, Phillips DA. Relationships between physical activity and the proximity of exercise facilities and home exercise equipment used by undergraduate university students. J Am Coll Health. 2005;53(6):285–290. doi: 10.3200/JACH.53.6.285-290. [DOI] [PubMed] [Google Scholar]
- 32.Sallis JF, Johnson MF, Calfas KJ, Caparosa S, Nichols JF. Assessing perceived physical environmental variables that may influence physical activity. Res Q Exerc Sport. 1997;68(4):345–351. doi: 10.1080/02701367.1997.10608015. [DOI] [PubMed] [Google Scholar]
- 33.Van Dyck D, Cardon G, Deforche B et al. Environmental and psychosocial correlates of accelerometer-assessed and self-reported physical activity in Belgian adults. Int J Behav Med. 2011;18(3):235–245. doi: 10.1007/s12529-010-9127-4. [DOI] [PubMed] [Google Scholar]
- 34.Ramirez ER, Norman GJ, Rosenberg DE et al. Adolescent screen time and rules to limit screen time in the home. J Adolesc Health. 2011;48(4):379–385. doi: 10.1016/j.jadohealth.2010.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 36.Steptoe A, Doherty S, Kerry S, Rink E, Hilton S. Sociodemographic and psychological predictors of changes in dietary fat consumption in adults with high blood cholesterol following counseling in primary care. Health Psychol. 2000;19(5):411–419. doi: 10.1037//0278-6133.19.5.411. [DOI] [PubMed] [Google Scholar]
- 37.Wickrama KA, Ralston PA, O’Neal CW et al. Life dissatisfaction and eating behaviors among older African Americans: the protective role of social support. J Nutr Health Aging. 2012;16(9):749–753. doi: 10.1007/s12603-012-0404-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.El Ansari W, Lovell G. Barriers to exercise in younger and older non-exercising adult women: a cross sectional study in London, United Kingdom. Int J Environ Res Public Health. 2009;6(4):1443–1455. doi: 10.3390/ijerph6041443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Falba TA, Sindelar JL. Spousal concordance in health behavior change. Health Serv Res. 2008;43(1 pt 1):96–116. doi: 10.1111/j.1475-6773.2007.00754.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kegler MC, Swan D, Alcantara I, Feldman L, Glanz K. The influence of rural home and neighborhood environments on healthy eating, physical activity and weight. Prev Sci. 2014;15(1):1–11. doi: 10.1007/s11121-012-0349-3. [DOI] [PubMed] [Google Scholar]
- 41.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 42.Fulkerson JA, Rydell S, Kubik MY et al. Healthy Home Offerings via the Mealtime Environment (HOME): feasibility, acceptability, and outcomes of a pilot study. Obesity (Silver Spring) 2010;18(suppl 1):S69–S74. doi: 10.1038/oby.2009.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hutfless S, Gudzune KA, Maruthur N et al. Strategies to prevent weight gain in adults: a systematic review. Am J Prev Med. 2013;45(6):e41–e51. doi: 10.1016/j.amepre.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 44.Evans AE, Dave J, Tanner A et al. Changing the home nutrition environment: effects of a nutrition and media literacy pilot intervention. Fam Community Health. 2006;29(1):43–54. doi: 10.1097/00003727-200601000-00006. [DOI] [PubMed] [Google Scholar]
- 45.Gorin AA, Raynor HA, Fava J et al. Randomized controlled trial of a comprehensive home environment-focused weight-loss program for adults. Health Psychol. 2013;32(2):128–137. doi: 10.1037/a0026959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: Take Action—a group-randomized trial. Obesity (Silver Spring) 2011;19(10):2082–2088. doi: 10.1038/oby.2010.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kegler MC, Alcantara I, Veluswamy JK, Haardorfer R, Hotz JA, Glanz K. Results from an intervention to improve rural home food and physical activity environments. Prog Community Health Partnersh. 2012;6(3):265–277. doi: 10.1353/cpr.2012.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kivelä K, Elo S, Kyngas H, Kaariainen M. The effects of health coaching on adult patients with chronic diseases: a systematic review. Patient Educ Couns. 2014 doi: 10.1016/j.pec.2014.07.026. Epub ahead of print August 1, 2014. [DOI] [PubMed] [Google Scholar]
- 49.World Health Organization. Community health workers: what do we know about them? Available at: http://www.who.int/hrh/documents/community_health_workers.pdf. Accessed September 12, 2015.
- 50.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 51.US Department of Agriculture. Your personal path to health: steps to a healthier you. Available at: https://aglearn.usda.gov/customcontent/DMASON2/DMASON101/shared/resources/libfut/usdahealth.pdf. Accessed September 12, 2015.
- 52.US Department of Health and Human Services, US Department of Agriculture. Finding your way to a healthier you: based on the Dietary Guidelines for Americans. Available at: http://health.gov/dietaryguidelines/dga2005/document/pdf/brochure.pdf. Accessed September 12, 2015.
- 53.US Department of Health and Human Services. Be active your way. A guide for adults. Available at: http://health.gov/paguidelines/pdf/adultguide.pdf. Accessed September 12, 2015.
- 54.Ma Y, Olendzki BC, Pagoto SL et al. Number of 24-hour diet recalls needed to estimate energy intake. Ann Epidemiol. 2009;19(8):553–559. doi: 10.1016/j.annepidem.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schakel SF, Buzzard IM, Gebhardt SE. Procedures for estimating nutrient values for food composition databases. J Food Compos Anal. 1997;10(2):102–114. [Google Scholar]
- 56.Schakel SF, Jasthi B, Van Heel N, Harnack L. Adjusting a nutrient database to improve calculation of percent calories from macronutrients. J Food Compos Anal. 2009;22:S32–S36. [Google Scholar]
- 57.Schakel SF, Sievert YA, Buzzard IM. Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc. 1988;88(10):1268–1271. [PubMed] [Google Scholar]
- 58.Sallis JF, Haskell WL, Wood PD et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121(1):91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 59.Johnson-Kozlow M, Sallis J, Gilpin E, Rock C, Pierce J. Comparative validity of the IPAQ and 7-Day PAR among women diagnosed with breast cancer. Int J Behav Nutr Phys Act. 2006;3:7. doi: 10.1186/1479-5868-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sloane R, Snyder D, Demark-Wahnefried W, Lobach D, Kraus W. Comparing the 7-Day PAR with a triaxial accelerometer for measuring time in exercise. Med Sci Sports Exerc. 2009;41(6):1334–1340. doi: 10.1249/MSS.0b013e3181984fa8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Spurrier NJ, Magarey AA, Golley R, Curnow F, Sawyer MG. Relationships between the home environment and physical activity and dietary patterns of preschool children: a cross-sectional study. Int J Behav Nutr Phys Act. 2008;5:31. doi: 10.1186/1479-5868-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kristal AR, Shattuck AL, Patterson RE. Differences in fat-related dietary patterns between Black, Hispanic and White women: results from the Women’s Health Trial Feasibility Study in Minority Populations. Public Health Nutr. 1999;2(3):253–262. doi: 10.1017/s1368980099000348. [DOI] [PubMed] [Google Scholar]
- 63.Fulkerson JA, Story M, Neumark-Sztainer D, Rydell S. Family meals: perceptions of benefits and challenges among parents of 8- to 10-year-old children. J Am Diet Assoc. 2008;108(4):706–709. doi: 10.1016/j.jada.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 64.Sirard JR, Nelson MC, Pereira MA, Lytle LA. Validity and reliability of a home environment inventory for physical activity and media equipment. Int J Behav Nutr Phys Act. 2008;5:24. doi: 10.1186/1479-5868-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 66.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 67.Haardörfer R, Alcantara IC, Patil D, Hotz J, Kegler MC. Physical activity profiles of overweight and obese women in rural Georgia. JAMA Intern Med. 2014;174(1):148–149. doi: 10.1001/jamainternmed.2013.11571. [DOI] [PubMed] [Google Scholar]
- 68.Posner BM, Martin-Munley SS, Smigelski C et al. Comparison of techniques for estimating nutrient intake: the Framingham Study. Epidemiology. 1992;3(2):171–177. doi: 10.1097/00001648-199203000-00016. [DOI] [PubMed] [Google Scholar]
- 69.Dubbert PM, Vander Weg MW, Kirchner KA, Shaw B. Evaluation of the 7-day physical activity recall in urban and rural men. Med Sci Sports Exerc. 2004;36(9):1646–1654. doi: 10.1249/01.mss.0000139893.65189.f2. [DOI] [PubMed] [Google Scholar]
- 70.Bogle M, Stuff J, Davis L et al. Validity of a telephone-administered 24-hour dietary recall in telephone and non-telephone households in the rural Lower Mississippi Delta region. J Am Diet Assoc. 2001;101(2):216–222. doi: 10.1016/S0002-8223(01)00056-6. [DOI] [PubMed] [Google Scholar]
- 71.Thompson FE, Midthune D, Williams GC et al. Evaluation of a short dietary assessment instrument for percentage energy from fat in an intervention study. J Nutr. 2008;138(1):193S–199S. doi: 10.1093/jn/138.1.193S. [DOI] [PubMed] [Google Scholar]
- 72.Scagliusi FB, Ferriolli E, Pfrimer K et al. Characteristics of women who frequently under report their energy intake: a doubly labelled water study. Eur J Clin Nutr. 2009;63(10):1192–1199. doi: 10.1038/ejcn.2009.54. [DOI] [PubMed] [Google Scholar]
- 73.Leblanc ES, O’Connor E, Whitlock EP, Patnode CD, Kapka T. Effectiveness of primary care-relevant treatments for obesity in adults: a systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. 2011;155(7):434–447. doi: 10.7326/0003-4819-155-7-201110040-00006. [DOI] [PubMed] [Google Scholar]
- 74.Moyer VA. Screening for and management of obesity in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(5):373–378. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- 75.Schauer GL, Woodruff RC, Hotz J, Kegler MC. A qualitative inquiry about weight counseling practices in community health centers. Patient Educ Couns. 2014;97(1):82–87. doi: 10.1016/j.pec.2014.05.026. [DOI] [PubMed] [Google Scholar]
- 76.Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Ann Fam Med. 2009;7(3):254–260. doi: 10.1370/afm.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nutting PA, Crabtree BF, Miller WL, Stange KC, Stewart E, Jaen C. Transforming physician practices to patient-centered medical homes: lessons from the national demonstration project. Health Aff (Millwood) 2011;30(3):439–445. doi: 10.1377/hlthaff.2010.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Institute of Medicine. Primary Care and Public Health: Exploring Integration to Improve Population Health. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]