Abstract
Background
Resident participation during hepatic and pancreatic resections varies. The impact of resident participation on surgical outcomes in hepatic and pancreatic operations is poorly defined.
Methods
We identified 25,511 patients undergoing a hepatic or pancreatic resection between 2006 and 2012 using the American College of Surgeons National Surgical Quality Improvement Program database. Multivariate regression models were constructed to determine any association between resident participation and surgical outcomes.
Results
Pancreatic resections (n = 16,045; 62.9%) were more common than liver resections (n = 9,466; 37%). Residents participated in the majority of cases (n = 21,857; 86%), with most involvement at the senior level (postgraduate year ≥ 3, n = 21,147; 97%). Resident participation resulted in slightly longer mean operative times (hepatic, 9 minutes; pancreatic, 22 minutes; both P < .01). Need for perioperative transfusion, hospital duration of stay, and reoperation rates were unaffected by resident participation (all P > .05). Resident participation resulted in a higher risk of overall morbidity (odds ratio [OR], 1.14; 95% CI, 1.05–1.24; P = .001), but not major morbidity (OR, 1.05; 95% CI, 0.93–1.20; P = .40) after liver and pancreas resection. Resident participation resulted in lower odds of 30-day mortality after liver and pancreas resections (OR, 0.75; 95% CI, 0.60–0.94; P = .01).
Conclusion
Although resident participation resulted in slightly longer operative times and a modest increase in overall complications after liver and pancreatic resection, other metrics such as duration of stay, major morbidity, and mortality were unaffected. These data have important implications for educating patients regarding resident participation in these complex cases.
Teaching hospitals across the United States serve as the nucleus for research and medical innovation. Perhaps equally as important, teaching hospitals also serve to train the future generation of medical professionals. With regard to surgical specialties, the education and training of surgery residents in teaching hospitals has long been conducted through an abundant exposure to and participation in a variety of operations. Because approximately one-half of all operative procedures are performed at teaching hospitals,1 the participation of residents in a variety of operations is critical in developing future competent surgeons.
Much debate has been raised regarding the impact of resident participation during operations and the subsequent potential impact on perioperative morbidity and mortality. Beginning in 2005, the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) Database began recording data on the presence or absence of a surgery resident in operative procedures. In addition, the postgraduate year (PGY) of the most senior resident participant was recorded, if applicable. Several previous studies have examined the impact of resident participation and outcomes using this database. Specifically, outcomes after operations in general,2,3 vascular,4,5 oncologic,6 and breast7 surgeries have been studied and reported. These reports on the impact of resident participation on perioperative outcome have been mixed; some studies show no effect, whereas others have shown a correlation between resident participation and poorer perioperative outcomes.
Hepatic and pancreatic resections are often complex operations with an associated morbidity and mortality greater than most other surgical subspecialties. As such, there has been increasing evidence to perform these operations at high-volume centers, the majority of which are teaching hospitals. Despite previous studies exploring the association between resident participation in operations and perioperative outcomes,8 no study to our knowledge has investigated outcomes after only hepatic and pancreatic resection using a national database. Thus, the objective of the current study was to analyze the impact of resident participation on perioperative morbidity and mortality among patients undergoing liver or pancreas resections using the ACS NSQIP database.
METHODS
We queried the ACS NSQIP database for all patients undergoing a liver or pancreatic resection between 2005 and 2012 using corresponding Current Procedural Terminology (CPT) codes (liver, 47100, 47120, 47122, 47125, 47130; pancreas, 48140, 48145, 48146, 48148, 48150, 48152, 48153, 48154, 48155). The cohort was categorized based on the presence or absence of a resident. The variables included and the quality assurance protocols used by the ACS for the NSQIP database have been described previously.9 Cases with a missing field for resident participation (n = 10,702) were excluded. The highest level of resident participation was further classified into 2 categories: junior level (PGY 1 and 2) and senior level (PGY ≥3) participation. Because the NSQIP database only records PGY years and does not designate between resident and fellow status, it is not possible to tell which participants were fellows; therefore, all participants beyond PGY3 were considered senior residents.
Outcomes
The primary outcome of this study was the incidence of any perioperative 30-day complication. The impact of resident participation on the incidence of perioperative 30-day mortality was also investigated. Superficial surgical site infections and urinary tract infections were classified as minor postoperative complications as previously described.4 Major postoperative complications included deep incisional or organ space infection, dehiscence, sepsis, postoperative hemorrhage requiring transfusion, reintubation or failure to wean from the ventilator, cardiac event, neurologic event, pneumonia, venous thromboembolic event, reoperation, graft failure, or acute renal failure.
Statistical analysis
Standard measures of frequencies and central tendency were calculated to summarize characteristics of patients, operations, and perioperative outcomes. Demographics, comorbidities, and multivariable-adjusted outcomes for 30-day perioperative morbidity and mortality were compared among operative cases in which a resident was or was not present. Multivariable logistic regression was used to adjust for variables that were statistically significant on univariable analysis (P <.05) or of clinical significance. Chi-square analysis was used for comparison of categorical variables and t test or Wilcoxon rank-sum test was utilized for continuous variables as indicated. P values are 2 tailed. All analyses were carried out with STATA version 13.0 (StataCorp LP, College Station, TX).
RESULTS
Description of cohort
We identified 25,511 patients undergoing a liver (16,045; 63%) or pancreas (n = 9,466; 37%) resection during the study period. The median age of the cohort was 62 years (interquartile range, 53–62) with a slight majority being female (52%) and a majority of white race (78%; Table I). Comorbidities were common as the majority of patients had an American Society of Anesthesiologists (ASA) classification of 3 or 4 (67%), the most common being hypertension (51%) and an active smoking history (20%). Of these patients, 16% had disseminated cancer with 6% of the cohort receiving chemotherapy within 30 days of surgery. At the time of surgery, the most common pancreas resection was coded as a partial pancreatectomy (CPT 48150; 23%), whereas the most common liver resection was coded as a partial lobectomy (CPT 47120; 22%).
Table I.
Clinicopathologic characteristics of cohort
| Characteristic | Total (n = 25,511) | Resident participation (n = 21,857) | No resident participation (n = 3,654) | P value |
|---|---|---|---|---|
| Age, y, median (IQR) | 62 (53, 62) | 63 (53, 63) | 62 (52, 62) | .002 |
| Male gender | 12,326 (48.4) | 10,609 (48.6) | 1717 (47.1) | .08 |
| Race | <.001 | |||
| White | 18,923 (78.4) | 16,157 (78.2) | 2,766 (79.2) | |
| Black | 2,238 (9.3) | 2,012 (9.7) | 226 (6.5) | |
| Hispanic | 1,924 (8.0) | 1,660 (8.0) | 264 (7.6) | |
| Other | 826 (4.0) | 236 (6.8) | ||
| Comorbidities | ||||
| IDDM | 2,138 (8.4) | 1,810 (8.3) | 328 (9.0) | .27 |
| Smoking | 5,033 (19.7) | 4,317 (19.8) | 716 (19.6) | .83 |
| Alcohol | 748 (3.0) | 654 (3.0) | 94 (2.6) | .22 |
| Hypertension | 12,876 (50.5) | 11,017 (50.4) | 1,859 (50.9) | .60 |
| End-stage renal disease | 106 (0.4) | 87 (0.4) | 19 (0.5) | .29 |
| Disseminated cancer | 4,189 (16.4) | 3,615 (16.6) | 574 (15.7) | .21 |
| Ascites | 253 (0.1) | 204 (0.9) | 49 (1.3) | .02 |
| Preoperative transfusion | 168 (0.6) | 121 (0.6) | 47 (1.3) | <.001 |
| Preoperative chemotherapy | 1,394 (5.5) | 1,261 (5.8) | 133 (3.7) | <.001 |
| Sepsis | 145 (0.6) | 113 (0.5) | 32 (0.9) | <.001 |
| ASA class | .14 | |||
| 1/2 | 8,380 (32.9) | 7,190 (32.9) | 1,370 (32.6) | |
| 3/4 | 17,093 (67.1) | 14,635 (67.0) | 2,458 (67.3) | |
| Emergency case | 297 (1.2) | 226 (1.0) | 71 (1.9) | <.001 |
| Pancreas resection | 16,045 (62.9) | 13,756 (62.9) | 2,289 (62.6) | .74 |
| Liver resection | 9,466 (37.1) | 8,101 (37.1) | 1, 365 (37.4) | .74 |
| Highest resident participant | 39 (17.4) | 15 (13.5) | 22 (21.0) | |
| Junior (PGY 1/2) | 710 (3.2) | N/A | ||
| Senior (PGY ≥3) | 21, 147 (96.8) | N/A | ||
ASA, American Society of Anesthesiologists; IDDM, insulin-dependent diabetes mellitus; IQR, interquartile range; PGY, postgraduate year.
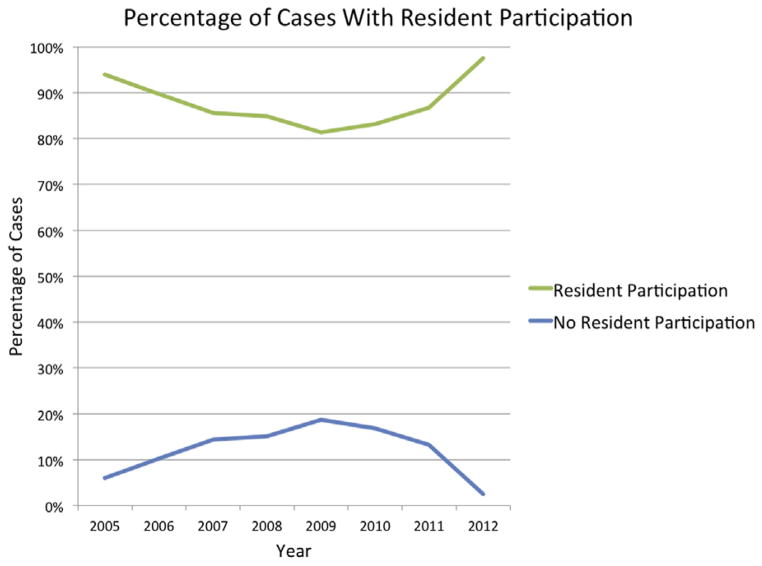
The majority of operations had a documented resident present during the operation (n = 21,857; 86%) and resident participation increased over the study period (Figure). Most operations with a resident participant were at the senior (97%) as opposed to the junior (3%) level. Several patient demographics differed among cases with and without resident participation. Specifically, patients without a resident participant had a lower median age, were more likely to be white, and were more likely to receive a preoperative blood transfusion or chemotherapy within 30 days of surgery (all P < .01). In the multivariable logistic regression model, there was a greater odds of resident participation among cases with black patients (odds ratio [OR], 1.48; 95% CI, 1.28–1.70; P < .001) and those performed after 2011 (OR, 2.42; 95% CI, 1.56–3.76; P <.001) (Table II). Contrastingly, older patients (OR, 0.91; 95% CI, 0.85–0.98; P = .01) and male patients (OR, 0.92; 95% CI, 0.86–0.99; P = .04) were less likely to have a resident participate during their operation.
Fig.
Percentage of cases with resident participation over time.
Table II.
Univariable and multivariable logistic regression for resident participation
| Variables | Univariable analysis
|
Multivariable analysis
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age >65 y | 0.91 | 0.85–0.98 | .008 | 0.91 | 0.85–0.98 | .01 |
| Male gender | 0.94 | 0.88–1.01 | .08 | 0.92 | 0.86–0.99 | .04 |
| White race | Ref | — | — | Ref | — | — |
| Black | 1.52 | 1.32–1.76 | <.001 | 1.48 | 1.28–1.70 | <.001 |
| Hispanic | 1.08 | 0.94–1.23 | .29 | 1.02 | 0.89–1.18 | .35 |
| Functional status | ||||||
| Independent | Ref | — | — | |||
| Partially dependent | 0.79 | 0.61–1.03 | .09 | |||
| Totally dependent | 1.06 | 0.69–1.62 | .79 | |||
| Smoking | 1.00 | 0.92–1.10 | .83 | |||
| Alcohol use | 1.15 | 0.92–1.43 | .22 | |||
| ASA class | ||||||
| 1/2 | Ref | — | — | — | — | — |
| 3/4 | 0.99 | 0.91–1.06 | .70 | — | — | — |
| Year | ||||||
| 2005 | Ref | — | — | Ref | — | — |
| 2006–2011 | 0.35 | 0.26–0.48 | <.001 | 0.35 | 0.26–0.49 | <.001 |
| 2012 | 2.51 | 1.63–3.86 | <.001 | 2.42 | 1.56–3.76 | <.001 |
| Pancreas resection | 1.01 | 0.94–1.09 | .74 | — | — | — |
ASA, American Society of Anesthesiologists; OR, odds ratio.
Perioperative morbidity and mortality
Mean operative time among all cases was 298 ± 142 minutes and was longer among patients undergoing a pancreas (330 ± 143 minutes) compared with a liver (245 ± 124 minutes) resection (P < .001; Table III). With regard to resident participation, operative time was longer among cases with a resident present for both pancreas (resident, 332 ± 142 vs no resident, 310 ± 145 minutes; P < .001) and liver (resident, 246 ± 123 vs no resident, 237 ± 132 minutes; P = .01) resections. Resident participation did not affect the incidence of intraoperative and postoperative transfusion among pancreas (P = .10) and liver (P = .84) resections. Hospital duration of stay and incidence of reoperation also did not differ whether a resident was present during the operation or not (all P >.05). Overall perioperative morbidity, however, was more common after pancreas (38%) compared with liver (29%) resections (P < .001). Similarly, the incidence of major morbidity was greater after pancreas (31%) versus liver (24%) resections (P < .001).
Table III.
Perioperative outcomes after pancreas and liver resection
| No resident pancreas | Resident pancreas | P value | No resident liver | Resident liver | P value | |
|---|---|---|---|---|---|---|
| Operative time, min, mean (SD) | 310 (145) | 332 (142) | <.001 | 237 (132) | 246 (123) | .01 |
| Intraoperative transfusion | 1,210 (52.9) | 7,525 (54.7) | .10 | 771 (56.5) | 4,552 (56.2) | .84 |
| Postoperative transfusion | 211 (9.2) | 1,345 (9.8) | .40 | 137 (10.0) | 813 (10.0) | .99 |
| Duration of stay, d, median (IQR) | 9 (7, 14) | 8 (6, 14) | .20 | 6 (5, 8) | 6 (4, 8) | .57 |
| Reoperation | 146 (6.4) | 885 (6.4) | .92 | 60 (4.4) | 335 (4.1) | .66 |
| Overall unadjusted mortality | 76 (3.3) | 339 (2.5) | .02 | 41 (3.0) | 208 (2.6) | .35 |
| Overall unadjusted morbidity | 807 (35.3) | 5,273 (38.3) | .005 | 365 (26.7) | 2,353 (29.1) | .08 |
| Minor | 220 (9.6) | 1,860 (13.5) | <.001 | 88 (6.5) | 686 (8.5) | .01 |
| Major | 702 (30.7) | 4,298 (31.2) | .58 | 319 (23.4) | 1,962 (24.2) | .50 |
IQR, Interquartile range; SD, standard deviation.
Patients with a resident participant experienced a higher unadjusted rate of perioperative morbidity (resident, 35% vs no resident, 32%; P = .001). After stratifying by resection type, cases with resident participation had a higher incidence of morbidity after pancreas resections (resident, 35% vs no resident, 31%; P = .005), but not liver resections (resident, 29% vs no resident, 27%; P = .08). Resident participation resulted in a greater incidence of superficial surgical site infections (resident, 7% vs no resident, 5%; P < .001). The incidence of major morbidity, however, was similar among pancreas (resident, 31% vs no resident, 31%; P = .58) and liver (resident, 24% vs no resident, 23%; P = .50) resections regardless of resident participation.
In the multivariable logistic regression model adjusting for all competing confounders, older patients (OR, 1.19; 95% CI, 1.11–1.26; P < .001), Hispanic patients (OR, 1.31; 95% CI, 1.19–1.44; P < .001), those patients with poorer functional status (partially dependent: OR, 1.96 [95% CI, 1.58–2.42] vs totally dependent: OR, 2.42 [95% CI, 1.78–3.30]; both P <.001) and more comorbidities (ASA class 3 or 4: OR, 1.56 [95% CI, 1.47–1.65]; P < .001), as well as those patients undergoing a pancreas resection (OR, 1.51; 95% CI, 1.43–1.61; P < .001) were at greater risk for perioperative morbidity (Table IV). Furthermore, resident participation was associated with a greater risk of perioperative morbidity as compared with cases without any resident participation (OR, 1.14; 95% CI, 1.05–1.24; P = .001). Resident participation was an independent risk factor for developing a superficial surgical site infection (OR, 1.46; 95% CI, 1.24–1.72; P < .001). However, with regard to major morbidity, resident participation was not associated with a higher risk in the multivariable model (OR, 1.05; 95% CI, 0.93–1.20; P = .40).
Table IV.
Univariable and multivariable logistic regression analysis for any perioperative complication
| Variables | Univariable analysis
|
Multivariable analysis
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age >65 y | 1.29 | 1.23–1.36 | <.001 | 1.19 | 1.11–1.26 | <.001 |
| Male gender | 0.85 | 0.81–0.89 | <.001 | — | — | — |
| White race | Ref | — | — | Ref | — | — |
| Black | 1.04 | 0.95–1.14 | .42 | 1.02 | 0.93–1.12 | .69 |
| Hispanic | 1.29 | 1.17–1.42 | <.001 | 1.31 | 1.19–1.44 | <.001 |
| Functional status | ||||||
| Independent | Ref | — | — | Ref | — | — |
| Partially dependent | 2.18 | 1.78–2.66 | <.001 | 1.96 | 1.58–2.42 | <.001 |
| Totally dependent | 2.89 | 2.15–3.89 | <.001 | 2.42 | 1.78–3.30 | <.001 |
| Smoking | 1.10 | 1.03–1.18 | .003 | 1.09 | 1.02–1.17 | .01 |
| Alcohol use | 1.20 | 1.04–1.40 | .02 | 1.17 | 0.99–1.36 | .06 |
| Disseminated cancer | 0.86 | 0.80–0.93 | <.001 | 1.06 | 0.97–1.15 | .23 |
| Preoperative chemotherapy | 1.24 | 1.11–1.38 | <.001 | 1.40 | 1.24–1.58 | <.001 |
| Diabetes | 1.21 | 1.16–1.26 | <.001 | 1.09 | 1.04–1.14 | <.001 |
| ASA class | ||||||
| 1/2 | Ref | — | — | Ref | — | — |
| 3/4 | 1.60 | 1.51–1.70 | <.001 | 1.56 | 1.47–1.65 | <.001 |
| Year | ||||||
| 2005 | Ref | — | — | Ref | — | — |
| 2006–2011 | 1.29 | 1.10–1.52 | .002 | 1.20 | 1.01–1.43 | .04 |
| 2012 | 1.71 | 1.41–2.06 | <.001 | 1.55 | 1.28–1.89 | <.001 |
| Pancreas resection | 1.51 | 1.43–1.60 | <.001 | 1.51 | 1.43–1.61 | <.001 |
| Resident participation | 1.13 | 1.05–1.22 | <.001 | 1.14 | 1.05–1.24 | .001 |
ASA, American Society of Anesthesiologists; OR, odds ratio.
Similar to the findings in the multivariate model for perioperative morbidity, we found several clincopathologic and operative characteristics associated with an increased risk of perioperative mortality (Table V). Specifically, older patients (OR, 1.95; 95% CI, 1.64–2.33; P < .001), those with poorer functional status (partially dependent: OR, 2.63 [95% CI, 1.81–3.82] vs totally dependent: OR, 2.97 [95% CI, 1.80–4.89]; both P < .001) and more comorbidities (ASA class 3 or 4: OR, 2.54 [95% CI, 1.97–3.29]; P <.001), as well as those patients who experienced perioperative morbidity (OR, 13.80; 95% CI, 10.78–17.66; P < .001) were at greater risk for perioperative mortality (Table IV). Interestingly, resident participation was associated with a lesser risk of perioperative mortality (OR, 0.75; 95% CI, 0.60–0.94; P = .01).
Table V.
Univariable and multivariable logistic regression analysis for perioperative mortality
| Variables | Univariable analysis
|
Multivariable analysis
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age >65 y | 2.39 | 2.01–2.93 | <.001 | 1.95 | 1.64–2.33 | <.001 |
| Male gender | 0.69 | 0.59–0.81 | <.001 | 0.75 | 0.63–0.88 | .001 |
| White race | Ref | — | — | |||
| Black | 0.84 | 0.62–1.13 | .24 | |||
| Hispanic | 1.21 | 0.92–1.59 | .18 | |||
| Functional status | ||||||
| Independent | Ref | — | — | Ref | — | — |
| Partially dependent | 4.93 | 3.54–6.86 | <.001 | 2.63 | 1.81–3.82 | <.001 |
| Totally dependent | 6.16 | 3.98–9.53 | <.001 | 2.97 | 1.80–4.89 | <.001 |
| Smoking | 0.93 | 0.77–1.13 | .49 | |||
| Alcohol use | 1.30 | 0.87–1.96 | .20 | |||
| Disseminated cancer | 0.91 | 0.74–1.13 | .39 | |||
| Preoperative chemotherapy | 0.76 | 0.52–1.11 | .15 | |||
| Diabetes | 1.35 | 1.22–1.51 | <.001 | 1.06 | 0.83–1.35 | .63 |
| ASA | ||||||
| 1/2 | Ref | — | — | Ref | — | — |
| 3/4 | 3.77 | 2.97–4.78 | <.001 | 2.54 | 1.97–3.29 | <.001 |
| Year | ||||||
| 2005 | Ref | — | — | Ref | — | — |
| 2006–2011 | 1.51 | 0.87–2.63 | .15 | 1.19 | 0.73–2.21 | .40 |
| 2012 | 1.07 | 0.56–2.05 | .84 | 0.90 | 0.47–1.72 | .74 |
| Pancreas resection | 0.98 | 0.84–1.15 | .83 | 0.92 | 0.78–1.08 | .32 |
| Perioperative morbidity | 14.78 | 11.68–18.71 | <.001 | 13.80 | 10.78–17.66 | <.001 |
| Resident participation | 0.78 | 0.63–0.95 | .01 | 0.75 | 0.60–0.94 | .01 |
ASA, American Society of Anesthesiologists; OR, odds ratio.
DISCUSSION
The impact of resident participation on perioperative outcomes has been greatly debated in recent years through various methodologies. Single-institution studies as well as large, multi-institution studies have analyzed the impact of resident participation after a variety of operations in general,2,3 vascular,4,5 oncologic,6 and breast7 subspecialties. However, to our knowledge, the impact of resident participation on perioperative outcomes after only complex liver and pancreatic resections has not been studied. The study of this potential association between outcomes and resident participation is important for several reasons. Recently, there have been several investigators advocating for centralization and concentration of care of liver and pancreatic surgical diseases in high-volume centers.10,11 In fact, recent studies show that the majority of pancreatic and hepatic resections performed in the United States are in fact performed at teaching hospitals.12 As such, investigation into the impact of resident participation during liver and pancreatic resections is pertinent and necessary. Using the ACS NSQIP database, we found that although both liver and pancreas resections with resident participants resulted in a longer operative time, perioperative major morbidity was unaffected. Interestingly, resident participation was more likely in cases with black patients and those treated after 2011, indicating a nonrandom pattern of care and a potential area of disparate care. Perhaps equally as important, patients with a resident participant during their resection had a mortality benefit compared with cases with no resident present.
Several hypotheses have been proposed as to the potential association and impact of residents on surgical outcomes. Raval et al13 hypothesized that the impact of resident participation on perioperative outcomes after operative procedures was multifactorial. The authors proposed increased intraoperative technical complications, unmeasured case mix differences, and reporting bias of these perioperative outcomes as potential factors related to the resident impact seen.13 With regard to technical complications, our data show that operative time was significantly longer owing to resident participation in both liver and pancreatic resections. Because residents likely do not have experience with these complex operations, it is perhaps not surprising that operative time is lengthened. This increased mean operative time potentially may have led to the increase in the incidence of minor perioperative complications, particularly superficial surgical site infections, seen with resident participation. This association of increased morbidity with prolonged operative time has been well-described.14 Our data support this notion; the majority of increased morbidity was owing to a higher incidence of surgical site infections. In fact, patients who had a resident present were at 1.46 greater odds of developing a superficial surgical site infection compared with those cases without a resident present. Despite this, major clinically relevant morbidity was unaffected by resident participation (P = .21). Furthermore, overall hospital duration of stay was unaffected by resident participation. These results corroborate previous reports using the ACS NSQIP database that found an increase in minor, but not major, morbidity owing to resident participation.3,9 In aggregate, resident participation in liver and pancreatic resections should be encouraged; major morbidity seems to be unaffected by their participation.
Of all the measurable factors analyzed, the occurrence of a perioperative complication was found to have the strongest association with perioperative mortality. In fact, patients who experienced a perioperative complication were >14 times more likely to experience perioperative death compared with those who had no perioperative complication. Despite cases with resident participants having an overall greater incidence of perioperative morbidity, resident participation was found to be not associated independently with an increased risk of mortality. In fact, resident participation was an independent protective factor; the odds of perioperative mortality were decreased by 25%. These findings are likely explained by the fact that the increase in morbidity found with resident participation were minor and likely clinically insignificant. Rather, resident participation may have a beneficial effect in the perioperative period. To this point, Raval et al13 found that resident participation was associated with 1.4 fewer deaths per 1,000 general and vascular surgery cases. Similarly, Castleberry et al6 found an increase in perioperative morbidity but a lesser mortality rate among patients undergoing gastrointestinal oncologic procedures. The current study is unique; our data focused on only liver and pancreas resections. As noted, the findings of a protective survival benefit with resident participation may in fact be owing to improved postoperative care. As opposed to nonteaching hospitals, surgery residents often staff the hospital wards 24 hours a day and thus may be able to provide more comprehensive postoperative care. This presence may also help to prevent mortality after a perioperative complication (ie, improved failure to rescue rate15). However, the exact causes of these findings are difficult to determine as resident involvement during an operation does not always imply resident participation during postoperative care, because this is not recorded in the NSQIP database. Taken together, resident participation during liver and pancreas resections is associated with a lesser risk of perioperative mortality and thus provides further support for resident participation during these cases.
Recent changes to training in surgery have resulted in a decreased ability of surgery residents to gain appropriate exposure complex cases. Sachs et al16 showed that nearly one-half of all graduating chief surgery residents in the United States performed <10 cases in liver and pancreas categories at the time of graduation. Furthermore, the number of teaching assistant cases logged by graduating chief residents for hepatopancreaticobiliary procedures in 2012 was nearly zero. As such, it seems that, upon graduation, surgery residents may have inadequate exposure to complex hepatopancreatic cases. These data are pertinent because the impact of operative experience on perioperative outcomes has been well-established, particularly with regard to liver and pancreas surgery.17 The failure of surgery residents to achieve a high number of cases in these categories is undoubtedly multifactorial. Data from the current study, however, provides strong evidence that resident participation during these cases has no major clinical impact on perioperative outcomes and may even result in an improved perioperative mortality rate. As such, our data provide strong support for the participation of residents during liver and pancreas resections.
There are several limitations to this study that should be considered when interpreting the data. Primarily, the limitations of this study are related to the administrative nature of the ACS NSQIP database. Specific to this study, data on procedure-specific morbidity such as pancreatic fistula leak or bile leak are not available currently. Thus, morbidity rates after these operations may in fact be underreported. Furthermore, ACS NSQIP membership is overrepresented by tertiary centers and specialized high-volume institutions and thus may not be representative of all hospitals performing these operations in the United States. The goal of this study, however, was to analyze the impact of resident participation on surgery outcomes and not the impact of hospital-level factors on the incidence of morbidity and mortality. Finally, as with all retrospective studies, selection bias with regard to resident participation is a possibility because it was not assigned randomly. This potentially could have had an effect on the differences in outcomes seen between the 2 groups in our study.
In conclusion, although resident participation resulted in slightly longer operative times and a modest increase in minor complications after liver and pancreatic resection, other metrics such as hospital duration of stay, major morbidity, and mortality were unaffected. These data have important implications for educating patients regarding resident participation in these complex cases.
Footnotes
Presented at the 10th Annual Academic Surgical Congress in Las Vegas, Nevada, February 3–5, 2015.
References
- 1.Association of American Colleges. Key facts about teaching hospitals. updated 2009; cited 2014Sep 1. Available at: www.aamc.org/download/82452/data/keyfactsaboutth.pdf.
- 2.Advani V, Ahad S, Gonczy C, Markwell S, Hassan I. Does resident involvement effect surgical times and complication rates during laparoscopic appendectomy for uncomplicated appendicitis? An analysis of 16,849 cases from the ACS-NSQIP. Am J Surg. 2012;203:347–51. doi: 10.1016/j.amjsurg.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Davis SS, Jr, Husain FA, Lin E, Nandipati KC, Perez S, Sweeney JF. Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg. 2013;216:96–104. doi: 10.1016/j.jamcollsurg.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Iannuzzi JC, Chandra A, Rickles AS, Kumar NG, Kelly KN, Gillespie DL, et al. Resident involvement is associated with worse outcomes after major lower extremity amputation. J Vasc Surg. 2013;58:827–831. e1. doi: 10.1016/j.jvs.2013.04.046. [DOI] [PubMed] [Google Scholar]
- 5.Reeves JG, Kasirajan K, Veeraswamy RK, Ricotta JJ, 2nd, Salam AA, Dodson TF, et al. Characterization of resident surgeon participation during carotid endarterectomy and impact on perioperative outcomes. J Vasc Surg. 2012;55:268–73. doi: 10.1016/j.jvs.2011.08.039. [DOI] [PubMed] [Google Scholar]
- 6.Castleberry AW, Clary BM, Migaly J, Worni M, Ferranti JM, Pappas TN, et al. Resident education in the era of patient safety: a nationwide analysis of outcomes and complications in resident-assisted oncologic surgery. Ann Surg Oncol. 2013;20:3715–24. doi: 10.1245/s10434-013-3079-2. [DOI] [PubMed] [Google Scholar]
- 7.Fischer JP, Wes AM, Kovach SJ. The impact of surgical resident participation in breast reduction surgery–outcome analysis from the 2005–2011 ACS-NSQIP datasets. J Plast Surg Hand Surg. 2014;48:315–21. doi: 10.3109/2000656X.2014.882345. [DOI] [PubMed] [Google Scholar]
- 8.Relles DM, Burkhart RA, Pucci MJ, Sendecki J, Tholey R, Drueding R, et al. Does resident experience affect outcomes in complex abdominal surgery? Pancreaticoduodenectomy as an example. J Gastrointest Surg. 2014;18:279–85. doi: 10.1007/s11605-013-2372-5. [DOI] [PubMed] [Google Scholar]
- 9.Tseng WH, Jin L, Canter RJ, Martinez SR, Khatri VP, Gauvin J, et al. Surgical resident involvement is safe for common elective general surgery procedures. J Am Coll Surg. 2011;213:19–26. doi: 10.1016/j.jamcollsurg.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 10.Rosales-Velderrain A, Bowers SP, Goldberg RF, Clarke TM, Buchanan MA, Stauffer JA, et al. National trends in resection of the distal pancreas. World J Gastroenterol. 2012;18:4342–9. doi: 10.3748/wjg.v18.i32.4342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tol JA, van Gulik TM, Busch OR, Gouma DJ. Centralization of highly complex low-volume procedures in upper gastrointestinal surgery. A summary of systematic reviews and meta-analyses. Dig Surg. 2012;29:374–83. doi: 10.1159/000343929. [DOI] [PubMed] [Google Scholar]
- 12.Hyder O, Sachs T, Ejaz A, Spolverato G, Pawlik TM. Impact of hospital teaching status on length of stay and mortality among patients undergoing complex hepatopancreaticobiliary surgery in the USA. J Gastrointest Surg. 2013;17:2114–22. doi: 10.1007/s11605-013-2349-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raval MV, Wang X, Cohen ME, Ingraham AM, Bentrem DJ, Dimick JB, et al. The influence of resident involvement on surgical outcomes. J Am Coll Surg. 2011;212:889–98. doi: 10.1016/j.jamcollsurg.2010.12.029. [DOI] [PubMed] [Google Scholar]
- 14.Schroeder RA, Marroquin CE, Bute BP, Khuri S, Henderson WG, Kuo PC. Predictive indices of morbidity and mortality after liver resection. Ann Surg. 2006;243:373–9. doi: 10.1097/01.sla.0000201483.95911.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spolverato G, Ejaz A, Hyder O, Kim Y, Pawlik TM. Failure to rescue as a source of variation in hospital mortality after hepatic surgery. Br J Surg. 2014;101:836–46. doi: 10.1002/bjs.9492. [DOI] [PubMed] [Google Scholar]
- 16.Sachs TE, Ejaz A, Weiss M, Spolverato G, Ahuja N, Makary MA, et al. Assessing the experience in complex hepatopancreatobiliary surgery among graduating chief residents: is the operative experience enough? Surgery. 2014;156:385–93. doi: 10.1016/j.surg.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tseng JF, Pisters PW, Lee JE, Wang H, Gomez HF, Sun CC, et al. The learning curve in pancreatic surgery. Surgery. 2007;141:694–701. doi: 10.1016/j.surg.2007.04.001. [DOI] [PubMed] [Google Scholar]