We thank Dr. Barthel and colleagues for taking an interest in our review on primary and secondary glioblastoma (1). They present the case of a 72-year-old patient with an IDH1 mutation–negative glioblastoma, monitored by combined [11C]methionine (MET) amino acid transport PET/MRI. They diagnosed the first tumor as a low-grade astrocytoma, based on the absence of contrast enhancement in MRI, and unremarkable nuclear magnetic resonance (NMR) spectroscopy, but without histologic confirmation. Only 6 weeks later, a typical contrast-enhancing mass on MRI with further increase in amino acid transport was shown. Resection and histopathologic examination revealed a glioblastoma. The very short clinical history, absence of an IDH1 mutation, and the evidence of EGFR overexpression and LOH at the PTEN locus on chromosome 10, strongly support the diagnosis of a primary glioblastoma. This most common glioblastoma type is typically defined by a lack of clinical, radiologic, or histologic evidence of a less malignant precursor lesion. Their evolution is so fast that early lesions almost always escape clinical detection. The case presented by Dr. Barthel and colleagues is an exceptional observation as it shows a small precursor lesion shortly before the diagnosis of a large glioblastoma. We present a similar observation (Fig. 1; ref. 2). Following a seizure attack, the MRI of the 79-year-old patient showed a small cortical lesion that within 10 weeks developed into a full-blown glioblastoma with perifocal edema and central necrosis. For neither of these cases do we postulate that the precursor lesion was a low-grade astrocytoma. Instead, we got a rare glimpse of the remarkable dynamics of the evolution of primary glioblastomas.
Figure 1.
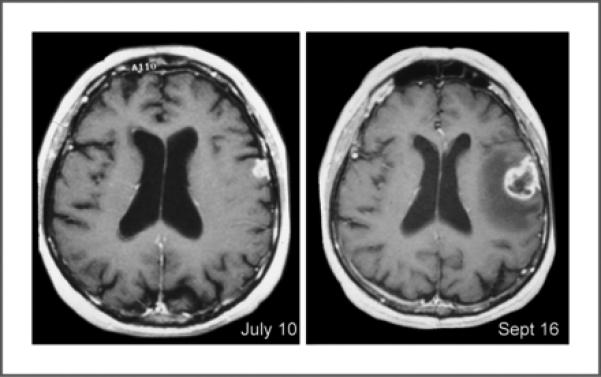
Primary glioblastoma. The first MRI revealed a small cortical lesion. Only 2 months later, the second MRI showed a full-blown glioblastoma with perifocal edema and central necrosis.
Footnotes
Disclosure of Potential Conflicts of Interest No potential conflicts of interest were disclosed.
References
- 1.Ohgaki H, Kleihues P. The definition of primary and secondary glioblastoma. Clin Cancer Res. 2013;19:764–72. doi: 10.1158/1078-0432.CCR-12-3002. [DOI] [PubMed] [Google Scholar]
- 2.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, editors. WHO classi-fication of tumours of the central nervous system. 4th ed. International Agency for Research on Cancer; Lyon, France: 2007. [Google Scholar]


