Abstract
Background:
A suitable sedative status during gastro-enteric endoscopies results in better physicians’ approach and more stable view of internal organs. Therefore, we evaluated the effect of ketamine for sedation in endoscopic procedures of adult patients.
Materials and Methods:
Patients who were candidates for gastro-enteric endoscopy during the years 2014-2015 were included into the study and divided into two groups of case (administered 5 mg/kg of oral ketamine half an hour before initiation of the procedure) and control (administered placebo in a same pattern). After endoscopy, patients and physicians’ satisfaction of sedation was assessed. SPSS-22 was used for data analysis.
Results:
Eighty-six patients participated into the study of which divided into each groups. The pain and discomfort scores were 2.4 ± 1.8 and 5.81 ± 1.48 in case and control groups, respectively, (P < 0.001). Mann-Whitney test revealed statistical difference among groups about physician's satisfaction of sedation during endoscopy (P < 0.001). Patients who received ketamine had better sedative status (P < 0.001). None of the patients in the case group was completely awake but all of the patients in the control group were awake. The number of retching during endoscopy showed that individuals in the control group had more frequent retching episodes (P = 0.04).
Conclusion:
Low-dose oral administration of ketamine could make a satisfied sedation for gastro-enteric endoscopy.
Keywords: Gastro-enteric endoscopy, ketamine, sedation
INTRODUCTION
Endoscopy is the most accurate and beneficial way for the diagnosis of dyspepsia, peptic ulcers, and malignancies.[1] Sedative drugs are used for both patient and physician satisfaction during the procedure; type of endoscopy, duration, degree of difficulty, and patients’ physical status are the criteria which determine the suitable type of sedation for endoscopy.[2] Although there are several drugs and techniques for the induction of sedation and reduction of pain during gastro-enteric endoscopies, there is no standardized method of sedation, and physicians themselves choose the best method regarding their experience.[3,4,5,6]
Benzodiazepines are mostly used for the goal of sedation,[7,8] and among them, midazolam is the drug of choice. Opioids (including pethidine and fentanyl), propofol, ketamine, and droperidol are other sedative drugs used for the same purpose.[9,10] Ketamine could be used as a substitute of opioids and benzodiazepines for sedation during endoscopy with a wide spectrum effects on pain, amnesia, anesthesia, and sedation which can be administered intravenous, intramuscular, or even oral and rectal. Dose of 0.2-0.5 mg/body weight (Kg) is usually used for reduction of pain and after 10-15 min, the full consciousness is returned. Delusion, auditory and visual hallucinations, and other side effects which may occurred in a period of 24 h after ketamine administration make some limitations for drug usage. A potential contractive effect on laryngeal muscles in unwell patients also would lead to significantly unpredictable decrease in blood pressure and cardiac output. Previous studies had worked on the combination of ketamine and midazolam for the induction of sedation in pediatric gastro-enteric endoscopy but there is no similar study on adults.[12]
In some areas of the world, ketamine is mostly used in sedation for endoscopy for all ages due to lack of other medications.[13] Ketamine is also used for the reduction of neuropathic pains such as postherpetic neuralgia, complex regional pain syndrome, malignancy, orofacial pain, and limb phantom pain.[14] Due to lack of enough data about the effect of ketamine on endoscopic sedation, we designed this study to evaluate the mentioned purpose.
MATERIALS AND METHODS
This double-blinded, randomized clinical trial study was done by the grant of Isfahan University of Medical Sciences during the years 2014-2015 with the group of patients who were candidates for gastro-enteric endoscopy. Inclusion criteria were the following: Age between 18 and 65 years, absence of hypersensitivity or any contraindication for ketamine, absence of mental or physical retardation, and no history of hypertension, seizure, hyperthyroidism, immune deficiency, or increased intraocular pressure. Any patient who required emergent intervention or who showed drug sensitivity during the study was excluded from the study.
All the patients who had the inclusion criteria were informed about the study protocols and procedures and fulfilled a written consent, after that they were divided into two groups of case and controls by computer randomizing system meaning that every participant had a number categorized into case or control group by the computer.
A questionnaire including demographic data was fulfilled; patients in case group administered 5 mg/body weight (Kg) of ketamine,[21,22] 30 min before the endoscopy and the control group received placebo in the same order. For complete blindness of the study, drug or placebo was solved in 10 cc of apple juice because of the bitter taste of ketamine and after that, medication was given to the patient by a nurse who was blinded about the study protocols. After finishing the procedure, pain severity, degree of sedation, and physicians’ satisfaction of sedation were measured in both groups. Visual analog scale was used for pain assessment and physicians’ satisfaction of sedation was measured with the following scale: Very bad (scale 0), bad (scale 1), intermediate (scale 2), good (scale 3), and very good (scale 4). The sedation was also assessed with 1 = completely awake, 2 = awake but drowsy, 3 = asleep but responsive to verbal commands, 4 = asleep but responsive to tactile stimulus, and 5 = asleep and not responsive to any stimulus.
Finally, all the gathered data were analyzed using SPSS-20 software (SPSS Inc., Chicago, Illinois, USA); t-test, independent t-test, Mann-Whitney test, and Chi-square test were used for data analysis and P < 0.05 was considered statistically significant.
RESULTS
Eighty-six patients (43 in case group and 43 in control group) who were candidates for gastro-enteric endoscopy were included into this study; of which 43 (50%) individuals were males and 43 (50%) were females. As seen in Table 1, no differences were seen among groups regarding age, sex, and level of academic degree. Most of the patients had high school education in both groups.
Table 1.
Demographic and educational data of case and control group
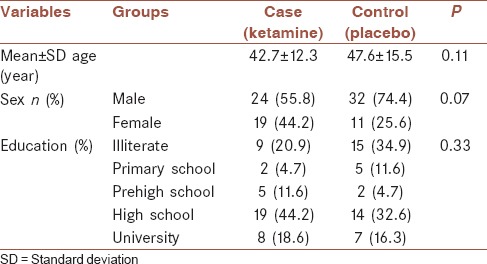
Table 2 shows that the mean number of pain severity and discomfort during endoscopy were 2.4 ± 1.8 and 5.81 ± 1.48 in case and control groups, respectively, which showed significant differences among groups (P < 0.001) [Figure 1].
Table 2.
Distribution of pain and discomfort, endoscopist's satisfaction, sedation score, and retching in case and control groups
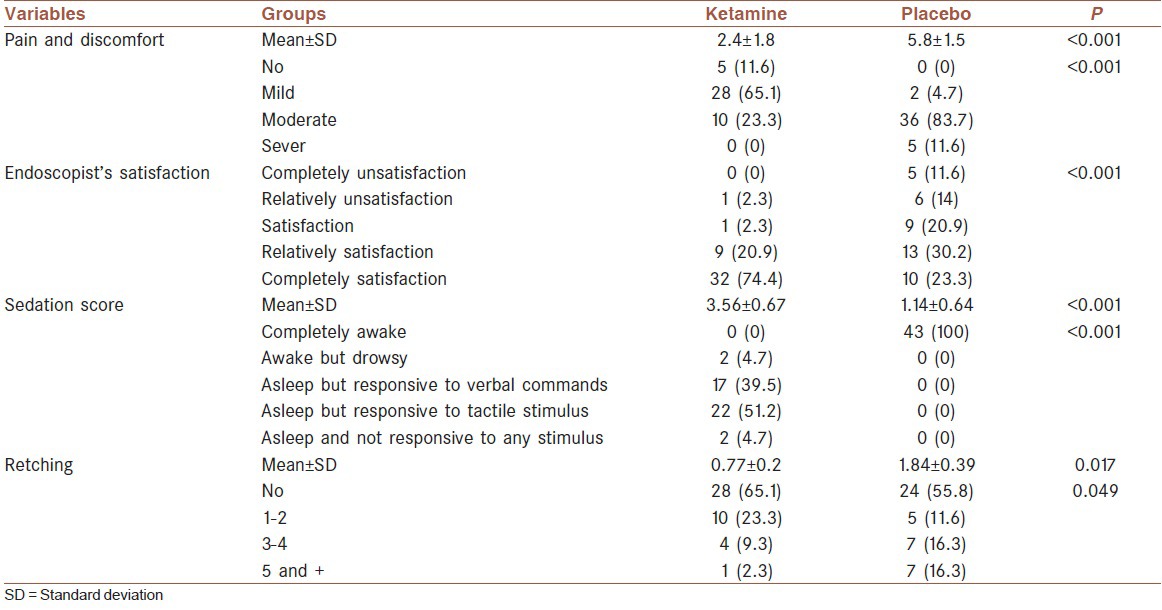
Figure 1.
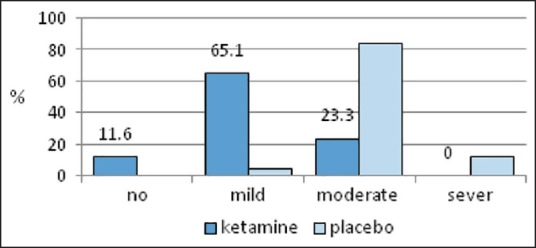
Severity of pain and nausea in case and control groups
As seen in Table 2, none of the patients in the case group had severe nausea and pain otherwise there were five individuals in the control group who had severe nausea and pain. Overall, regarding categorization of pain and nausea in both groups, there was difference among groups. Endoscopist's satisfaction measurement showed that most of the patients in the case group were categorized as “completely satisfaction” (32 patients; 74.4%), but most of the patients in the control group were in “relatively satisfaction” group (13 patients; 30.2%). Mann-Whitney test revealed statistical difference among groups about physician's satisfaction of sedation during endoscopy (P < 0.001) [Figure 2].
Figure 2.
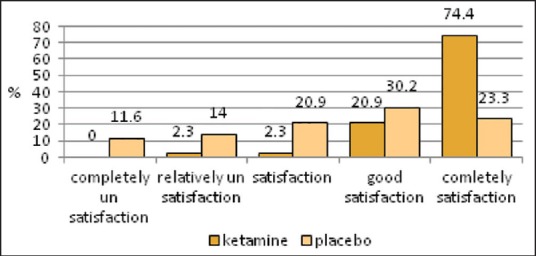
Endoscopist's satisfaction of sedation during endoscopy in case and control groups
The sedation score was assessed in both groups, and patients who received ketamine had better sedative status (Mann-Whitney test; P < 0.001). None of the patients in the case group was completely awake, but all of the patients in the control group were awake. The number of retching during endoscopy showed that individuals in the control group had more frequent retching episodes [Table 2].
Fifteen patients in the case group showed complications including nausea (four patients), nausea and vomiting (three patients), tachycardia (six patients), and deep sedation (one patient). One patient in the control group had severe nausea. Ketamine-induced sedation had more complications in comparison with those administered with placebo (P < 0.001).
DISCUSSION
The main goal of this study was to find a response to a question that is whether low-dose oral ketamine administration can ameliorate patients’ pain and discomfort and also increase physicians’ satisfaction during gastro-enteric endoscopy. Our data revealed that low-dose administration of ketamine, 30 min before initiation of the endoscopy, can significantly decrease patient's pain and discomfort. We also found that physicians reported better satisfaction of sedation in patients who received ketamine comparing with those who received placebo.
Studies and experiences suggested that a successful gastro-enteric endoscopy can be done with a moderately potent sedative medication. A previous meta-analysis revealed that a moderate sedation can increase patient and physician's satisfaction. Although propofol is growing to be used as a moderate sedative medication, midazolam plus one opioid is considered as a standardized sedative method.[11]
There are several studies worked on the effect of ketamine on pain reduction[17,18,19,20] and most of them are focused on the intravenous injection of ketamine and its effect on some special pains such as neuropathic pains.[14] Moharari et al. found that injection of 10 cc lidocaine plus 2 cc of ketamine into the urethra can significantly decrease pain during cystoscopy, especially in the first 5 min of the procedure.[15] Another study designed to find a suitable sedative method for pediatric gastro-enteric endoscopy revealed that combination of oral ketamine with intravenous injection of midazolam is a perfect way to decrease pain and induction of sedation; however, further episodes of vomiting were reported due to oral administration of ketamine.[16] Khademi et al. in a 2011 study on 78 pediatric patients showed that peri-tonsillar infiltration of ketamine (0.5 mg/kg) leads to reduced pain and postsurgery vomiting after adenotonsillectomy.[17] Another study on 180 patients aged 18-60 and candidates for cholecystectomy revealed that subcutaneous injection of 2 mg/kg of ketamine or intravenous injection of 1 mg/kg of ketamine 15 min before initiation of the surgery can decrease postsurgery pain.[18] Combination of ketamine (0.25 mg/kg) and meperidine (5 mg) had been shown to have effects on pain reduction and decreased need to opioids after major abdominal surgeries in patients aged 15-60 years.[19] Results of a recent investigation by Shavakhi et al. revealed that sublingual administration of alprazolam resulted in better sedative status, decreased anxiety, and increased patient's satisfaction during endoscopic procedures compared with oral route of administration.[23] Lack of measurement of awaking time and ending time of procedure can be mentioned as our study limitation. As we searched, there was no study which compared the effect of ketamine compared with placebo, so we did not compared the effect of ketamine with other sedative agents.
CONCLUSION
Our data showed that a low-dose oral administration of ketamine could make a suitable sedation for gastro-enteric endoscopy. Patients experienced less pain and less frequent retching and physicians had greater satisfaction of sedation compared with those placebo-treated group. We would like to suggest using ketamine as a suitable medication for the induction of sedation during gastro-endoscopic procedures if there is no contraindication.
Financial support and sponsorship
This study was done by grant of Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
AUTHOR'S CONTRIBUTION
SM contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. AK contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. MK contributed in the conception and design of the work, drafting and revising the draft, and agreed for all aspects of the work. SD contributed in the drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. PA contributed in the conception and design of the work, drafting and revising the draft, and agreed for all aspects of the work. MM and RK contributed in the conception and design of the work and agreed for all aspects of the work.
REFERENCES
- 1.Bell GD. Preparation, premedication, and surveillance. Endoscopy. 2004;36:23–31. doi: 10.1055/s-2004-814117. [DOI] [PubMed] [Google Scholar]
- 2.Cohen LB. Sedation issues in quality colonoscopy. Gastrointest Endosc Clin N Am. 2010;20:615–27. doi: 10.1016/j.giec.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Porostocky P, Chiba N, Colacino P, Sadowski D, Singh H. A survey of sedation practices for colonoscopy in Canada. Can J Gastroenterol. 2011;25:255–60. doi: 10.1155/2011/783706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fanti L, Agostoni M, Gemma M, Radaelli F, Conigliaro R, Beretta L, et al. Sedation and monitoring for gastrointestinal endoscopy: A nationwide web survey in Italy. Dig Liver Dis. 2011;43:726–30. doi: 10.1016/j.dld.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Paspatis GA, Manolaraki MM, Tribonias G, Theodoropoulou A, Vardas E, Konstantinidis K, et al. Endoscopic sedation in Greece: Results from a nationwide survey for the Hellenic Foundation of gastroenterology and nutrition. Dig Liver Dis. 2009;41:807–11. doi: 10.1016/j.dld.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Cohen LB, Wecsler JS, Gaetano JN, Benson AA, Miller KM, Durkalski V, et al. Endoscopic sedation in the United States: Results from a nationwide survey. Am J Gastroenterol. 2006;101:967–74. doi: 10.1111/j.1572-0241.2006.00500.x. [DOI] [PubMed] [Google Scholar]
- 7.Riphaus A, Rabofski M, Wehrmann T. Endoscopic sedation and monitoring practice in Germany: Results from the first nationwide survey. Z Gastroenterol. 2010;48:392–7. doi: 10.1055/s-0028-1109765. [DOI] [PubMed] [Google Scholar]
- 8.Baudet JS, Borque P, Borja E, Alarcón-Fernández O, Sánchez-del-Río A, Campo R, et al. Use of sedation in gastrointestinal endoscopy: A nationwide survey in Spain. Eur J Gastroenterol Hepatol. 2009;21:882–8. doi: 10.1097/MEG.0b013e328314b7ca. [DOI] [PubMed] [Google Scholar]
- 9.Heuss LT, Froehlich F, Beglinger C. Changing patterns of sedation and monitoring practice during endoscopy: Results of a nationwide survey in Switzerland. Endoscopy. 2005;37:161–6. doi: 10.1055/s-2004-826143. [DOI] [PubMed] [Google Scholar]
- 10.London: British Society of Gastroenterology; 2003. Safety and Sedation during Endoscopic Procedures. [Google Scholar]
- 11.Byrne MF, Chiba N, Singh H, Sadowski DC. Clinical Affairs Committee of the Canadian Association of Gastroenterology. Propofol use for sedation during endoscopy in adults: A Canadian Association of Gastroenterology position statement. Can J Gastroenterol. 2008;22:457–9. doi: 10.1155/2008/268320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillman PK. Monoamine oxidase inhibitors, opioid analgesics and serotonin toxicity. Br J Anaesth. 2005;95:434–41. doi: 10.1093/bja/aei210. [DOI] [PubMed] [Google Scholar]
- 13.Gilger MA, Spearman RS, Dietrich CL, Spearman G, Wilsey MJ, Jr, Zayat MN. Safety and effectiveness of ketamine as a sedative agent for pediatric GI endoscopy. Gastrointest Endosc. 2004;59:659–63. doi: 10.1016/s0016-5107(04)00180-4. [DOI] [PubMed] [Google Scholar]
- 14.Amornyotin S, Chalayonnawin W, Kongphlay S. Clinical efficacy of the combination of Propofol and ketamine versus propofol alone for deep sedation for colonoscopy. Eur J Anaesthesiol. 2011;28:30. [Google Scholar]
- 15.Moharari RS, Najafi A, Khajavi MR, Moharari GS, Nikoobakht MR. Intraurethral instillation of ketamine for male rigid cystoscopy. J Endourol. 2010;24:2033–6. doi: 10.1089/end.2010.0193. [DOI] [PubMed] [Google Scholar]
- 16.Motamed F, Aminpour Y, Hashemian H, Soltani AE, Najafi M, Farahmand F. Midazolam-ketamine combination for moderate sedation in upper GI endoscopy. J Pediatr Gastroenterol Nutr. 2012;54:422–6. doi: 10.1097/MPG.0b013e3182323c75. [DOI] [PubMed] [Google Scholar]
- 17.Khademi S, Ghaffarpasand F, Heiran HR, Yavari MJ, Motazedian S, Dehghankhalili M. Intravenous and peritonsillar infiltration of ketamine for postoperative pain after adenotonsillectomy: A randomized placebo-controlled clinical trial. Med Princ Pract. 2011;20:433–7. doi: 10.1159/000327657. [DOI] [PubMed] [Google Scholar]
- 18.Safavi M, Honarmand A, Nematollahy Z. Pre-incisional analgesia with intravenous or subcutaneous infiltration of ketamine reduces postoperative pain in patients after open cholecystectomy: A randomized, double-blind, placebo-controlled study. Pain Med. 2011;12:1418–26. doi: 10.1111/j.1526-4637.2011.01205.x. [DOI] [PubMed] [Google Scholar]
- 19.Nourozi A, Talebi H, Fateh S, Mohammadzadeh A, Eghtesadi-Araghi P, Ahmadi Z, et al. Effect of adding ketamine to pethidine on postoperative pain in patients undergoing major abdominal operations: A double blind randomized controlled trial. Pak J Biol Sci. 2010;13:1214–8. doi: 10.3923/pjbs.2010.1214.1218. [DOI] [PubMed] [Google Scholar]
- 20.Benson AA, Cohen LB, Waye JD, Akhavan A, Aisenberg J. Endoscopic sedation in developing and developed countries. Gut Liver. 2008;2:105–12. doi: 10.5009/gnl.2008.2.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lauven PM. Pharmacology of drugs for conscious sedation. Scand J Gastroenterol Suppl. 1990;179:1–6. doi: 10.3109/00365529009093164. [DOI] [PubMed] [Google Scholar]
- 22.Waring JP, Baron TH, Hirota WK, Goldstein JL, Jacobson BC, Leighton JA, et al. Guidelines for conscious sedation and monitoring during gastrointestinal endoscopy. Gastrointest Endosc. 2003;58:317–22. doi: 10.1067/s0016-5107(03)00001-4. [DOI] [PubMed] [Google Scholar]
- 23.Shavakhi A, Soleiman S, Gholamrezaei A, Khodadoostan M, Shavakhi S, Tahery A, et al. Premedication with sublingual or oral alprazolam in adults undergoing diagnostic upper gastrointestinal endoscopy. Endoscopy. 2014;46:633–9. doi: 10.1055/s-0034-1377305. [DOI] [PubMed] [Google Scholar]


