Abstract
Objectives
To characterise the differences in care seeking behaviour and dispensing outcomes between adults and children purchasing drugs for malaria at retail shops in Nigeria.
Methods
In Nasarawa State, retail drug shops were enumerated and a subset of those stocking antimalarials were selected as study sites and surveyed. Customers exiting shops after purchasing antimalarial drugs were surveyed and tested with a malaria rapid diagnostic test. Sick adults and caregivers accompanying sick children were eligible, but individuals purchasing drugs for a sick person that was not present were excluded. Multivariate regression analysis was used to identify the correlates of care seeking and the quality of interaction at the shop.
Results
Of 737 participants, 80% were adults and 20% were children (under age 18). Caregivers of sick children were more likely to obtain a prescription prior to attending a drug retailer than adults seeking care for themselves and waited a shorter time before seeking care. Caregivers of sick children were also more likely than sick adults to have been asked about symptoms by the retailer, to have been given an examination, and to have purchased an ACT. Fewer than half of respondents had purchased an ACT. Only 14% of adults, but 27% of children were RDT-positive; RDT-positive children were more likely to have had an ACT purchased for them than RDT-positive adults.
Conclusions
Children with suspected malaria tend to receive better care at drug retailers than adults. The degree of overtreatment and prevalence of dispensing non-recommended antimalarials emphasise the need for routine diagnosis before treatment to properly treat both malaria and non-malaria illnesses.
Keywords: care seeking, drug shops, malaria, Nigeria
Introduction
Malaria is a major public health problem in sub-Saharan Africa, constituting 15% of disability-adjusted life years lost [1] and one of the leading causes of avoidable death, especially among children [2]. In Nigeria, malaria is a significant public health problem, incurring costs equal to 1.3% of economic growth per annum for treatment and lost productivity [3]. Among children under five, malaria accounts for 60% of outpatient visits and 30% of hospitalisations [4].
Since April 2001, the World Health Organisation (WHO) has recommended the use of artemisinin-based combination therapies (ACTs) in countries where Plasmodium falciparum (Pf) malaria is resistant to chloroquine, sulphadoxine-pyrimethamine, and amodiaquine [5]. Nigeria's national guidelines were amended in 2005 to recommend ACTs as the standard first-line treatment for uncomplicated malaria [6]. To prevent or delay the development of Pf resistance to ACTs, researchers encourage rational use of the drug by ensuring parasitological confirmation of all suspected cases of malaria via microscopy [7,8]. In resource-poor settings, rapid diagnostic tests (RDTs) are as a simple and cost-effective alternative for early diagnosis and prompt treatment of malaria when quality-assured microscopy is unavailable [9,10]. According to the latest national guidelines for malaria case management in Nigeria, ‘prompt parasitological confirmation by microscopy or RDTs is recommended in all patients suspected of malaria before treatment’ [[11], pg xiii]. However, access to diagnosis is limited by shortages of trained microscopists and reliable equipment [12] and RDTs are not yet widely available in Nigeria [13].
As a result, individuals seeking care for malaria at retail drug shops are usually presumptively treated [14]. Drug retailers are the first source of care for 77% of children with febrile illnesses [15], and for 35–55% of adults with suspected malaria [16,17]. Recognising the role of retailers in ensuring equitable access to essential medicines, Nigeria, like a number of other countries, permits the two major categories of retailer – pharmacies and proprietary and patent medicine vendors (PPMVs) – to sell a range of antimalarial drugs, including ACTs [18]. Yet, drug retailers are not authorised to use or sell RDTs under current policy [19–21].
Although both types of retailers lack of diagnostic capability, there are important differences that may affect the quality of care they provide [14]. Pharmacies must have a trained pharmacist as either the owner or the staff of the outlet and are permitted to sell a range of medicines, including prescription drugs; some pharmacy shops also employ untrained personnel as sales staff [16]. PPMVs are only permitted to sell pre-packaged, over-the-counter medicines, and licensees are required to be at least 21 years of age and must submit the names of two referees [22]. PPMVs typically do not undergo formal medical training; by convention, the minimum educational requirement is primary school [22] and most complete an apprenticeship with a more senior PPMV [23,24].
There are concerns over the quality of malaria drug dispensing among retailers in Nigeria [25,14,24]. Quality issues may include the dispensing of inappropriate or ineffective drugs [26,16], dispensing of inadequate doses [27,28] and poor communication of drug information to clients [22,29,30]. Furthermore, quality of care is partly a function of appropriate diagnosis [30], and the lack of diagnostics in the retail sector contributes to presumptive treatment of malaria [14]. However, few of the studies that have highlighted concerns over the quality of malaria drug dispensing in the retail sector have measured the extent of overtreatment against actual diagnostic results, relying rather on self-reported fever symptoms.
There has also been little examination of quality of care outcomes among clients of drug retailers by either retailer type or client characteristics. Yet, previous studies show variation in care seeking behaviour based on factors such as perceived severity [21,30], price (including travel and time costs of seeking treatment), income, information about appropriate treatment and the difficulties patients have in assessing the quality of treatment they receive [16]. Among caregivers of children under the age of five, low awareness of the cause of malaria [31], higher risks for malaria among children, and inappropriate treatment with leftover medicines or non-ACTs [32,33] may also contribute to delayed care seeking for the child. Poor knowledge of the causes and signs and symptoms of malaria has also been documented among adults [34,35], which may also contribute to inappropriate care seeking [14,36].
The aim of this paper is to characterise the differences between malaria care received by adults and children at retail shops. We do this by investigating two sets of outcomes: (i) care seeking behaviour in terms of time waited before seeking care, whether or not the customer obtained a prescription before attending the retailer, and type of retailer attended; and (ii) the quality of the interaction at the retailer based on whether or not the retailer asked about the symptoms of the sick person, whether or not the retailer performed any type of examination on the sick person, and whether or not an ACT was purchased. The implications of these behavioural and quality differences are then placed into context by juxtaposing them against the actual malaria status of clients as measured by RDT testing.
Methods
Ethical considerations
The Nigerian Health Research Ethical Review Committee (NHREC Approval Number NHREC/01/01/2007-21/09/2013) and the University of California, San Francisco's Committee for Human Research (reference 072086) approved all study protocols.
Study area and sample selection
The study was conducted in Karu Local Government Area of Nasarawa State in the North Central geopolitical zone of Nigeria. Located along the main road from the nearby capital city, Abuja, the string of communities in Karu is densely populated and growing fast due to a vibrant commercial scene that attracts many migrants [37]. At US$1,481, Nasarawa ranks 21st among Nigeria's 36 states and the Federal Capital Territory in terms of per capita gross domestic product [38]. Like much of Nigeria, malaria transmission in Nasarawa is stable, with an entomological inoculation rate of about 10 per year [39].
In August–September 2013, all drug shops in Karu were enumerated, producing a complete listing of 747 shops: 569 PPMVs and 178 pharmacies. From this list, 147 shops were deemed more eligible for participation in the study because they stocked a larger variety of antimalarial drugs (not limited to ACTs) and hence were more likely to receive customers seeking care for malaria. A second in-person visit to each of these shops was conducted to visually assess customer traffic and the volume of drug sales relative to non-drug sales at peak business hours, from 3 to 8 pm when most customers stop in on their way to home from work. Thirty shops (10 pharmacies, 20 PPMVs) in which no drug sales were observed to have taken place during peak business hours were eliminated, leaving 117 eligible shops. Survey interviewers visited all remaining eligible shops to obtain informed consent from the person in charge at the time. After two PPMV shops declined to participate, 115 shops were enrolled as participant recruitment sites. However, customers were only successfully recruited from 91 shops during the course of the study; customers meeting the eligibility criteria were not found at the remaining 24 shops (seven pharmacies, 17 PPMVs) on the days that surveyors were assigned to recruit at these shops. During the data collection period, two more PPMV shops that had previously given consent to participate requested to end their participation; we excluded all customers (n = 4) interviewed at these shops from the final analysis, which reflects observations from 89 shops (37 pharmacies and 52 PPMVs).
A survey researcher trained on interviewing techniques and performing malaria rapid diagnostic tests (RDTs) was stationed at enrolled shops during the evening commute hours (typically from 3 to 8 pm) on randomly selected days of the week, excluding Sunday. Retailers were not notified in advance of which days surveyors would be present. Surveyors approached customers as they exited the drug store to assess eligibility. The inclusion criteria were as follows: the participant must be a non-pregnant adult having purchased treatment for malaria for him- or herself or an accompanying sick child (child must have been present at the time). Malaria ‘treatment’ was defined as any drug purchased by the customer that she/he intended to take for their current episode of suspected malaria, which may include inappropriate drugs for malaria. While seeking consent, the participant was informed that if they agreed to participate, they would be offered an RDT and would be compensated for their time with a small mobile phone credit of 200 Naira (∼US$1.20) for completing the interview. There was not a minimum sample size target for customer recruitment per shop; the number of data collection days was determined a priori according to budgetary constraints.
Customer survey
After eligibility and informed consent were verified, the participant was offered an RDT and interviewed using a standard questionnaire that captured background socio-demographics, symptoms experienced, and care seeking actions taken for the current episode of suspected malaria. At the end of the survey, the participant was provided with the result of his or her test. Surveyors provided participants with standard advice according to their RDT results. If the participant tested positive for malaria, he/she was told that the positive result indicated the presence of malaria. To ensure that RDT-positive individuals had a quality-assured antimalarial drug, a free course of ACTs was provided along with dosing instructions. If the test was negative, the participant was told that the negative result indicated the absence of malaria and that antimalarial drugs they purchased were not needed. Regardless of the test result, all participants were referred to local clinics and hospitals where they could seek care if their condition was not malaria, or if their illness became worse. Interviews were conducted in English or Hausa (the dominant language of most ethnic groups in the area) by surveyors who were fluent in both languages.
Survey data were independently double-entered into database interface forms using a standardised data dictionary and compared for errors and corrections. A 10% random check was performed to ensure 99.5% data entry accuracy. A second round of quality checks was conducted for all data fields in the codebook to examine outliers and miscodes on an individual case-by-case basis. Where discrepancies were found, data inputs were cross-checked with the original paper survey for final reconciliation. All indeterminate cases were coded to missing.
Care seeking behaviour
We operationalised the care seeking behaviour of customers attending a retail drug shop through three measures: (i) time waited before seeking care, (ii) whether or not the customer obtained a prescription before attending the retailer and (iii) type of retailer attended. The type of retailer attended is a binary variable for attending a PPMV rather than a pharmacy. Customers were coded as having obtained a prescription if they reported that a formally trained provider (i.e. doctor, nurse or community health extension worker)1 other than a retailer chose the antimalarial that they purchased at the shop. Time waited before seeking care is an ordinal variable reflecting how many days the sick person waited before seeking care at any source for the same illness incident for which drugs were being purchased: less than a day (0 days), 1, 2, 3, or 4 or more days.
Shop interaction and dispensing outcomes
The second set of outcomes pertains to the quality of care customers received at the retailer they attended, as reported by the customer. We measure the quality of the interaction through two binary variables indicating (i) whether or not the retailer asked about the symptoms of the sick person and (ii) whether or not the retailer performed any type of examination on the sick person. ‘Examination’ was left open to the customer to define and could therefore include anything from checking eye colour or blood pressure to performing an RDT. Additionally, we measure proper dispensing as a binary indicator of whether or not the customer purchased an ACT (verified by the surveyor). Note that all of the retail shops included in the study stocked ACTs at the time of enumeration.
Statistical analysis
To assess bivariate differences between adults seeking care for themselves and caregivers seeking care for a sick child, we conduct statistical significance tests using bivariate logistic regressions for all categorical and dummy variables (with standard errors clustered by site to adjust for autocorrelation among shop patrons) and Kruskal–Wallis nonparametric tests for continuous variables. The same procedure was used to test for differences between PPMVs and pharmacies on shop-level characteristics. Multivariate analyses for all outcome variables were performed using logistic regression, with the exception of wait time for which an ordered logit model was used. Our main independent variable of interest is whether the sick person for whom antimalarials were being purchased was a child below age 18 or an adult age 18 or older (18 is the legal age of maturity in Nigeria). Thus, three observations with missing age information were excluded from all analyses.
Additional covariates for respondent and household characteristics and the current illness incident are included in multivariate regressions. Respondent characteristics include gender, age, religion (Muslim or Christian), employment status, and highest educational attainment. Household characteristics include asset wealth index quintiles (constructed following standard approaches; see [40]. The location of the shop (rural, urban, or peri-urban) was also controlled for. The illness was coded as severe if the respondent reported that the illness was affecting the sick person's ability to carry out normal daily activities. We also included a binary indicator for home treatment if the participant reported that the sick person took any drugs or herbal remedies prior to attending the retailer.
For the multivariate analyses of shop interaction and ACT dispensing, we also included the type of retail location (PPMV or pharmacy) as a covariate because previous studies have found that antimalarial dispensing outcomes differ between them [14,19,16,20]. In the model for ACT dispensing, we also include an indicator for whether the customer reported having chosen the particular type of antimalarial purchased, because literature suggests that much retail drug dispensing in Nigeria is driven by customer demand [13,41,24].
Drugs purchased, the total cost of drugs purchased, and results of the RDTs are further descriptively analysed comparing adults with children and PPMVs with pharmacy outlets. The total cost of drugs reflects self-reported total expenditure on all drugs purchased at the shop and not necessarily the cost of antimalarial drugs alone.
Results
Sample characteristics
Panel A in Table 1 describes the characteristics of the 737 participants, including 586 adults and 151 children (age under 18). A higher percentage of sick adults seeking care for themselves were male (64.6%), employed (73.5%), and had secondary education or more (82.2%) compared to caregivers of sick children who were more often female (72.2%), not currently employed (51.0%), and less educated (69.5% with secondary education or more). A greater percentage of sick children were from the lower two wealth quintiles (49.0%) and recruited in rural areas (28.5%) than sick adults (37.7% and 17.2%, respectively). The mean age of sick children was about 5 years. Compared to sick adults, significantly more caregivers of sick children reported a severe illness (60.3% vs. 42.1%) and that they treated at home first before coming to the drug shop (62.9% vs. 49.1%). Only 18.7% of participants reported that they had chosen the drugs purchased, spending an average of 425 Naira (∼USD2.65).
Table 1.
Characteristics of customer and retail shop observations
| Total |
Sick adult |
Caregiver of sick child |
|||||
|---|---|---|---|---|---|---|---|
| Panel A: Customer observations | Mean | SD | Mean | SD | Mean | SD | Diff† |
| Respondent characteristics | |||||||
| Male | 0.570 | 0.646 | 0.278 | *** | |||
| Age (mean years) | 32.6 | 9.6 | 32.5 | 9.8 | 33.0 | 8.7 | |
| Muslim | 0.152 | 0.152 | 0.152 | ||||
| Employed | 0.685 | 0.735 | 0.490 | *** | |||
| Education | *** | ||||||
| Less than secondary | 0.204 | 0.178 | 0.305 | ||||
| Secondary | 0.444 | 0.432 | 0.490 | ||||
| University and above | 0.352 | 0.390 | 0.205 | ||||
| Household wealth | * | ||||||
| Quintile 1 (poorest) | 0.198 | 0.186 | 0.245 | ||||
| Quintile 2 | 0.202 | 0.191 | 0.245 | ||||
| Quintile 3 | 0.201 | 0.201 | 0.199 | ||||
| Quintile 4 | 0.201 | 0.203 | 0.192 | ||||
| Quintile 5 (richest) | 0.198 | 0.218 | 0.119 | ||||
| Child characteristics | |||||||
| Child age (mean years) | 5.0 | 4.3 | |||||
| Male child | 0.547 | ||||||
| Illness incident | |||||||
| Severe illness | 0.458 | 0.421 | 0.603 | *** | |||
| Home treatment | 0.520 | 0.491 | 0.629 | *** | |||
| Drug choice | |||||||
| Customer chose drug | 0.187 | 0.198 | 0.145 | ||||
| Mean cost of drugs (Naira) | 425 | 474 | 416 | 495 | 461 | 374 | *** |
| Care seeking behaviour | |||||||
| Attended a PPMV (vs. pharmacy) | 0.536 | 0.510 | 0.636 | ** | |||
| Obtained prescription from a health provider‡ | 0.071 | 0.059 | 0.117 | ** | |||
| Days waited (mean) | 2.21 | 2.29 | 1.88 | *** | |||
| 0 | 0.148 | 0.137 | 0.192 | ||||
| 1 | 0.283 | 0.264 | 0.358 | ||||
| 2 | 0.113 | 0.118 | 0.093 | ||||
| 3 | 0.124 | 0.132 | 0.093 | ||||
| 4+ | 0.332 | 0.349 | 0.265 | ||||
| Location of shop attended | |||||||
| Urban | 0.431 | 0.445 | 0.377 | ||||
| Peri-urban | 0.373 | 0.382 | 0.338 | ||||
| Rural | 0.195 | 0.172 | 0.285 | ||||
| Interaction at the shop | |||||||
| Asked symptoms | 0.849 | 0.822 | 0.954 | *** | |||
| Did examination | 0.170 | 0.150 | 0.247 | ** | |||
| Bought ACT | 0.457 | 0.401 | 0.675 | *** | |||
| Bought sulphadoxine–pyrimethamine | 0.346 | 0.410 | 0.099 | *** | |||
| Bought an artemisinin monotherapy | 0.068 | 0.073 | 0.046 | ||||
| Bought chloroquine | 0.046 | 0.034 | 0.093 | ** | |||
| Bought only non-antimalarial | 0.091 | 0.089 | 0.099 | ||||
| N | 737 | 586 | 151 | ||||
| Total |
PPMV |
Pharmacy |
|||||
|---|---|---|---|---|---|---|---|
| Panel B: Retail shop observations | Mean | SD | Mean | SD | Mean | SD | Diff† |
| Shop location | |||||||
| Urban | 0.404 | 0.308 | 0.541 | ||||
| Peri-urban | 0.416 | 0.442 | 0.378 | ||||
| Rural | 0.180 | 0.250 | 0.081 | ||||
| Staffing | |||||||
| Years in business | 4.7 | 4.4 | 5.1 | 4.3 | 4.1 | 4.5 | *** |
| Number of workers | 2.9 | 1.7 | 2.0 | 0.9 | 4.2 | 1.8 | *** |
| At least one worker with formal health training§ | 0.663 | 0.500 | 0.892 | *** | |||
| Any staff attended training in last year | 0.565 | 0.608 | 0.500 | *** | |||
| Participates in social marketing distribution | 0.092 | 0.039 | 0.167 | *** | |||
| Malaria diagnostics | |||||||
| Sells RDTs | 0.112 | 0.058 | 0.189 | *** | |||
| Performs RDTs | 0.090 | 0.077 | 0.108 | ||||
| N | 89 | 52 | 37 | ||||
Significance tests conducted using bivariate logistic regressions for all categorical and dummy variables (with standard errors clustered by site to adjust for autocorrelation among shop patrons) and Kruskal–wallis nonparametric tests for continuous variables.
Defined as a doctor, nurse, or community health extension workers.
Defined as a doctor, nurse, community health extension worker, pharmacist or laboratory technician.
P < 0.01,
P < 0.05,
P < 0.1.
Sample characteristics of the 89 shops participating as recruitment sites are presented in Panel B. PPMV shops, on average, had been operating 1 year longer than pharmacies. Pharmacies were larger, employing 4.2 workers on average, compared to 2.0 workers for PPMVs. Nearly 90% of pharmacies employed at least one worker with formal health training (which included trained pharmacists, as well as doctors, nurses, community health extension workers, and laboratory technicians) compared to only 50% of PPMV shops, but PPMV shops were more likely to have had a staff member attend a training in the past year (60.8%) than pharmacies (50.0%). Only 9.2% of all shops were participating in social marketing distribution programmes, which are typically operated by local non-governmental organisations for family planning products and antimalarial drugs. A larger percentage of pharmacies (18.9%) than PPMVs (5.8%) reported that they sold malaria RDTs, but fewer than 10% of participating retailers reported that they performed RDTs (which is not permitted under the scope of practice for either PPMVs or pharmacies).
Care seeking behaviour
Table 1 also shows that caregivers of sick children are significantly more likely to seek care for suspected malaria at a PPMV, rather than a pharmacy, compared to sick adults (63.6% and 51.0% respectively) in unadjusted analysis. Multivariate logistic regression results displayed in Table 2 indicate that this difference becomes insignificant once additional controls are added. However, respondents with university education or more (OR = 0.346; 95% CI 0.197–0.612) and who reside in a household in the highest two wealth strata (quintile 4 OR = 0.478; 95% CI 0.262–0.871; quintile 5 OR = 0.424; 95% CI 0.225–0.801) are the least likely to patronise a PPMV shop. In contrast, careseekers attending peri-urban shops (OR = 3.568; 95% CI 1.098–11.594) are over three times as likely to attend a PPMV than those of residents in urban areas; those attending rural shops are more than six times as likely to go to a PPMV rather than a pharmacy, but this estimate is only marginally significant at the 10% level.
Table 2.
Logistic regression results predicting days waited before seeking care, obtaining a prescription before purchasing drugs, and attending a PPMV shop in Nasarawa, Nigeria, 2013 (adjusted odds-ratios reported)
| PPMV | Prescription | Days waited† | |
|---|---|---|---|
| Sick child | 1.195 [0.702–2.036] | 2.051* [0.963–4.366] | 0.531*** [0.362–0.779] |
| Respondent male | 0.997 [0.618–1.607] | 0.521** [0.304–0.893] | 0.815 [0.615–1.080] |
| Respondent age | 0.997 [0.978–1.017] | 1.022 [0.993–1.052] | 0.994 [0.978–1.011] |
| Muslim | 1.025 [0.539–1.949] | 0.543 [0.223–1.325] | 0.654** [0.438–0.977] |
| Employed | 0.896 [0.530–1.514] | 1.770 [0.825–3.795] | 1.320 [0.926–1.882] |
| Secondary school | 0.693 [0.401–1.200] | 1.289 [0.625–2.658] | 0.837 [0.576–1.218] |
| University & above | 0.346*** [0.196–0.612] | 1.055 [0.399–2.791] | 0.832 [0.539–1.283] |
| Wealth quintile 2 | 0.908 [0.479–1.723] | 0.928 [0.390–2.206] | 0.595** [0.355–0.999] |
| Wealth quintile 3 | 0.561* [0.306–1.027] | 0.533 [0.211–1.342] | 0.575** [0.336–0.983] |
| Wealth quintile 4 | 0.478** [0.262–0.871] | 0.610 [0.246–1.509] | 0.860 [0.502–1.474] |
| Wealth quintile 5 | 0.424*** [0.225–0.801] | 1.135 [0.464–2.773] | 0.815 [0.461–1.441] |
| Peri-urban | 3.568** [1.098–11.594] | 0.685 [0.316–1.487] | 0.979 [0.684–1.401] |
| Rural | 6.189* [0.921–41.609] | 0.048*** [0.006–0.355] | 0.702 [0.457–1.078] |
| Illness severe | 1.335 [0.842–2.115] | 1.346 [0.758–2.392] | 1.359** [1.029–1.795] |
| Home treatment | 1.015 [0.685–1.506] | 2.298** [1.130–4.670] | 2.327*** [1.714–3.159] |
| Constant cut1 | 0.113*** [0.054–0.236] | ||
| Constant cut2 | 0.575 [0.291–1.136] | ||
| Constant cut3 | 0.957 [0.484–1.892] | ||
| Constant cut4 | 1.701 [0.844–3.431] | ||
| Constant | 1.377 [0.384–4.940] | 0.025*** [0.005–0.126] | |
| Observations | 731 | 716 | 729 |
Robust standard errors clustered by shop.
95% confidence intervals in brackets.
Estimated with an ordered logistic regression.
P < 0.01,
P < 0.05,
P < 0.1.
Although only 7.1% of sick individuals obtained a prescription prior to coming to the shop (see Table 1), caregivers of sick children were more likely to do so than sick adults (11.9% and 5.9%, respectively). However, this difference is only marginally significant once controls are added (see Table 2). Male participants were half as likely to obtain a prescription (OR = 0.521; 95% CI 0.304–0.893) and those attending rural shops were the least likely of all (OR = 0.048; 95% CI 0.006–0.355) to obtain a prescription. Participants who had treated at home prior to coming to the shop were more than twice as likely to have obtained a prescription (OR = 2.298; 95% CI 1.130–4.670).
On average, caregivers of sick children waited about half a day less (1.9 days) before seeking care than adults (2.3 days), and this difference remained significant in multivariate analysis (OR = 0.531; 95% CI 0.362–0.779). Muslim participants (OR = 0.654; 95% CI 0.438–0.977) and those in wealth quintiles 2 (OR = 0.595; 95% CI 0.355–0.999) and 3 (OR = 0.575; 95% CI 0.336–0.983) waited for a significantly shorter time than Christian and wealthier participants. Individuals experiencing a severe illness (OR = 1.359; 95% CI 1.029–1.795) and those who had already treated themselves at home (OR = 2.327; 95% CI 1.714–3.159) waited significantly longer before seeking care.
Interaction at the shop and dispensing outcomes
In unadjusted analysis (Table 1), caregivers seeking care for a child were more likely to report that the retailer asked about symptoms experienced (95.4%) than adults seeking care for themselves (82.2%). After regression adjustment (Table 3), caregivers of sick children were still more than three times as likely to have been asked about symptoms (OR = 3.259; 95% CI 1.457–7.291). In addition, participants at PPMVs were nearly three times as likely as those at pharmacies to have been asked about symptoms (OR = 2.708; 95% CI 1.416–5.177).
Table 3.
Logistic regression predicting if customers were asked about their symptoms, had any type of examination of the sick person, or purchased an ACT at drug retail shops in Nasarawa, Nigeria, 2013 (adjusted odds ratios reported)
| Asked symptoms | Had examination | Bought ACT | |
|---|---|---|---|
| Sick child | 3.259*** [1.457–7.291] | 2.076** [1.102–3.908] | 3.912*** [2.608–5.866] |
| Respondent male | 0.764 [0.502–1.163] | 1.189 [0.689–2.051] | 1.259 [0.887–1.787] |
| Respondent age | 0.979* [0.956–1.003] | 0.980 [0.949–1.013] | 1.001 [0.982–1.019] |
| Muslim | 1.029 [0.546–1.939] | 0.963 [0.497–1.863] | 0.686 [0.408–1.153] |
| Employed | 0.675 [0.415–1.098] | 0.220*** [0.139–0.348] | 1.008 [0.664–1.530] |
| Secondary school | 0.854 [0.447–1.634] | 0.930 [0.430–2.011] | 1.017 [0.626–1.654] |
| University & above | 0.635[0.328–1.228] | 1.537 [0.662–3.570] | 1.057 [0.650–1.719] |
| Wealth quintile 2 | 0.785 [0.402–1.536] | 1.752 [0.775–3.962] | 1.253 [0.743–2.114] |
| Wealth quintile 3 | 1.302 [0.629–2.698] | 2.340** [1.011–5.413] | 0.916 [0.485–1.728] |
| Wealth quintile 4 | 1.126 [0.578–2.193] | 1.426 [0.564–3.608] | 0.908 [0.539–1.527] |
| Wealth quintile 5 | 1.026 [0.523–2.012] | 1.445 [0.634–3.290] | 1.576 [0.894–2.776] |
| Peri-urban | 1.376 [0.796–2.377] | 1.517 [0.742–3.104] | 0.864 [0.551–1.353] |
| Rural | 1.544 [0.505–4.726] | 3.194 [0.927–11.002] | 0.704 [0.397–1.249] |
| Illness severe | 0.949 [0.616–1.463] | 0.379*** [0.240–0.599] | 1.201 [0.885–1.629] |
| Home treatment | 0.992 [0.614–1.603] | 0.610** [0.378–0.984] | 0.913 [0.641–1.301] |
| PPMV | 2.708*** [1.416–5.177] | 0.608 [0.278–1.330] | 0.580*** [0.384–0.876] |
| Customer chose drug | 0.432*** [0.282–0.661] | ||
| Constant | 10.742*** [3.298–34.984] | 0.593 [0.172–2.038] | 0.852 [0.358–2.028] |
| Observations | 730 | 729 | 716 |
Robust standard errors clustered by shop.
95% confidence interval in brackets.
P < 0.01,
P < 0.05,
P < 0.1.
Sick children were also twice as likely to have been examined by the retailer than sick adults (OR = 2.076; 95% CI 1.102–3.908). Employed participants (OR = 0.220; 0.139–0.348), those perceiving a severe illness (OR = 0.379; 95% CI 0.240–0.599), and those that had previously treated themselves at home (OR = 0.610; 95% CI 0.378–0.984) were significantly less likely to have been examined. Individuals in the middle wealth quintile were twice as likely to have been examined (OR = 2.340; 95% CI 1.011–5.413). Residents in rural areas were three times more likely to receive an examination, but this estimate was only marginally significant.
Compared to sick adults, caregivers of sick children were nearly four times as likely to have purchased an ACT (OR = 3.912; 95% CI 2.608–5.866). Participants at PPMV shops (OR = 0.580; 95% CI 0.384–0.876) and those who had chosen the drug themselves (OR = 0.432; 95% CI 0.282–0.661) were significantly less likely to have purchased an ACT. A substantial portion of respondents also purchased non-ACT antimalarials or only drugs that are not antimalarials (Table 1). Sick adults were significantly more likely to have purchased sulphadoxine–pyrimethamine2 (41.0%) than caregivers of sick children (9.9%), but caregivers were more likely to have purchased chloroquine (9.3%, compared to 3.4% for adults). About 9% of all participants purchased only drugs that are not antimalarials (primarily paracetamol, antibiotics, vitamins and supplements; data not shown).
Differences in drug purchases between adults and children correspond to differences in amount spent. On average, individuals buying ACTs paid more than those buying other types of antimalarials (see Figure1). For sick adults, those buying at pharmacies paid significantly more than those buying at PPMVs, regardless of whether an ACT was purchased or not. Similarly, for customers attending PPMV shops, more was spent on drugs for children than adults, regardless of whether an ACT was purchased or not.
Figure 1.
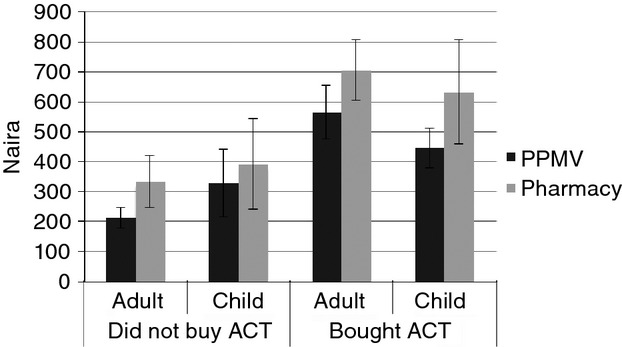
Average amount spent by ACT purchase, sick adult or child, and type of retailer. 1 USD = ∼160 Naira (at the time of the study).
RDT results
Overall, 16.7% of participants tested positive for malaria according to RDTs – 14.0% of adults and 27.3% of children (Table 4). Significantly more sick children at PPMVs (34.7%) were RDT-positive than those going to a pharmacy (14.5%) (P < 0.001). Among RDT-positive individuals, 70.7% of caregivers of sick children compared to 43.9% of adults had purchased an ACT (P < 0.001).
Table 4.
RDT positivity among sick children and adults and percentage of RDT-positives who purchased an ACT, by retailer type, Nasarawa, Nigeria, 2013
| Location of purchase | Purchasing for | Percentage RDT-positives | 95% CI | Percentage of RDT-positives who purchased an ACT | 95% CI | ||
|---|---|---|---|---|---|---|---|
| PPMV | Adult | 17.1 | 12.8 | 21.3 | 39.2 | 25.8 | 53.9 |
| Child | 34.7 | 25.0 | 44.5 | 69.7 | 51.3 | 84.4 | |
| Total | 21.3 | 17.3 | 25.4 | 51.2 | 40.0 | 62.3 | |
| Pharmacy | Adult | 10.8 | 7.2 | 14.5 | 75.0 | 34.9 | 96.8 |
| Child | 14.5 | 4.9 | 24.2 | 51.6 | 33.1 | 69.8 | |
| Total | 11.4 | 8.0 | 14.8 | 56.4 | 39.6 | 72.2 | |
| Full sample | Adult | 14.0 | 11.2 | 16.8 | 43.9 | 33.0 | 55.3 |
| Child | 27.3 | 20.1 | 34.5 | 70.7 | 54.5 | 83.9 | |
| Total | 16.7 | 14.0 | 19.4 | 53.8 | 43.6 | 61.9 | |
Discussion
Effective management of malaria requires that adults and caregivers of sick children have access to appropriate and affordable treatment and initiate treatment within 24 h of the onset of symptoms [42]. Our results show that, compared to adults, caregivers of sick children waited a significantly shorter time before seeking care (but still more than the recommended 24 h) and were also somewhat more likely to obtain a prescription prior to purchasing drugs. While at the drug shop, sick children were more likely to have been asked about symptoms, been examined, and purchased an ACT than sick adults. This suggests that sick children are more likely to receive better care than adults, which may be attributable to higher perceived risk of infection in this age group [43]. A study conducted in northern Nigeria similarly found that 75% of PPMVs studied examined the sick children who presented at their shops [25].
We also find that home treatment more than doubles the delay in care seeking. Home management of illnesses is common in many malaria-endemic countries, including tepid sponging, using leftover medications and herbs, and if the condition does not improve, then care from a provider is sought [30]. Even though home management is associated with a higher likelihood of obtaining a prescription prior to attending the drug shop, the overall percentage of individuals having a prescription is low (only 7%). This corroborates evidence from multiple studies showing little demand for obtaining a diagnosis and prescription from a healthcare provider before initiating treatment for malaria or other illnesses [44,22,45,29,24].
Even though the results of this and other studies [46,14,30] show that lower socio-economic and rural populations are more likely to seek care from PPMVs who may offer lower quality care than pharmacies, our results also suggest that some aspects of service provision may be comparatively better at PPMVs. Staff of PPMV shops were nearly three times as likely to ask participants about their symptoms as those of pharmacies. Differential customer bases may account for this difference; pharmacies, which are typically located in urban hubs, may receive higher customer volumes and therefore provide less personalised attention to medical concerns compared to PPMVs which are more likely to be located in rural areas, and may have fewer customers and potentially more time to attend to their needs. Although this study was not designed to assess differential customer volumes, our retail shop enumeration revealed that 83% of pharmacies were located in urban hubs vs. only 42% of PPMV shops (data not shown) and that participating pharmacies employed more workers, suggesting larger sales volumes.
However, this result is tempered by the finding that participants at PPMV shops were less likely to have purchased ACTs than those attending pharmacies, even after controlling for the fact that their customers are more rural and poorer. Both types of retailers continue to sell non-recommended antimalarials, but the practice is more common among PPMVs, corroborating previous findings [14]. While the use of ineffective antimalarials risks lack of illness recovery, 6.8% of customers also purchased an artemisinin-based monotherapy, which risks fuelling drug resistance.
Substandard drug dispensing may partially be explained by strong customer demand for inappropriate treatments [44,22,45,41,24]. In this study, only 18.6% of participants chose their drugs themselves, but those who did so were less likely to buy an ACT. This may be related to the higher cost of ACTs compared with other antimalarials. Although subsidies via the Affordable Medicines Facility-malaria (AMFm)3 mechanism have made ACTs available at USD1.40 in 2011, the price for an adult-equivalent dose of chloroquine was USD0.27 and for sulphadoxine–pyrimethamine USD0.45 [13]. As expected, customers in this study who purchased ACTs spent more than those who did not, regardless of retailer type.4 Poor knowledge among providers may also contribute to improper dispensing [13], especially among PPMVs for whom health training is not required and who are less likely to employ someone with a health certification. Thus, continued attention to both provider and customer behaviour change is needed to improve adherence to treatment guidelines.
Several limitations to this study should be noted. Measuring the quality of care is difficult, and participant exit interviews may be subject to recall bias. Drug costs are self-reported and reflect the total amount of all drugs purchased; the cost of antimalarials alone cannot be separated for individuals who purchased multiple products, and we cannot determine with accuracy whether or not individuals purchased full or partial dosages. Even though a complete census of all potential shops in our study area was carried out, the recruitment sites were chosen purposefully to target areas where larger volumes of malaria treatment were occurring at shops that stocked some type of antimalarial drug at the time of enumeration. Thus, shops were not randomly selected and are not representative of drug shops in Karu. Further, their customers are not necessarily representative of the local population, and individuals purchasing for others who did not take the sick person or child to the shop with them were also excluded. The care seeking behaviours analysed from this sample may not reflect behaviours of more marginalised populations that do not patronise shops that carry antimalarials, and extremely sick people who may not have been brought to the shop. To the authors' knowledge, the distribution of AMFm-subsidised ACTs was the only malaria intervention operating in Nasarawa state at the time of the study, which included some of the participating drug shops (9.2% as reported in Table 1); while these activities may have influenced shop enrolment, it is less likely that customer exit interview participation was influenced.
These limitations notwithstanding, our results indicate that the extent of overtreatment for malaria was high for both adults and children in the study area; only 14.0% of adults and 27.2% of children were RDT-positive (16.7% in total), which is in line with several previous studies. A study among pharmacy customers nearby in the nation's capital, Abuja, found that only 13.6% of careseekers were RDT-positive [47]. In southwest Oyo State, 32.1% of febrile children brought to a tertiary hospital were RDT-positive [48]. However, in the same area, only 3.9% of participants purchasing antimalarial drugs at retail drug shops were RDT-positive [14]. Introducing malaria diagnosis, such as RDTs, at the first point of care for management of fever and other malaria-related symptoms [49,42] will not only improve the rational use of ACTs [50,51], but also increase the quality of care for both malaria and non-malaria febrile illnesses. However, current restrictions on the scope of practice for drug retailers prohibit the sale or conduct of invasive diagnostic tests, including RDTs [18,52]. Given that most customers of drug retailers do not seek formal diagnosis or a prescription before purchasing drugs, it is unlikely that the rational use of ACTs will improve without policy change to increase access to malaria diagnosis at these points of care. Due to the higher percentage of RDT-positives among sick children attending PPMVs (34.7%), and given the disproportionate presence of PPMV shops in rural areas, increasing access to diagnostic testing at these outlets is especially important for malaria case management among children.
Acknowledgments
We acknowledge ExxonMobil for financial support of this study. Our appreciation also goes to survey data collectors and management staff, including Eric Schatzkin, Erikan Obotetukudo, Adetunji Ilori, and Emmaneul Omotoyinbo.
Footnotes
No customers reported obtaining a diagnosis or prescription from a lab technician.
Sulfadoxine-pyrimethamine is recommended for malaria prophylaxis in pregnant women, but pregnant women were excluded from this study.
At the time of this study, the AMFm program was the only ACT subsidy in Nigeria, distributing to the general population through public and private sector facilities and retail outlets.
In this study, because drug expenditure amounts reported by participants also include non-antimalarial drugs (e.g. paracetamol, vitamins, supplements, and antibiotics) that may have additionally been purchased, we cannot separately report the cost of only ACTs.
References
- 1.Institute for Health Metrics and Evaluation (IHME) 2013. GBD Compare. Seattle, WA IHME, University of Washington, (Available from: http://vizhub.healthdata.org/gbd-compare) [21 January 2015]
- 2.Black RE, Cousens S, Johnson HL, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–1987. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. World Malaria Report: 2013. Geneva, Switzerland: WHO; 2013. [Google Scholar]
- 4.Federal Ministry of Health (FMOH) National Malaria Strategic Plan 2014–2020. Abuja, Nigeria: National Malaria Elimination Programme, Federal Ministry of Health; 2013. [Google Scholar]
- 5.World Health Organization (WHO) 2006. WHO Briefing on Malaria Treatment Guidelines and Artemisinin Monotherapies. Geneva, 19 April. (Available from: http://www.who.int/malaria/publications/atoz/meeting_briefing19april.pdf) [Accessed 21 January 2015]
- 6.Federal Ministry of Health (FMOH) 2005. National Antimalarial Treatment Policy. Abuja, Nigeria Federal Ministry of Health, Federal Republic of Nigeria, (Available from: http://apps.who.int/medicinedocs/documents/s18401en/s18401en.pdf) [17 September 2014]
- 7.Ughasoro MD, Okafor HU, Okoli CC. Malaria diagnosis and treatment amongst health workers in University of Nigeria Teaching Hospital Enugu, Nigeria. Niger J Clin Pract. 2013;16:329–333. doi: 10.4103/1119-3077.113456. [DOI] [PubMed] [Google Scholar]
- 8.Uneke CJ. Concurrent malaria and typhoid fever in the tropics: the diagnostic challenges and public health implications. J Vector Borne Dis. 2008;45:133–142. [PubMed] [Google Scholar]
- 9.Ben-Edet AE, Lesi FE, Mafe AG, Grange AO. Diagnosis of plasmodium falciparum malaria in children using the immuno-chromatographic diagnostic technique. Niger J Paediatr. 2006;31:71–78. [Google Scholar]
- 10.Kattenberg J, Ochodo E, Boer K, et al. Systematic review and meta-analysis: rapid diagnostic tests versus placental histology, microscopy and PCR for malaria in pregnant women. Malar J. 2011;10:321. doi: 10.1186/1475-2875-10-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Federal Ministry of Health (FMOH) National Guidelines for Diagnosis and Treatment of Malaria. Abuja, Nigeria: National Malaria and Vector Control Division, Federal Ministry of Health; 2011. [Google Scholar]
- 12.World Health Organization [WHO] Guidelines for the Treatment of Malaria. 2nd edn. Geneva, Switzerland: WHO; 2010. [PubMed] [Google Scholar]
- 13.ACTwatch Group, SFH/Nigeria and the Independent Evaluation Team. Endline outlet survey report 2011 for the baseline independent evaluation of phase 1 of the affordable medicines facility -malaria (AMFm), Nigeria. Abuja: ACTwatch/SFH/PSI; 2012. [Google Scholar]
- 14.Isiguzo CI, Anyanti J, Ujuju C, et al. Presumptive treatment of malaria from formal and informal drug vendors in Nigeria. PLoS One. 2014;9:e110361. doi: 10.1371/journal.pone.0110361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Population Commission (NPC) [Nigeria] and ICF International. 2014. Nigeria Demographic and Health Survey. Abuja, Nigeria, and Rockville, Maryland. USA: NPC and ICF International; 2013. [Google Scholar]
- 16.Onwujekwe O, Hanson K, Uzochukwu B. Do poor people use poor quality providers? Evidence from the treatment of presumptive malaria in Nigeria. Tropical Med Int Health. 2011;16:1087–1098. doi: 10.1111/j.1365-3156.2011.02821.x. [DOI] [PubMed] [Google Scholar]
- 17.Uguru NP, Onwujekwe OE, Uzochukwu BS, et al. Inequities in incidence, morbidity and expenditures on prevention and treatment of malaria in southeast Nigeria. BMC Int Health Hum Rights. 2009;9:21. doi: 10.1186/1472-698X-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Federal Ministry of Health [FMOH] Essential Medicine List, 5th revision 2010. Abuja, Nigeria: Federal Ministry of Health. Federal Republic of Nigeria; 2010. [Google Scholar]
- 19.Onwujekwe O, Dike N, Uzochukwu B, Ezeoke O. Informal payments for healthcare: differences in expenditures from consumers and providers perspectives for treatment of malaria in Nigeria. Health Policy. 2010;96:72–79. doi: 10.1016/j.healthpol.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 20.Onwujekwe O, Obikeze E, Uzochukwu U, Okoronkwo I. Improving quality of malaria treatment services: assessing inequities in consumers' perceptions and providers' behaviour in Nigeria. Int J Equity Health. 2010;9:22. doi: 10.1186/1475-9276-9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uzochukwu BS, Onwujekwe OE, Okwuosa C, Ibe OP. Patent medicine dealers and irrational use of medicines in children: the economic cost and implications for reducing childhood mortality in Southeast Nigeria. PLoS One. 2014;9:e91667. doi: 10.1371/journal.pone.0091667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brieger WR, Osamor PE, Salami KK, et al. Interactions between patent medicine vendors and customers in urban and rural Nigeria. Health Policy Plan. 2004;19:177–182. doi: 10.1093/heapol/czh021. [DOI] [PubMed] [Google Scholar]
- 23.Berendes S, Adeyemi O, Oladele EA, et al. Are patent medicine vendors effective agents in malaria control? Using lot quality assurance sampling to assess quality of practice in Jigawa, Nigeria. PLoS One. 2012;7:e44775. doi: 10.1371/journal.pone.0044775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okeke TA, Uzochukwu BS, Okafor HU. An in-depth study of patent medicine sellers' perspectives on malaria in a rural Nigerian community. Malar J. 2006;5:97. doi: 10.1186/1475-2875-5-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Akuse RM, Eseigbe EE, Ahmed A, Brieger WR. Patent medicine sellers: how can they help control childhood malaria? Malar Res Treat. 2010;2010:1–7. doi: 10.4061/2010/470754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adedeji AA, Sanusi B, Tella A, et al. Exposure to anti-malarial drugs and monitoring of adverse drug reactions using toll-free mobile phone calls in private retail sector in Sagamu, Nigeria: implications for pharmacovigilance. Malar J. 2011;10:230. doi: 10.1186/1475-2875-10-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brieger WR, Salako LA, Umeh RE, et al. Promoting prepackaged drugs for prompt and appropriate treatment of febrile illnesses in rural Nigerian communities. Int Q Community Health Educ. 2001;21:19–40. [Google Scholar]
- 28.Tekobo AM, Tayo F, Mabadeje AF. Knowledge and practice of drug retailers in malaria management in Lagos Nigeria: a preliminary survey. Nig Q J Hosp Med. 2008;14:84–87. [Google Scholar]
- 29.Fajola A, Asuzu MC, Owoaje ET, et al. A rural-urban comparison of client-provider interactions in patent medicine shops in South West Nigeria. Int Q Community Health Educ. 2011;32:195–203. doi: 10.2190/IQ.32.3.c. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization [WHO] Partnerships for Malaria Control: Engaging the Formal and Informal Private Sectors. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 31.Agu A, Nwojiji O. Childhood malaria: mothers' perception and treatment seeking behaviour in a community in Ebonyi State, South East Nigeria. J Commun Med Prim Health Care. 2005;17:45–50. [Google Scholar]
- 32.Oguonu T, Okafor HU, Obu HA. Caregivers's knowledge, attitude and practice on childhood malaria and treatment in urban and rural communities in Enugu, south-east Nigeria. Public Health. 2005;119:409–414. doi: 10.1016/j.puhe.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 33.Uzochukwu BSC, Onwujekwe EO, Onoka CA, Ughasoro MD. Rural-urban differences in maternal responses to childhood fever in South East Nigeria. PLoS One. 2008;3:e1788. doi: 10.1371/journal.pone.0001788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adedotun AA, Morenikeji OA, Odaibo AB. Knowledge, attitudes and practices about malaria in an urban community in south-western Nigeria. J Vector Borne Dis. 2010;47:155–159. [PubMed] [Google Scholar]
- 35.Oladepo O, Tona GO, Oshiname FO, Titiloye MA. Malaria knowledge and agricultural practices that promote mosquito breeding in two rural farming communities in Oyo State, Nigeria. Malar J. 2010;9:91. doi: 10.1186/1475-2875-9-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu J, Modrek S, Anyanti J, et al. How do risk preferences relate to malaria care seeking behavior and the acceptability of a new health technology in Nigeria? BMC Health Serv Res. 2014;14:374. doi: 10.1186/1472-6963-14-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.United Nations Human Settlements Programme (UN-Habitat) 2012. Nigeria: Karu Urban Profile. (Available from: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=8&ved=0CFEQFjAH&url=http%3A%2F%2Fmirror.unhabitat.org%2Fpmss%2FgetElectronicVersion.aspx%3Fnr%3D3410%26alt%3D1&ei=PVXZU9XhOOWwj-ALdw4DgBw&usg=AFQjCNEGXIHw19tuhkoTfd3c9gE8_JLnHg&bvm=bv.72185853,d.cGE) [30 July 2013]
- 38.Federal Republic of Nigeria (FRN) 2015. States & Regions. (Available from: http://services.gov.ng/states) [20 January 2015]
- 39.Gething PW, Patil AP, Smith DL, et al. A new world malaria map: Plasmodium falciparum endemicity in 2010. Malar J. 2011;10:1475–2875. doi: 10.1186/1475-2875-10-378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 41.Erhun WO, Osagie A. Management of malaria by medicine retailers in a Nigerian urban community. J Health Popul Dev Ctries. 2004;8:1–6. [Google Scholar]
- 42.Uzochukwu BS, Ezeoke OP, Emma-Ukaegbu U, et al. Malaria treatment services in Nigeria: a review. Nigeria Med J. 2010;51:114–119. [Google Scholar]
- 43.Briggs MA, Kalolella A, Bruxvoort K, et al. Prevalence of malaria parasitemia and purchase of artemisinin-based combination therapies (ACTs) among drug shop clients in two regions in Tanzania with ACT subsidies. PLoS One. 2014;9:e94074. doi: 10.1371/journal.pone.0094074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ajayi IO, Falade CO, Adeniyi JD, Bolaji MO. The role of patent medicine sellers in home management of childhood malaria: a situational analysis of experience in rural Nigeria. Int Q Community Health Educ. 2002;21:271–281. [Google Scholar]
- 45.Chukwuocha UM, Nwakwuo GC, Mmerole I. Artemisinin-based combination therapy: knowledge and perceptions of patent medicine dealers in Owerri Metropolis, Imo State, Nigeria and implications for compliance with current malaria treatment protocol. J Community Health. 2013;38:759–765. doi: 10.1007/s10900-013-9676-y. [DOI] [PubMed] [Google Scholar]
- 46.Bloom G, Standing H, Lucas H, et al. Making health markets work better for poor people: the case of informal providers. Health Policy Plan. 2011;26(suppl 1):i45–i52. doi: 10.1093/heapol/czr025. [DOI] [PubMed] [Google Scholar]
- 47.Ikwuobe JO, Faragher BE, Alawode G, Lalloo DG. The impact of rapid malaria diagnostic tests upon anti-malarial sales in community pharmacies in Gwagwalada, Nigeria. Malar J. 2013;12:380. doi: 10.1186/1475-2875-12-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rabiu OR, Kosoko AM, Falade CO, Ademowo OG. Evaluation of the performances of two rapid diagnostic tests (Cyscope® mini and Paracheck-Pf®) in the diagnosis of malaria among febrile children in southwest Nigeria. Med Princ Pract. 2012;22:255–259. doi: 10.1159/000345642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oladosu OO, Oyibo WA. Overdiagnosis and overtreatment of malaria in children that presented with fever in Lagos, Nigeria. Int Sch Res Notices. 2013;2013:1–6. [Google Scholar]
- 50.Mbonye AK, Ndyomugyenyi R, Turinde A, et al. The feasibility of introducing rapid diagnostic tests for malaria in drug shops in Uganda. Malar J. 2010;9:367. doi: 10.1186/1475-2875-9-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Steinhardt LC, Chinkhumba J, Wolkon A, et al. Quality of malaria case management in Malawi: results from a nationally representative health facility survey. PLoS One. 2014;9:e89050. doi: 10.1371/journal.pone.0089050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pharmacists Council of Nigeria (PCN) Pharmacists Council of Nigeria Website. (Available from: http://pcn.gov.ng/index.htm) [2 December 2014]


