Dear Editor:
High-intensity, costly treatments for patients are common at the end of life (EOL). The impact of such treatments may go beyond their influence on the individual patient and additionally impact family caregivers, who are increasingly relied upon for provision of informal care and EOL decision making. While evidence suggests that treatment intensity impacts the stress and mental health of caregivers (e.g., increased stress for caregivers post ICU usage1 and decreased depression for surviving spouses post hospice care2), the impact of patient EOL care on family caregivers' own health care choices and spending has not been studied. Current EOL health care cost estimates do not consider potential downstream costs associated with the health care expenditures of family caregivers.
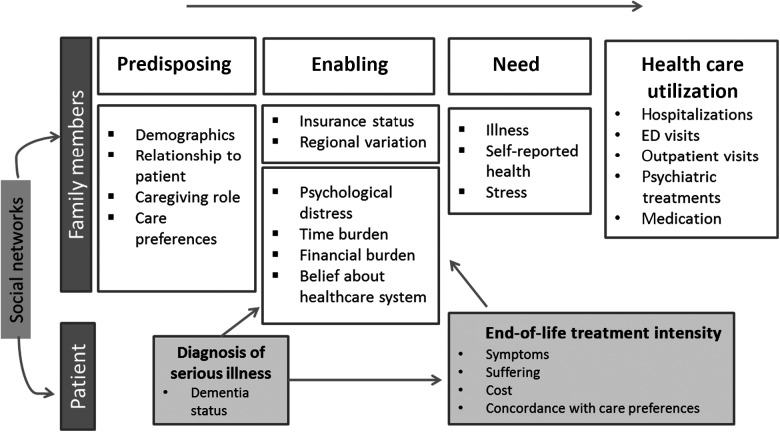
We present a framework for conceptualizing how EOL costs for patients may impact health care utilization for family caregivers that suggests that family health care utilization is impacted by patient treatment intensity because of shared social networks, the financial burden of costs, and the impact of treatments on patient symptom burden (see Fig. 1). Our model is guided by an adapted version of the Aday-Anderson behavioral model of health care utilization,3 which proposes that predisposing, enabling, and need characteristics influence access to and use of health care and incorporates the stress process model of caregiving,4 which conceptualizes caregiving as a chronic stressor that gives rise to strains in multiple domains. Furthermore, we include patient suffering as an independent source of distress for caregivers.5
FIG. 1.
Conceptual framework linking patient end-of-life and family member health care utilization.
We posit that the intensity of health care treatment received by a patient influences patient symptoms, suffering, and costs, which in turn impact enabling factors for the family caregiver, such as financial and time burden and lack of belief in the efficacy of the health care system. Because of this burden, there is a decrease in preventive and self-care behaviors, which ultimately results in increased urgent care use and health care spending for bereaved family members. Finally, we propose that family health care utilization is impacted by patient health care utilization within the context of shared social networks. Behaviors such as use of high-intensity treatments at EOL may be impacted by shared experiences within these social networks.
The impact of EOL treatments may go beyond their influence on the individual patient and additionally impact family caregivers' own health, health care decisions, and future health care utilization. As large datasets of patients with serious illness increasingly survey caregivers and allow for linkages to health care utilization data (e.g., the Health and Retirement Study [http://hrsonline.isr.umich.edu]), these questions can and should be readily answered. By reframing the impact of EOL health care beyond an individual patient, research may influence EOL health care decision making, improve health of family caregivers, and provide a comprehensive estimate of EOL care cost. As such, we will meet a critical need for individuals and families as well as for policymakers in our current era of Medicare reform.
Acknowledgments
Dr. Ornstein's work was supported by the National Institute on Aging (grant K01AG047923) and the National Palliative Care Research Center.
References
- 1.Anderson WG, Arnold RM, Angus DC, Bryce CL: Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med 2008;23:1871–1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ornstein KA, Aldridge MD, Garrido MM, et al. : Association between hospice use and depressive symptoms in surviving spouses. JAMA Intern Med 2015;175:1138–1146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aday LA, Andersen R: A framework for the study of access to medical care. Health Serv Res 1974;9:208–220 [PMC free article] [PubMed] [Google Scholar]
- 4.Pearlin LI, Mullan JT, Semple SJ, Skaff MM: Caregiving and the stress process: An overview of concepts and their measures. Gerontologist 1990;30:583–594 [DOI] [PubMed] [Google Scholar]
- 5.Schulz R, Monin JK, Czaja SJ, et al. : Measuring the experience and perception of suffering. Gerontologist 2010;50:774–784 [DOI] [PMC free article] [PubMed] [Google Scholar]