Abstract
Parent–physician bereavement meetings may benefit parents by facilitating sense making, which is associated with healthy adjustment after a traumatic event. Prior research suggests a reciprocal relationship between sense making and positive emotions. We analyzed parents’ use of emotion words during bereavement meetings to better understand parents’ emotional reactions during the meeting and how their emotional reactions related to their appraisals of the meeting. Parents’ use of positive emotion words increased, suggesting the meetings help parents make sense of the death. Parents’ use of positive emotion words was negatively related to their own and/or their spouse’s appraisals of the meeting, suggesting that parents who have a positive emotional experience during the meeting may also have a short-term negative reaction. Language analysis can be an effective tool to understand individuals’ ongoing emotions and meaning making processes during interventions to reduce adverse consequences of a traumatic event, such as a child’s death.
Keywords: bereavement, language analysis, health, family, physician, meaning making, actor–partner interdependence
The death of a child is one of the most traumatic events an individual or family can face. Bereaved parents often experience serious mental and physical health effects, including depression and anxiety (Kreicbergs, Valdimarsdottir, Onelov, Henter, & Steineck, 2004; McCarthy et al., 2010), complicated grief (Meert et al., 2010), and even death (Li, Precht, Mortensen, & Olsen, 2003). More than 80% of deaths among hospitalized children occur following admission to an intensive care unit (Angus et al., 2004). Findings from studies conducted by the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN) indicated that many bereaved parents wanted to meet with the physician who cared for their child in the pediatric intensive care unit (PICU; Meert et al., 2007). Parents’ primary reason for wanting to meet with the PICU physician was to gain further information about the circumstances surrounding the death. Parents also wanted to reconnect with the physician and staff and to gain reassurance that everything possible had been done for the child. Findings from these studies also indicated that physicians were willing to conduct bereavement meetings, primarily because they felt the meetings would be beneficial to parents (Eggly et al., 2013; Meert et al., 2011).
Based on these findings, the CPCCRN developed and pilot tested the feasibility of a framework for conducting parent–physician bereavement meetings in the weeks or months following a child’s death in a PICU (Eggly et al., 2011; Meert et al., 2014). The bereavement meetings are designed to reduce the development of adverse health effects related to a child’s death. Briefly, the framework provides suggestions for the meeting content and structure, such as topics that parents may want to discuss and the potential duration and location of the meeting. The framework specifically suggests that physicians discuss the medical circumstances of the death and provide reassurance, as needed or requested by parents. Also, the framework provides suggestions for ways physicians can communicate effectively during the meeting, such as by encouraging parents to set the meeting agenda and responding directly and empathically to parents’ medical and psychosocial questions and concerns. (Details of the intervention are available elsewhere [Eggly et al., 2011]). Prior to implementing the framework for the pilot study, PICU physicians were trained in the use of the framework via a face-to-face or web-based small group workshop. The workshop included a lecture on the health consequences of bereavement, a description of key aspects of the framework, and a viewing of three simulated bereavement meetings. In the current study, we analyzed transcripts of language used by bereaved parents during bereavement meetings held as part of the pilot study to better understand (1) parents’ emotional reactions throughout the meetings and (2) how their emotional reactions were related to their appraisals of the meeting.
The expressed desires of bereaved parents to meet with a physician who cared for their deceased child may reflect a struggle to make meaning of the death. Research on meaning making suggests that, for many people, traumatic or stressful events challenge their basic assumptions about themselves and the world, causing distress and leading them to engage in various processes to make meaning, or to restore a sense that the world is meaningful and life is worthwhile (Holland, Currier, & Neimeyer, 2006; Meert et al., in press; Park, 2010). Bereaved parents, in particular, face a crisis of meaning as they try to reconstruct their personal world (Keesee, Currier, & Neimeyer, 2008). Successful meaning making is associated with better adjustment to the tragic event, whereas unsuccessful meaning making leads to continued distress and ongoing attempts to find meaning (Gillies & Neimeyer, 2006; Park, 2010).
Several types of meaning-making processes have been described. One type—sense making—has been shown to be crucial to a healthy grieving process (Holland et al., 2006; Keesee et al., 2008). Sense making, also called searching for comprehensibility (Janoff-Bulman & Frantz, 1997), refers to attempts to comprehend a loss or find a benign explanation for an inexplicable experience (Holland et al., 2006; Janoff-Bulman & Frantz, 1997; Park, 2010). In a study of bereaved college students, Holland et al. (2006) found that a higher degree of sense making predicted lower levels of grief complication over the first 2 years of bereavement. Similarly, in a study of bereaved parents, Keesee et al. (2008) found that a higher degree of sense making was associated with less intense grief. In a qualitative analysis of responses by these same parents, Lichtenthal, Currier, Neimeyer, and Keesee (2010) found that nearly half (45%) of the parents could not make sense of their child’s death, suggesting that bereaved parents may benefit from opportunities for sense making.
Meeting with a physician who cared for the child at the end of the child’s life may provide an opportunity for bereaved parents to work toward making sense of their child’s death. These physicians are uniquely qualified to facilitate parents’ meaning making because of their knowledge of the specific medical circumstances of the child’s death and because of the relationship they developed with the family during a time of great emotional intensity. However, assessing parents’ meaning making in this context is quite difficult, as research has been limited by self-report, single-item measures (Holland et al., 2006; Park, 2010), which rely heavily on the subjective assessment of individuals’ own meaning-making processes. Assessing parents’ ongoing emotions as they occur during the meetings may shed some light on their meaning-making processes. Fredrickson (2000) and Fredrickson and Joiner (2002) suggest that positive meaning and positive emotions go hand in hand. More specifically, finding meaning triggers positive emotions, and positive emotions explain the benefit attributed to finding meaning. Possibly, as physicians provide information and parents begin to make sense of the death, their emotions become more positive.
Language analysis is a method increasingly used to examine emotions as they unfold in naturalistic settings (Pennebaker, Mehl, & Niederhoffer, 2003). Building on early psychological research and theory, researchers over the past two decades have demonstrated that the words people use in their daily lives reflect what they are thinking about, how they are feeling, and how they organize their thoughts (Pennebaker, 2011; Tausczik & Pennebaker, 2010). These researchers have systematically analyzed writing samples or transcripts of spoken language to identify links between the language patterns and various psychological dimensions of interest (Tausczik & Pennebaker, 2010). Language analysis software, and in particular, Linguistic Inquiry and Word Count (LIWC; Pennebaker, Booth, & Francis, 2007), has been used to show that word use accurately reflects people’s emotional states (Kahn, Tobin, Massey, & Anderson, 2007; Slatcher, Vazire, & Pennebaker, 2008; Tausczik & Pennebaker, 2010) and changes as people adjust to emotional upheaval (Abe, 2009; Pennebaker et al., 2003).
LIWC is a widely used computerized text analysis program that categorizes and quantifies language use by counting the proportion of text that falls into a given category, such as grammatical markers (e.g., articles, prepositions) or psychological processes (e.g., emotion, cognitive, social). For example, Kahn, Tobin, Massey, and Anderson (2007) used LIWC software to examine individual differences in emotional expressivity, emotional reactivity, and personality. Using writing samples from college students, these researchers found that word use, as identified by four LIWC categories—positive emotion, positive feeling, negative emotions, and sadness/depression—could meaningfully indicate emotion. Findings from other researchers suggest that this software could potentially be useful as an alternative or complement to self-reported emotion (Hexem, Miller, Carroll, Faerber, & Feudtner, 2013). In another study, Slatcher et al. (2008) found that LIWC software was able to predict relationship quality by examining how the emotion words couples use in everyday life are linked to the quality of their relationship. Studies also suggest that word use analysis can be used to predict longer term health (Danner, Snowdon, & Friesen, 2001; Gottschalk & Glaser, 1969; Pennebaker, 2011; Pennebaker et al., 2003). Pennebaker (1997, 2011), Pennebaker and Chung (2011), Pennebaker et al., 2003, Pennebaker, Kiecolt-Glaser, and Glaser (1988) have conducted many studies showing that writing (and in some cases, talking) about a traumatic event, even for a short period of time, can improve psychological and physical health, and that this improvement is predicted by the use of positive emotion words in the writing. However, no studies have examined the trajectory of emotion word use that occurs during discussions of traumatic events.
In this study, we examined the trajectory of bereaved parents’ emotion words expressed during parent–physician bereavement meetings. First, we predicted that parents would use more positive emotion words (e.g., “happy”, “nice”) and fewer negative emotion words (e.g., “hurt”, “angry”) as the meeting progressed. For bereaved parents, meeting with the physician and discussing the circumstances of the death is likely to provoke strong negative emotions. As parents gain information and explanations, they can begin to construct a coherent narrative, or make sense, of the child’s death. Once these explanations are received and tentatively accepted, the discussion can turn to other topics, such as sharing memories of the child, expressing appreciation, and gaining reassurance from the physician, and parents may begin to express more positive emotions and fewer negative emotions. Second, we predicted that the pattern of parents’ emotion word use (e.g., more positive and less negative emotion words as the meeting progressed) would be related to parents’ perceptions that the meetings were generally helpful, informative, and would help them cope. Third, based on prior research showing that an individual’s emotion word use influences his or her partner’s perceptions (Slatcher et al., 2008), we hypothesized that changes in mothers’ and fathers’ word use over the course of the meeting would be related to their spouse’s perceptions of the meeting.
Method
Settings and Participants
This secondary analysis used data from a pilot study of parent–physician bereavement meetings conducted by the CPCCRN, a National Institute of Child Health and Human Development–funded multicenter research network consisting of seven academic pediatric centers (Meert et al., 2014). The study was approved by the institutional review boards at each data collection site and the CPCCRN data coordinating center. All participants provided informed consent.
The data included 35 bereavement meetings conducted according to the CPCCRN framework (Eggly et al., 2011). Study participants were PICU physicians (N = 23) and parents (N = 53). Parents were eligible if their child died in a CPCCRN-affiliated PICU, if they spoke English or Spanish, if they were ≥ 18 years of age, and if a participating PICU physician trained in the use of the framework participated in their child’s care. Recruitment details and other procedures for the original study are provided elsewhere (Meert et al., 2014). Each physician conducted one to three meetings; one follow-up meeting was conducted per family. Meetings included one PICU physician and at least one parent; 16 meetings included more than one parent.
Physicians were 41.0 years of age on average (SD = 7.8); 12 (52%) were male; 18 (78%) were White, and 20 (87%) were non-Hispanic. Parents were 37.7 years of age on average (SD = 9.8); 32 (60%) were mothers and 21 (40%) were fathers; 39 (74%) were married; 39 (74%) were White, and 40 (75%) were non-Hispanic. Deceased children (N =35) of participating parents were 6.9 years of age on average at the time of death (SD = 7.0); 17 (49%) were boys; 9 (26%) died suddenly, and 26 (74%) died from chronic conditions.
Procedure
On average, meetings lasted 1.2 hours (SD = 0.6) and occurred 14.5 weeks after the child’s’ death (SD = 6.3). They were held in a conference room at the hospital where the child died or at another on-campus location. Approximately 1 week after attending a meeting, parents completed an investigator-developed telephone questionnaire designed to elicit their perspectives on the meeting. There were 8 items with either a rating scale response format (1 = strongly disagree, 5 = strongly agree) or a brief open-ended response format. Three of the rating scale items were used for this secondary analysis: “The information discussed at the meeting was important to me,” “The meeting was helpful to me,” and “The meeting will help me in the future to cope with the loss of my child.”
Linguistic Analyses
Meetings were video recorded and transcribed. Transcripts were separated by speaker, divided into five equal time segments, and processed using LIWC (Pennebaker et al., 2007). Analyses focused on positive emotion words (PEW) and negative emotion words (NEW) used by mothers and fathers during the meeting.1
Statistical Analyses
To examine our hypotheses, we used a multilevel model framework to fit the data to multivariate outcome actor–partner interdependence models (Cook & Kenny, 2005) using HLM 7.01 (Raudenbush, Bryk, & Congdon, 2010). Level-1 of the model contained within-dyad outcomes and predictors, and Level-2 contained between-dyad predictors. Predicted values for the outcomes (i.e., percentage of emotion words per meeting segment) could not be less than zero; therefore, we used a Poisson regression with variable duration defined by meeting segment length (i.e., total meeting length in minutes divided by 5) to model the outcomes. For each outcome (PEW and NEW), scores at each time point for each parent were nested within dyads. We used four separate dummy indicator variables to identify to which outcome and which parent each score corresponded (i.e., Dad PEW, Dad NEW, Mom PEW, Mom NEW). We coded separate time variables for each outcome by mother or father to estimate parameters for the PEW and NEW trajectories separately. We centered time at the fifth meeting segment (i.e., segment 5 = 0, segment 4 = −1, etc.) to model the intercept for each trajectory as the mean PEW or mean NEW for each parent at segment 5. This way, the model intercept would be more contextually interpretable since parents talked more as the meetings progressed. We included a squared term for time (TSq) to model the trajectories’ quadratic departure from linearity. Time and TSq were coded as “0” when they did not correspond to a particular score for a particular parent gender. The Level-1 model took the following form:
The modeled outcome, referred to as the incidence rate η, is the log of the “score” (i.e., the percent of emotion words). We excluded the Level-1 intercept from the model so that we can interpret the coefficients associated with the indicator variables Dad PEW, Dad NEW, Mom PEW, and Mom NEW as the intercepts, or the mean incidence rates of emotion word use during segment 5 of the meeting (Raudenbush, Brennan, & Barnett, 1995). The coefficients for Time and TSq indicate the shape of the trajectories for emotion words over the course of the meeting. Coefficients associated with Time represent the instantaneous rate of change in incidence rates at segment 5 (i.e., the linear increase or decrease in PEW or NEW at segment 5). The exponentiation of these coefficients represents the event rate ratios (ERR)—the ratio of outcome scores differing in one unit of time—at segment 5. Coefficients associated with the TSq variables represent quadratic rate of change of the PEW and NEW trajectories and are interpreted as the curvature of the trajectory (i.e., the extent to which the emotion word trajectories deviate from linearity).
Results
Emotion Word Trajectories
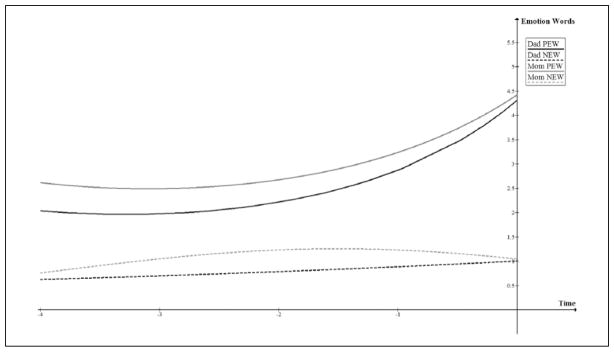
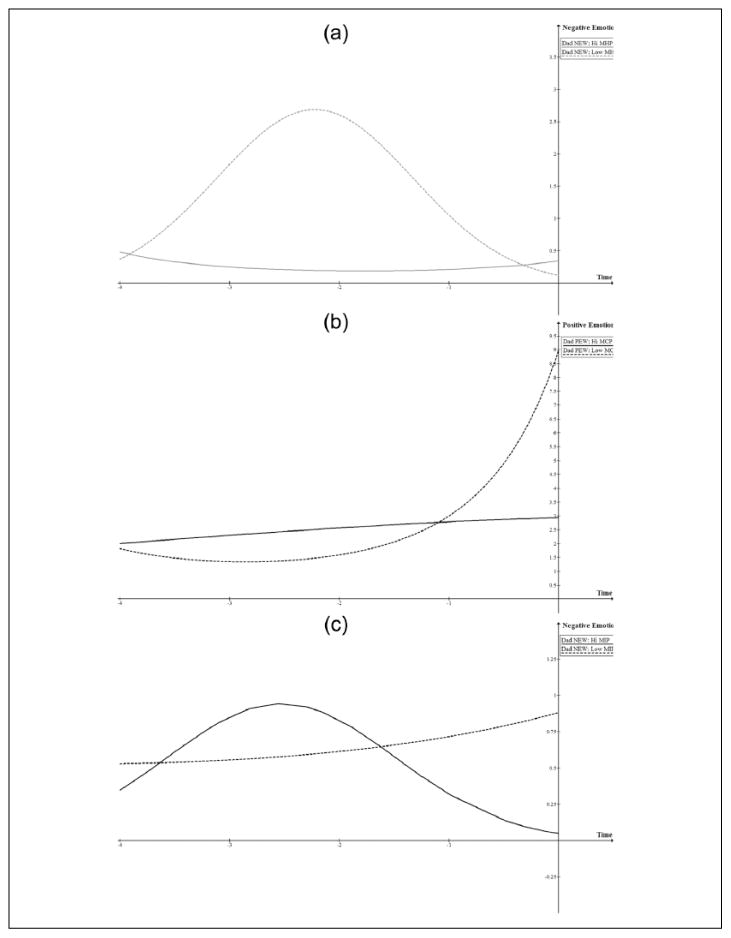
Our first hypothesis was that parents’ use of PEW would increase and NEW would decrease over the course of the meeting. Table 1 displays results for the preliminary model, which did not include dyad level predictors. The coefficient βs are expressed in their mixed-model forms as γs. For fathers, we found no significant change in NEW and marginal change in PEW. For mothers, we found a significant change in PEW, and the marginal Mom PEW TSq coefficient suggests that the change was not linear. There was no significant change in mothers’ NEW (Figure 1).
Table 1.
Results of Multivariate Actor–Partner Interdependence Model (APIM) Modeling Emotion Word Trajectory During Meetings.
| Fixed Effects | γ | SE | p | ERR | ERR 95% CI | |
|---|---|---|---|---|---|---|
| Dad PEW | −1.23* | 0.27 | .00 | 0.29 | 0.17 | 0.51 |
| Dad PEW Time | 0.48† | 0.27 | .08 | 1.61 | 0.94 | 2.79 |
| Dad PEW TSq | 0.07 | 0.06 | .24 | 1.08 | 0.95 | 1.22 |
| Dad NEW | −2.69* | 0.29 | .00 | 0.07 | 0.04 | 0.12 |
| Dad NEW Time | 0.13 | 0.32 | .70 | 1.13 | 0.59 | 2.18 |
| Dad NEW TSq | 0.00 | 0.08 | .98 | 1.00 | 0.86 | 1.17 |
| Mom PEW | −1.21* | 0.14 | .00 | 0.30 | 0.22 | 0.40 |
| Mom PEW Time | 0.37* | 0.13 | .01 | 1.45 | 1.12 | 1.87 |
| Mom PEW TSq | 0.06† | 0.04 | .10 | 1.06 | 0.99 | 1.14 |
| Mom NEW | −2.65* | 0.19 | .00 | 0.07 | 0.05 | 0.10 |
| Mom NEW Time | −0.24 | 0.20 | .24 | 0.78 | 0.52 | 1.18 |
| Mom NEW TSq | −0.08 | 0.05 | .11 | 0.92 | 0.83 | 1.02 |
Note. PEW = positive emotion words; NEW = negative emotion words; Tsq = squared term for time; ERR = event rate ratio.
p< .10.
p< .05.
Figure 1.
Trajectories for fathers’ and mothers’ positive emotion words (PEW) and negative emotion words (NEW).
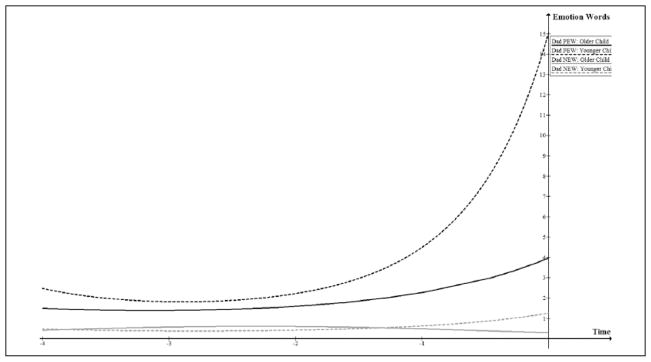
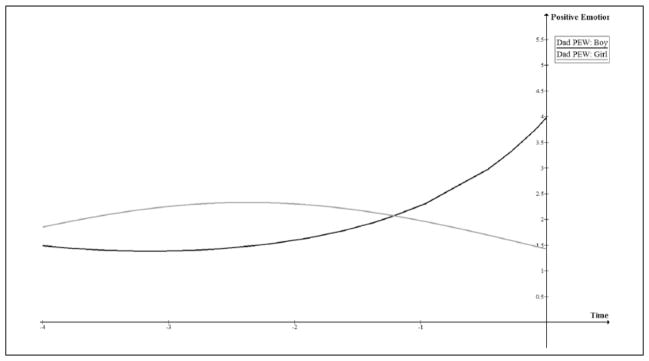
Though the t-tests of the coefficients for fathers’ PEW trajectories were not significantly different from 0 (Table 2), both the graphical representation of the trajectory and the magnitude of the coefficients, as compared with those for mothers, suggested that fathers’ PEW changed over the course of the meeting. Two potential reasons for the nonsignificant change in fathers’ PEW are (1) the effects of time are similar to, but less robust than the effects of time for mothers’ PEW, and therefore less likely to be significant given sample size or (2) dyad-level variation in the estimates of the coefficients for Dad PEW Time and Dad PEW TSq yielded larger standard errors of the estimates and thus smaller t-statistics for the tests of significance. Our examination of the random effects for the fathers’ PEW trajectory showed significant dyad-level variance in all the parameters associated with the fathers’ PEW trajectory: all χ2s(18) > 48, ps < .001). There was also significant dyad-level variance in the coefficient for Dad NEW, χ2(18) = 75.88, p< .001, and Mom PEW, χ2(18) = 45.80, p< .001. Therefore, we included three dyad-level variables (whether child’s death was sudden, child gender, and whether the child was <3 years old) as predictors of the Level-1 coefficients (i.e., cross-level interactions). Significant moderating effects of dyad-level covariates were: Child’s age significantly influenced trajectories for fathers’ PEW and fathers’ NEW, such that the death of a younger child significantly increased coefficients for Dad PEW (γ = 1.33, t[31] = 2.87, p< .01), Dad NEW (γ = 1.44, t[31] = 2.49, p< .05), and Dad NEW time (γ = 1.46, t[31] = 2.27, p< .05). This indicated that fathers of younger children had a higher percent PEW at segment 5 and a higher percent NEW and steeper increase in NEW at segment 5 compared with fathers of older children (Figure 2). Child gender significantly influenced fathers’ PEW, such that the death of a girl significantly decreased Dad PEW (γ = −1.02, t[31] = −2.23, p< .05) and Dad PEW Time (γ = −1.08, t[31] = −2.17, p< .05). This indicates that fathers of girls, compared with fathers of boys, had a smaller percentage of PEW at segment 5 and their trajectories for PEW were decreasing through segment 5 (Figure 3). There were no statistically significant effects of a child’s sudden death on fathers’ PEW or NEW. None of the dyad-level covariates significantly influenced mothers’ PEW or NEW.
Figure 2.
Effects of children’s age on trajectories for fathers’ positive emotion words (PEW) and negative emotion words (NEW).
Figure 3.
Effect of children’s gender on trajectory for fathers’ positive emotion words (PEW).
Actor and Partner Effects
Hypotheses 2 and 3 examined associations between parents’ emotion words and (1) their own (actor effects) and (2) their spouses’ perceptions of the meetings (partner effects). Different numbers of fathers (N = 18) and mothers (N = 31) provided postmeeting perceptions. To avoid reduction in sample size because of list-wise deletion when mothers’ perceptions were predictors, we tested for actor–partner effects in two separate models: one for fathers’ and another for mothers’ perceptions of the meeting. The Level-1 model was the same as the preliminary model used to examine the first hypothesis. To test our hypotheses, we simultaneously included perceptions of how informative, how generally helpful, and how helpful for coping the meetings were as dyad-level predictors of the Level-1 trajectory parameters. We controlled for child’s age and gender because they were shown to influence trajectories for fathers’ PEW and NEW.
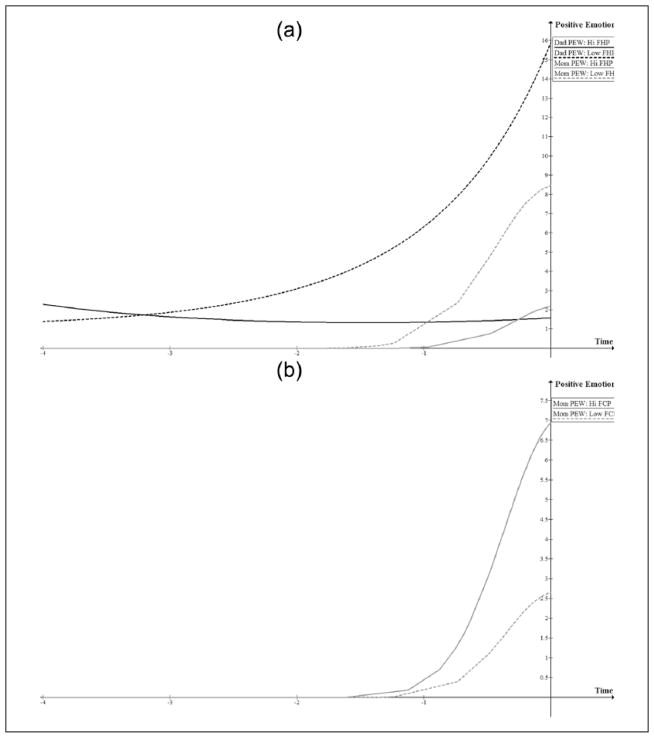
Fathers’ Perceptions of the Meetings
Fathers’ perceptions of the meeting’s helpfulness were negatively associated with Dad PEW (γ = −2.23, t[12] = −2.24, p< .05) and with Mom PEW (γ = −1.31, t[14] = −2.28, p< .05). When fathers’ PEW at segment 5 was higher, fathers thought the meeting was less helpful; when mothers’ PEW at segment 5 was higher, fathers saw the meeting as less helpful (Figure 4a). There were no other significant actor or partner effects associated with fathers’ perceptions of the meeting’s helpfulness.
Figure 4.
(a) Effects of fathers’ helpfulness perceptions (FHP) (plotted at 0.5 SD above and below mean helpfulness) on trajectories of fathers’ and mothers’ Positive Emotion Words (PEW), holding constant parents’ other perceptions and control variables. (b) Effects of fathers’ coping perceptions (FCP) (plotted at 0.5 SD above and below mean coping) on trajectory of mothers’ positive emotion words (PEW), holding constant parents’ other perceptions and control variables.
Fathers’ perceptions of whether the meeting would help them cope were positively associated with Mom PEW (γ = 0.91, t[14] = 2.19, p< .05). When mothers’ PEW was higher during segment 5, fathers had more favorable perceptions that the meetings would help them cope (Figure 4b). There were no other significant actor or partner effects associated with fathers’ coping perceptions, and no actor or partner effects associated with fathers’ perceptions of how informative the meetings were.
Mothers’ Perceptions of the Meetings
Mothers’ perceptions of the meeting’s helpfulness were positively associated with Dad NEW Time (γ = 2.09, t[26] = 2.52, p< .05) and Dad NEW TSq (γ = 0.49, t[26] = 2.45, p< .05). Examining plots of the trajectories suggested that mothers thought the meetings were more helpful when fathers’ NEW remained relatively lower and unchanged for the duration of the meetings (Figure 5a).
Figure 5.
(a) Effects of mothers’ helpfulness perceptions (MHP) (plotted at 1 SD above and below mean coping) on trajectory of fathers’ negative emotion words (NEW), holding constant parents’ other perceptions and control variables. (b) Effects of mothers’ coping perceptions (MCP) (plotted at 0.5 SD above and below mean coping) on trajectory of fathers’ positive emotion words (PEW), holding constant parents’ other perceptions and control variables. (c) Effects of mothers’ perceptions of meeting informativeness (MIP) (plotted at 1 SD above and below mean coping) on trajectory of fathers’ negative emotion words (NEW), holding constant parents’ other perceptions and control variables.
Mothers’ perceptions that the meeting would help them cope were negatively associated with Dad PEW (γ = −1.02, t[25] = −3.66, p< .01), Dad PEW Time (γ = −1.18, t[25] = −3.19, p< .01), and Dad PEW TSq (γ = −0.23, t[25] = −2.33, p< .05). For fathers whose PEW showed greater increase throughout the meeting, mothers had lower coping perceptions (Figure 5b).
Mothers’ perceptions of the meeting’s informativeness were negatively associated with Dad NEW (γ = −1.82, t[26] = −4.40, p< .01) and Dad NEW Time (γ = −1.63, t[26] = −2.16, p< .05). For fathers whose NEW showed relatively greater increase throughout the meeting, mothers thought the meeting was less informative (Figure 5c). There were no significant actor effects of mothers’ meeting perceptions.
Discussion
This novel study provided some promising, albeit preliminary, findings. Our first finding supported our prediction that bereaved parents, in general, would use more positive emotion words and fewer negative emotion words over the course of the meeting. While speculative, this finding may also support our suggestion that the meetings coincide with bereaved parents’ active struggle to make meaning of the death, and that the meeting, especially the discussion of the medical circumstances of the child’s death, provokes strong negative emotions. As the meeting progresses, parents’ emotion words become more positive as parents begin to accept the physician’s explanation, and the discussion turns to more positive topics, such as asking for reassurance that everything was done on behalf of their child, reminiscing about the child, and expressing appreciation for the care their child received.
While preliminary, our finding about parents’ increasing use of positive emotion words suggests that bereavement meetings are beneficial to parents. As described above, positive emotion and sense making after a stressful or traumatic event are independently and reciprocally related to better adjustment to the event (Frederickson & Joiner, 2002; Holland et al., 2006; Keesee et al., 2008; Lichtenthal, et al., 2010). Research also shows that using positive emotion words when writing about a traumatic event is related to improvement in psychological and physical health (Pennebaker, 1997, 2011; Pennebaker & Chung, 2011; Pennebaker et al., 1988; Pennebaker et al., 2003). Writing/talking exercises benefit individuals by providing an opportunity for them to transform their thoughts and feelings into language (Pennebaker, 2011), and thus to construct a coherent narrative of the event. Follow-up meetings provide bereaved parents a similar opportunity by addressing their need to gain information about the circumstances of the child’s death and to reconnect with physicians and healthcare staff that cared for their child (Meert et al., 2007). Our finding that there were individual differences in the trajectory of emotion word use suggests variability in parents’ emotional experience of the meeting. Further research should be conducted with a larger sample and a longer term longitudinal design to confirm this trajectory and to determine its relationship with discussion topics or long-term health, and the extent of individual differences.
Our second finding was that increases in parents’ use of positive emotion words during the meeting were negatively associated with parents’ own and their spouse’s perceptions of the meeting. This surprising finding was consistent with results found in a population of parents whose children were receiving palliative care (Hexem et al., 2013). In that study, researchers compared two measures of emotions, language analyses using LIWC software and self-reports on a validated affect scale. LIWC software was used to measure the use of positive and negative emotion words parents used during semistructured interviews about their experience with medical decision making. Parents reported their emotions by completing the Positive and Negative Affect Schedule (PANAS; Crawford & Henry, 2004). Findings showed that positive emotions expressed during the semistructured interviews were negatively associated with self-reported positive affect. Our findings and those of Hexem et al. (2013) may be explained by prior research suggesting that individuals increase their use of positive emotion words when writing about trauma, but also feel worse immediately after writing (Pennebaker, 1997). Possibly, bereaved parents had a similar experience: the process of expressing positive emotions relating to the death of their child was accompanied by their own and their spouse’s worse feelings immediately following the meeting. Previous research also indicates that despite negative moods individuals experience immediately after writing about traumatic events, they experience long-term health benefits (Pennebaker & Beall, 1986).
Although the general pattern was that increases in positive emotion word use were associated with negative perceptions of the meetings, this language analysis revealed some intriguing exceptions to the pattern. We found that when mothers used more positive emotion words over the course of the meeting, fathers had more favorable perceptions of whether the meetings would help them cope with the death. Perhaps this is an example of an instance in which positive perceptions are evident despite any post-meeting negative emotions. Also, we found that for some fathers, the use of negative emotion words peaked in the middle of the meeting (potentially around the time the discussion turned to psychosocial topics) and then steadily decreased through the end of the meeting. Among fathers who showed this curvilinear pattern, mothers perceived the meeting as less helpful, but more informative. We are aware of no other studies of the effect of individuals’ word use on their significant or close other’s perceptions. These findings, therefore, suggest that further research is warranted to extend the robust body of research showing relationships between individuals’ word use and their own characteristics and/or outcomes.
There were several limitations of this study. Because this secondary analysis was based on a pilot study, a small sample size was used, limiting our statistical power, the generalizability of our findings, and our ability to conduct further analyses, such as potential effects of the child’s clinical variables. Also, the items used to assess parents’ perceptions of the meetings have face validity, but because they are single items, we cannot determine whether they reliably assessed the underlying constructs of interest. However, findings from this study were consistent with those reported by Hexem et al. (2013), in which participants completed a well-validated affect scale. Finally, parents did not provide information about their social or psychological characteristics or long-term health outcomes. Thus, although these preliminary findings suggest that the emotion words parents use during bereavement meetings matter, precisely how they matter—especially in the long-term—remains unclear.
Conclusions
Findings from this study suggest that language analyses, such as those offered by LIWC software, may provide an effective tool with which to understand the ongoing emotions and meaning-making processes of individuals during interventions to prevent or reduce adverse consequences of a traumatic event, such as a child’s death. Ultimately, these types of analyses may be useful as a tool to better understand whether, how, and for whom these interventions provide a long-term benefit for bereaved parents. Further, this study, along with our prior research (Meert et al., 2014; Meert et al., in press), provides evidence that bereavement meetings conducted according to the CPCCRN framework are feasible, acceptable, and potentially beneficial through providing an opportunity for meaning making. It is particularly important for physicians caring for children at the end of life to be aware of parents’ emotional trajectory during bereavement meetings. Although physicians may be reluctant to hold bereavement meetings because of their concerns about upsetting parents, the meetings may ultimately provide a benefit. Thus, while limited, findings suggest that future studies using larger samples and a longitudinal design to test the effectiveness of bereavement meetings on parents’ longer-term physical and psychosocial outcomes are warranted. Also, although examining physician language was beyond the scope of this study, future studies might include a comprehensive analysis of physician language used during the meetings. This type of analysis might explore the influence of physician language associated with the CPCCRN framework, such as the bereavement-related topics they discuss and the linguistic features they use to discuss them, on parents’ language, and in turn, on parent outcomes.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by cooperative agreements from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services (U10HD050096, U10HD049981, U10HD063108, U10HD063106, U10HD063114, U10HD050012 and U01HD049934).
Biographies
Susan Eggly, PhD, is anassociate professor in the Department of Oncology, Karmanos Cancer Institute, Wayne State University. Her research focuses on the effect of patient–physician communication on health outcomes related to cancer, health disparities, and end of life care.
Mark A. Manning, PhD, is anassistant professor in the Department of Oncology, Karmanos Cancer Institute, Wayne State University. His research focuses on predicting health behaviors and health behavioral decision making.
Richard B. Slatcher, PhD, is an associate professor in the Department of Psychology at Wayne State University. The focus of his research is on understanding close relationships and their impact on health and well-being.
Robert A. Berg, MD, is Division Chief of Critical Care Medicine at the Children’s Hospital of Philadelphia and professor of anesthesiology and critical care medicine and pediatrics at the Perelman School of Medicine at the University of Pennsylvania. He is a principal investigator for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN).
David L. Wessel, MD, is Executive Vice President and Chief Medical Officer for Hospital and Specialty Services at Children’s National Medical Center, and professor of anesthesiology and critical care medicine and pediatrics at George Washington University. He is a principal investigator for the CPCCRN.
Christopher J. L. Newth, MD, is Research Director of Anesthesiology Critical Care Medicine at Children’s Hospital Los Angeles; and professor of pediatrics at University of Southern California Keck School of Medicine. He is a principal investigator for the CPCCRN.
Thomas P. Shanley, MD, is Associate Dean for Clinical and Translational Research; Director of the Michigan Institute for Clinical & Health Research (MICHR); and professor of pediatrics and communicable diseases at the University of Michigan. He is a principal investigator for the CPCCRN.
Rick Harrison, MD, is Vice Chair for Clinical Affairs; professor of pediatrics at Mattel Children’s Hospital University of California, Los Angeles. He is a principal investigator for the CPCCRN.
Heidi Dalton, MD, is Chief of Critical Care, Phoenix Children’s Hospital; and professor of child health, University of Arizona College of Medicine. She is a principal investigator for the CPCCRN.
J. Michael Dean, MD, MBA, is Chief, Division of Pediatric Critical Care; Vice-Chairman, Department of Pediatrics; and professor of pediatrics at University of Utah. He is theprincipal investigator for the CPCCRN Data Coordinating Center.
Allan Doctor, MD, is Director of the Division of Pediatric Critical Care Medicine at St. Louis Children’s Hospital; an associate professor of biochemistry and molecular biophysics, and of pediatrics at Washington University School of Medicine. He is Chairman of the CPCCRN Steering Committee.
Tammara Jenkins, RN, MS, is NICHD project scientist for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network.
Kathleen L. Meert, MD, is Chief of the Division of Critical Care Medicine at Children’s Hospital of Michigan; and professor of pediatrics at Wayne State University. She is a principal investigator for the CPCCRN.
Footnotes
In separate models not reported here, we examined whether physicians’ use of positive and negative emotion words significantly influenced fathers’ and mothers’ positive and negative emotion word use. First, we examined whether physicians’ emotion word use changed over the course of the meeting. Since results indicated no change over time, we averaged physicians’ positive and negative word use over the meeting segments, and included the averages as predictors of fathers’ and mothers’ emotion word use trajectories at Level-2 of the models. Analyses indicated that physicians’ emotion word use had no effect on fathers’ and mothers’ emotion word use, and so they were excluded from the models.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Abe JAA. Words that predict outstanding performance. Journal of Research in Personality. 2009;43:528–531. [Google Scholar]
- Angus DC, Barnato AE, Linde-Zwirble WT, Weissfeld LA, Watson RS, Rickert T, Rubenfeld GD. Use of intensive care at the end of life in the United States: An epidemiologic study. Critical Care Medicine. 2004;32:638–643. doi: 10.1097/01.ccm.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- Cook WL, Kenny DA. The actor-partner interdependence model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development. 2005;29:101–109. [Google Scholar]
- Crawford JR, Kenney JD. The Positive and Negative Affect Scale (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. British Journal of Clinical Psychology. 2004;43:245–265. doi: 10.1348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- Danner DD, Snowdon DA, Friesen WV. Positive emotions in early life and longevity: Findings from the nun study. Journal of Personality and Social Psychology. 2001;80:804–813. [PubMed] [Google Scholar]
- Eggly S, Meert KL, Berger J, Zimmerman J, Anand KJ, Newth CJ Eunice Kennedy Shriver National Institute of Child Health, Human Development Collaborative Pediatric Critical Care Research Network. A framework for conducting follow-up meetings with parents after a child’s death in the pediatric intensive care unit. Pediatric Critical Care Medicine. 2011;12:147–152. doi: 10.1097/PCC.0b013e3181e8b40c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggly S, Meert KL, Berger J, Zimmerman J, Anand KJ, Newth CJ Pediatric Critical Care Research Network. Physicians’ conceptualization of “closure” as a benefit of physician-parent follow-up meetings after a child’s death in the pediatric intensive care unit. Journal of Palliative Care. 2013;29:69–75. [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL. Cultivating positive emotions to optimize health and well-being. Prevention & Treatment. 2000;3:1–25. [Google Scholar]
- Fredrickson BL, Joiner T. Positive emotions trigger upward spirals toward emotional well-being. Psychological Science. 2002;13:172–175. doi: 10.1111/1467-9280.00431. [DOI] [PubMed] [Google Scholar]
- Gillies J, Neimeyer R. Loss, grief, and the search for significance: Toward a model of meaning reconstruction in bereavement. Journal of Constructivist Psychology. 2006;19:31–65. [Google Scholar]
- Gottschalk LA, Gleser CG. The measurement of psychological states through the content analysis of verbal behavior. Berkeley, CA: University of California Press; 1969. [Google Scholar]
- Hexem KR, Miller VA, Carroll K, Faerber JA, Feudtner C. Putting on a happy face: Emotional expression in parents of children with serious illness. Journal of Pain and Symptom Management. 2013;45:542–551. doi: 10.1016/j.jpainsymman.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland JM, Currier JM, Neimeyer RA. Meaning reconstruction in the first two years of bereavement: The role of sense making and benefit finding. Omega. 2006;53:175–191. [Google Scholar]
- Janoff-Bulman R, Frantz CM. The impact of trauma on meaning: From meaningless world to meaningful life. In: Power JJ, Brewin CR, editors. The transformation of meaning in psychological therapies: Integrating theory and practice. Hoboken, NJ: Wiley; 1997. pp. 91–106. [Google Scholar]
- Kahn JH, Tobin RM, Massey AE, Anderson JA. Measuring emotional expression with the Linguistic Inquiry and Word Count. American Journal of Psychology. 2007;120:263–286. [PubMed] [Google Scholar]
- Keesee NJ, Currier JM, Neimeyer RA. Predictors of grief following the death of one’s child: The contribution of finding meaning. Journal of Clinical Psychology. 2008;64:1145–1163. doi: 10.1002/jclp.20502. [DOI] [PubMed] [Google Scholar]
- Kreicbergs U, Valdimarsdottir U, Onelov E, Henter JI, Steineck G. Anxiety and depression in parents 4–9 years after the loss of a child owing to a malignancy: A population-based follow-up. Psychological Medicine. 2004;34:1431–1441. doi: 10.1017/s0033291704002740. [DOI] [PubMed] [Google Scholar]
- Li J, Precht DH, Mortensen PB, Olsen J. Mortality in parents after death of a child in Denmark: a nationwide follow-up study. Lancet. 2003;361:363–367. doi: 10.1016/S0140-6736(03)12387-2. [DOI] [PubMed] [Google Scholar]
- Lichtenthal WG, Currier JM, Neimeyer RA, Keesee NJ. Sense and significance: A mixed methods examination of meaning making after the loss of one’s child. Journal of Clinical Psychology. 2010;66:791–812. doi: 10.1002/jclp.20700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy MC, Clarke NE, Ting CL, Conroy R, Anderson VA, Heath JA. Prevalence and predictors of parental grief and depression after the death of a child from cancer. Journal of Palliative Medicine. 2010;13:1321–1326. doi: 10.1089/jpm.2010.0037. [DOI] [PubMed] [Google Scholar]
- Meert KL, Donaldson AE, Newth CJ, Harrison R, Berger J, Zimmerman J Eunice Kennedy Shriver National Institute of Child Health, Human Development Collaborative Pediatric Critical Care Research Network. Complicated grief and associated risk factors among parents following a child’s death in the pediatric intensive care unit. Archives of Pediatrics & Adolescent Medicine. 2010;164:1045–1051. doi: 10.1001/archpediatrics.2010.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meert KL, Eggly S, Berg RA, Wessel DL, Newth CJ, Shanley TP Eunice Kennedy Shriver National Institute of Child Health, Human Development Collaborative Pediatric Critical Care Research Network. Feasibility and perceived benefits of a framework for physician-parent follow-up meetings after a child’s death in the PICU. Critical Care Medicine. 2014;42:148–157. doi: 10.1097/CCM.0b013e3182a26ff3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meert KL, Eggly S, Berger J, Zimmerman J, Anand KJ, Newth CJ Eunice Kennedy Shriver National Institute of Child Health, Human Development Collaborative Pediatric Critical Care Research Network. Physicians’ experiences and perspectives regarding follow-up meetings with parents after a child’s death in the pediatric intensive care unit. Pediatric Critical Care Medicine. 2011;12:e64–e68. doi: 10.1097/PCC.0b013e3181e89c3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meert KL, Eggly S, Kavanaugh K, Berg RA, Wessel DL, Newth CJ, Park CL. Meaning making during parent-physician bereavement meetings after a child’s death. Health Psychology. doi: 10.1037/hea0000153. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meert KL, Eggly S, Pollack M, Anand KJ, Zimmerman J, Carcillo J National Institute of Child Health, Human Development Collaborative Pediatric Critical Care Research Network. Parents’ perspectives regarding a physician-parent conference after their child’s death in the pediatric intensive care unit. Journal of Pediatrics. 2007;151:50–55. doi: 10.1016/j.jpeds.2007.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL. Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychological Bulletin. 2010;136:257–301. doi: 10.1037/a0018301. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW. Writing about emotional experiences as a therapeutic process. Psychological Science. 1997;8:162–166. [Google Scholar]
- Pennebaker JW. The secret life of pronouns: What our words say about us. New York, NY: Bloomsbury Press; 2011. [Google Scholar]
- Pennebaker JW, Beall SK. Confronting a traumatic event: Toward an understanding of inhibition and disease. Journal of Abnormal Psychology. 1986;95:274–281. doi: 10.1037//0021-843x.95.3.274. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW, Booth RJ, Francis ME. Linguistic inquiry and word count: LIWC. Austin, TX: Pennebaker Conglomerates; 2007. Retrieved from www.LIWC.net. [Google Scholar]
- Pennebaker JW, Chung CK. Expressive writing: Connections to physical and mental health. In: Friedman HS, editor. Oxford handbook of health psychology. New York, NY: Oxford University Press; 2011b. pp. 417–437. [Google Scholar]
- Pennebaker JW, Kiecolt-Glaser JK, Glaser R. Disclosure of traumas and immune function:Health implications for psychotherapy. Journal of Consulting and Clinical Psychology. 1988;56:239–245. doi: 10.1037//0022-006x.56.2.239. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW, Mehl MR, Niederhoffer KG. Psychological aspects of natural language use: our words, our selves. Annual Review of Psychology. 2003;54:547–577. doi: 10.1146/annurev.psych.54.101601.145041. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Brennan RT, Barnett RC. A multivariate hierarchical model for studying psychological change within married couples. Journal of Family Psychology. 1995;9:161–174. [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM 7: Hierarchical linear and nonlinear modeling (Version 7.01) Skokie, IL: Scientific Software International; 2010. [Google Scholar]
- Slatcher RB, Vazire S, Pennebaker JW. Am “I” more important than “we”? Couples’ word use in instant messages. Personal Relationships. 2008;15:407–424. [Google Scholar]
- Tausczik YR, Pennebaker JW. The psychological meaning of words: LIWC and computerized text analysis methods. Journal of Language and Social Psychology. 2010;29:24–54. [Google Scholar]