ABSTRACT
Objectives:
To assess nutritional status, knowledge, practices and lifestyle characteristics of Turks and Caicos Islands (TCI) primary school children.
Subjects and Methods:
Sociodemographic, nutrition knowledge and lifestyle information were collected via an interviewer-assisted questionnaire from grade 5 to 6 participants in a cross-sectional survey; anthropometrics were collected by trained interviewers.
Results:
Two hundred and ninety-seven students (mean age = 10.91 ± 1.01 years; female = 162 [54.5%]; overweight/obese = 121 [40.8%]) participated. Most were born (61.8%) or resided in TCI for more than five years (76.1%). Dietary patterns of breakfast (75.8%); ≥ 2 meals/day (81.2%); ≥ 1 snack/day (65%) and consumption of vegetables (14.5%) and fruits (27.3%) ≥ 2/day were reported. Multinomial regression examined lifestyle and sociodemographic characteristics among body mass index (BMI) categories. Breakfast-eaters were 54% less likely (OR = 0.46; p = 0.025) to be obese; consumers of < 3 meals/day were approximately twice more likely to be obese (OR = 2.074; p = 0.02); participants who “ate out” < 2 times/day (including lunch) were less likely to be overweight (OR = 0.365; p = 0.02). More boys reported strenuous activity (p = 0.05) while more girls reported moderate activity (p = 0.004). No vigorous exercise for ≥ 4 days/week was associated with obesity (OR = 2.0; p = 0.03). Most (> 80%) knew the food groups and that non-communicable diseases were related to diet and obesity (> 70%).
Conclusion:
Findings should inform policy, via the “Health in All” policy initiatives, to develop multisectoral interventions to positively impact children's nutritional status and ultimately eliminate obesogenic environments.
Keywords: Children, knowledge, lifestyle, obesity
RESUMEN
Objetivos:
Evaluar las características nutricionales de status, conocimientos, prácticas y estilo de vida de los niños de escuela primaria de las Islas Turcas y Caicos (TCI).
Sujetos y métodos:
Mediante una encuesta transversal consistente en un cuestionario asistido por un entrevistador, aplicado a participantes de los grados 5 a 6, se recogió información sobre demografía, conocimientos de nutrición, y estilo de vida. Los datos antropométricos fueron recogidos por entrevistadores entrenados.
Resultados:
Participaron doscientos noventa y siete estudiantes (edad promedio = 10.91 ± 1.01 años; hembras = 162 [54.5%]; sobrepeso u obesos = 121 [40.8%]). La mayoría nacieron (61.8%) o residieron en TCI por más de cinco años (76.1%). Se reportaron los patrones dietéticos de desayuno (75.8%); ≥ 2 comidas al día (81.2%); ≥ 1 merienda/día (65%) y el consumo de verduras (14.5%) y frutas (27.3%) ≥ 2 al día. Mediante regresión multinomial se examinaron el estilo de vida y las características sociodemográficas entre las categorías de índice de masa corporal (IMC). Aquellos acostumbrados al desayuno como comida principal, tenían 54% menos de probabilidades (OR = 0.46; p = 0.025) de ser obesos; los que consumían < 3 comidas/día eran aproximadamente dos veces más propensos a ser obesos (OR = 2.074; p = 0.02); los participantes dados a “salir a comer afuera” < 2 veces al día (incluyendo almuerzo) eran menos propensos a tener sobrepeso (OR = 0.365; p = 0.02). Más muchachos reportaron actividades extenuantes (p = 0.05) en tanto que más muchachas reportaron actividades moderadas (p = 0.004). No hubo asociación de ejercicios fuertes ≥ 4 días/semana con la obesidad (OR = 2.0; p = 0.03). La mayoría (> 80%) conocían los grupos de alimentos, y sabían que las enfermedades no trasmisibles no tenían relación con la dieta y la obesidad (> 70%).
Conclusión:
Los hallazgos deben integrarse en las políticas a través de iniciativas como “Salud en todos”, a fin de desarrollar intervenciones multisectoriales para impactar positivamente el estado nutricional de los niños, y en última instancia eliminar ambientes obesogénicos.
INTRODUCTION
The rising prevalence of childhood overweight and obesity, reflected by cross-sectional and secular trend data, has been widely reported globally but especially in developing countries. It is increasingly recognized as a serious public health concern in the latter, which includes Caribbean countries such as the Turks and Caicos Islands [TCI] (1–3).
Globally, about 10% of school-aged children 5–19 years are assessed as overweight or obese. Prevalence rates range from approximately 6% in Pakistan (4) to 42% in Mexico (5). This global increase in the prevalence of overweight and obesity in young people is also observed in the Caribbean (6), including English-speaking Caribbean countries similar to TCI (1, 7, 8).
Several studies have shown the association between excess weight gain in young children and the development of chronic non-communicable diseases (NCDs), including hypertension, Type 2 diabetes and cardiovascular disease (CVD) even into adulthood. Weight gain has also been attributed to various CVD risk factors such as hyperlipidaemia and abnormal glucose tolerance (2, 9–13).
Studies have also shown an association between obesity and frequent psychosocial problems leading to low self-esteem and diminished quality of life (3, 14–18).
As developing countries, including many in the Americas such as Brazil, Mexico, Trinidad and Tobago, and Jamaica, go through nutrition, economic and demographic transitions, the trend of overall increases in weight gain has been attributed, in part, to decreases in physical activity and concomitant increases in sedentary behaviours (19, 20). In the TCI, lifestyle factors such as diet and physical inactivity are modifiable risk factors for NCDs, such as obesity, which is increasingly seen in TCI children (1, 21).
Similar to westernized cultures, the English-speaking Caribbean consumes a dietary pattern that is characterized by consumption of high levels of refined carbohydrates, fats, sugars and a relatively low intake of fibre, fruits and vegetables (22, 23). Evidence shows that the TCI, including the TCI elementary school population, is no exception in this regard (1, 21).
To date, few studies have investigated health and nutritional status indicators of the TCI paediatric population. The first, a 1974 national paediatric survey, investigated the anthropometric and anaemia status of children and adolescents. A high prevalence of anaemia was found among pre-school and school-aged children. It was also found that among the school-aged children, girls were heavier and taller than boys even at age seven years. Children in the TCI were also taller and heavier than those in other Caribbean countries, except Bermuda (24). The second study, the first and only national survey to examine dietary practices, define food habits and assess dietary iron consumption in the TCI, was conducted in 1984. It found marked inter-island variation in dietary patterns and dietary iron scores (25, 26).
There is, therefore, an urgent need to evaluate nutritional status and initiatives designed to encourage healthy lifestyles in young people and utilize the data to inform policy development and to intervene as necessary to halt or reverse the increasing overweight/obesity trend (27).
With overweight/obesity itself an NCD, as well as a modifiable risk factor for many other NCDs such as hypertension, Type 2 diabetes mellitus and CVD, increasing in both adult and paediatric populations globally, there is increasing interest in TCI in investigating and monitoring risk factors for paediatric obesity. These include diet, nutrition knowledge, anthropometry and levels of physical activity with a view to intervening as necessary to improve the nation's short- and long-term health status profile (1, 21).
To this end, this investigation aims to assess the nutritional status and knowledge, and lifestyle characteristics of TCI elementary school children as part of the Student Physical Activity, Nutrition and Knowledge about Seafood Illnesses Survey (SPANKS), conducted on 5th and 6th graders. It will generate evidence to inform health in all policies in general and health policy in particular to facilitate multisectoral intervention needed to eliminate obesogenic environments and positively impact the risk factors of diet, physical inactivity and overweight/obesity that contribute to NCDs in children and into adulthood.
SUBJECTS AND METHODS
The SPANKS study was approved by both the TCI Ministry of Health and Human Services (MOHHS) and the TCI Research Ethics Committee (TCIREC). As a part of that study, a semi-structured interviewer-assisted questionnaire was administered to elementary school students in the TCI. The current cross-sectional study is based on findings from the survey. The survey was administered to students in the six public elementary schools on the islands of Grand Turk (n = 2), Providenciales (n = 3) and South Caicos (n = 1). These three islands account for > 90% of the TCI population (28).
All students enrolled in the 5th and 6th grades of the participating schools (n = 600) were eligible for inclusion in the study. However, only those students whose parents signed informed consent forms and who themselves signed assent forms were allowed to participate. Following this procedure, 297 students completed the survey. This number represented the final sample size and a participation rate of 50%. During the interviews, each question was read aloud in a classroom setting and students completed questionnaires with personal responses.
The study questionnaire, which was piloted at a private elementary school in TCI, included seven sections. However, the current study focusses only on the demographic, nutritional, physical activity and anthropometric sections of the survey.
Demographics: Students were asked about their gender, age, ethnicity, years lived in the TCI and nationality. Given that diet is directly influenced by one's culture (29) and many children in TCI are born in one country but descend from and are raised by parents born in another eg Haiti, mother's (rather than child's) place of birth was used for nationality in analysis performed in the current study.
Nutrition: Dietary intakes were measured using Food Frequency Questionnaires (FFQ) whereby students were asked the frequency with which various foods were consumed on the preceding day [weekdays between Tuesday and Friday were used for survey administration to avoid biases that may result from targeting weekends as the day of recall] (30). Responses for foods in similar food groups were summed to determine the total number of times a food group was consumed. A binomial variable was then created for each of the food groups based on whether or not they met recommended intakes by the Caribbean Food and Nutrition Institute (CFNI): four servings of staples, two servings of fruit, two servings of vegetables, two servings of food from animals and one serving of legumes (31). Given the difficulty in assessing fat consumption in children, fried food consumption (‘none’/‘1 or more’) was assessed. Consistent with the CFNI recommendation, an additional “miscellaneous” group was formed based on the consumption of “sugary” beverages, pastries and candies (‘0– 1’/‘2 or more’).
Dietary habits: Four variables defined dietary pattern for the current study: breakfast consumption (yes/no), number of meals eaten (‘less than 3’/‘3 or more’), number of snacks eaten (‘less than 3’/‘3 or more’) and number of times meals were consumed outside of the home including school lunches (‘less than 2’/‘2 or more’), all of which were based on the previous day's consumption.
Physical activity: Students were asked the number of days per week they engaged in both moderate and vigorous physical activity. Strenuous/vigorous activity lasted 30 minutes and resulted in an accelerated heart rate or induced hard/heavy breathing while moderate activity was defined as exercise that lasted 20 minutes and was less intense. A single measure of physical activity was then created based on whether students met recommended levels: seven days of exercise of at least moderate intensity including at least three days in which the exercise was considered vigorous (32).
Anthropometry: Anthropometric measurements (weights and heights) were conducted for each child by National Epidemiology and Research Unit (NERU) trained interviewers using standard methodologies. Body mass indices (BMIs) were calculated for each child. Using this information, BMI-for-age Z-scores were calculated based on World Health Organization (WHO) age and gender child growth standards (33). Four weight classes were then determined according to the Z score: underweight (Z < −1), normal weight (−1 < Z ≤ 1), overweight (1 < Z ≤ 2) and obese [Z > 2] (34). However, given the small number of underweight students, the underweight and normal weight classes were combined to generate a three category outcome.
Data analysis
Descriptive statistics were obtained for all sociodemographic variables. Bivariate comparisons were then performed on the nutrition, dietary pattern, physical activity and weight category variables by both gender and mother's place of birth using Pearson's Chi-squared (χ2) test. To determine the association between each of the nutrition, dietary pattern and physical activity variables and the weight category variables, separate multinomial logistic regressions were conducted. During this process, two odds ratios were obtained for each variable; one that described the strength of association between the respective variable and overweight compared to under/normal weight and the other that described the strength of the association between the variable and obesity compared to under/normal weight. In each regression, adjustments were made for gender, age, nationality and years lived in the TCI. Significance was assessed at the p = 0.05 level. All analyses were conducted using Statistical Packages for Social Sciences (SPSS) version 20 (35).
RESULTS
The 297 elementary school students (mean age = 10.91 years; SD = 1.01) were primarily of African descent (87.2%). More than half (54.5%) were female. Although almost half of the participants' mothers were born in Haiti (42.5%), the majority of participants resided in the TCI for more than five years (76.1%) and included approximately two-thirds of participants (61.8 %) who, reportedly, were born in TCI.
Table 1 provides dietary intakes/nutrition, dietary patterns and physical activity levels by gender and nationality. A dietary pattern emerged whereby the majority of children did not meet the CFNI recommended levels of servings from the respective food groups (31). These include fruits (72.7%), vegetables (85.5%) and legumes (59.9%). However, most students consumed the recommended frequency of food from animals (80.9%). The majority of students (74.4%) also reported that they did not meet the recommended four servings of staples. Additionally, a large majority of students ate at least one fried food (81.1%) and two or more miscellaneous (sugar based) foods (91.9%) on the index day.
Table 1. Distribution of nutrition, dietary pattern and physical activity variables by gender and nationality among students completing the survey.
| Variable | Total n = 297 |
TCI n = 80 |
Haitian n = 122 |
Other n = 85 |
p | Male n = 135 |
Female n = 162 |
p | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Nutrition | ||||||||||
| Staples | Less than 4 times | 74.4 | 75.9 | 74.8 | 75.3 | 0.98 | 69.0 | 78.8 | 0.06 | |
| 4 or more 4 times | 25.6 | 24.1 | 25.2 | 24.7 | 31.0 | 21.0 | ||||
| Fruits | Less than 2 times | 72.7 | 77.5 | 73.0 | 64.7 | 0.18 | 71.1 | 74.1 | 0.57 | |
| Fruits | 2 or more times | 27.3 | 22.8 | 27.0 | 35.3 | 28.9 | 26.9 | |||
| Vegetables | Less than 2 times | 85.5 | 88.8 | 80.3 | 88.2 | 0.16 | 84.4 | 86.4 | 0.63 | |
| 2 or more times | 14.5 | 11.2 | 19.7 | 11.8 | 15.6 | 13.6 | ||||
| Legumes | None | 59.9 | 74.4 | 47.1 | 62.4 | 0.001 | 57.8 | 0.42 | ||
| 1 or more | 40.1 | 25.6 | 52.9 | 37.6 | 62.4 | 37.6 | 42.4 | |||
| Food from animals | Less than 3 times | 19.1 | 15.2 | 21.7 | 20.0 | 0.52 | 17.3 | 20.6 | 0.47 | |
| 3 or more times | 80.9 | 84.8 | 78.3 | 80.0 | 82.7 | 79.4 | ||||
| Fried foods | None | 18.9 | 13.8 | 25.4 | 16.5 | 0.09 | 20 | 17.9 | 0.57 | |
| 1 or more | 81.1 | 86.2 | 74.6 | 83.5 | 80 | 82.1 | ||||
| Miscellaneous§ | 0 –1 | 8.1 | 6.2 | 11.3 | 6.2 | 0.33 | 10.9 | 5.8 | 0.11 | |
| 2 or more | 91.9 | 93.8 | 88.7 | 93.8 | 89.1 | 94.2 | ||||
| Dietary pattern | ||||||||||
| Breakfast | Yes | 76.0 | 80.0 | 74.4 | 74.1 | 0.60 | 76.1 | 75.9 | 0.97 | |
| No | 24.0 | 20.0 | 25.6 | 25.9 | 23.9 | 24.1 | ||||
| Number of meals | Less than 3 times | 43.4 | 37.5 | 47.5 | 41.2 | 0.34 | 51.1 | 37.0 | 0.02 | |
| 3 or more times | 58.7 | 62.5 | 52.5 | 58.8 | 48.9 | 63.0 | ||||
| Number of snacks | Less than 3 times | 84.8 | 81.2 | 84.3 | 89.4 | 0.33 | 85.8 | 84.6 | 0.76 | |
| 3 or more times | 14.8 | 18.8 | 15.7 | 10.6 | 14.2 | 15.4 | ||||
| Number of times eaten out | Less than 2 times | 39.1 | 38.8 | 35.2 | 42.4 | 0.58 | 44.4 | 34.1 | 0.08 | |
| 2 or more times | 60.9 | 61.3 | 64.8 | 57.6 | 55.6 | 65.9 | ||||
| Physical activity | ||||||||||
| Moderate physical activity | Less than recommended* | 53.5 | 45.6 | 59.8 | 54.1 | 0.14 | 51.9 | 55.3 | 0.56 | |
| Recommended levels | 46.1 | 54.5 | 40.2 | 45.9 | 48.1 | 44.7 | ||||
Represents sugary beverages, desserts, pastries and candies.
Recommended levels = 7 days of exercise of at least moderate intensity including at least 3 days in which the exercise was considered vigorous
Dietary intake did not differ significantly by nationality or by gender with the exception that Haitian children were significantly more likely to consume legumes (χ2 = 15.09; p = 0.001).
With regard to participants' dietary pattern, breakfast was consumed by a large majority of participants (76.0%) and most children ate at least three meals (58.7%) a day. Most children, however, ate less than three snacks (84.8%) but ate out at least two times, including lunch (60.9%) [Table 1]. The only significant difference observed with regard to dietary pattern was that girls were significantly more likely to eat three or more meals a day than boys (χ2 = 5.94; p = 0.02).
Most students also did not engage in the recommended levels of physical activity (53.5%), irrespective of gender and nationality. However, boys were significantly more likely to meet the minimum threshold of engaging in vigorous exercise (p = 0.02).
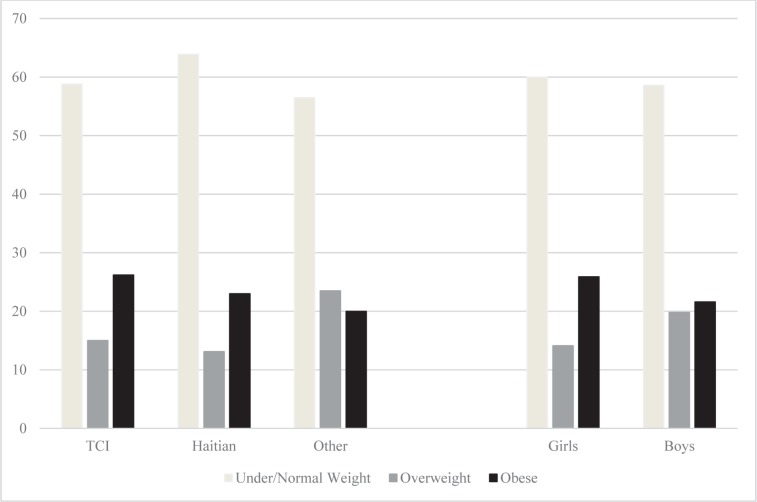
Assessment of obesity status (Figure) revealed that whereas half of the students (n = 149; 50.1%) were of normal weight, 51 (17.2%) were overweight, 70 (23.6%) were categorized as obese and 27 (9.1%) were classified as underweight. Few significant differences in weight class were observed by gender and nationality. Boys (23.5%) and girls (28.3%) from countries other than Haiti and TCI were most likely to be overweight, while girls from TCI were most likely to be obese (26.1%).
Figure. Bar chart showing the proportion of students characterized as under/normal weight, overweight and obese by gender and by nationality.
Table 2 presents the results from multinomial logistic regression that assessed the relationship between diet/nutrition, dietary pattern and physical activity variables and obesity status. When gender, age, nationality and number of years in TCI were adjusted, no significant association was found between weight class and any of the dietary intake variables. However, significant associations were found according to dietary pattern. It was found that the students who ate breakfast were 54% less likely (OR = 0.46; p = 0.025) to be obese compared to those that did not eat breakfast. Additionally, persons who ate less than three meals were approximately twice more likely to be obese than those who ate three or more meals on the day before (OR = 2.074; p = 0.02). Finally, students who reportedly ate out less than twice (including lunch) were less likely to be overweight compared to their counterparts who ate out two or more times (OR = 0.365; p = 0.02).
Table 2. Results from multinomial logistic regression that assessed the relationship between each of the nutrition, dietary pattern and physical activity variables and overweight and obesity.
| Variable | Overweight | Obese | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | p | 95%CI | OR | p | 95%CI | |||
| Nutrition | ||||||||
| Staples | Less than 4 times | 2.45 | 0.06 | 0.95 – 6.31 | 2.06 | 0.07 | 0.95 – 4.46 | |
| 4 or more times | --- | --- | --- | --- | --- | --- | ||
| Fruits | Less than 2 times | 2.23 | 0.09 | 0.89 – 5.56 | 0.96 | 0.91 | 0.49 – 1.88 | |
| 2 or more times | --- | --- | --- | --- | --- | --- | ||
| Vegetables | Less than 2 times | 3.77 | 0.08 | 0.85 – 16.72 | 1.05 | 0.92 | 0.47 – 2.34 | |
| 2 or more times | --- | --- | --- | --- | --- | --- | ||
| Legumes | None | 1.01 | 0.98 | 0.49 – 2.08 | 0.74 | 0.351 | 0.39 – 1.37 | |
| 1 or more | --- | --- | --- | --- | --- | --- | ||
| Food from animals | Less than 3 times | 1.83 | 0.17 | 0.77 – 4.31 | 0.99 | 0.28 | 0.91 – 3.23 | |
| 3 or more times | --- | --- | --- | --- | --- | --- | ||
| Fried food | None | 1.30 | 0.57 | 0.53 – 3.20 | 1.43 | 0.36 | 0.67 – 3.04 | |
| 1 or more times | --- | --- | --- | --- | --- | --- | ||
| Miscellaneous§ | 0 – 1 | 0.71 | 0.67 | 0.15 – 3.43 | 2.09 | 0.14 | 0.78 – 5.57 | |
| 2 or more times | --- | --- | --- | --- | --- | --- | ||
| Dietary pattern | ||||||||
| Breakfast | Yes | 0.78 | 0.56 | 0.34 – 1.79 | 0.46 | 0.03 | 0.23 – 0.91 | |
| No | --- | --- | --- | --- | --- | --- | ||
| Number of meals | Less than 3 times | 1.27 | 0.52 | 0.61 – 2.63 | 2.07 | 0.02 | 1.11 – 3.88 | |
| 3 or more times | --- | --- | --- | --- | --- | --- | ||
| Number of snacks | Less than 3 times | 0.66 | 0.25 | 0.32 – 1.98 | 1.79 | 0.23 | 0.69 – 4.63 | |
| 3 or more times | --- | --- | --- | --- | --- | --- | ||
| Number of times eaten out | Less than 2 times | 0.37 | 0.02 | 0.15 – 0.88 | 0.69 | 0.38 | 0.30 – 1.60 | |
| 2 or more times | --- | --- | --- | --- | --- | --- | ||
| Physical activity | ||||||||
| Physical activity | Less than recommended | 0.85 | 0.66 | 0.412 – 1.75 | 1.41 | 0.28 | 0.76 – 2.65 | |
| Recommended | --- | --- | --- | --- | --- | |||
--- Represents the reference category
Represents sugary beverages, desserts, pastries and candies
With regard to physical activity, no significant association was found between weight class and whether or not students met recommended physical activity levels. However, children who did not exercise vigorously for at least four days were significantly more likely to be obese than those who did (OR = 2.0; p = 0.03). Overall, computer/internet use of 3.81 ± 1.97 hours/day and video/TV games use of 3.27 ± 2.24 hours/day were reported by student participants.
DISCUSSION
The findings of this study are similar to the 16% at risk and 15% overweight found for the 2004–2006 entrants to one high school in TCI (35) and the more recent TCI study of cardiovascular disease risk factors in children entering high school during 2008–2013, which found two in five children were either at risk or overweight (1, 21). Findings are also markedly similar to the 22% of American children and adolescents classified as overweight in NHANESIII (36).
One study showed that as many as 70% of obese children aged 10–13 years old become obese adults (37). Indeed, an increase in CVD risk factor levels (ie increases in the likelihood of developing CVD) are listed as intermediate on the three-level scale of consequences (immediate, intermediate and long-term) that are adjudged to result from childhood and adolescent obesity (38).
The findings of this survey of unacceptable levels of overweight/obesity (40.8%) coupled with suboptimal levels of fruit and vegetable consumption, suboptimal levels of physical activity, and relationships between obesity status, physical activity and dietary consumption patterns among elementary school students confirm what has become a trend globally, regionally and in TCI.
The findings are consistent with others in the published literature from other Caribbean countries such as Jamaica and elsewhere. A study of children aged 10 years in Quebec, Canada, found approximately one-quarter (26%) of children were overweight/obese (38). Similar reports of 16% of children and adolescents classified as overweight and 34% at risk of overweight came from the United States of America (39, 40), while one-tenth (11%) of children 10–11 years old from Jamaica were classified as overweight or obese (38).
Development of paediatric obesity is multifactorial and contributing factors may include genetics, diet and lifestyles, social, economic and cultural factors (income, education), behaviour (eating patterns, cultural norms regarding food), and environmental factors (food availability, and economic factors). Hence, a multifaceted approach is needed to address this problem; the desirable outcome being the prevention of childhood obesity. The identification of children at risk and providing interventions designed to prevent inappropriate weight gain are important (38).
Whereas the immediate consequences of paediatric obesity include higher total cholesterol, high-density lipoprotein (HDL) and triglyceride levels, insulin resistance and increases in Type 2 diabetes, long-term consequences include significant increases in morbidity and mortality in adulthood (41).
It is generally accepted that overweight in adulthood is a risk factor for health problems including NCDs such as hypertension, heart disease and Type 2 diabetes. Childhood overweight does not necessarily result in adult health risk (42). However, obesity during adolescence increases long-term (approximately 50-year) risk of morbidity and mortality in adulthood, independent of adult obesity status (43).
This survey, in addition to assessing anthropometric status, also examined nutrition knowledge and practices. It found that despite knowing the different food groups, the children were not clear as to the relative contributions each group should make to one's daily dietary intake.
The findings also demonstrated differences in lifestyle characteristics based on the nationality of the mothers and socio-economic status. Also, even though the majority of children reported they consumed breakfast, the quality of the breakfast was not assessed.
Whereas efforts were made to minimize biases by using standard procedures, various limitations existed. Dietary recall of the previous day as a means of assessing dietary intake has its inherent limitations. However, it has been found to be the better choice for young children compared to (a) the traditional FFQ, which solicits information about dietary intake over a longer, specified period of time, eg past six months, or (b) usual intakes. This study used a modified FFQ where children were asked about frequency of consumption of a list of foods during the previous day. Information on serving sizes was not collected, and is also a limitation.
The information collected on physical activity has similar limitations as it relates to the children's ability to recall and quantify the frequency and intensity of physical activity engaged in. Even though anthropometrics were done by trained personnel following standard procedures, thereby minimizing bias, the BMIs calculated and used for weight category/class assignment did not take into consideration differences in body frame and pubertal stage of this age group; the latter could have a major impact on children's BMI (1, 21).
Despite the relatively small sample size (n = 297) and response rate of 50%, our findings as it relates to obesity status was consistent with findings of other ongoing studies of TCI children, which lends credibility to our findings.
This study is timely and highlights the need for a multisectoral approach to the global childhood obesity crisis. Additional investigations of the socio-economic status, parental involvement and dietary intakes of the children in TCI to enable targeted interventions to take place are extremely important. Focus on nutrition education targeted at parents and children and an emphasis on lifestyle modification by infusing health and nutrition messages into the elementary school's curriculum (44) is imperative to positively impact nutritional status of the paediatric and future adult generations of TCI and Caribbean nationals.
Findings could inform development of “Health in Policies” in recognition of the need for a multisectoral approach to positively impact nutritional practices and ultimately positively impact the elimination of obesogenic environments and positively impact the global childhood obesity crisis.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the financial support for this project provided by the Global Health Research Initiative (GHRI) by way of a Global Health Leadership Award #103460-071 to Dr Terese Maitland and the assistance and collaboration provided by the Director and Deputy Director of the Department of Education, Turks and Caicos Islands, and in particular the principals and staff of the Eliza Simons, Ona Glinton, Iris Stubbs, Ianthe Pratt, Osetta Jolly and Enid Capron Public Primary Schools for their cooperation and participation, and Newman's Preparatory (Grand Turk) for serving as the pilot school. Also, colleagues within the Ministry of Health and Human Services (MOHHS), Mr Michael Williams of TCI Hospital and the parents and students from the aforementioned schools are thanked for their assistance, patience and understanding. The survey was conducted by the National Epidemiology and Research Unit (NERU) of the MOHHS of TCI.
REFERENCES
- 1.Maitland TE, Malcolm S, Handfield S, Malcolm K. Trends in obesity and other cardiovascular disease risk factors among elementary school children in the Turks and Caicos Islands (2008–2013) West Indian Med J. 2014;63(Suppl 2):48–48. [Google Scholar]
- 2.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–525. [PubMed] [Google Scholar]
- 3.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obesity. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 4.Jafar TH, Qadri Z, Islam M, Hatcher J, Bhutta ZA, Chaturvedi N. Rise in childhood obesity with persistently high rates of undernutrition among urban school-aged Indo-Asian children. Arch Dis Child. 2008;93:373–378. doi: 10.1136/adc.2007.125641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moraes SA, Beltrán Rosas J, Mondini L, Freitas IC. Prevalence of overweight and obesity, and associated factors in school children from urban area in Chilpancingo, Guerrero, Mexico, 2004. Cad Saude Publica. 2006;22:1289–1301. doi: 10.1590/s0102-311x2006000600018. [DOI] [PubMed] [Google Scholar]
- 6.Schwiebbe L, van Rest J, Verhagen E, Visser RW, Holthe JK, Hirasing RA. Childhood obesity in the Caribbean. West Indian Med J. 2011;60:442–445. [PubMed] [Google Scholar]
- 7.Gaskin PS, Walker SP. Obesity in a cohort of black Jamaican children as estimated by BMI and other indices of adiposity. Eur J Clin Nutr. 2003;57:420–426. doi: 10.1038/sj.ejcn.1601564. [DOI] [PubMed] [Google Scholar]
- 8.Gulliford MC, Nunes C, Rocke B. Food insecurity, weight control practices and body mass index in adolescents. Public Health Nutr. 2006;9:570–574. doi: 10.1079/phn2005886. [DOI] [PubMed] [Google Scholar]
- 9.Ferguson M, Gutin B, Owens S, Litaker M, Tracy R, Allison J. Fat distribution and haemostatic measures in obese children. Am J Clin Nutr. 1998;46:1136–1140. doi: 10.1093/ajcn/67.6.1136. [DOI] [PubMed] [Google Scholar]
- 10.Erikson J, Forester T, Osmond C, Barker D. Early rebound in childhood and risk of type 2 diabetes in adult life. Diabetologia. 2003;46:190–194. doi: 10.1007/s00125-002-1012-5. [DOI] [PubMed] [Google Scholar]
- 11.Ford ES, Galuska DA, Gillespe C, Will JC, Giles WH, Dietz WH. C-reactive protein and body mass index in children: findings from the Third National Health and Examination Survey, 1988–94. J Pediatr. 2001;138:486–492. doi: 10.1067/mpd.2001.112898. [DOI] [PubMed] [Google Scholar]
- 12.Tounian P, Aggoun Y, Dubern B, Varille V, Guy-Grand B, Sidi D, et al. Presence of increased stiffness of the common carotid artery and endothelial dysfunction in severely obese children: a perspective study. Lancet. 2001;358:1400–1404. doi: 10.1016/S0140-6736(01)06525-4. [DOI] [PubMed] [Google Scholar]
- 13.Han JC, Lawlor DA, Kimm S. Childhood obesity. Lancet. 2010;375:1737–1748. doi: 10.1016/S0140-6736(10)60171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moyer AV, Klein JD, Ockene JK, Teutsch SM, Jhonson MS, Allan JD. Screening for overweight in children and adolescence: where is the evidence? A commentary by the Childhood Obesity Working Group of the US Preventive Services Task Force. Pediatrics. 2005;116:235–238. doi: 10.1542/peds.2005-0305. [DOI] [PubMed] [Google Scholar]
- 15.Benson L, Baer HJ, Kaelber DC. Trends in the diagnosis of overweight and obesity in children and adolescents: 1999–2007. Pediatrics. 2009;123:e153–e158. doi: 10.1542/peds.2008-1408. [DOI] [PubMed] [Google Scholar]
- 16.Whitlock EP, Williams SB, Gold R, Smith PR, Slipman SA. Screening and interventions for childhood overweight: a summary of evidence for the US Prevention Services Task Force. Pediatrics. 2005;116:e125–e144. doi: 10.1542/peds.2005-0242. [DOI] [PubMed] [Google Scholar]
- 17.Bua J, Olsen LW, Sorensen TI. Secular trends in childhood obesity in Denmark during 50 years in relation to economic growth. Obesity. 2007;15:977–985. doi: 10.1038/oby.2007.603. [DOI] [PubMed] [Google Scholar]
- 18.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA. 2001;286:2845–2848. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- 19.Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5:104–104. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- 20.Wareham N, van Sluijs E, Ekelund U. Physical activity and obesity prevention: a review of the current evidence. Proc Nutr Soc. 2005;64:229–247. doi: 10.1079/pns2005423. [DOI] [PubMed] [Google Scholar]
- 21.Maitland TE, Ramsay C, Malcolm S, Nash K, Ewing R. Risk factors for cardiovascular disease in youth from Turks and Caicos Islands. West Indian Med J. 2009;58(Suppl 2):38–38. [Google Scholar]
- 22.Caribbean Food and Nutrition Institute Childhood obesity. Nyam News. 2005;1:2–2. [Google Scholar]
- 23.Martorell R, Khan LK, Hughes ML, Grummer-Strawn LM. Obesity in Latin American women and children. J Nutr. 1998;128:1464–1473. doi: 10.1093/jn/128.9.1464. [DOI] [PubMed] [Google Scholar]
- 24.Cohen MP, Morgan P, Baker P. The nutritional status of children in the Turks and Caicos Islands. West Indian Med J. 1974;23:937–937. [PubMed] [Google Scholar]
- 25.Maitland TE. Variation in dietary patterns in the Turks and Caicos [MSc thesis] Kingston, Jamaica: University of the West Indies; 1985. [Google Scholar]
- 26.Maitland TE. Dietary habits, diversity, and the indigenous diet of the Turks and Caicos Islands: implications for island-specific nutrition intervention. West Indian Med J. 2006;55:374–386. doi: 10.1590/s0043-31442006000600003. [DOI] [PubMed] [Google Scholar]
- 27.Biddle S, Mutrie N. Psychology of physical activity. 2nd ed. London: Routledge; 2008. [Google Scholar]
- 28.Turks and Caicos Islands Governor's Office Preliminary 2012 TCI census data published. Grand Turk, Turks and Caicos Islands: Strategic Policy and Planning Unit. 2012. [[cited 2013 March 6]]. Available from: http://turksandcaicosislands.fco.gov.uk/en/news/?view=News&id=796072382.
- 29.Gaskin PS, Lai P, Guy D, Knight J, Jackson M, Nickson AL. Diet, physical activity, weight status, and culture in a sample of children from the developing world. J Nutr Metab. 2012;242875:25–32. doi: 10.1155/2012/242875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kirkpatrick SI, Guenther PM, Dodd KW. The effects of recall sequence/mode and day of week on the estimation of usual intake from 24-hour recall data: an analysis of the 2003–2004 National Health and Nutrition Examination Survey. FASEB Journal. 2013;27:621–625. [Google Scholar]
- 31.Caribbean Food and Nutrition Institute (CFNI) Food guide. Cajanus. 2010;39:110–122. [Google Scholar]
- 32.World Health Organization (WHO) Global recommendations on physical activity for health. Geneva, Switzerland: WHO; 2012. [Google Scholar]
- 33.World Health Organization Multicentre Growth Reference Study Group . WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height, and body mass index-for-age (5–19 years): methods and development. Geneva: WHO; 2006. [Google Scholar]
- 34.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:649–732. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maitland TE, Ramsay C, Malcolm S, Nash K, Ewing R. Anaemia in the Turks and Caicos Islands School Children: then (1974) versus now (2008) West Indian Med J. 2009;58:21–21. [Google Scholar]
- 36.Strauss RS, Knight J. Influence of home environment on the development of obesity in children. Pediatrics. 1999;103:e85–e85. doi: 10.1542/peds.103.6.e85. [DOI] [PubMed] [Google Scholar]
- 37.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 38.Dubois L, Francis D, Burnier D, Tatone-Tokuda F, Girard M, Gordon-Strachan G, et al. Household food insecurity and childhood overweight in Jamaica and Québec: a gender-based analysis. BMC Public Health. 2011;11:199–199. doi: 10.1186/1471-2458-11-199. Available from: http://www.biomedcentral.com/1471-2458/11/199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obesity. 1999;23:S2–S11. doi: 10.1038/sj.ijo.0800852. [DOI] [PubMed] [Google Scholar]
- 40.Wang Y, Beydoun MA. The obesity epidemic in the United States – gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 41.Lewis MT, Schaalma H, Jansen M, Mur-veeman I, Leger L, DeVries N. Development of a collaborative model to improve school health promotion in the Netherlands. Health Promot Int. 2005;20:296–305. doi: 10.1093/heapro/dai004. [DOI] [PubMed] [Google Scholar]
- 42.Wright CM, Parker L, Lamont D, Craft AW. Implications of childhood obesity for adult health: findings from thousand families cohort study. BMJ. 2001;323:1280–1284. doi: 10.1136/bmj.323.7324.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents. N Engl J Med. 1992;327:1350–1355. doi: 10.1056/NEJM199211053271904. [DOI] [PubMed] [Google Scholar]
- 44.Henry C, Kalyn B, Ramdath D, Mangroo S. Involving stakeholders in integrating health and nutrition into the school curriculum. In: Bacsu J, Smith FM, editors. Innovations in knowledge translation: the SPHERU KT Casebook. Ottawa, Ontario: Canadian Institutes of Health Research; 2011. [Google Scholar]