Abstract
Background
Many studies have reported an association between glycated hemoglobin A1c (HbA1c) and metabolic syndrome (MetS) in non-diabetes patients. Each component of MetS is in fact related to chronic kidney disease (CKD) incidence and progression. Therefore, HbA1c in non-diabetic mellitus (DM) may be intrinsically associated with the prevalence of CKD. The hypothesis of the present study was that high HbA1c in non-DM patients is associated with CKD.
Patients and Methods
The total number of participants in this study was 24,594. The participants were divided into three groups according to their HbA1c levels: a Low group (<5.7% or <39 mmol/mol), a Middle group (5.7–6.0% or 39–42 mmol/mol), and a High group (>6.0% or >42 mmol/mol). The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation.
Results
The number of participants allocated to the Low, Middle, and High groups was 8,651, 4,634, and 1,387, respectively. Linear regression analyses were performed to evaluate the association between variables. Standardized β ± standard error was 0.25 ± 0.22 for waist circumference, 0.44 ± 0.20 for fasting glucose, –0.14 ± 0.30 for high-density lipoprotein cholesterol levels, 0.15 ± 2.31 for triglyceride levels, 0.21 ± 0.00 for systolic blood pressure, 0.10 ± 0.00 for diastolic blood pressure, and –0.22 ± 0.42 for eGFR (P < 0.001 for all variables). eGFR in non-diabetes participants was inversely associated with the HbA1c level, where eGFR decreased as HbA1c levels increased. Standardized βs were –0.04 ± 0.42 in multivariable analysis (P < 0.001). The proportion of participants with only MetS, only CKD, or both MetS and CKD was higher in the High group than in the Low and Middle groups.
Conclusion
High HbA1c in non-DM patients may be associated with CKD. Renal function in patients with high HbA1c levels may need to be monitored.
Background
Chronic kidney disease (CKD) is a widely recognized public health issue and associated with high morbidity and mortality when compared to the non-CKD population [1,2]. The United States Real Data System 2014 Annual Data Report showed that CKD occurs in approximately 13.6% of the general population [3]. Indeed, the prevalence of CKD appears to be rising rapidly with increased life expectancy. Overall Medicare expenditures for CKD were $44,581 million in 2012 [3]. Screening for and effective monitoring of CKD are essential for increasing patient quality of life and decreasing the public health burden.
Glycated hemoglobin (HbA1c) is an important indicator for long-term glucose control and has recently been recommended for use in the diagnosis of diabetes mellitus (DM) by the American Diabetes Association (ADA) [4]. However, the use of HbA1c for identifying pre-diabetes is a controversial topic [5]. In 2015, the ADA suggested that an HbA1c of 5.7–6.4% (39–46 mmol/mol) is reasonable for the diagnosis of pre-diabetes and that patients with HbA1c > 6.0% (>42 mmol/mol) should be considered to be at very high risk for DM [4]. Although the clinical significance of HbA1c as a surrogate marker of metabolic syndrome (MetS) has not yet been fully examined, many studies have reported an association between HbA1c and MetS in non-DM patients [6–8]. Each component of MetS is in fact related to CKD incidence and progression [9]. Therefore, HbA1c in non-DM may be intrinsically associated with the prevalence of CKD. The aim of the present study was to evaluate the clinical association between HbA1c and CKD in non-DM patients. The hypothesis of the present study was that high HbA1c in non-DM patients is associated with CKD.
Patients and Methods
Study population
Data from the Korean National Health and Nutrition Examination Survey (KNHANES 2011–2013) were used for this analysis. The KNHANES is a nationwide, multi-stage, stratified survey of a representative sample of the South Korean population and is conducted by the Korea Centers for Disease Control and Prevention. The total number of participants from KNHANES analyzed in this study was 24,594. Participants were excluded from the present study based on the following criteria: data could not be provided for HbA1c (n = 2,350) or renal function (n = 2) or participants were younger than 18 years of age (n = 5,385) or had DM (defined as a self-reported history of a DM diagnosis, a fasting glucose level of ≥126 mg/dL, or HbA1c ≥ 6.5% (≥48 mmol/mol; n = 2,185). As a result, 14,672 participants were ultimately included in this study. Ethical approval for this study was obtained from the institutional review board of Yeungnam University Hospital (2015-04-004). The board waived the need for informed consent, as the subjects’ records and information were anonymized and de-identified prior to analysis.
Study variables
Clinical and laboratory data collected during clinical examination included the following: age, sex, serum creatinine (mg/dL), body mass index (BMI, kg/m2), waist circumference (WC, cm), HbA1c (%, mmol/mol), fasting blood glucose (mg/dL), total cholesterol (mg/dL), high-density lipoprotein (HDL) cholesterol levels (mg/dL), triglyceride levels (mg/dL), systolic blood pressure (mmHg), diastolic blood pressure (mmHg), smoking status, alcohol intake, and levels of physical activity.
HbA1c levels were measured using a high performance liquid chromatography system (HLC-723G7; Tosoh Co., Tokyo, Japan). In the present study, the participants were divided into three groups according to their HbA1c levels: a Low group (<5.7% or <39 mmol/mol), a Middle group (5.7–6.0% or 39–42 mmol/mol), and a High group (>6.0% or >42 mmol/mol). Serum creatinine levels were measured using a Hitachi Automatic Analyzer (alkaline picrate, Jaffé kinetic). The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [10]. CKD was defined as an eGFR <60 mL/min/1.73 m2. Urine albumin level was measured from random samples using a turbidimetric immunoassay (Hitachi Automatic Analyzer 7600, Hitachi). Urine creatinine level was measured using a colorimetric method (Hitachi Automatic Analyzer 7600, Hitachi). Urine albumin and creatinine concentrations were measured in the same laboratory for all surveys. The inter-assay coefficient of variation for all laboratory work was consistenly low (<3.1%). The urine albumin-creatinine ratio (UACR) was calculated in mg per g of creatinine (mg/g). Albuminuria was defined as UACR ≥30 mg/g.
Patients were classified according to smoking status as current smokers, ex-smokers, or non-smokers. Alcohol intake was defined using the Korean version of ‘standard drinking’ based on the WHO classification [11,12]. Alcohol intake was classified into 3 categories: abstinence (no consumption of alcohol within the last year); moderate drinking (women: 0.1–19.99 g pure alcohol/day; men: 0.1–39.99 g pure alcohol/day), and heavy drinking (women: ≥20 g pure alcohol/day; men: ≥40 g pure alcohol/day). Physical activity was assessed by the presence of exercise. The presence of exercise was defined as moderate activity for more than 30 min/day, for 5 days/week or intense activity for more than 20 min/day, for 3 days/week, or walking more than 30 min/day, for 5 days/week. Coronary artery disease (CAD) was defined as a self-reported history of angina or myocardial infarction. Cerebrovascular accident (CVA) was defined as a self-reported history of stroke.
MetS was defined according to the Adult Treatment Panel III criteria using the modified cutoff values for Asian populations as suggested by the Asia-Pacific guidelines [13,14]. Briefly, elevated blood glucose was defined as a fasting blood glucose level ≥100 mg/dL or a self-reported history of DM. Elevated blood pressure was defined as a systolic or diastolic blood pressure ≥130/85 mmHg and a self-reported history of hypertension. A low HDL cholesterol level was defined as <40 mg/dL in men and <50 mg/dL in women. Elevated triglyceride levels were defined as a serum triglyceride level of ≥150 mg/dL. Abdominal obesity was defined as a WC >90 cm in men and >80 cm in women. MetS was defined as the presence of ≥3 components of MetS.
Statistical analyses
The data were analyzed using the Statistical package for the Social Sciences software package (SPSS v.21, Chicago, IL., USA). Categorical variables were expressed as both counts and percentages. Continuous variables were expressed as the mean ± standard deviation (SD). UACR was a non-parametric variable expressed as a median (95% CI), and was compared using the Kruskal-Wallis test. The Pearson’s χ2 or Fisher’s exact test was used to analyze categorical variables. For continuous variables, means were compared using a one-way analysis of variance. Correlations were analyzed in order to assess the strength of the relationship between continuous variables. Linear regression analysis was performed to assess independent predictors of eGFR or number of MetS components. Variance inflation factor was used to identify multicollinearity for the multivariable linear regression model. Variance inflation factor greater than 10 was not accepted. Logistic regression analyses were used for estimating the odds ratios (OR) and 95% confidence intervals (CI), which were then applied towards determining the relationship between HbA1c and CKD or MetS.
Confounders were defined by their likelihood of preceding or contributing to the development of MetS or CKD. The selection of confounder was based on previous literatures [15,16]. For MetS, the covariates were HbA1c, age, sex, BMI, alcohol intake, smoking status, and physical activity. For CKD, the covariates were HbA1c, age, sex, BMI, alcohol intake, smoking status, physical activity, CAD, CVA, WC, HDL cholesterol levels, triglyceride levels, systolic blood pressure, and diastolic blood pressure. Discrimination–which is the ability of the model to differentiate between participants who have CKD or MetS and those who do not–was examined using the area under the receiver operating characteristic (AUROC) curve. AUROC analysis was also performed in order to calculate cutoff values, sensitivity, and specificity. Optimal cutoff risk point was defined as the maximum Youden index in the AUROC. The AUROC was calculated using the MedCalc software package (v.11.6.1.0, MedCalc, Mariakerke, Belgium). We also calculated the integrated discrimination improvement (IDI) and the net reclassification improvement (NRI) with a category-free option among models, following the methodology of Penica et al. [17,18]. A restricted cubic spline curve was used to evaluate non-linear relationships between the HbA1c level and CKD, which was adjusted for age and sex. The restricted cubic spline curve was plotted using statistical software SAS version 9.4 (SAS Campus Drive, Cary, NC, USA). A P-value less than 0.05 was considered statistically significant.
Results
Clinical characteristics of participants
The number of participants allocated to the Low, Middle, and High groups was 8,651, 4,634, and 1,387, respectively (Table 1). Age, BMI, WC, eGFR, total cholesterol, fasting blood glucose, triglyceride levels, and systolic and diastolic blood pressure were higher in the High group than either the Low or Middle group.
Table 1. Clinical characteristics of participants by HbA1c level.
| Low (n = 8,651) | Middle (n = 3,865) | High (n = 2,156) | P-value* | |
|---|---|---|---|---|
| Age (years) | 43.2 ± 15.6 | 53.2 ± 15.4 | 59.7 ± 12.6 | <0.001 |
| Sex (male, %) | 3,608 (41.7%) | 2,037 (44.0%) | 563 (40.6%) | 0.017 |
| HbA1c (%, mmol/mol) | 5.35 ± 0.22, 35 ± 2 | 5.82 ± 0.11, 40 ± 1 | 6.20 ± 0.11, 44 ± 1 | <0.001 |
| Body mass index (kg/m2) | 23.0 ± 3.2 | 24.0 ± 3.3 | 24.9 ± 3.3 | <0.001 |
| Creatinine (mg/dL) | 0.82 ± 0.19 | 0.84 ± 0.18 | 0.86 ± 0.37 | <0.001 |
| Waist circumference (cm) | 78.3 ± 9.5 | 81.9 ± 9.3 | 84.6 ± 9.2 | <0.001 |
| Total cholesterol (mg/dL) | 184.0 ± 33.7 | 196.8 ± 36.0 | 199.4 ± 39.8 | <0.001 |
| Fasting blood glucose (mg/dL) | 90.1 ± 7.9 | 95.3 ± 8.9 | 102.1 ± 10.2 | <0.001 |
| Triglyceride (mg/dL) | 115.3 ± 91.3 | 138.6 ± 105.1 | 152.4 ± 104.5 | <0.001 |
| High density lipoprotein (mg/dL) | 54.6 ± 12.9 | 51.9 ± 11.9 | 49.6 ± 11.7 | <0.001 |
| Systolic blood pressure (mmHg) | 114.9 ± 15.8 | 120.0 ± 16.8 | 124.6 ± 17.0 | <0.001 |
| Diastolic blood pressure (mmHg) | 74.8 ± 10.4 | 76.3 ± 10.3 | 77.0 ± 10.4 | <0.001 |
| Physical activity (%) | 3897 (45.0%) | 1,993 (45.2%) | 543 (40.9%) | <0.001 |
| Coronary artery disease (%) | 72 (0.8%) | 113 (2.4%) | 70 (5.0%) | <0.001 |
| Cerebrovascular accident (%) | 65 (0.8%) | 87 (1.9%) | 45 (3.2%) | <0.001 |
| Alcohol intake | <0.001 | |||
| Abstinence | 1866 (21.6%) | 1,334 (28.8%) | 505 (36.4%) | |
| Moderate drinking | 6071 (70.2%) | 2,929 (63.2%) | 784 (56.5%) | |
| Heavy drinking | 382 (4.4%) | 147 (3.2%) | 39 (2.8%) | |
| Unknown | 332 (3.8%) | 224 (4.8%) | 59 (4.3%) | |
| Smoking | 0.004 | |||
| Non-smoker | 5190 (60.0%) | 2,616 (56.5%) | 806 (58.1%) | |
| Ex-smoker | 1490 (17.2%) | 897 (19.4%) | 265 (19.1%) | |
| Current smoker | 1653 (19.1%) | 902 (19.5%) | 257 (18.5%) | |
| Unknown | 318 (3.7%) | 219 (4.7%) | 59 (4.3%) | |
| eGFR (mL/min/1.73 m2) | 96.6 ± 18.0 | 91.0 ± 17.0 | 87.0 ± 17.2 | <0.001 |
Data are expressed as numbers (percentages) for categorical variables and mean ± standard deviations for continuous variables.
*P values were tested by one-way analysis of variance for continuous variables and Pearson χ2 test or Fisher exact test for the categorical variables.
The proportion of participants with only MetS in the Low, Middle, and High groups was 9.1%, 20.4%, and 33.9%, respectively (P < 0.001), whereas the proportion of participants with only CKD in the Low, Middle, and High groups was 0.9%, 2.0%, and 3.5%, respectively (P < 0.001). The proportion of participants with both MetS and CKD in the Low, Middle, and High groups was 0.2%, 0.7%, and 2.0%, respectively (P < 0.001). The proportion of participants with only MetS, only CKD, or both MetS and CKD was higher in the High group than in the Low and Middle groups.
Association between HbA1c level and MetS or CKD
We performed univariate linear regression analyses to evaluate the association between HbA1c and each MetS components. Standardized β ± standard error was 0.25 ± 0.22 for WC, 0.44 ± 0.20 for fasting glucose,–0.14 ± 0.30 for HDL cholesterol levels, 0.15 ± 2.31 for triglyceride levels, 0.21 ± 0.00 for systolic blood pressure, and 0.10 ± 0.00 for diastolic blood pressure (P < 0.001 for all variables). There were positive associations between HbA1c levels and WC, fasting glucose, triglyceride levels, systolic blood pressure, and diastolic blood pressure, and negative association between HbA1c levels and HDL cholesterol levels. In addition, HbA1c in non-diabetes participants was associated with the number of MetS components observed (S1 Table). Numbers of MetS components increased in accordance with increased HbA1c levels.
Univariate and multivariable linear regression analyses were also performed to evaluate the association between HbA1c level and eGFR (S1 Table). eGFR in non-diabetes participants was inversely associated with the HbA1c level, where eGFR decreased as HbA1c levels increased.
Logistic regression showed that the OR for only MetS with a 1% (11 mmol/mol) increase in HbA1c was 7.53 (95% CI, 6.51–8.70) in univariate analysis and 3.38 (95% CI, 2.85–4.00) in multivariable analysis (S2 Table). The OR for only CKD with a 1% (11 mmol/mol) increase in HbA1c was 9.32 (95% CI, 6.16–14.11) in univariate analysis and 2.13 (95% CI, 1.33–3.40) in multivariable analysis. The OR for both MetS and CKD with a 1% (11 mmol/mol) increase in the level of HbA1c was 21.49 (95% CI, 10.86–42.52) on univariate analysis and 4.12 (95% CI, 1.80–9.39) on multivariable analysis. A restricted cubic spline curve was plotted, with 5.6% (38 mmol/mol) as the median HbA1c level, and it was adjusted for age and sex (S1 Fig). A high HbA1c level was associated with increased OR for CKD.
To estimate the incremental value of HbA1c level to predict only MetS, only CKD or both MetS and CKD, we compared the probabilities of events and nonevents of models using relative IDI and category-free NRI (S3 Table). The IDI of adding HbA1c level to the multivariable model improved significantly. The addition of HbA1c to multivariable models resulted in a significant improvement of the category-free NRI.
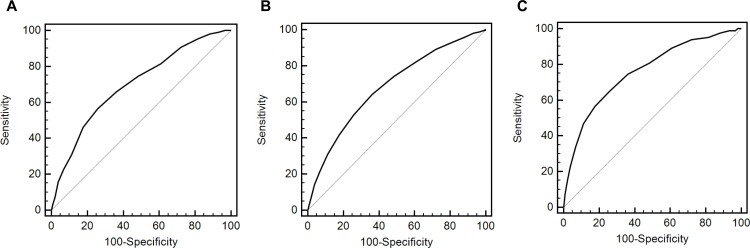
The AUROC value of HbA1c was 0.700 (95% CI, 0.692–0.708) for only MetS, 0.685 (95% CI, 0.678–0.693) for only CKD, and 0.760 (95% CI, 0.752–0.768) for both MetS and CKD (P < 0.001). The cutoff value was >5.7% (>39 mmol/mol) for only MetS, >5.6% (>38 mmol/mol) for only CKD, and >5.7% (>39 mmol/mol) for both MetS and CKD (Fig 1). Sensitivity and specificity for predicting only MetS were 56.7% and 74.2%, respectively. Those for predicting only CKD were 64.2% and 63.8%, respectively, while those for predicting both MetS and CKD were 65.1% and 74.2%, respectively.
Fig 1. Receiver operating characteristic curves of HbA1c for the prediction of metabolic syndrome or chronic kidney disease.
A. Only metabolic syndrome. B. Only chronic kidney disease. C. Both metabolic syndrome and chronic kidney disease.
Association between HbA1c level and UACR
In participants with eGFR ≥60 mL/min/1.73 m2, the correlation coefficient between UACR and HbA1c was 0.043 (P < 0.001). UACR in the Low, Middle, and High groups was 9.2 (95% CI, 8.1–10.2), 11.5 (95% CI, 9.9–13.1), and 15.9 (95% CI, 12.6–19.1), respectively (P < 0.001). The portion of participants with albuminuria in the Low, Middle, and High groups was 329 (4.3%), 239 (5.6%), and 104 (8.2%), respectively (P < 0.001).
Discussion
In the present study, a clear association was observed between HbA1c and MetS in non-DM Asian patients, which is in line with numerous other studies that have shown an association between these two variables [6–9,19–23]. Studies aiming to investigate this association should exclude patients with DM as this condition is a critical confounding factor for the prevalence of MetS and certain studies have reported no exclusion of patients with HbA1c ≥ 6.5% (≥48 mmol/mol) [21,23]. While a few previous studies did exclude DM patients with HbA1c ≥ 6.5% (≥48 mmol/mol), the majority of these were single-center studies with a possibility of selection bias [8,21,23]. The present study analyzed a nationwide, multi-stage, stratified survey of a representative sample of the South Korean population and excluded patients with HbA1c ≥ 6.5% (≥48 mmol/mol). Results were adjusted for variable confounders and revealed that HbA1c in non-DM patients is associated with the number of MetS components. The linear regression analyses did show an association between HbA1c and each component of MetS as continuous variables.
The present study showed an association between the HbA1c level and CKD with or without MetS. The associations between insulin resistance and CKD are very complex and not clear. Previous studies have shown that each component of MetS is associated with development and progression of CKD. Among the components of MetS, insulin resistance may be the most important related etiological factor for CKD [24]. HbA1c is an indicator predicting insulin resistance. High HbA1c level in pre-diabetes is associated with insulin resistance or metabolic syndrome, which can lead to development and progression of CKD. Our results suggest that high HbA1c is mainly associated with insulin resistance, which may result in development of CKD. However, CKD results in interference with the intracellular signaling pathway initiated by insulin, which results in insulin resistance [25].
The literature has shown conflict results concerning an association between HbA1c and CKD. Certain studies have shown that HbA1c is associated with development of CKD in non-DM patients [26–29]. Gerstein et al. conducted a prospective study with an average 4.5-year follow-up and successfully showed that HbA1c is associated with development of overt nephropathy defined by albuminuria or proteinuria [26]. Zhang et al. evaluated a cross-sectional study using a German cohort and showed an association between HbA1c and eGFR or CKD defined as eGFR < 60 mL/min/1.73 m2 [27]. Although DM was adjusted for in multivariable analysis, this study did include DM patients. A study by Plantinga et al. enrolled non-DM patients using data from the USA; however, this group evaluated the association between CKD and pre-diabetic status classified by fasting glucose level [28]. In contrast to the afore-mentioned studies, there have been reports that no association exists between the two variables if variable cardiovascular risk factors are adjusted for [30–33]. Selvin et al. observed no significant difference in the development of CKD in patients with HbA1c 5.7–6.5% (39–48 mmol/mol) when compared to patients with HbA1c <5.7% (<39 mmol/mol) [31]. However, that study did not include HbA1c as a diagnostic criterion for DM and could possibly include DM patients. To the best of our knowledge, this is the first study to evaluate the association between HbA1c and CKD in an Asian population. The results of the present study do show an association between HbA1c and eGFR as a continuous variable for renal function or CKD as a categorical variable. In addition, we calculated IDI and NRI as more advanced prediction analyses; these analyses showed that in comparison with multivariable models using only traditional risk factors, the addition of HbA1c to multivariable models improved both IDI and NRI. Unfortunately, cross-sectional study such as this cannot evaluate the causal relationship among these variables. Further prospective studies are needed to identify the causality between two variables.
The present study showed the association between HbA1c and albuminuria as a surrogate marker for early CKD. In participants with eGFR ≥60 mL/min/1.73 m2, UACR and the proportion of participants with albuminuria increased as HbA1c increased. Previous studies demonstrated that HbA1c level is associated with albuminuria in participants with DM [34–39]. Poor glycemic control in DM plays a key role in rapid progression to diabetic nephropathy, which is caused by variable hemodynamic, metabolic, or endothelial dysfunction [40]. Many previous studies have demonstrated pathophysiology or factors associated with progression to albuminuria in DM, but there have been few studies regarding the association between HbA1c and albuminuria in non-DM participants. The present study reveals that high-normal HbA1c levels previously considered to be in the normal range may be associated with albuminuria and may function as a marker for early CKD in non-DM participants.
The pathophysiology of the association between CKD and HbA1c in non-DM participants may be the same as that in high-glucose DM participants. This may ultimately result in subclinical or clinical atherosclerosis in various vessels. Glycemic control is a well-known risk factor for the development of atherosclerosis in DM participants. Previous studies also showed a positive association between prediabetes and atherosclerosis as measured by carotid intimal thickness, subclinical myocardial damage, or coronary artery calcium [41–43]. These pathologic changes can develop in the renal vasculature, which results in CKD with albuminuria.
Very low HbA1c level may be associated with malnutrition, inflammation, and atherosclerosis. However, in our study, a spline curve showed that low HbA1c level is not associated with CKD compared to median HbA1c level. Two factors may be associated with this discordance. First, malnutrition combined with low HbA1c level is common in participants with severe comorbidities, such as advanced cancer or end-stage renal disease, compared with the general population. Participants enrolled in our study may have been healthier than other selected populations who visited hospitals, which could have resulted in selection bias. Second, HbA1c may be used as a nutritional marker, but it mainly reflects glucose intake. The numbers of participants with total cholesterol < 100 mg/dL as another marker of malnutrition were 6, 7, and 0 in the Low, Middle, and High groups, respectively. There were few participants with malnutrition defined by total cholesterol level in our study.
This study has a number of limitations. First, it is a retrospective cross-sectional design and therefore cannot establish causality between two variables. Second, the available data did not include post-prandial blood glucose levels as a criterion for DM and a small number of DM patients could therefore have included. However, all participants have HbA1c < 6.5% (<48 mmol/mol) and a fasting blood glucose <126 mg/dL. Third, KDIGO guidelines define CKD as eGFR < 60 mL/min/1.73 m2 for >3 months [44]. In our study, CKD was defined using a single serum creatinine or single spot urine sample. However, the effect of these limitations will be reduced by the strength of a nation-wide representative sample.
In conclusion, high HbA1c in non-DM patients may be associated with CKD. Renal function in patients with high HbA1c levels may need to be monitored.
Supporting Information
Spline curve was adjusted for age and sex.
(TIF)
(DOCX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the 2014 Yeungnam University Research Grant. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351: 1296–1305. [DOI] [PubMed] [Google Scholar]
- 2. Jin DC, Han JS. Renal replacement therapy in Korea, 2012. Kidney Res Clin Pract 2014;33:9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Renal Data System, USRDS 2014 Annual Data Report: Atlas of Chronic Kidney Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2014.
- 4. American Diabetes Association. Standards of medical care in diabetes-2015. Diabetes Care 2015;38 Suppl 1: S1–S10. [PubMed] [Google Scholar]
- 5. Grundy SM. Pre-diabetes, metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol 2012;59: 635–643. 10.1016/j.jacc.2011.08.080 [DOI] [PubMed] [Google Scholar]
- 6. Osei J, Rhinesmith S, Gaillard T, Schuster D. Is glycosylated hemoglobin A1c a surrogate for metabolic syndrome in nondiabetic, first-degree relatives of African-American patient with type 2 diabetes? J Clin Endocrinol Metab 2003;88: 4596–4601. [DOI] [PubMed] [Google Scholar]
- 7. Ong KL, Tso AW, Lam KS, Cherny SS, Sham PC, Cheung BM. Using glycosylated hemoglobin to define the metabolic syndrome in the United States adults. Diabetes Care 2010;33: 1856–1858. 10.2337/dc10-0190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Park SH, Yoon JS, Won KC, Lee HW. Usefulness of glycated hemoglobin as diagnostic criteria for metabolic syndrome. J Korean Med Sci 2012;27: 1057–1061. 10.3346/jkms.2012.27.9.1057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen J, Muntner P, Hamm LL, Jones DW, Batuman V, Fonseca V, et al. The metabolic syndrome and chronic kidney disease in U.S. adults. Ann Intern Med 2004;140: 167–174. [DOI] [PubMed] [Google Scholar]
- 10. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150: 604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, et al. Alcohol use In: Ezzati M, Lopez A, Rodgers A, Murray CJL eds. Comparative Quantification of Health Risks: global and regional burden of disease attributable to selected major risk factors. Geneva, World Health Organization, 2004:959–1108. [Google Scholar]
- 12.The Korea Centers for Disease Control and Prevention: Alcohol drinking. [internet]. Available: http://health.mw.go.kr/HealthInfoArea/HealthInfo/View.do?idx=5800&subIdx=3&searchCate=&searchType=&searchKey=&pageNo=&category=&category_code=&dept=&sortType=viewcount&page=1&searchField=&searchWord=.
- 13. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnostic and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112: 2735–2752. [DOI] [PubMed] [Google Scholar]
- 14. Alberti KG, Zimmet P, Shaw J. 2005. The metabolic syndrome-a new worldwide definition. Lancet. 366, 1059–1062. [DOI] [PubMed] [Google Scholar]
- 15. Kim Y, Je Y. Dairy consumption and risk of metabolic syndrome: a meta-analysis. Diabet Med 2015. October 3 10.1111/dme.12970 [DOI] [PubMed] [Google Scholar]
- 16. Johnson DW, Atai E, Chan M, Phoon RK, Scott C, Toussaint ND, et al. KHA-CARI guideline: Early chronic kidney disease: detection, prevention and management. Nephrology 2013;18:340–50. 10.1111/nep.12052 [DOI] [PubMed] [Google Scholar]
- 17. Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 2008;27:157–72. [DOI] [PubMed] [Google Scholar]
- 18. Pencina MJ, D’Agostino RB Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 2011;30:11–21. 10.1002/sim.4085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Veeranna V, Ramesh K, Zalawadiya SK, Pradhan J, Jacob S, Afonso L. Glycosylated hemoglobin and prevalent metabolic syndrome in nondiabetic multiethnic U.S. adults. Metab Syndr Relat Disord 2011;9: 361–367. 10.1089/met.2011.0032 [DOI] [PubMed] [Google Scholar]
- 20. Nguyen QM, Srinivasan SR, Xu JH, Chen W, Berenson GS. Distribution and cardiovascular risk correlates of hemoglobin A(1c) in nondiabetic younger adults: the Bogalusa Heart Study. Metabolism 2008; 57: 1487–1492. 10.1016/j.metabol.2008.04.011 [DOI] [PubMed] [Google Scholar]
- 21. Sung KC, Rhee EJ. Glycated haemoglobin as a predictor for metabolic syndrome in non-diabetic Korean adults. Diabet Med 2007;24: 848–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dilley J, Ganesan A, Deepa M, Sharada G, Williams OD, Mohan V. Association of A1C with cardiovascular disease and metabolic syndrome in Asian Indians with normal glucose tolerance. Diabetes Care 2007;30: 1527–1532 [DOI] [PubMed] [Google Scholar]
- 23. Kim JH, Choi SR, Lee JR, Shin JH, Lee SJ, Han MA, et al. Association of hemoglobin A1c with cardiovascular disease risk factors and metabolic syndrome in nondiabetic adults. Korean Diabetes J 2008;32: 435–444. [Google Scholar]
- 24. Prasad GV. Metabolic syndrome and chronic kidney disease: Current status and future directions. World J Nephrol 2014;3:210–9. 10.5527/wjn.v3.i4.210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Thomas SS, Zhang L, Mitch WE. Molecular mechanisms of insulin resistance in chronic kidney disease. Kidney Int. 2015. October 7 10.1038/ki.2015.305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gerstein HC, Progue J, Mann JF, Lonn E, Dagenais GR, McQueen M, et al. The relationship between dysglycaemia and cardiovascular and renal risk in diabetic and non-diabetic participants in the HOPE study: a prospective epidemiological analysis. Diabetologia 2005;48: 1749–1755. [DOI] [PubMed] [Google Scholar]
- 27. Zhang QL, Koenig W, Raum E, Stegmaier C, Brenner H, Rothenbacher D. Epidemiology of chronic kidney disease: results from a population of older adults in Germany. Prev Med 2009;48: 122–127. 10.1016/j.ypmed.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 28. Plantinga LC, Crews DC, Coresh J, Miller ER 3rd, Saran R, Yee J, et al. Prevalence of chronic kidney disease in US adults with undiagnosed diabetes or prediabetes. Clin J Am Soc Nephrol 2010;5: 673–682. 10.2215/CJN.07891109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hernandez D, Espejo-Gil A, Bernal-Lopez MR, Mancera-Romero J, Baca-Osorio AJ, Tinahones FJ, et al. Association of HbA1c and cardiovascular and renal disease in an adult Mediterranean population. BMC Nephrol 2013;17: 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fox CS, Larson MG, Leip EP, Meigs JB, Wilson PW, Levy D. Glycemic status and development of kidney disease: the Framingham Heart Study. Diabetes Care 2005;28: 2436–2440. [DOI] [PubMed] [Google Scholar]
- 31. Selvin E, Ning Y, Steffes MW, Bash LD, Klen R, Wong TY, et al. Glycated hemoglobin and the risk of kidney disease and retinopathy in adults with and without diabetes. Diabetes 2011;60: 298–305. 10.2337/db10-1198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schöttker B, Brenner H, Koenig W, Müller H, Rothenbacher D. Prognostic association of HbA1c and fasting plasma glucose with reduced kidney function in subjects with and without diabetes mellitus. Results from a population-based cohort study from Germany. Prev Med 2013;57: 596–600. 10.1016/j.ypmed.2013.08.002 [DOI] [PubMed] [Google Scholar]
- 33. Xing FY, Neeland IJ, Gore MO, Ayers CR, Paixao AR, Turer AT, et al. Association of prediabetes by fasting glucose and/or haemoglobin A1c levels with subclinical atherosclerosis and impaired renal function: observations from the Dallas Heart Study. Diab Vasc Dis Res 2014;11: 11–18. 10.1177/1479164113514239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nelson RG, Kunzelman CL, Pettitt DJ, Saad MF, Bennett PH, Knowler WC. Albuminuria in type 2 (non-insulin-dependent) diabetes mellitus and impaired glucose tolerance in Pima Indians. Diabetologia 1989;32:870–6. [DOI] [PubMed] [Google Scholar]
- 35. Wiseman M, Viberti G, Mackintosh D, Jarrett RJ, Keen H. Glycaemia, arterial pressure and micro-albuminuria in type 1 (insulin-dependent) diabetes mellitus. Diabetologia 1984;26:401–5. [DOI] [PubMed] [Google Scholar]
- 36. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–86. [DOI] [PubMed] [Google Scholar]
- 37. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008;359:1577–89. 10.1056/NEJMoa0806470 [DOI] [PubMed] [Google Scholar]
- 38. Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39. 10.1056/NEJMoa0808431 [DOI] [PubMed] [Google Scholar]
- 39. Perkovic V, Heerspink HL, Chalmers J, Woodward M, Jun M, Li Q, et al. Intensive glucose control improves kidney outcomes in patients with type 2 diabetes. Kidney Int. 2013;83:517–23. 10.1038/ki.2012.401 [DOI] [PubMed] [Google Scholar]
- 40. Lim AKh. Diabetic nephropathy-complications and treatment. Int J Nephrol Renovasc Dis 2014;15:361–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. McNeely MJ, McClelland RL, Bild DE, Jacobs DR Jr, Tracy RP, Cushman M, et al. The association between A1C and subclinical cardiovascular disease: the multi-ethnic study of atherosclerosis. Diabetes Care 2009;32:1727–33. 10.2337/dc09-0074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Moebus S, Stang A, Mohlenkamp S, Dragano N, Schmermund A, Slomiany U, et al. Association of impaired fasting glucose and coronary artery calcification as a marker of subclinical atherosclerosis in a population-based cohort–results of the Heinz Nixdorf Recall Study. Diabetologia 2009;52:81–9. 10.1007/s00125-008-1173-y [DOI] [PubMed] [Google Scholar]
- 43. Selvin E, Lazo M, Chen Y, Shen L, Rubin J, McEvoy JW, et al. Diabetes mellitus, prediabetes, and incidence of subclinical myocardial damage. Circulation 2014;130:1374–82. 10.1161/CIRCULATIONAHA.114.010815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kidney Disease Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013;3:1–150. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Spline curve was adjusted for age and sex.
(TIF)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.