Abstract
Purpose
The benefit of milk intake remains controversial. The association between milk consumption and Framingham Risk Score (FRS) in a population consuming relatively low amounts of dairy products is undetermined.
Materials and Methods
A total of 13736 adults (5718 male and 8018 female) aged 20-80 years from the Korea National Health and Nutrition Examination Survey (2008-2011) were divided into groups according to milk consumption (rarely, monthly, weekly, and daily) and compared according to FRS after relevant variable adjustments.
Results
The mean FRS in males and females were 6.53 and 5.74, respectively. Males who consumed milk daily (15.9%) had a significantly lower FRS than males having milk rarely (31.6%) or monthly (17.4%; p=0.007). Females who consumed milk daily (22.3%) also had significantly lower FRS than rarely (29.8%), monthly (13.8%), or weekly (34%; p=0.001) consumers. In particular, males ≥60 years old who consumed milk daily had a significantly lower FRS than males who consumed less milk (p<0.001). The odds ratio in this age group showed a significant and gradual increase in the weekly [OR=2.15; 95% confidence interval (CI) 1.14-4.03], monthly (OR=2.29; 95% CI 1.15-4.54), and rarely (OR=3.79; 95% CI 2.01-7.14) milk consumption groups when compared with the daily milk consumption group.
Conclusion
Milk consumption was associated with a lower FRS in a low milk-consuming population. In particular, daily milk consumption in males over 60 years old may be beneficial for those at risk for cardiovascular disease.
Keywords: Milk consumption, Framingham Risk Score, Koreans
INTRODUCTION
Dairy products including milk have been reported to have a beneficial effect on hypertension1 and insulin sensitivity,2 as they are rich in various nutrients, such as calcium, magnesium, potassium, and other food components. Despite their contribution of saturated fatty acid to the diet, there is no clear evidence that dairy products are associated with a higher risk of cardiovascular disease (CVD).3 In prospective cohort studies, milk intake was not associated with total mortality but may have been inversely associated with overall CVD risk4 and myocardial infarction risk.5 Furthermore, three servings of dairy food consumption per day was found to lead to a better nutrient status, improved bone health, lower blood pressure, and reduced risk of CVD and type 2 diabetes.6,7 In a Japanese study, drinking milk 1-2 times a month and 3-4 times a week were associated with lower all-cause mortality in men and women, respectively, compared to those who never drank milk.8
On the other hand, harmful effects of milk consumption have been reported as well. Although the role of dairy product consumption in mortality generally appeared to be neutral in men, dairy fat intake was reported to be associated with slightly increased all-cause and ischemic heart disease mortality.9 In a recent large cohort study (mean follow-up of 20.1 years), three or more glasses of milk a day was associated with higher mortality in men and women and higher fracture incidence in women.10 In addition, one meta-analysis reported that dairy product consumption was associated with a non-significant increased risk of gastric cancer.11 The Framingham Risk Score (FRS), which is based on data obtained from the Framingham Heart Study, is generally considered to be a useful tool for assessing future cardiovascular risk.12 It is a gender-specific algorithm used to estimate the 10-year cardiovascular risk of an individual. The FRS can be calculated based on gender, age, total cholesterol (TC), high-density lipoprotein cholesterol (HDLC), blood pressure, and smoking status. The original FRS was published in 1998,13 and the current version of the FRS was published in 2002.14 A recent study15 indicated that 70% of subjects aged 40 years or older from the National Health and Nutrition Examination Survey (2003-2004) were found to have low (<10%) 10-year CVD risk, while 19% had intermediate (10-20%) risk and 11% had high (≥20%) risk.
Given this controversy surrounding the effect of milk consumption on CVD risk and the lack of a related report in Korea, the association between milk consumption and FRS in the Korean population, which consumes relatively low amounts of dairy products, was evaluated using data from the Korean National Health and Nutrition Examination Survey (KNHANES, 2008-2011).
MATERIALS AND METHODS
Study data
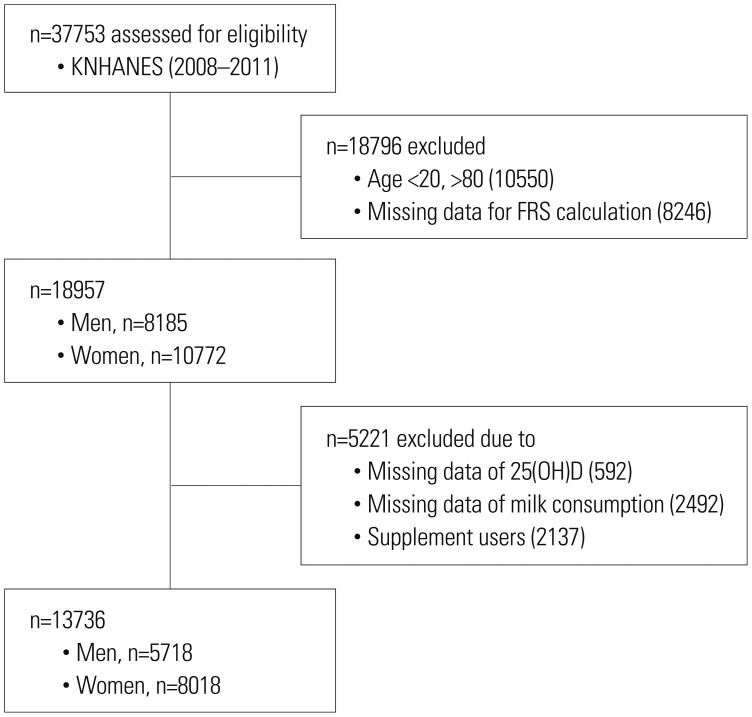
The KNHANES has been conducted periodically by the Korea Centers for Disease Control and Prevention. This study provides comprehensive information on health status, health behavior, nutritional status, and socio-demographics in 600 national districts in Korea. For this cross-sectional study, data were used from the fourth (IV-2 and IV-3; 2008, 2009) and fifth (V-1 and V-2; 2010, 2011) KNHANES; these contained information on milk consumption and elements required for FRS calculation, such as age, gender, TC, HDLC, smoking status, systolic blood pressure (SBP), and presence of hypertension or medication for hypertension. In our data, the ranges (means) of FRS in men and women were -10 to 19 (8.5) and -8 to 26 (7.4), respectively. Data on demographic characteristics, diet, and health-related variables were collected through personal interviews and self-administered questionnaires. Physical examinations and blood sampling were carried out at a mobile examination center. From an initial total of 37753 men and women, 18796 people were excluded due to missing data from FRS elements and age limitations (<20 and >80 years). Additionally, 5221 subjects were also excluded due to missing data from 25-hyroxyvitamin D [25(OH)D], milk consumption, and any supplement use. Ultimately, the analysis in this study was conducted using data from 13736 subjects (5718 males and 8018 females), as shown in Fig. 1. Although we excluded a large number of subjects due to the exclusion criteria, the selected data were nevertheless representative, considering their relatively even distribution for each year (25.8% in 2008, 27.9% in 2009, 23.7% in 2010, and 22.6% in 2011). All participants provided written informed consent before the survey.
Fig. 1. Selection of study data. KNHANES, Korea National Health and Nutrition Examination Survey; FRS, Framingham Risk Score.
Measurements
Blood samples, after an 8-h fast, were collected year-round. They were immediately processed, refrigerated, and transported in cold storage to the central testing institute (NeoDin Medical Institute, Seoul, Korea), where they were analyzed within 24 hours. Serum 25(OH)D concentration was measured with a radioimmunoassay kit (DiaSorin Inc., Stillwater, MN, USA) using a γ-counter (1470 Wizard; PerkinElmer, Turku, Finland) at the same institute, which conducted quality control every other week throughout the analysis period to minimize the analytical variation. The TC, triglyceride (TG), HDLC, and creatinine concentrations were measured using an Hitachi 7600-110 chemistry analyzer (Hitachi, Tokyo, Japan). Fasting blood sugar was measured using an automated analyzer with an enzymatic assay (Pureauto S GLU: Daiichi, Tokyo, Japan).
Physical examinations were performed by a trained examiner following a standardized procedure. Body weight and height were measured in light indoor clothing without shoes to the nearest 0.1 kg and 0.1 cm, respectively. Body mass index (BMI) was calculated as the ratio of weight/height2 (kg/m2). SBP and diastolic blood pressure were measured in the right arm using a standard mercury sphygmomanometer (Baumanometer, Baum, Copiague, NY, USA). We used a self-administered questionnaire to collect information on hypertension, smoking status, alcohol intake, job, moderate physical activity, and total energy intake. In women, the questionnaire further collected information about menopausal status, hormone replacement therapy, and oral contraceptive use, which was used to make appropriate adjustments. Current smokers were defined as those who had smoked more than five packs of cigarettes during their life and were currently smoking, past smokers were those who had smoked in the past but had quit smoking, and nonsmokers had no history of smoking. Regular alcohol drinkers were defined as those who had one drink or more at least once a month, and others were all deemed nondrinkers. Nutrient intake including total calories was assessed with a 24-hour dietary recall questionnaire administered by a trained examiner. The results were calculated using the Food Composition Table developed by the National Rural Resources Development Institute (seventh revision).16 Milk consumption was determined by a food frequency questionnaire, and the results were recorded by a trained examiner. We categorized milk consumption into four groups, according to the food-frequency questionnaire: rarely (almost never or several times per year), monthly (several times per month), weekly (several times per week), and daily (1-3 times per day). In this study, milk intake refers to consuming whole milk, low-fat milk, skim milk, processed milk, or nonfat dry milk. Physical activity was assessed using a questionnaire and categorized as yes or no, with yes meaning >30 minutes of moderate physical activity three or more times in the last week in which the subject was tired compared to ordinary levels.
Statistical analysis
A complex sample analysis was used for the KNHANES data so as to weigh all values according to the statistical guidelines of the Korea Centers for Disease Control and Prevention. General characteristics including age, BMI, blood pressure, TC, HDLC, TG, fasting blood glucose, smoking status, alcohol intake, and moderate physical activity were presented for both genders after weighting the data. An ANCOVA was performed to evaluate the differences in FRS (as a dependent variable) among the milk consumption groups (as fixed factors; rarely, monthly, weekly, and daily) in both genders after adjusting for age, BMI, job, alcohol intake, moderate physical activity, and serum 25(OH)D. In women, menopause, hormone replacement therapy, and oral contraceptive use were also used as adjustment factors. For further comparison of FRS, we divided the data into age groups (20-39 years, 40-59 years, and ≥60 years) and compared FRS in each age group via ANCOVA after relevant factor adjustment. Finally, the odds ratio for the highest quartile of FRS was determined in men over 60 years old, in whom significant differences in FRS were found according to milk consumption. A logistic regression analysis was performed (FRS quartile as a dependent factor, milk consumption group as a fixed factor) after adjusting for age, BMI, job, alcohol intake, moderate physical activity, and serum 25(OH)D in Model 1 and further adjusting for total calorie intake and calcium intake in Model 2. All p values were used to assess the significance of all analyses, and p values <0.05 were considered statistically significant. Data were analyzed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
With respect to general characteristics, the mean ages of males and females were 43.3 and 44.8 years old, respectively. The mean 25(OH)D levels were 19.4 ng/mL (males) and 16.8 ng/mL (females), and dietary calcium intake levels were 574.4 mg/day (males) and 453.8 mg/day (females). As presented in Table 1, 31.6% of Korean adults consumed milk rarely, and only 15.9% of adults drank milk daily. The mean FRSs in males and females were 6.53 and 5.74, respectively. Other metabolic parameters were within their normal ranges (Table 1).
Table 1. Framingham Risk Scores and General Health-Related Characteristics of Study Subjects.
| Variables | Men (n=5718) | Women (n=8018) | p value |
|---|---|---|---|
| Age (yrs) | 43.3 (0.3) | 44.8 (0.3) | <0.05 |
| 20-39 | 1740 (30.4) | 2685 (33.5) | |
| 40-59 | 2182 (38.2) | 3064 (38.2) | |
| ≥60 | 1796 (31.4) | 2269 (28.3) | |
| BMI (kg/m2) | 24.1 (0.1) | 23.2 (0.1) | <0.05 |
| SBP (mm Hg) | 117.7 (0.3) | 113.4 (0.3) | <0.05 |
| DBP (mm Hg) | 77.4 (0.2) | 72.6 (0.2) | <0.05 |
| TC (mg/dL) | 186.8 (0.6) | 185.8 (0.2) | <0.05 |
| HDL (mg/dL) | 49.4 (0.2) | 55.5 (0.2) | <0.05 |
| Triglyceride (mg/dL) | 157.4 (2.2) | 109.3 (1.1) | <0.05 |
| FBS (mg/dL) | 98.4 (0.4) | 95.1 (0.3) | <0.05 |
| 25(OH)D (ng/mL) | 19.4 (0.2) | 16.8 (0.2) | <0.05 |
| Energy intake (kcal/day) | 2363.8 (16.2) | 1660.3 (10.5) | <0.05 |
| Calcium intake (mg/day) | 574.4 (5.7) | 453.8 (4.8) | <0.05 |
| FRS | 6.53 (1.14) | 5.74 (0.14) | <0.05 |
| Q1 | -10-4 | -8-0 | |
| Q2 | 5-10 | 1-8 | |
| Q3 | 11-13 | 9-14 | |
| Q4 | 14-19 | 15-26 | |
| Smoking, n (%) | <0.05 | ||
| Yes | 2449 (42.8) | 423 (5.3) | |
| No | 3269 (57.2) | 7595 (94.7) | |
| Alcohol, n (%) | <0.05 | ||
| Yes | 4192 (73.6) | 3058 (38.3) | |
| No | 1505 (26.4) | 4930 (61.7) | |
| Activity, n (%) | <0.05 | ||
| Yes | 815 (14.3) | 1119 (14.0) | |
| No | 4902 (85.7) | 6887 (86.0) | |
| Milk consumption, n (%) | <0.05 | ||
| Rarely | 1806 (31.6) | 2389 (29.8) | |
| Monthly | 995 (17.4) | 1106 (13.8) | |
| Weekly | 2010 (35.2) | 2727 (34.0) | |
| Daily | 907 (15.9) | 1796 (22.4) |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; HDL, high-density lipoprotein; FBS, fasting blood sugar; FRS, Framingham Risk Score; 25(OH)D, serum 25-hyroxyvitamin D; energy intake, total calorie intake; smoking, current smoking status; alcohol, current alcohol consumption; activity, moderate physical activity.
Data are expressed as mean (standard error). p values are from a general linear model and χ2 test after data weighting.
On comparing FRS according to milk consumption in each gender, FRS decreased as milk consumption increased after adjustment for age, BMI, job, alcohol intake, moderate physical activity, and serum 25(OH)D, as well as menopause, oral contraceptive use, and hormone replacement therapy in women. Particularly, FRS in males of the daily milk consumption group was significantly lower than that in males of the rarely and monthly groups (p=0.007). FRS in females of the daily milk consumption group was also significantly lower than that in females of the rarely, monthly, and weekly groups (p=0.001) (Table 2). To further compare FRS, we stratified the data into different age groups (20-39 years, 40-59 years, and ≥60 years) for each gender. In males over 60 years old, the FRS of the daily milk consumption group was significantly lower than that of those in the other groups (p<0.001). In females (Table 3), although not clinically significant, the FRS of the 20-39 years age group showed a significant p for trend (p=0.018). Finally, the odds ratio for the highest quartile of FRS in males over 60 years old significantly increased in the weekly [OR=2.21; 95% confidence interval (CI) 1.12-4.10], monthly (OR=2.36; 95% CI 1.21-4.70), and rarely (OR=4.00; 95% CI 2.17-7.38) milk consumption groups in Model 1 [adjustment for age, BMI, job, alcohol intake, moderate physical activity, serum 25(OH)D]. In Model 2 (further adjusted for total calorie intake and calcium intake), the odds ratio was also increased in the weekly (OR=2.15; 95% CI 1.14-4.03), monthly (OR=2.29; 95% CI 1.15-4.54), and rarely (OR=3.79; 95% CI 2.01-7.14) milk consumption groups (Table 4).
Table 2. Framingham Risk Score (FRS) According to Milk Consumption.
| Groups | Men (n=5718) | Women (n=8018) | ||
|---|---|---|---|---|
| n (%) | FRS | n (%) | FRS | |
| Rarely | 1806 (31.6) | 6.75 (0.12) | 2389 (29.8) | 5.89 (0.09) |
| Monthly | 995 (17.4) | 6.86 (0.15) | 1106 (13.8) | 5.98 (0.13) |
| Weekly | 2010 (35.2) | 6.46 (0.11)§ | 2727 (34.0) | 5.75 (0.09) |
| Daily | 907 (15.9) | 6.15 (0.17)*† | 1796 (22.4) | 5.42 (0.09)*†‡ |
| p value | 0.007 | 0.001 | ||
FRS are expressed as mean (standard error). p values represent p for trends found via ANCOVA after adjusting for age, body mass index, job, alcohol intake, moderate physical activity, and serum 25-hydroxyvitamin D. Further adjustments were made for menopause, oral contraceptive use, and hormone replacement therapy in cases of women.
*p<0.05 in the comparison between rarely vs. daily, †p<0.05 in the comparison between monthly vs. daily, ‡p<0.05 in the comparison between weekly vs. daily, §p<0.05 in the comparison between monthly vs. weekly.
Table 3. Framingham Risk Score (FRS) According to Milk Consumption by Age.
| Variables | FRS, mean (SE)/n (%) | ||
|---|---|---|---|
| 20-39 yrs | 40-59 yrs | ≥60 yrs | |
| Men (n) | 1740 | 2182 | 1796 |
| Rarely | 1.41 (0.39)/255 (14.7) | 9.63 (0.12)/699 (32.0) | 13.56 (0.06)/852 (47.4) |
| Monthly | 1.53 (0.34)/261 (15.0) | 9.83 (0.16)/417 (19.1) | 13.36 (0.11)/317 (17.7) |
| Weekly | 1.06 (0.18)/812 (46.7) | 9.71 (0.12)/770 (35.3) | 13.32 (0.08)§/428 (23.8) |
| Daily | 0.92 (0.23)/412 (23.7) | 9.45 (0.20)/296 (13.6) | 12.96 (0.12)*†‡/199 (11.1) |
| P for trend | 0.383 | 0.512 | <0.001 |
| Women (n) | 2685 | 3064 | 2269 |
| Rarely | -1.61 (0.20)/405 (15.1) | 8.40 (0.12)/831 (27.1) | 16.69 (0.09)/1153 (50.8) |
| Monthly | -1.20 (0.29)/336 (12.5) | 8.21 (0.14)/468 (15.3) | 16.50 (0.14)/302 (13.3) |
| Weekly | -1.77 (0.14)/1102 (41.0) | 8.11 (0.11)/1116 (36.4) | 16.56 (0.14)/509 (22.4) |
| Daily | -2.10 (0.15)/842 (31.4) | 8.19 (0.13)/649 (21.2) | 16.35 (0.15)/305 (13.4) |
| P for trend | 0.018 | 0.332 | 0.222 |
FRS are expressed as mean (standard error). p values represent p for trends found via ANCOVA after adjusting for age, body mass index, job, alcohol intake, moderate physical activity, and serum 25-hydroxyvitamin D. Further adjustments were made for menopause, oral contraceptive use, and hormone replacement therapy in cases of women.
*p<0.05 in the comparison between rarely vs. daily, †p<0.05 in the comparison between monthly vs. daily, ‡p<0.05 in the comparison between weekly vs. daily, §p<0.05 in the comparison between monthly vs. weekly.
Table 4. Odds Ratios According to Milk Consumption in Men Over 60 Years Old for the Highest Quartile of Framingham Risk Scores.
| Milk consumption | Odds ratio (95% CI) | ||
|---|---|---|---|
| Crude | Model 1 | Model 2 | |
| Rarely | 3.14 (1.85-5.35) | 4.00 (2.17-7.38) | 3.79 (2.01-7.14) |
| Monthly | 1.84 (1.05-3.22) | 2.36 (1.21-4.70) | 2.29 (1.15-4.54) |
| Weekly | 1.63 (0.94-2.82) | 2.21 (1.12-4.10) | 2.15 (1.14-4.03) |
| Daily | 1 (reference) | 1 (reference) | 1 (reference) |
Data represent odds ratios with a 95% confidence interval (CI) based on logistic regression analysis after adjustment for age, body mass index, job, moderate physical activity, alcohol intake, and serum 25-hydroxyvitamin D in Model 1 and further adjustment for total calorie intake and calcium intake in Model 2.
DISCUSSION
In this cross-sectional study, we found that milk consumption was inversely associated with FRS in males and females who consumed relatively low amounts of dairy products. In addition, daily milk consumption in males over 60 years old was found to be beneficial in lowering the risk of a high FRS.
Previous studies suggest higher mortality rates from fracture17 and ischemic heart disease,18 as well as from certain cancers,19,20 in countries with high milk consumption. In addition, those who consumed high amounts of non-fermented milk were reported to have less favorable cardiovascular risk factor profiles, with higher blood pressure, lower HDLC levels, and higher insulin resistance.21 On the other hand, cheese and fermented milk consumption has been reported to be associated with an increased HDLC levels, reduced insulin resistance, and a lower risk of CVD. A possible mechanism for such different responses may be related to the D-galactose content in different types of dairy products,10,22 which is associated with oxidative stress, chronic inflammation,23 and the development of such diseases.24
In accordance with the current study, a prospective study (22.8 years of follow-up) reported that SBP was 10.4 mm Hg lower in the group with the highest milk consumption than in a group that did not consume milk.25 In addition, consumption of milk and dairy products was inversely associated with CVD death among women in Japan26 and related to lower levels of specific CVD risk factors in China,27 where milk consumption is relatively low. We used the FRS to evaluate CVD risk according to different milk consumption groups. FRS is a simple tool to assess future CVD risk,12 and it significantly predicts coronary heart disease events.28 In our study, we were not able to determine the association between FRS and high milk consumption, as only 0.7% and 0.3% of males and 1.2% and 0.3% of females were found to drink milk 2 and 3 times per day, respectively. In this low milk-consuming population, daily milk consumption was beneficial for lower FRS than weekly, monthly, or rare consumption. A more interesting result was that the odds ratio for the top quartile of FRS showed a gradual increase with a decrease in milk consumption in older men (≥60 years old) even after adjustments for 25(OH)D, total calories, and calcium intake. This may indicate that proper consumption of milk may be related to a lower FRS in men over 60 years old who have a relatively higher risk of CVD. However, it is not clear why women over 60 years old did not show a similar effect on CVD risk. These results may be partially due to gender difference and different metabolic risks.
The current study has several limitations. First, this study used a cross-sectional design to evaluate the association between milk consumption and FRS in one ethnic group. Second, only the frequency of milk consumption was considered, and quantitative information on milk consumption was not. However, this is the first study to evaluate the association between milk consumption and FRS, a future CVD risk factor, using representative data from the KNHANES.
In conclusion, milk consumption was inversely associated with FRS in males and females. In addition, males over 60 years old who drank milk daily had a lower FRS and a lower risk of a higher FRS after relevant variable adjustment. A large and prospective study is warranted to determine the exact amount of milk consumption required and future CVD risk and mortality in this ethnic group with low milk consumption.
ACKNOWLEDGEMENTS
This work was carried out with the support of the "Cooperative Research Program for Agriculture Science & Technology Development" (grant number PJ010059) from the Rural Development Administration, Republic of Korea.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Steffen LM, Kroenke CH, Yu X, Pereira MA, Slattery ML, Van Horn L, et al. Associations of plant food, dairy product, and meat intakes with 15-y incidence of elevated blood pressure in young black and white adults: the coronary artery risk development in young adults (CARDIA) study. Am J Clin Nutr. 2005;82:1169–1177. doi: 10.1093/ajcn/82.6.1169. [DOI] [PubMed] [Google Scholar]
- 2.Turner KM, Keogh JB, Clifton PM. Dairy consumption and insulin sensitivity: a systematic review of short- and long-term intervention studies. Nutr Metab Cardiovasc Dis. 2015;25:3–8. doi: 10.1016/j.numecd.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 3.German JB, Gibson RA, Krauss RM, Nestel P, Lamarche B, van Staveren WA, et al. A reappraisal of the impact of dairy foods and milk fat on cardiovascular disease risk. Eur J Nutr. 2009;48:191–203. doi: 10.1007/s00394-009-0002-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, Hu FB, Engberink MF, Willett WC, et al. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr. 2011;93:158–171. doi: 10.3945/ajcn.2010.29866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patterson E, Larsson SC, Wolk A, Åkesson A. Association between dairy food consumption and risk of myocardial infarction in women differs by type of dairy food. J Nutr. 2013;143:74–79. doi: 10.3945/jn.112.166330. [DOI] [PubMed] [Google Scholar]
- 6.Rice BH, Quann EE, Miller GD. Meeting and exceeding dairy recommendations: effects of dairy consumption on nutrient intakes and risk of chronic disease. Nutr Rev. 2013;71:209–223. doi: 10.1111/nure.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Markey O, Vasilopoulou D, Givens DI, Lovegrove JA. Dairy and cardiovascular health: friend or foe? Nutr Bull. 2014;39:161–171. doi: 10.1111/nbu.12086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C, Yatsuya H, Tamakoshi K, Iso H, Tamakoshi A. Milk drinking and mortality: findings from the Japan collaborative cohort study. J Epidemiol. 2015;25:66–73. doi: 10.2188/jea.JE20140081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldbohm RA, Chorus AM, Galindo Garre F, Schouten LJ, van den Brandt PA. Dairy consumption and 10-y total and cardiovascular mortality: a prospective cohort study in the Netherlands. Am J Clin Nutr. 2011;93:615–627. doi: 10.3945/ajcn.110.000430. [DOI] [PubMed] [Google Scholar]
- 10.Michaëlsson K, Wolk A, Langenskiöld S, Basu S, Warensjö Lemming E, Melhus H, et al. Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ. 2014;349:g6015. doi: 10.1136/bmj.g6015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun Y, Lin LJ, Sang LX, Dai C, Jiang M, Zheng CQ. Dairy product consumption and gastric cancer risk: a meta-analysis. World J Gastroenterol. 2014;20:15879–15898. doi: 10.3748/wjg.v20.i42.15879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhu B, Haruyama Y, Muto T, Yamasaki A, Tarumi F. Evaluation of a community intervention program in Japan using Framingham risk score and estimated 10-year coronary heart disease risk as outcome variables: a non-randomized controlled trial. BMC Public Health. 2013;13:219. doi: 10.1186/1471-2458-13-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 14.National cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 15.Ferket BS, van Kempen BJ, Hunink MG, Agarwal I, Kavousi M, Franco OH, et al. Predictive value of updating Framingham risk scores with novel risk markers in the U.S. general population. PLoS One. 2014;9:e88312. doi: 10.1371/journal.pone.0088312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Rural Resources Development Institute. Food Composition Table. 7th ed. Suwon: Rural Development Administration; 2006. [Google Scholar]
- 17.Hegsted DM. Fractures, calcium, and the modern diet. Am J Clin Nutr. 2001;74:571–573. doi: 10.1093/ajcn/74.5.571. [DOI] [PubMed] [Google Scholar]
- 18.Segall JJ. Hypothesis: is lactose a dietary risk factor for ischaemic heart disease? Int J Epidemiol. 2008;37:1204–1208. doi: 10.1093/ije/dyn169. [DOI] [PubMed] [Google Scholar]
- 19.Song Y, Chavarro JE, Cao Y, Qiu W, Mucci L, Sesso HD, et al. Whole milk intake is associated with prostate cancer-specific mortality among U.S. male physicians. J Nutr. 2013;143:189–196. doi: 10.3945/jn.112.168484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lampe JW. Dairy products and cancer. J Am Coll Nutr. 2011;30(5 Suppl 1):464S–470S. doi: 10.1080/07315724.2011.10719991. [DOI] [PubMed] [Google Scholar]
- 21.Sonestedt E, Wirfält E, Wallström P, Gullberg B, Orho-Melander M, Hedblad B. Dairy products and its association with incidence of cardiovascular disease: the Malmö diet and cancer cohort. Eur J Epidemiol. 2011;26:609–618. doi: 10.1007/s10654-011-9589-y. [DOI] [PubMed] [Google Scholar]
- 22.Gross KC, Acosta PB. Fruits and vegetables are a source of galactose: implications in planning the diets of patients with galactosaemia. J Inherit Metab Dis. 1991;14:253–258. doi: 10.1007/BF01800599. [DOI] [PubMed] [Google Scholar]
- 23.Cui X, Zuo P, Zhang Q, Li X, Hu Y, Long J, et al. Chronic systemic D-galactose exposure induces memory loss, neurodegeneration, and oxidative damage in mice: protective effects of R-alpha-lipoic acid. J Neurosci Res. 2006;84:647–654. doi: 10.1002/jnr.20899. [DOI] [PubMed] [Google Scholar]
- 24.Jumbo-Lucioni PP, Hopson ML, Hang D, Liang Y, Jones DP, Fridovich-Keil JL. Oxidative stress contributes to outcome severity in a drosophila melanogaster model of classic galactosemia. Dis Model Mech. 2013;6:84–94. doi: 10.1242/dmm.010207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Livingstone KM, Lovegrove JA, Cockcroft JR, Elwood PC, Pickering JE, Givens DI. Does dairy food intake predict arterial stiffness and blood pressure in men?: evidence from the Caerphilly prospective study. Hypertension. 2013;61:42–47. doi: 10.1161/HYPERTENSIONAHA.111.00026. [DOI] [PubMed] [Google Scholar]
- 26.Kondo I, Ojima T, Nakamura M, Hayasaka S, Hozawa A, Saitoh S, et al. Consumption of dairy products and death from cardiovascular disease in the Japanese general population: the NIPPON DATA80. J Epidemiol. 2013;23:47–54. doi: 10.2188/jea.JE20120054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sun Y, Jiang C, Cheng KK, Zhang W, Leung GM, Lam TH, et al. Milk consumption and cardiovascular risk factors in older Chinese: the Guangzhou biobank cohort study. PLoS One. 2014;9:e84813. doi: 10.1371/journal.pone.0084813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gander J, Sui X, Hazlett LJ, Cai B, Hébert JR, Blair SN. Factors related to coronary heart disease risk among men: validation of the Framingham risk score. Prev Chronic Dis. 2014;11:E140. doi: 10.5888/pcd11.140045. [DOI] [PMC free article] [PubMed] [Google Scholar]