Malignant melanoma is one of the most rapidly growing neoplasms that develop during pregnancy. Traditionally, it has been stated that women who are pregnant at the time of diagnosis have a poorer prognosis than women who are not pregnant. Additionally, the subsequent pregnancies were believed to increase the recurrence rate. There are very few studies in this area, but some authors of retrospective studies show that gestating women have poorer prognosis than non-pregnant women. Other authors report the presence of sex-hormone receptors in the melanoma tissue, suggesting a hormonal sensitivity of this neoplasm. There is also a group of studies that do not confirm these findings.
A 32-year-old healthy patient reported to the Gynaecology Clinic, Jagiellonian University Medical College (JUMC) in her twenty-first week of gestation with a verrucous lesion on the back in the interscapular area. The patient was consulted at the Outpatient Clinic of the Department of Dermatology, JUMC. A melanocytic nevus, often irritated by the patient, was described. There were neither clinical nor dermoscopic features of an underlying neoplastic process, so photo-documentation was not performed at that time. The patient did not report any other illnesses or symptoms, and she did not take any medication. The pregnancy was endangered, so the patient decided to postpone the surgical excision of the lesion after giving birth. Five months later, the patient returned to the Clinic with a noticeably enlarged (now 3 × 2 cm), polypous, ulcerated tumour. An excisional biopsy of the lesion was made – with a macroscopic margin of 10 mm. The patient received chloramphenicol ointment, and dressings were applied. Histologically, the lesion was described as malignant melanoma, nodular type with ulceration. The neoplasm was in the vertical phase of growth, Clarke V, Breslow IV with mitotic activity of 14 mitotic figures/mm2. Features of vascular invasion were observed on the basis of the lesion. In the dermis and subcutaneous area, numerous microsatellite foci were found, with the greatest being 2.2 mm in size. The lesion was removed with microscopic borders of 1.2 mm and 4 mm laterally and 6.5 mm deep. Abdominal ultrasound revealed hypo- and hyperechoic lesions in the liver (max. size: 47 × 29 × 36 mm) and hypoechoic lesions in the spleen with a single enlarged lymph node near the head of the pancreas (16 × 7 mm). Nuclear magnetic resonance (NMR) confirmed hypo- and isointense lesions in T1 with enhancement after contrast, the largest being 36 × 44 mm in segment V. Similar lesions were described in the spleen (max. 15 mm). The patient was tested for the BRAF mutation. A chest X-ray revealed no abnormalities.
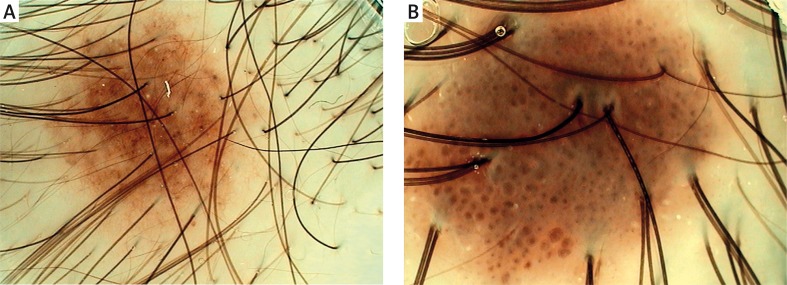
Two weeks later the patient observed a nodular lesion located on the right side of her parietal scalp. Dermoscopy of the lesion was performed (Figures 1 A, B). The patient also complained of nonspecific muscle and lower limb pain. She was consulted by a neurologist who recommended Mg and K supplementation.
Figure 1 A, B.
Dermoscopic images of metastatic melanoma on the right side of the crown of the head
Nuclear magnetic resonance of the head revealed numerous small foci consistent with metastatic lesions to the brain: in the right cerebellar hemisphere (3 mm), in the right and left temporal lobes (max. 3 mm in size) and in the left parietal lobe (2 and 6 mm). Additional metastases were discovered in the right humerus (the patient did not report any pain in the right arm), as well as the thoracic and lumbar vertebra. Ultrasound revealed a lymph node package in the right axilla (69 × 32 mm) and a single node in the right supraclavicular area (15 × 15 mm). Brain and bone radiation therapy were recommended. During hospitalization, the patient reported severe weakness, dizziness, dyspnoea and peripheral oedema. Laboratory tests revealed: monocytosis 12.5% (range: 4–11), eosinophilia 0.8% (range: 1–5), microcytic anaemia with red blood cell (RBC) 3.44 mln/µl (range: 37–47), haemoglobin (Hb) 9.4 (range: 12–16), mean platelet volume (MPV) 7.9 fl (range: 8.8–12), red cell distribution width (RDW) 15% (range: 11.5–14.5). The patient was administered buprenorphine transdermal therapy, tramadol, diazepam, dexamethasone, ketoprofen, omeprazole, estazolam, and diclofenac. One month after excision of the lesion, she received brain radiotherapy (6 MV, 20 Gy). Unfortunately, disease progression was observed, with an increase in the liver parameters: alanine aminotransferase (ALT) 158 U/l (range: 5–31), aspartate transferase (AST) 223 U/l (range: 5–32), γ-glutamyl transpeptidase (GGTP) 540 U/l (range: 6–42), low total protein 52.7 g/l (range: 64–83), hypoalbuminemia 27.6/24.3 g/l (range: 34–48), hyperbilirubinemia 25.85 µmol/l (< 21), C-reactive protein (CRP) was 97.25 mg/l (range: 0–5) and mild hyponatremia and hypercalcemia were observed.
Complete blood count (CBC) revealed white blood cells (WBC) of 23.34 × 103/mm3 (range: 4.3–10); progress of microcytic anaemia with RBC of 3.3/3.16 × 106/mm3 (range: 4–5.2), Hb 8.9/8.6 g/dl, haematocrit (Hct) 27/27%, mean corpuscular volume (MCV) 81.8. (83 × 103), mean cell haemoglobin (MCH) 27 pg (range: 28–34) and thrombocytopenia 136/93 × 103/mm3 (range: 150–350), platelet-crit (PCT) 0.5% (range: 0.2–0.4), leucocytosis 24.9 thousand/µl (range: 4–10) and lymphocytosis 6.9 thousand/µl (range: 1.00–3.50). Despite the blood transfusions and albumin infusions, the patient developed electrolyte imbalance followed by cardiopulmonary and renal insufficiency (creatinine level of 155.5 µmol/l, urea 31.76). These changes were the direct cause of death. Later, the results of the BRAF qualification studies showed that the patient was positive for a BRAF mutation and, therefore, could have received treatment with drugs targeting the BRAF/MEK growth pathway.
It is important to mention that laboratory tests for viruses performed between the sixth and eighth weeks of pregnancy were non-diagnostic. A HIV screen and hepatitis B surface antigen test were initially positive, with non-reactive anti-HCV. The subsequent laboratory tests had to be repeated several times, due to “lack of coherence” in hepatitis B surface antigen results; anti-HCV was negative. Western blot did not confirm HIV infection. Blood testing done at the beginning of the 4th month of gestation excluded hepatitis B infection. In the fourth month of gestation, C-reactive protein reached 14.9 mg/l (range: 0–5), while the other results remained within their reference ranges throughout the pregnancy. Prenatal studies performed in the first trimester showed an increased risk of aneuploidy due to enhanced nuchal translucency (21 trisomy risk – 1 : 29, 18 – 1 : 784, 13 – 1 : 4190), and the PAPP-A value was normal. Ultrasound of the foetus revealed a shortened jaw, impaired gastric filling, and a dilated renal pelvis. Some malformations of the lower part of cerebellar vermis were also observed. Ultimately, the patient developed polyhydramnios, and the clinical pattern was consistent with esophageal atresia. A spontaneous delivery occurred at 37 weeks gestation. The child was born weighing 2910 g, received 10 points on the Apgar scale and was positive for esophageal atresia.
Malignant melanoma is the major cause of death from neoplasms in women of child-bearing age [1]. The incidence in gestation ranges from 0.14 to 2.8 per 1000 pregnancies, which accounts for approximately 8% of all malignancies arising during gestation. Various studies show that it is the first or the second most common neoplasm diagnosed during pregnancy [1, 2]. According to Lambe, 5.6% of neoplasms diagnosed in women of child-bearing age occurred concurrently with pregnancy or lactation. Furthermore, the incidence of melanoma is increasing among women aged 15–39 years [3].
Many immunological changes are observed during pregnancy. The innate immunity is downregulated favouring allograft tolerance. Murine models show that T cells become aware of foetal alloantigens during gestation. The precise mechanism of this process remains unknown [4–7]. The total number of effector cells is altered with an increase in granulocytes and decrease in lymphocytes. T-lymphocytes show impaired interleukin-2 (IL-2) and interferon γ (IFN-γ) production after stimulation. These processes clinically manifest as frequent remission of psoriasis and autoimmune diseases, such as rheumatoid arthritis and multiple sclerosis. Taking these changes into consideration, pregnancy was considered an aggravating factor of melanoma [8].
In the early 1950s, Pack and Scharnagel reported poor outcomes in 32 women with melanoma diagnosed during pregnancy. The authors recommended avoiding pregnancy for 3 to 5 years after completion of treatment [9]. Byrd and McGanity even postulated that female melanoma patients should be surgically sterilized [10]. In 1981, Houghton et al. compared 12 pregnant women with melanoma to 175 non-pregnant controls. After 5 years of follow-up there was no significant difference in survival between pregnant and non-pregnant women (55% vs. 58%). However, pregnant patients had prognostically poorer primary sites of melanoma and more advanced stage of the neoplasm [11]. Studies from the late 1980s through the early 1990s compared large numbers of pregnant and non-pregnant patients and demonstrated thicker melanoma tumours in the pregnant group compared to controls. The authors attributed the results to delayed diagnosis in pregnant women [12]. Few studies from this period revealed a difference in survival between groups of pregnant and non-pregnant women with melanoma [13–15].
Khosrotehrani et al. showed that pregnancy results in increased lymphangiogenesis and subsequent metastases in mice. Melanomas from pregnant mice had an increased expression of vascular endothelial growth factor A (VEGF A) at both the RNA and protein levels [16]. Nguyen-Huu et al. also postulated that tumours are thicker in pregnant women compared to controls [17]. Stoica et al. found that melanocytes have the ability to bind oestrogen and progesterone [18]. More recent studies on larger groups of patients with melanoma (450 post-pregnant women compared to 3000 non-pregnant individuals) demonstrated no difference in survival between the groups [19]. Miller et al. showed that pregnant women had more advanced disease than non-pregnant controls. The mean Breslow thickness was higher in the pregnancy group (4.28 mm) than in controls (1.69 mm). This difference failed to reach statistical significance; most likely due to the small trial group. The number of melanoma-positive nodes, however, was significantly higher. There was also a higher mortality rate (of borderline significance) in the pregnancy group compared to the control groups [20, 21]. These results are in line with Reintgen's study of 1985 [22, 23].
A few in vitro trials have revealed the presence of progesterone and oestrogen receptors on melanoma cells [24–26]. On the contrary, Morvillo et al. reported a lack of progesterone and oestrogen receptors, but instead found evidence that their melanoma cell lines were positive for androgen receptors. They demonstrated that testosterone, oestrogen and progesterone significantly stimulated melanoma cell proliferation [27]. Another in vitro study revealed that oestrogen and dihydrotestosterone changed nuclear morphology in melanoma cells. Kanda and Watanabe, on the other hand, reported that melanoma cell lines containing hormone receptors were down-regulated by 17β-oestradiol, progesterone, and testosterone. Cell lines without those receptors were not influenced by the sex hormones [28]. Miller et al. found a limited number of oestrogen receptors in melanoma tissue (2 positive out of 69 melanoma specimens) [29]. Melanoma tissue was also found positive for luteinizing hormone releasing hormone (LHRH) receptors – the cell line showed inhibited proliferation and reduced metastatic activity in response to an LHRH receptor agonist [30]. Some epidemiologic studies report that the melanoma risk decreases with higher parity and has a tendency to increase in individuals who delayed their first pregnancy. A French prospective study suggests that the risk of melanoma is reduced with decreased exposure to ovarian hormones [31–33]. A study conducted by Ellerhorst et al. shows that melanoma cells proliferate in response to TRH and TSH, but also indicates that leptin may play the role of melanoma growth factor [34, 35]. In their study, melanoma cells strongly expressed the leptin receptor, whereas nevi had less receptor expression. Since leptin regulates many processes during gestation, interacts with gestation-specific serum-borne factors and steroid receptors, and it is linked to preeclampsia, gestational diabetes and intrauterine growth restriction, it can be assumed that pregnancy and melanoma may affect each other [36].
Melanoma is one of few neoplasms (including leukemias, lymphomas, lung and breast cancer) that has the potential to metastasize to the placenta. In fact, it is the most common neoplasm involving the foetus and placenta (approximately 31% of all neoplasms). The risk of metastasis to the placenta and foetus is low and occurs in patients with widely metastatic melanoma [37]. Metastases have a predilection to male new-borns (80% of children with melanoma metastases). Since the first report in 1866 until 2003 only 87 cases of placental or foetal metastasis were reported. Many authors suspect that placentas from pregnancies where the mother had MM were not always examined microscopically or that follow-up of children derived from these pregnancies was too short [37].
Hormone replacement therapy (HRT) and contraception do not seem to be risk factors for melanoma development. MacKie et al. reported that the use of HRT after treatment for stage 1 melanoma did not have adverse effects on patients’ outcomes [14]. Likewise, Tang et al. showed that menopausal hormone therapy did not affect the overall incidence of melanoma or non-melanoma skin neoplasms in postmenopausal patients [38].
Since most melanoma recurrences happen within 2 years after surgical excision of the neoplasm, several authors suggest delaying pregnancy for 2–3 (or even 5) years after completion of treatment. The exact time depends on the tumour thickness, presence of ulceration, and sentinel node metastasis [39]. The treatment options are similar in pregnant and non-pregnant individuals. Patients with superficial lesions require excision with wide surgical margins under local anaesthesia, followed by close clinical monitoring. Studies show that excisional biopsy under local anaesthesia poses a very low risk either to the mother or foetus. Furthermore, sentinel node biopsy with dye and lymphoscintigraphy is not contraindicated during pregnancy. Some authors, however, recommend avoiding lymphoscintigraphy before the 30th week of gestation and postponing sentinel node biopsy until delivery [40].
Melanoma is a rapidly growing neoplasm that can rarely metastasise to the placenta and the foetus if it occurs during pregnancy. Early reports suggested a rapid progression of the disease during pregnancy, but more recent data do not support this statement. In our case, we observed dynamic progression of the disease, which coincides with the early case reports. Caring for an expecting mother with melanoma is emotionally difficult and challenging for every provider. This is probably the reason why cases of melanoma occurring during pregnancy are described so often in the literature. Unfortunately, our patient's child was born with several malformations. Of note, there have been no studies implicating melanoma as a trigger or risk factor for developmental abnormalities. The most recent studies show that the prognosis of melanoma during pregnancy is similar to that of non-pregnant women. Despite this fact, follow-up examinations of pigmented skin lesions should be performed with care, and other risk factors for malignant melanoma should be explored [41]. Additionally, the placentas of women with suspected or known disseminated disease should be examined carefully.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Jhaveri MB, Driscoll MS, Grant-Kels JM. Melanoma in pregnancy. Clin Obstet Gynecol. 2011;54:537–45. doi: 10.1097/GRF.0b013e318236e18b. [DOI] [PubMed] [Google Scholar]
- 2.Mathew M, Sheik S, Rao K, et al. Metastatic malignant melanoma during pregnancy: case report and a review of the literature. Sultan Qaboos Univ Med J. 2009;9:79–83. [PMC free article] [PubMed] [Google Scholar]
- 3.Lambe M, Ekbom A. Cancers coinciding with childbearing: delayed diagnosis during pregnancy? BMJ. 1995;311:1607–8. doi: 10.1136/bmj.311.7020.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luppi P. How immune mechanisms are affected by pregnancy. Vaccine. 2003;21:3352–7. doi: 10.1016/s0264-410x(03)00331-1. [DOI] [PubMed] [Google Scholar]
- 5.Osiński M, Żaba C. Antiretroviral drugs usage in HIV-positive pregnant women. Postep Derm Alergol. 2012;29:132–5. [Google Scholar]
- 6.Podolec-Rubiś M, Wołek M, Brzewski P, Wojas-Pelc A. Suspicion of pulmonary embolism during treatment of pemphigoid gestationis. Postep Derm Alergol. 2013;30:59–61. doi: 10.5114/pdia.2013.33381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oleszczuk L, Oleszczuk J, Kwiecińska B, et al. Use of diet supplements, synthetic drugs and herbal remedies with immunotropic activity during pregnancy. III. Conjugated linoleic acid. Centr Eur J Immunol. 2011;36:308–10. [Google Scholar]
- 8.Brady MS, Noce NS. Pregnancy is not detrimental to the melanoma patient with clinically localized disease. J Clin Aesthet Dermatol. 2010;3:22–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Pack GT, Scharnagel IM. The prognosis for malignant melanoma in the pregnant woman. Cancer. 1951;4:324–34. doi: 10.1002/1097-0142(195103)4:2<324::aid-cncr2820040218>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 10.Silipo V, De Simone P, Mariani G, et al. Malignant melanoma and pregnancy. Melanoma Res. 2006;16:497–500. doi: 10.1097/01.cmr.0000232295.91536.09. [DOI] [PubMed] [Google Scholar]
- 11.Byrd BF, McGanity WJ. The effect of pregnancy on the clinical course of malignant melanoma. South Med J. 1954;47:196–9. doi: 10.1097/00007611-195403000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Houghton AN, Flannery J, Viola MV. Malignant melanoma of the skin occurring during pregnancy. Cancer. 1981;48:407–10. doi: 10.1002/1097-0142(19810715)48:2<407::aid-cncr2820480231>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 13.Travers RL, Sober AJ, Berwick M. Increased thickness of pregnancy-associated melanoma. Br J Dermatol. 1995;132:876e83. doi: 10.1111/j.1365-2133.1995.tb16942.x. [DOI] [PubMed] [Google Scholar]
- 14.MacKie RM, Bufalino R, Morabito A. Lack of effect of pregnancy on outcome of melanoma. Lancet. 1991;337:653e5. doi: 10.1016/0140-6736(91)92462-b. [DOI] [PubMed] [Google Scholar]
- 15.Wong JH, Sterns EE, Kopald KH. Prognostic significance of pregnancy in stage 1 melanoma. Arch Surg. 1989;124:1227e31. doi: 10.1001/archsurg.1989.01410100133023. [DOI] [PubMed] [Google Scholar]
- 16.Khosrotehrani K, Nguyen Huu S, Prignon A, et al. Pregnancy promotes melanoma metastasis through enhanced lymphangiogenesis. Am J Pathol. 2011;178:1870–80. doi: 10.1016/j.ajpath.2010.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen-Huu S, Aractingi S, Oster M, Khosrotehrani K. Enhanced maternal and fetal derived angiogenesis in melanomas during pregnancy. 37th Annual Meeting of the European Society for Dermatological Research, Zurich, Switzerland 5-8 September, 2007. J Investig Dermatol. 2007;S51 [Google Scholar]
- 18.Stoica A, Hoffman M, Marta L, Voiculetz N. Estradiol and progesterone receptors in human cutaneous melanoma. Neoplasma. 1991;38:137–45. [PubMed] [Google Scholar]
- 19.Lens MB, Rosdahl I, Ahlbom A, et al. Effect of pregnancy on survival in women with cutaneous malignant melanoma. J Clin Oncol. 2004;22:4369–75. doi: 10.1200/JCO.2004.02.096. [DOI] [PubMed] [Google Scholar]
- 20.Stensheim H, Moller B, van Dijk T, Fossa SD. Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: a registry-based cohort study. J Clin Oncol. 2009;27:45–51. doi: 10.1200/JCO.2008.17.4110. [DOI] [PubMed] [Google Scholar]
- 21.Miller E, Barnea Y, Gur E, et al. Malignant melanoma and pregnancy: second thoughts. J Plast Reconstr Aesthet Surg. 2010;63:1163–8. doi: 10.1016/j.bjps.2009.05.050. [DOI] [PubMed] [Google Scholar]
- 22.Reintgen DS, McCarty KS, Vollmer R. Malignant melanoma and pregnancy. Cancer. 1985;55:1340e4. doi: 10.1002/1097-0142(19850315)55:6<1340::aid-cncr2820550630>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 23.Slingluff CL, Reintgen DS, Vollmer RT. Malignant melanoma arising during pregnancy. A study of 100 patients. Ann Surg. 1990;211:552e9.11. doi: 10.1097/00000658-199005000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fernö M, Borg A, Erichsen C, et al. Estrogen and progesterone receptors in melanoma metastases with special reference to analytical methods and prognosis. Anticancer Res. 1984;4:179–82. [PubMed] [Google Scholar]
- 25.Tanemura A, van Hoesel AQ, Mori T, et al. The role of estrogen receptor in melanoma. Expert Opin Ther Targets. 2007;11:1639–48. doi: 10.1517/14728222.11.12.1639. [DOI] [PubMed] [Google Scholar]
- 26.Li J, Fang X, Chen X, Chen J. Selective expression of progesterone receptor in malignant melanoma was inversely correlated with PCN. J Huazhong Univ Sci Technolog Med Sci. 2008;28:216–8. doi: 10.1007/s11596-008-0226-2. [DOI] [PubMed] [Google Scholar]
- 27.Morvillo V, Luthy IA, Bravo AI. Androgen receptors in human cell lines 2B-MEL-LES and 2B-MEL IAN and in human melanoma metastases. Melanoma Res. 2002;12:529e38. doi: 10.1097/00008390-200212000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Kanda N, Watanabe S. 17beta-estradiol, progesterone, and dihydrotestosterone suppress growth of human melanoma by inhibiting IL-8 production. J Invest Dermatol. 2001;117:274e83. doi: 10.1046/j.1523-1747.2001.01422.x. [DOI] [PubMed] [Google Scholar]
- 29.Miller JG, Gee J, Price A, et al. Investigation of oestrogen receptors, sex steroids and soluble adhesion molecules in the progression of malignant melanoma. Melanoma Res. 1997;7:197–208. doi: 10.1097/00008390-199706000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Keller G, Schally AV, Gaiser T, et al. Human malignant melanomas express receptors for luteinizing hormone releasing hormone allowing targeted therapy with cytotoxic luteinizing hormone releasing hormone analogue. Cancer Res. 2005;65:5857–63. doi: 10.1158/0008-5472.CAN-04-3816. [DOI] [PubMed] [Google Scholar]
- 31.Karagas MR, Zens MS, Stukel TA, et al. Pregnancy history and incidence of melanoma in women: a pooled analysis. Cancer Causes Control. 2006;17:11–9. doi: 10.1007/s10552-005-0281-y. [DOI] [PubMed] [Google Scholar]
- 32.Gandini S, Iodice S, Koomen E, et al. Hormonal and reproductive factors in relation to melanoma in women: current review and meta-analysis. Eur J Cancer. 2011;47:2607–17. doi: 10.1016/j.ejca.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 33.Kvaskoff M, Bijon A, Mesrine S, et al. Cutaneous melanoma and endogenous hormonal factors: a large French prospective study. Am J Epidemiol. 2011;173:1192–202. doi: 10.1093/aje/kwq503. [DOI] [PubMed] [Google Scholar]
- 34.Ellerhorst JA, Diwan AH, Dang SM, et al. Promotion of melanoma growth by the metabolic hormone leptin. Oncol Rep. 2010;23:901–7. doi: 10.3892/or_00000713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Henson MC, Castracane VD. Leptin in pregnancy: an update. Biol Reprod. 2006;74:218–29. doi: 10.1095/biolreprod.105.045120. [DOI] [PubMed] [Google Scholar]
- 36.Driscoll MS, Grant-Kels JM. Melanoma and pregnancy. G Ital Dermatol Venereol. 2008;143:251–7. [PubMed] [Google Scholar]
- 37.Alexander A, Samlowski WE, Grossman D, et al. Metastatic melanoma in pregnancy: risk of transplacental metastases in the infant. J Clin Oncol. 2003;21:2179–86. doi: 10.1200/JCO.2003.12.149. [DOI] [PubMed] [Google Scholar]
- 38.Tang JY, Spaunhurst KM, Chlebowski RT, et al. Menopausal hormone therapy and risks of melanoma and nonmelanoma skin cancers: women's health initiative randomized trials. J Natl Cancer Inst. 2011;103:1469–75. doi: 10.1093/jnci/djr333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Albersen M, Westerling VI, van Leeuwen PAM. The influence of pregnancy on the recurrence of cutaneous malignant melanoma in women. Dermatol Res Pract. 2010;2010:214745. doi: 10.1155/2010/214745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Andtbacka RH, Donaldson MR, Bowles TL, et al. Sentinel lymph node biopsy for melanoma in pregnant women. Ann Surg Oncol. 2013;20:689–96. doi: 10.1245/s10434-012-2633-7. [DOI] [PubMed] [Google Scholar]
- 41.Borges V, Puig S, Malvehy J. Melanocytic nevi, melanoma, and pregnancy. Actas Dermosifiliogr. 2011;102:650–7. doi: 10.1016/j.ad.2011.02.004. [DOI] [PubMed] [Google Scholar]