Abstract
OBJECTIVE
Women with gestational diabetes mellitus (GDM) demonstrate chronic and progressive insulin resistance and a markedly increased risk of converting to type 2 diabetes after pregnancy. However, the cellular mechanisms underlying this insulin resistance are unknown.
RESEARCH DESIGN AND METHODS
We investigated the progression of insulin resistance in nine obese women with GDM during late pregnancy (30–36 weeks) and 1 year postpartum. Skeletal muscle biopsies were obtained at each visit, and insulin resistance was determined by the hyperinsulinemic-euglycemic clamp technique.
RESULTS
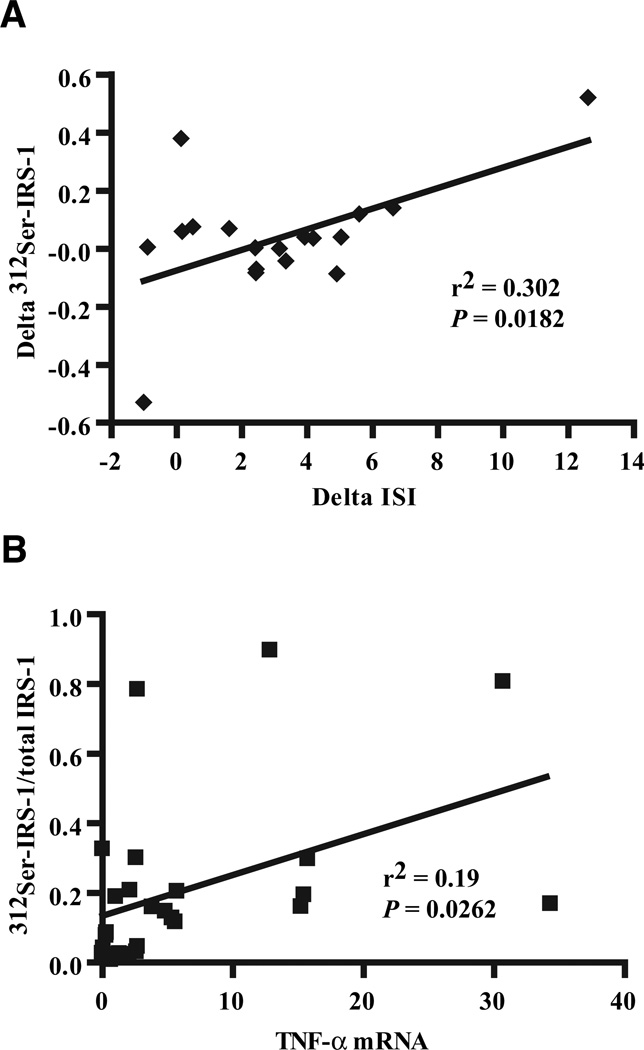
Insulin resistance was not significantly improved in GDM women (4.1 ± 0.4 vs. 5.8 ± 1.1 10−2 mg · kg FFM · min−1/µU · ml−1). Subjects did not experience significant weight loss postpartum. Body weight, fat mass, fasting glucose, and plasma tumor necrosis factor (TNF)-α remained higher 1 year postpartum than seen in previously studied normal glucose-tolerant women. Skeletal muscle TNF-α mRNA was elevated five- to sixfold in GDM women and remained higher 1 year postpartum. While levels of insulin receptor (IR), IR substrate (IRS)-1, and p85α improved postpartum, insulin-stimulated IR tyrosine phosphorylation and receptor tyrosine kinase activity did not significantly improve postpartum in GDM. The levels of 312Ser-IRS-1 also did not improve postpartum and correlated with TNF-α mRNA (r2 = 0.19, P < 0.03), consistent with a state of subclinical inflammation and chronic skeletal muscle insulin resistance.
CONCLUSIONS
These results suggest the mechanisms underlying chronic insulin resistance in GDM women may be driven by increased inflammation that impinges on the IR and IRS-1 signaling cascade in skeletal muscle. These findings have important implications for the health of GDM women during subsequent pregnancies and their risk for progression to type 2 diabetes.
Gestational diabetes mellitus (GDM), defined as impaired glucose tolerance first recognized in pregnancy, is associated with increased whole-body insulin resistance compared with obese women with normal glucose tolerance (NGT) (1,2), and it often precedes the clinical diagnosis of type 2 diabetes (3,4). Women with a history of GDM have up to a 60% chance of progressing to type 2 diabetes within 5 years after pregnancy (1,5), depending on advancing insulin resistance and deterioration of islet function (6,7). Subjects with a history of GDM tend to have a higher BMI (8), an athrogenic lipid profile (8–10), and evidence of subclinical inflammation (11–13), all characteristics associated with a state of chronic insulin resistance. The insulin signaling abnormalities that underlie this excess insulin resistance and increased risk for progression to type 2 diabetes have not been investigated previously.
Pregnancy is normally associated with a significant (~50%) decline in insulin sensitivity from the first to the third trimester (2). At the cellular level, women who maintain NGT during pregnancy experience decrements in the insulin receptor (IR) and IR substrate (IRS)-1 signaling cascade that are restored to normal within the first year postpartum (14,15). In women with GDM, skeletal muscle insulin-stimulated glucose transport and whole-body insulin sensitivity are significantly lower during late pregnancy than in weight-matched pregnant women with NGT (16,17). In addition to reduced glucose transport activity, GDM is associated with specific impairments in insulin signaling in skeletal muscle and adipose tissue (16,18–21). We previously observed a two- to threefold increase in the p85α phosphoinositide 3 kinase (PI3K) subunit in skeletal muscle and adipose tissue from GDM subjects during late pregnancy compared with obese nonpregnant subjects (16). Besides increased p85α expression, GDM subjects have reduced insulin-stimulated IR and IRS-1 tyrosine phosphorylation, which is associated with a 50% reduction in the levels of IRS-1 protein (16,18,22). Whether these abnormalities persist during the postpartum period in former GDM women is unknown.
The present study was designed as a prospective longitudinal study to investigate the potential mechanism(s) underlying chronic insulin resistance in skeletal muscle in GDM women after pregnancy. We previously characterized the cellular changes responsible for the postpartum return in insulin sensitivity in women with NGT (14). The women in the present study were obese and were diagnosed with GDM during pregnancy. They were studied during late pregnancy and again 1 year postpartum. We hypothesized that pregnancy-induced insulin signaling abnormalities in GDM women would return to normal, but that other defects might remain to help explain the chronic insulin resistance characteristic of these women postpartum. Our results show that obese women with GDM failed to return to their prepregnancy weight and maintained their insulin resistance postpartum. They continued to have impaired IR tyrosine phosphorylation, increased 312Ser-IRS-1 phosphorylation, and increased TNF-α mRNA in skeletal muscle, suggesting the mechanisms underlying chronic insulin resistance in former GDM women may be driven by inflammation that impinges on the insulin signaling cascade in skeletal muscle. While some of the pregnancy-induced mechanisms of insulin resistance (decreased IRS-1 and increased p85α) improved postpartum, these results suggest that increased adiposity postpartum may prompt progressive insulin resistance with important implications for increased risk for type 2 diabetes.
RESEARCH DESIGN AND METHODS
Subjects
Nine women with GDM (age 36 ± 2 years) volunteered to participate in the study (Table 1). GDM during pregnancy was established according to the criteria of Carpenter and Coustan (23). Prior physical activity was evaluated using the Minnesota Leisure Time Physical Activity questionnaire (24). For late pregnancy, physical activity was assessed from the last menstrual period, and for postpartum, it was assessed from delivery up to a maximum of 12 months. All pregnancy data were collected between 30 and 36 weeks gestation. All postpartum evaluations were performed ~1 year after delivery, when the women had stopped breastfeeding. These data were obtained during the follicular phase of the menstrual cycle and none of the women were using hormonal contraception. The experimental protocol was approved by the Institutional Review Board at MetroHealth Medical Center, and written informed consent was obtained from all subjects before enrollment into the study.
TABLE 1.
Descriptive characteristics during late pregnancy and postpartum in women with GDM
| Late pregnancy |
Postpartum | |
|---|---|---|
| Age (years) | 36.1 ± 1.9 | 36.9 ± 1.9* |
| Parity (n) | 0–1 (n = 4) | |
| >1 (n = 5) | ||
| Weight (kg) | 95.8 ± 6.0 | 90.4 ± 7.0 |
| BMI (kg/m2) | 35.2 ± 2.0 | 33.0 ± 2.6 |
| Body fat (%) | 39.2 ± 1.7 | 42.6 ± 2.1* |
| Fasting plasma glucose (mg/dl) | 92 ± 2 | 105 ± 5* |
| Fasting plasma insulin (µU/ml) | 24.6 ± 3.4 | 17.7 ± 2.4** |
Data are means ± SE; n = 9.
P < 0.05,
P < 0.01 vs. late pregnancy.
Oral glucose tolerance tests
A standard 75-g oral glucose tolerance test (OGTT) was performed on all subjects within 1 year postpartum. The OGTT was performed after a 10- to 12-h overnight fast. Venous blood samples for glucose and insulin determination were drawn in the fasting state and at 30, 60, 90, and 120 min after ingestion of the glucose drink. Glucose tolerance was classified according to the American Diabetes Association Clinical Practice Recommendations (25). Subjects were instructed to eat a diet consisting of at least 60% of energy as complex carbohydrate, 25% as fat, and 15% as protein for the week before the test.
Body composition
Body composition was determined by hydrostatic weighing according to the method described by Catalano et al. (26). Height was measured to the nearest 1.0 cm without shoes and body weight was measured to the nearest 0.1 kg.
Hyperinsulinemic-euglycemic clamps
A single-stage 2-h hyperinsulinemic-euglycemic clamp with [6,6-2H]glucose kinetics (5 mmol/l glucose, 40 mU · m−2 · min−1) was performed during late pregnancy (30–36 weeks) and was repeated ~1 year after delivery, as previously described (27). Insulin sensitivity (M) was computed from the glucose infusion rate that was required to maintain blood glucose at 90 mg/dl, plus residual endogenous glucose output based on [6,6-2H]glucose kinetics. The subjects were counseled by a nutritionist 1 week before study to maintain a carbohydrate and fat intake of 50–55% and 30–35%, respectively, after adjusting for the caloric demands of pregnancy.
Muscle biopsy
Muscle biopsies were performed using the Bergstrom needle biopsy procedure as previously described (28). Approximately 100 mg of tissue was obtained from the vastus lateralis muscle during late pregnancy and again ~1 year postpartum. Both biopsies were performed under basal conditions after an overnight fast. The muscle sample was immediately frozen in liquid nitrogen and stored at −80°C for subsequent analysis.
IR and IR tyrosine kinase assays
IR content, IR tyrosine phosphorylation, and IR tyrosine kinase (IRTK) activity in response to insulin was measured in triplicate by enzyme-linked immunosorbent assay (ELISA) as previously described (14,18).
Western blot analysis
The levels of IRβ, IRS-1, 312Ser-IRS-1 phosphorylation, p85α, Akt, p70S6 kinase, and GLUT4 were determined in the muscle biopsy samples as previously reported (14). Each protein sample was run in duplicate and normalized to either GAPDH or β-actin, and the results were expressed as percent change relative to the value obtained in late pregnancy. Antibodies to Akt and p70S6 kinase were purchased from Cell Signaling Technology (Danvers, MA); IRβ, IRS-1, GLUT4, GAPDH, and actin were from Santa Cruz Biotechnology (Santa Cruz, CA); 312Ser-IRS-1 and p85α were from Upstate (Millipore, Bellerica, MA).
Quantitative real-time PCR
Total RNA was extracted from ~20 mg of frozen muscle. The samples were disrupted on ice by pellet pestle motor (Kimble Kontes, Vineland, NJ) and homogenized in 20 mg/ml proteinase K at 55°C. Total RNA was then isolated using RNeasy Mini kit (Qiagen, Valencia, CA) according to the manufacturer’s directions and DNase-treated (Ambion, Austin, TX). The quality of the isolated RNA was assessed by electrophoresis on 1.5% agarose gels based on the integrity of 28S and 18S bands after ethidium bromide staining. The quantity of total RNA was determined spectrophotometrically at an absorbance of 260 nm. cDNA was prepared from 2 µg total RNA using random decamers and reverse transcriptase kit from Ambion.
TNF-α gene expression was determined by quantitative real-time PCR. Housekeeping gene β-actin and human TNF-α PCR primer sets were purchased from Roche Applied Science (Indianapolis, IN). A 2-µl sample of diluted cDNA was amplified in FastStart SYBR Green reagents (Roche) using 30 cycles at 95°C for 10 s, 55°C for 10 s, and 72°C for 18 s in a LightCycler PCR system (Roche). The data were normalized to β-actin expression using the relative standard curve method and expressed as fold-increase. The specificity of the amplified PCR product was assessed from the melting curve. Negative controls (RNA without reverse transcriptase) were included in each assay as a check for contamination.
Plasma glucose, insulin, and TNF-α assays
All samples were measured for glucose, insulin, and TNF-α and were run in duplicate in a single assay. Plasma glucose concentrations were measured by the glucose oxidase method. Blood samples for insulin measurements were centrifuged at 4°C and the plasma was stored at −80°C for subsequent analysis by a double-antibody radioimmunoassay as previously described (29). Plasma TNF-α concentrations were measured by ELISA (Quantikine HS; R&D Systems, Minneapolis, MN). The intra-assay coefficient of variation was 14%, the minimum detectable limit of the assay was 0.18 pg/ml, and the lowest standard was 0.5 pg/ml.
Statistical analysis
All values are presented as means ± SE. Differences between dependent variables were examined using a paired Student’s t test or a Wilcoxon’s signed-rank test. The relationship between the change in insulin sensitivity measured during the clamp and change in plasma TNF-α or insulin signaling proteins was based on univariate correlation analysis. The data were analyzed using Statview II (Abacus Concepts, Berkeley, CA) or Prism 4 (GraphPad Software, San Diego, CA). P < 0.05 was considered statistically significant.
RESULTS
Insulin sensitivity
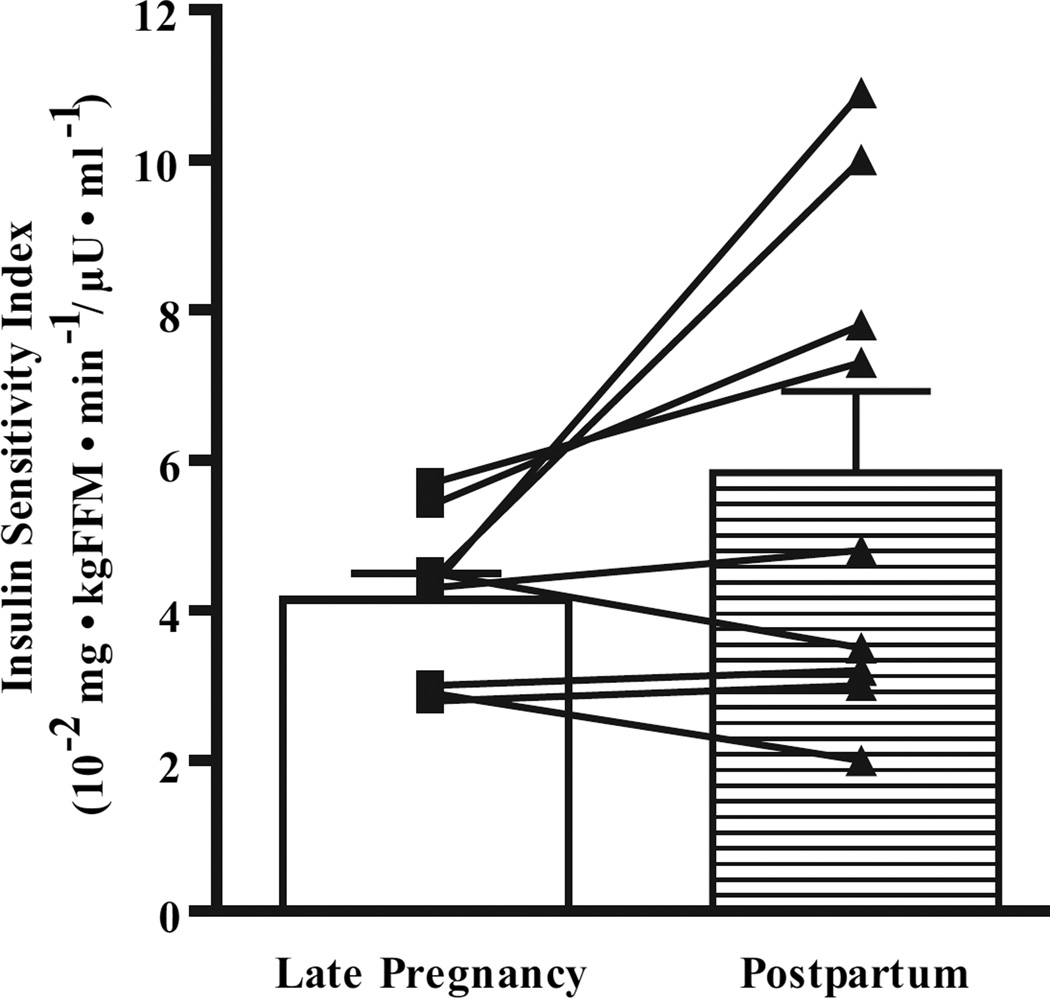
Insulin sensitivity was determined in obese GDM subjects during late third trimester and again ~1 year postpartum using the hyperinsulinemic-euglycemic clamp technique as outlined under RESEARCH DESIGN AND METHODS. One year postpartum GDM women demonstrated insulin resistance that was not significantly different from values obtained in late pregnancy (4.1 ± 0.4 vs. 5.8 ± 1.1 10−2 mg · kg FFM · min−1/µU · ml−1, P = 0.1034) (Fig. 1). As shown in Table 1, fasting plasma glucose increased postpartum (P < 0.05), while fasting plasma insulin levels declined significantly postpartum (P < 0.01). Five of the nine subjects had a fasting glucose >100 mg/dl postpartum. Complete OGTT data were obtained on eight of the nine subjects in the postpartum follow up. The mean 2-h OGTT value was 131 ± 10 mg/dl. Two of the nine subjects had 2-h glucose values >140 mg/dl but <200 mg/dl. In addition, two of the four subjects with normal fasting glucose levels had 2-h values >130 mg/dl but <140 mg/dl. Thus, seven of the nine subjects had impaired or abnormally high glucose tolerance postpartum.
FIG. 1.
Insulin sensitivity measured during hyperinsulinemic-euglycemic clamps performed during late pregnancy (30–36 weeks) and repeated ~1 year postpartum. Data are means ± SE, n = 9. No significant difference was found (P = 0.1034). The M value was calculated for the final 150–180 min of the clamp. Units are expressed relative to fat-free mass (FFM).
Body composition
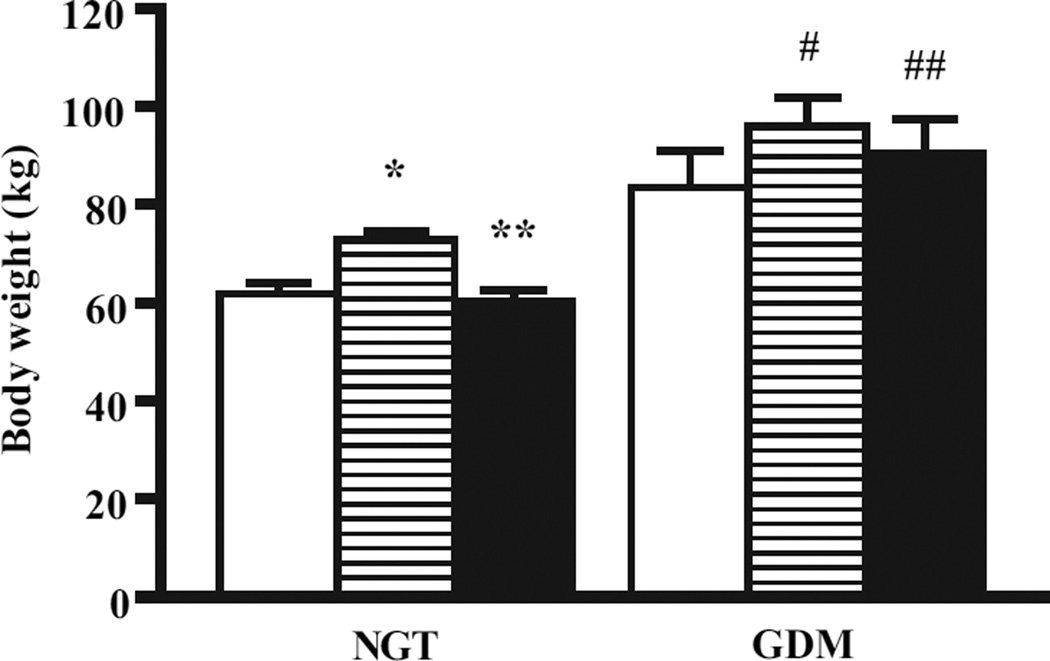
Body composition was determined by hydrostatic weighing during late gestation and ~1 year postpartum. GDM subjects did not lose a significant amount of body weight after pregnancy and did not return to their self-reported prepregnancy weight (Fig. 2), whereas a group of women with NGT (shown for comparison in Table 2) studied previously returned to prepregnancy body weight (14). In addition, although the BMI for GDM subjects was similar postpartum, fat mass increased slightly but significantly in the obese GDM women (P < 0.05) (Table 1).
FIG. 2.
Body weight based on self-reported weights prepregnancy (□) and measured weights during late pregnancy (30–36 weeks;  ) and ~1 year postpartum (■). Data are means ± SE, n = 9. *P < 0.0001 vs. prepregnancy, **P < 0.0001 vs. late pregnancy, #P < 0.005 vs. prepregnancy, and ##P < 0.05 vs. prepregnancy. Data for NGT patients were reported previously (14) and are included for reference purposes.
) and ~1 year postpartum (■). Data are means ± SE, n = 9. *P < 0.0001 vs. prepregnancy, **P < 0.0001 vs. late pregnancy, #P < 0.005 vs. prepregnancy, and ##P < 0.05 vs. prepregnancy. Data for NGT patients were reported previously (14) and are included for reference purposes.
TABLE 2.
Descriptive characteristics during late pregnancy and postpartum in women with normal glucose tolerance studied previously
| Late pregnancy | Postpartum | |
|---|---|---|
| Age (years) | 32.0 ± 1.6 | 33.2 ± 1.7* |
| Parity (n) | 0–1 (n = 6) | |
| >1 (n = 3) | ||
| Weight (kg) | 72.5 ± 2.0 | 60.0 ± 2.4* |
| BMI (kg/m2) | 25.6 ± 0.6 | 21.2 ± 0.8* |
| Body fat (%) | 28.9 ± 1.0 | 27.6 ± 1.6 |
| Fasting plasma glucose (mg/dl) | 80 ± 3 | 88 ± 2* |
| Fasting plasma insulin (µU/ml) | 11.7 ± 1.7 | 8.3 ± 0.9* |
Data are means ± SE; n = 9. From Kirwan et al. (14).
P < 0.05 vs. late pregnancy.
Physical activity
A standardized questionnaire was used to assess levels of physical activity during the 12 months preceding each clamp measurement (24). We did not see any major difference in these self-reported indexes for women with GDM postpartum (119 ± 49 units) compared with late pregnancy (110 ± 39 units) because of the wide range of activity.
Skeletal muscle insulin receptor expression and function
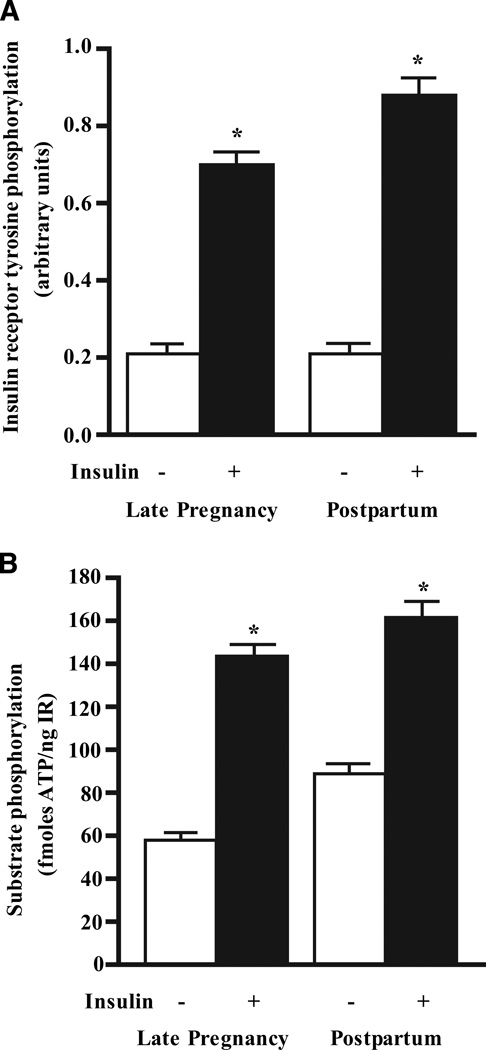
We previously demonstrated that during late pregnancy, women with GDM have a significant impairment in skeletal muscle IR tyrosine phosphorylation and reduced IRTK activity compared with weight-matched pregnant obese patients with NGT (16,18). To examine whether the decrement in IR activity persists or recovers in former GDM women, muscle biopsies were obtained in the same subjects during the late third trimester and 1 year postpartum. Using identical concentrations of insulin receptors isolated from skeletal muscle, we measured basal and maximal insulin-stimulated IR tyrosine phosphorylation in vitro. Basal IR phosphorylation was similar during late pregnancy and postpartum (Fig. 3A). Insulin-stimulated IR tyrosine phosphorylation increased three- to fourfold above basal levels. However, there was no significant changes found in maximal insulin-stimulated IR tyrosine phosphorylation 1 year postpartum compared with late pregnancy (Fig. 3A). Maximal insulin-stimulated IRTK activity measured against an artificial tyrosine substrate (Poly Glu:Tyr) was also unchanged from late pregnancy to postpartum, suggesting a lack of postpartum change in IR function (Fig. 3B).
FIG. 3.
Basal and insulin-stimulated IR tyrosine phosphorylation (A) and IRTK activity (B) measured in isolated insulin receptors from skeletal muscle obtained during late pregnancy and ~1 year postpartum. The IR concentration was measured in each biopsy based on a standard curve with purified insulin receptors, and an equal concentration of IR protein was tested for IR tyrosine phosphorylation and IRTK activity by ELISA as outlined previously (14). Data are means ± SE for obese women with GDM (n = 5). *P < 0.001 vs. basal (no insulin).
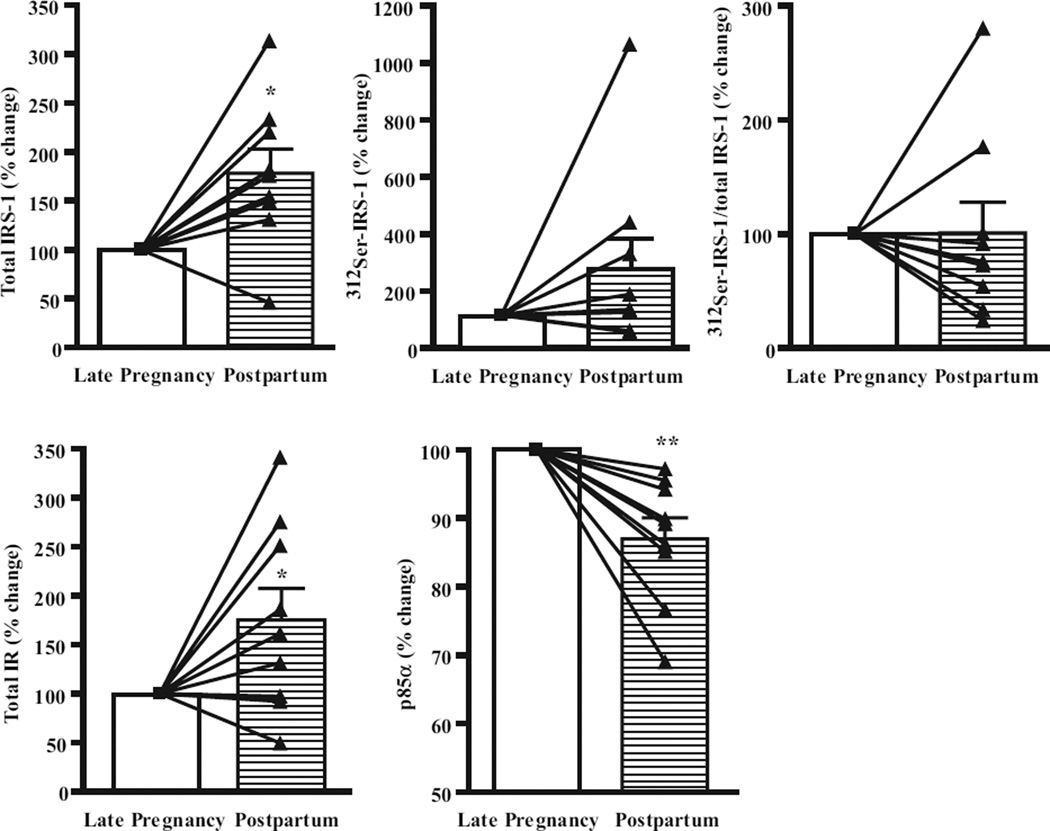
Downstream signaling, protein expression, and phosphorylation
The most immediate proteins downstream of the IR include the IRS family of proteins that includes IRS-1, which is the major IRS in adult human skeletal muscle. We previously documented a ~50% decrement in IRS-1 in GDM subjects compared with obese subjects in the nonpregnant state (16). In the present study, both IR and IRS-1 protein expression increased from late pregnancy to postpartum (P < 0.05) in women with GDM (Fig. 4). Phosphorylation of IRS-1 on serine 312 is known to negatively regulate IRS-1 tyrosine phosphorylation and may induce insulin resistance in response to increased fatty acid or cytokine activation (30). We measured the abundance of 312Ser-IRS-1 in the basal state using a phosphospecific antibody and found that in women with GDM the levels were not significantly changed postpartum. When expressed as a ratio of 312Ser-IRS-1 to total IRS-1, the ratio was also unchanged. Previously we found that levels of p85α regulatory subunit of PI3K are two to threefold higher during late pregnancy compared with obese nonpregnant women (16). In GDM subjects, the abundance of the p85α was reduced significantly postpartum (12%, P < 0.005). There were no differences in the expression of downstream signaling proteins Akt, p70S6 kinase, or the skeletal muscle glucose transporter, GLUT4, from late pregnancy to postpartum (data not shown).
FIG. 4.
Skeletal muscle insulin signaling proteins from vastus lateralis obtained during late pregnancy and ~1 year postpartum in obese GDM subjects. Equivalent amounts of protein isolated from skeletal muscle biopsies were subjected to SDS-PAGE and blotted with respective antibodies. Values are means ± SE (n = 9) and expressed as percent change from late pregnancy to postpartum. *P < 0.05 vs. late pregnancy, **P < 0.005 vs. late pregnancy.
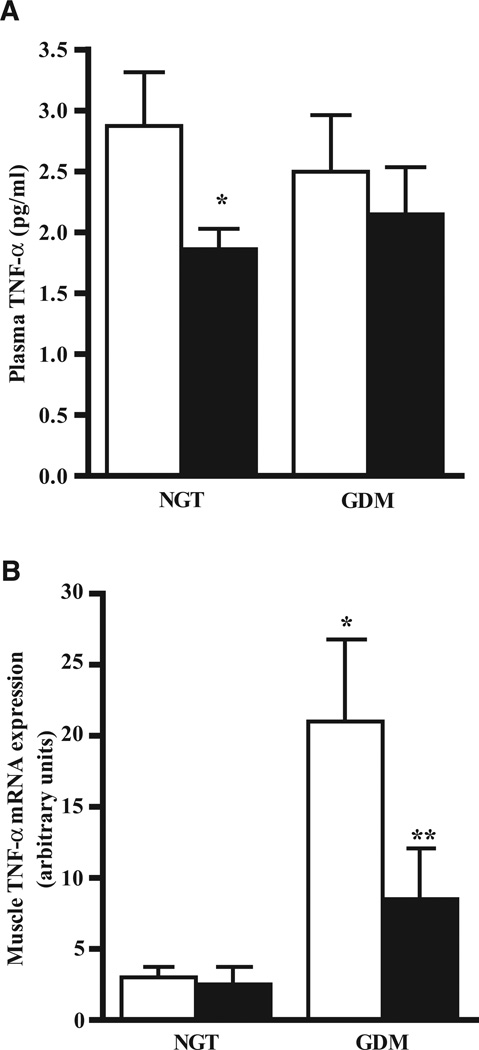
Plasma TNF-α and skeletal muscle TNF-α mRNA expression
TNF-α is a cytokine that is linked to insulin resistance. We have previously reported an increase in circulating TNF-α during late pregnancy (14). In the present study, circulating TNF-α remained unchanged postpartum compared with late pregnancy in women with GDM, while in women with NGT, these levels declined significantly postpartum (Fig. 5A). Pretranslational expression of TNF-α mRNA in muscle was determined by quantitative real-time PCR. Women with GDM had five- to sixfold higher skeletal muscle TNF-α mRNA compared with women with NGT during late pregnancy (Fig. 5B). GDM subjects experienced a significant reduction in TNF-α mRNA postpartum; however, expression remained threefold higher than in women with NGT. We performed correlation analysis between the change in insulin sensitivity (insulin sensitivity index [ISI]) and changes in skeletal muscle insulin signaling proteins from late pregnancy to postpartum. Combining the data from normal (n = 9) and GDM subjects (n = 9), the strongest correlation noted was between the change in 312Ser-IRS-1 and the change in ISI (r2 = 0.302, P < 0.02) (Fig. 6A). There was also a correlation between skeletal muscle TNF-α mRNA and 312Ser-IRS-1/total IRS-1 (r2 = 0.19, P < 0.03) (Fig. 6B), and between the change in plasma TNF-α and the change in insulin resistance (r2 = 0.52, P < 0.03) (not shown).
FIG. 5.
TNF-α during late pregnancy (30–36 weeks; □) and ~1 year postpartum (■). Data are presented as mean ± SE for obese women with GDM during pregnancy (n = 9) and women with NGT during pregnancy (n = 9). A: Plasma TNF-α was measured by ELISA. Data are mean ± SE, n = 9. *P < 0.05. B: Skeletal muscle TNF-α mRNA expression was measured by quantitative real-time PCR. Data are mean ± SE, n = 9. *P < 0.005 vs. NGT during late pregnancy, **P < 0.02 vs. GDM during late pregnancy. Data for NGT patients were reported previously (14) and are included for reference purposes.
FIG. 6.
A: Correlation between the change in 312Ser-IRS-1 and the change in ISI from late pregnancy to postpartum in NGT and GDM subjects. B: Correlation between 312Ser-IRS-1/total IRS-1 and TNF-α mRNA in NGT and GDM subjects.
DISCUSSION
Decreased insulin sensitivity with advancing gestation is a hallmark of pregnancy that involves changes in the insulin signaling cascade in human skeletal muscle, as outlined in our previous reports (15,16,18,22,31). To explore whether the mechanisms underlying insulin resistance are reversible in women with GDM, we followed women longitudinally and focused our attention on metabolic characteristics and expression and function of proteins in skeletal muscle biopsies obtained 1 year postpartum. Body weight, fat mass, and fasting glucose increased postpartum in women with GDM. Despite a failure to return to prepregnancy body weight, however, our longitudinal results demonstrate that GDM women experience changes in IR, IRS-1, and p85α expression in skeletal muscle that were similar to those seen previously in women with NGT (14), suggesting these changes were likely due to pregnancy-specific factors.
Despite these positive changes, however, insulin-stimulated IR tyrosine phosphorylation and IRTK activity were not improved, and whole-body insulin resistance was not significantly different in the obese GDM women postpartum. Although lack of postpartum weight loss in GDM subjects suggests that obesity may be a key factor underlying a lack of improvement in IR and IRTK function postpartum, it is also possible that these GDM women may carry an intrinsic defect that interacts with the IR and underlies their genetic prevalence for type 2 diabetes, as suggested recently (32). Ober et al. (33) found that risk for GDM in black and Caucasian subjects was not due to obesity per se but to interactions between obesity and variation in alleles for the IR in Caucasian and African-American women with GDM. They also noted that variation in IR appeared to interact with both BMI and history of diabetes in women with GDM to increase their risk for type 2 diabetes. More studies are necessary to understand the potential for genetic factors that may suppress IR function in former GDM women.
Both IR and IRS-1 serine phosphorylation have been suggested as major mechanisms for insulin resistance in mouse models of obesity and GDM (31,34,35) and in skeletal muscle of obese humans (36). We previously reported that during late pregnancy, obese GDM women had impaired IR and IRTK activity in vitro (18), as well as impaired insulin-stimulated IR and IRS-1 tyrosine phosphorylation in vivo (18). We also demonstrated that treating isolated insulin receptors from GDM women with alkaline phosphatase to remove existing serine phosphorylation resulted in a significant improvement (but not normalization) in insulin-stimulated IRTK activity, suggesting that decrements in insulin-stimulated IRTK activity during late pregnancy may be associated with increased serine kinase activity (18). Our results shown here that 312Ser-IRS-1 is not significantly improved in GDM women postpartum, together with lack of change in IR and IRTK activity, are consistent with a potential for increased serine kinase activity and insulin resistance. Serine phosphorylation of IRS proteins by mTOR-p70S6 kinase (p70S6K1)-dependent mechanism or other kinases, such as TNF-α–induced c-Jun NH2-terminal kinase (JNK), IKKβ, p38, and AMP kinase (rev. in 37) among others, can reduce the ability of IRS proteins to attract PI3K, thus triggering insulin resistance (34,38–42).
A major finding in the present studies is that the level of skeletal muscle TNF-α mRNA was remarkably elevated in obese GDM women during late pregnancy compared with women with NGT (14), and fell significantly postpartum but remained elevated by threefold compared with control women. These results suggest that a component of the pro-inflammatory pathway may be hyperactive locally in skeletal muscle from GDM subjects during pregnancy and remain increased postpartum. Based on the known effects of TNF-α to induce serine phosphorylation of both IR and IRS-1, which in turn impairs tyrosine phosphorylation of IRS-1 (40,43), it is possible that the increased TNF-α expression in skeletal muscle could lead to the marked impairment in whole-body insulin sensitivity in these obese GDM women. The change in 312Ser-IRS-1 postpartum correlated with the change in insulin sensitivity (r2 = 0.302, P < 0.02), while TNF-α mRNA correlated with 312Ser-IRS-1/total IRS-1 (r2 = 0.19, P < 0.03), supporting this concept. Whether the small increases in 312Ser–IRS-1 from late pregnancy to postpartum is attenuating the reversal of insulin resistance in GDM women remains to be determined. Interestingly, in control subjects with NGT, plasma TNF-α fell significantly in the postpartum period. This is consistent with the idea that the increase in circulating TNF-α during late pregnancy is a contribution of placental secretion and is a significant predictor of insulin resistance in late gestation (44). In GDM subjects, however, plasma TNF-α was similar to control subjects during late pregnancy but remained unchanged 1 year postpartum. Using NMR spectroscopy, Kautzky-Willer et al. (45) reported increased intramuscular lipid content in skeletal muscle of obese women with prior GDM. Increased free fatty acid (FFA) uptake and/or lipolysis of stored triglyceride in skeletal muscle of obese women could increase cytosolic long-chain acyl-CoA (LCA-CoA), which correlates with overall obesity (46) and could inhibit insulin action via increased IRS-1 serine phosphorylation (37,47).
We also found a small but significant decrease postpartum in the PI3K regulatory subunit p85α, which contrasts with the two- to threefold elevation found during late pregnancy (16). Under normal conditions, the p85α subunit exists in stochiometric excess to the catalytic p110 subunit, resulting in a pool of free p85 monomers in relation to the p85-p110 dimers, with the latter responsible for PI3K activity (48). An increase in the p85α regulatory subunit, which binds to phosphorylated IRS proteins, can compete with the p85-p110 heterodimer binding to tyrosine-phosphorylated IRS-1, thereby inhibiting PI3K activity and producing insulin resistance (49). In transgenic mice overexpressing human placental growth hormone, at levels similar to the third trimester of pregnancy, there is increased amounts of p85α regulatory subunit in skeletal muscle (50), and this resulted in impaired IRS-1–associated PI3K activity. Likewise, mice with heterozygous disruption of the p85α gene are more insulin-sensitive and display enhanced insulin signaling in skeletal muscle (51). Our data showing a small decline in p85α postpartum are consistent with the proposed role of increased p85α as a cellular mediator of skeletal muscle insulin resistance during pregnancy. The inverse relationship between insulin sensitivity and PI3K subunit ratio has been observed in human and animal models of insulin resistance (52–55), including obesity and type 2 diabetes (36). Finally, insulin resistance in skeletal muscle involves not only increased serine kinase activity and increased p85α, but also, as good evidence suggests, decreased activation downstream from PI3K at the level of Akt-2 (56) and atypical protein J.E. kinase C (PKC) (36,57–62) in patients with obesity and type 2 diabetes.
It is also possible that other circulating factors such as FFA, resistin, adiponectin, etc., may be contributing factors to the insulin resistance in women who do not lose weight postpartum. Impaired insulin-mediated FFA suppression occurs in GDM subjects both in late pregnancy (19) and postpartum in response to IVGTT-induced endogenous insulin secretion (63). The impaired FFA suppression is present in postpartum GDM women with the most severe β-cell dysfunction (those that required insulin during pregnancy) and, thus, this may be related to their insulin secretory dysfunction rather than their reduced insulin sensitivity per se. Indeed, worsening islet function in the face of progressive insulin resistance postpartum is a major determinant in the progression from GDM to type 2 diabetes (6). The earlier in life a woman is diagnosed with GDM, the more likely severe insulin resistance predated the pregnancy. Not losing weight between pregnancies is a clear risk factor for recurrent GDM and development of type 2 diabetes, suggesting that progressive insulin resistance may accelerate the decline in β-cell function that leads to diabetes (64).
In summary, we have observed chronically elevated skeletal muscle TNF-α expression, a lack of change in 312Ser-IRS-1 associated with insulin resistance and decreased insulin signaling in skeletal muscle of obese GDM women 1 year postpartum. The improvement in IR, IRS-1 and slight reduction in p85α found postpartum were similar to those observed previously in subjects with NGT (14), and suggests these changes may be specific to pregnancy-induced mechanisms of insulin resistance. GDM is associated with an extremely high risk (~50%) of developing type 2 diabetes in the subsequent 5–10 years, particularly those with obesity who require insulin during pregnancy and certain ethnic group status (65). Based on oral glucose tolerance testing, this postpartum insulin resistance is not benign. Indeed, seven of the nine women had evidence of either impaired or poor glucose tolerance 1 year postpartum. Thus, our results suggest the mechanisms underlying chronic insulin resistance in former GDM women may be driven by inflammation that impinge on the insulin signaling cascade in skeletal muscle to advance insulin resistance postpartum and may underlie the development of impaired glucose tolerance. The implications of these findings are that interventions to reduce obesity postpartum and possibly limit weight gain during pregnancy are critically needed in GDM women to slow the progression of insulin resistance and perhaps prevent the conversion to type 2 diabetes.
ACKNOWLEDGMENTS
This research was funded by the National Institutes of Health Grants HD-11089 (P.M.C.) and DK-62115 (J.E.F.), American Diabetes Association Clinical Research Grant (1-03.CR-07 to J.E.F), The University of Colorado Denver’s Center for Human Nutrition Metabolic Core Lab Grant (DK P30 DK048520), and the General Clinical Research Center Grant (RR-00080) to Case Western Reserve University. We thank the members of the Friedman laboratory for helpful discussions and particularly Rachel C. Janssen for her helpful assistance in preparation of figures and editing the manuscript.
Glossary
- ELISA
enzyme-linked immunosorbent assay
- FFA
free fatty acid
- GDM
gestational diabetes mellitus
- IR
insulin receptor
- IRS
insulin receptor substrate
- IRTK
insulin receptor tyrosine kinase
- ISI
insulin sensitivity index
- NGT
normal glucose tolerance
- OGTT
oral glucose tolerance test
- PI3K
phosphoinositide 3-kinase
REFERENCES
- 1.Buchanan TA, Xiang AH. Gestational diabetes mellitus. J Clin Invest. 2005;115:485–491. doi: 10.1172/JCI24531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Catalano PM, Huston L, Amini SB, Kalhan SC. Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes mellitus. Am J Obstet Gynecol. 1999;180:903–916. doi: 10.1016/s0002-9378(99)70662-9. [DOI] [PubMed] [Google Scholar]
- 3.Kaufmann RC, Schleyhahn FT, Huffman DG, Amankwah KS. Gestational diabetes diagnostic criteria: long-term maternal follow-up. Am J Obstet Gynecol. 1995;172:621–625. doi: 10.1016/0002-9378(95)90582-0. [DOI] [PubMed] [Google Scholar]
- 4.Kjos SL, Peters RK, Xiang A, Henry OA, Montoro M, Buchanan TA. Predicting future diabetes in Latino women with gestational diabetes: utility of early postpartum glucose tolerance testing. Diabetes. 1995;44:586–591. doi: 10.2337/diab.44.5.586. [DOI] [PubMed] [Google Scholar]
- 5.Kjos SL, Buchanan TA. Gestational diabetes mellitus. N Engl J Med. 1999;341:1749–1756. doi: 10.1056/NEJM199912023412307. [DOI] [PubMed] [Google Scholar]
- 6.Xiang AH, Wang C, Peters RK, Trigo E, Kjos SL, Buchanan TA. Coordinate changes in plasma glucose and pancreatic beta-cell function in Latino women at high risk for type 2 diabetes. Diabetes. 2006;55:1074–1079. doi: 10.2337/diabetes.55.04.06.db05-1109. [DOI] [PubMed] [Google Scholar]
- 7.Buchanan TA, Xiang A, Kjos SL, Watanabe R. What is gestational diabetes? Diabetes Care. 2007;30(Suppl. 2):S105–S111. doi: 10.2337/dc07-s201. [DOI] [PubMed] [Google Scholar]
- 8.Kousta E, Cela E, Lawrence N, Penny A, Millauer B, White D, Wilson H, Robinson S, Johnston D, McCarthy M, Franks S. The prevalence of polycystic ovaries in women with a history of gestational diabetes. Clin Endocrinol (Oxf) 2000;53:501–507. doi: 10.1046/j.1365-2265.2000.01123.x. [DOI] [PubMed] [Google Scholar]
- 9.Meyers-Seifer CH, Vohr BR. Lipid levels in former gestational diabetic mothers. Diabetes Care. 1996;19:1351–1356. doi: 10.2337/diacare.19.12.1351. [DOI] [PubMed] [Google Scholar]
- 10.O’Sullivan JB. Subsequent morbidity among gestational diabetic women. In: Sutherland HW, Stowers JM, editors. Carbohydrate Metabolism in Pregnancy and the Newborn. Edinburgh: Churchhill Livingstone; 1984. pp. 174–180. [Google Scholar]
- 11.Heitritter SM, Solomon CG, Mitchell GF, Skali-Ounis N, Seely EW. Subclinical inflammation and vascular dysfunction in women with previous gestational diabetes mellitus. J Clin Endocrinol Metab. 2005;90:3983–3988. doi: 10.1210/jc.2004-2494. [DOI] [PubMed] [Google Scholar]
- 12.Winzer C, Wagner O, Festa A, Schneider B, Roden M, Bancher-Todesca D, Pacini G, Funahashi T, Kautzky-Willer A. Plasma adiponectin, insulin sensitivity, and subclinical inflammation in women with prior gestational diabetes mellitus. Diabetes Care. 2004;27:1721–1727. doi: 10.2337/diacare.27.7.1721. [DOI] [PubMed] [Google Scholar]
- 13.Di Benedetto A, Russo GT, Corrado F, Di Cesare E, Alessi E, Nicocia G, D’Anna R, Cucinotta D. Inflammatory markers in women with a recent history of gestational diabetes mellitus. J Endocr Invest. 2005;28:34. doi: 10.1007/BF03345527. [DOI] [PubMed] [Google Scholar]
- 14.Kirwan JP, Varastehpour A, Jing M, Presley L, Shao J, Friedman JE, Catalano PM. Reversal of insulin resistance postpartum is linked to enhanced skeletal muscle insulin signaling. J Clin Endocrinol Metab. 2004;89:4678–4684. doi: 10.1210/jc.2004-0749. [DOI] [PubMed] [Google Scholar]
- 15.Barbour LA, McCurdy CE, Hernandez TL, Kirwan JP, Catalano PM, Friedman JE. Cellular mechanisms for insulin resistance in normal pregnancy and gestational diabetes. Diabetes Care. 2007;30:S112–S119. doi: 10.2337/dc07-s202. [DOI] [PubMed] [Google Scholar]
- 16.Friedman JE, Ishizuka T, Shao J, Huston L, Highman T, Catalano P. Impaired glucose transport and insulin receptor tyrosine phosphorylation in skeletal muscle from obese women with gestational diabetes. Diabetes. 1999;48:1807–1814. doi: 10.2337/diabetes.48.9.1807. [DOI] [PubMed] [Google Scholar]
- 17.Catalano PM, Tyzbir ED, Wolfe RR, Calles J, Roman NM, Amini SB, Sims EA. Carbohydrate metabolism during pregnancy in control subjects and women with gestational diabetes. Am J Physiol. 1993;264:E60–E67. doi: 10.1152/ajpendo.1993.264.1.E60. [DOI] [PubMed] [Google Scholar]
- 18.Shao J, Catalano PM, Yamashita H, Ruyter I, Smith S, Youngren J, Friedman JE. Decreased insulin receptor tyrosine kinase activity and plasma cell membrane glycoprotein-1 overexpression in skeletal muscle from obese women with gestational diabetes mellitus (GDM): evidence for increased serine/threonine phosphorylation in pregnancy and GDM. Diabetes. 2000;49:603–610. doi: 10.2337/diabetes.49.4.603. [DOI] [PubMed] [Google Scholar]
- 19.Catalano PM, Nizielski SE, Shao J, Preston L, Qiao L, Friedman JE. Downregulated IRS-1 and PPARgamma in obese women with gestational diabetes: relationship to FFA during pregnancy. Am J Physiol Endocrinol Metab. 2002;282:E522–E533. doi: 10.1152/ajpendo.00124.2001. [DOI] [PubMed] [Google Scholar]
- 20.Garvey WT, Maianu L, Zhu JH, Hancock JA, Golichowski AM. Multiple defects in the adipocyte glucose transport system cause cellular insulin resistance in gestational diabetes: heterogeneity in the number and a novel abnormality in subcellular localization of GLUT4 glucose transporters. Diabetes. 1993;42:1773–1785. doi: 10.2337/diab.42.12.1773. [DOI] [PubMed] [Google Scholar]
- 21.Ciaraldi TP, Kettel M, el-Roeiy A, Madar Z, Reichart D, Yen SS, Olefsky JM. Mechanisms of cellular insulin resistance in human pregnancy. Am J Obstet Gynecol. 1994;170:635–641. doi: 10.1016/s0002-9378(94)70241-1. [DOI] [PubMed] [Google Scholar]
- 22.Shao J, Catalano PM, Yamashita H, Ishizuka T, Friedman JE. Vanadate enhances but does not normalize glucose transport and insulin receptor phosphorylation in skeletal muscle from obese women with gestational diabetes mellitus. Am J Obstet Gynecol. 2000;183:1263–1270. doi: 10.1067/mob.2000.106816. [DOI] [PubMed] [Google Scholar]
- 23.Coustan DR, Carpenter MW. The diagnosis of gestational diabetes. Diabetes Care. 1998;21(Suppl. 2):B5–B8. [PubMed] [Google Scholar]
- 24.Taylor HL, Jacobs DR, Jr, Schucker B, Knudsen J, Leon AS, Debacker G. A questionnaire for the assessment of leisure time physical activities. J Chronic Dis. 1978;31:741–755. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- 25.American Diabetes Association: Diagnosis and classification of diabetes mellitus. Diabetes Care. 2007;30(Suppl. 1):S42–S47. doi: 10.2337/dc07-S042. [DOI] [PubMed] [Google Scholar]
- 26.Catalano PM, Wong WW, Drago NM, Amini SB. Estimating body composition in late gestation: a new hydration constant for body density and total body water. Am J Physiol. 1995;268:E153–E158. doi: 10.1152/ajpendo.1995.268.1.E153. [DOI] [PubMed] [Google Scholar]
- 27.Kirwan JP, Huston-Presley L, Kalhan SC, Catalano PM. Clinically useful estimates of insulin sensitivity during pregnancy: validation studies in women with normal glucose tolerance and gestational diabetes mellitus. Diabetes Care. 2001;24:1602–1607. doi: 10.2337/diacare.24.9.1602. [DOI] [PubMed] [Google Scholar]
- 28.Kirwan JP, del Aguila LF, Hernandez JM, Williamson DL, O’Gorman DJ, Lewis R, Krishnan RK. Regular exercise enhances insulin activation of IRS-1-associated PI3-kinase in human skeletal muscle. J Appl Physiol. 2000;88:797–803. doi: 10.1152/jappl.2000.88.2.797. [DOI] [PubMed] [Google Scholar]
- 29.Pender C, Goldfine ID, Kulp JL, Tanner CJ, Maddux BA, MacDonald KG, Houmard JA, Youngren JF. Analysis of insulin-stimulated insulin receptor activation and glucose transport in cultured skeletal muscle cells from obese subjects. Metabolism. 2005;54:598–603. doi: 10.1016/j.metabol.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 30.Boden G, Shulman GI. Free fatty acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and beta-cell dysfunction. Eur J Clin Invest. 2002;32(Suppl. 3):14–23. doi: 10.1046/j.1365-2362.32.s3.3.x. [DOI] [PubMed] [Google Scholar]
- 31.Shao J, Yamashita H, Qiao L, Draznin B, Friedman JE. Phosphatidylinositol 3-kinase redistribution is associated with skeletal muscle insulin resistance in gestational diabetes mellitus. Diabetes. 2002;51:19–29. doi: 10.2337/diabetes.51.1.19. [DOI] [PubMed] [Google Scholar]
- 32.Watanabe RM, Black MH, Xiang AH, Allayee H, Lawrence JM, Buchanan TA. Genetics of gestational diabetes mellitus and type 2 diabetes. Diabetes Care. 2007;30(Suppl. 2):S134–S140. doi: 10.2337/dc07-s205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ober C, Xiang KS, Thisted RA, Indovina KA, Wason CJ, Dooley S. Increased risk for gestational diabetes mellitus associated with insulin receptor and insulin-like growth factor II restriction fragment length polymorphisms. Genet Epidemiol. 1989;6:559–569. doi: 10.1002/gepi.1370060502. [DOI] [PubMed] [Google Scholar]
- 34.Um SH, Frigerio F, Watanabe M, Picard F, Joaquin M, Sticker M, Fumagalli S, Allegrini PR, Kozma SC, Auwerx J, Thomas G. Absence of S6K1 protects against age- and diet-induced obesity while enhancing insulin sensitivity. Nature. 2004;431:200–205. doi: 10.1038/nature02866. [DOI] [PubMed] [Google Scholar]
- 35.Hirosumi J, Tuncman G, Chang L, Gorgun CZ, Uysal KT, Maeda K, Karin M, Hotamisligil GS. A central role for JNK in obesity and insulin resistance. Nature. 2002;420:333–336. doi: 10.1038/nature01137. [DOI] [PubMed] [Google Scholar]
- 36.Bandyopadhyay GK, Yu JG, Ofrecio J, Olefsky JM. Increased p85/55/50 expression and decreased phosphotidylinositol 3-kinase activity in insulin-resistant human skeletal muscle. Diabetes. 2005;54:2351–2359. doi: 10.2337/diabetes.54.8.2351. [DOI] [PubMed] [Google Scholar]
- 37.Herschkovitz A, Liu YF, Ilan E, Ronen D, Boura-Halfon S, Zick Y. Common inhibitory serine sites phosphorylated by IRS-1 kinases, triggered by insulin and inducers of insulin resistance. J Biol Chem. 2007;282:18018–18027. doi: 10.1074/jbc.M610949200. [DOI] [PubMed] [Google Scholar]
- 38.Patti ME, Kahn BB. Nutrient sensor links obesity with diabetes risk. Nat Med. 2004;10:1049–1050. doi: 10.1038/nm1004-1049. [DOI] [PubMed] [Google Scholar]
- 39.Birnbaum MJ. Turning down insulin signaling. J Clin Invest. 2001;108:655–659. doi: 10.1172/JCI13714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aguirre V, Werner ED, Giraud J, Lee YH, Shoelson SE, White MF. Phosphorylation of Ser307 in insulin receptor substrate-1 blocks interactions with the insulin receptor and inhibits insulin action. J Biol Chem. 2002;277:1531–1537. doi: 10.1074/jbc.M101521200. [DOI] [PubMed] [Google Scholar]
- 41.Lee YH, White MF. Insulin receptor substrate proteins and diabetes. Arch Pharm Res. 2004;27:361–370. doi: 10.1007/BF02980074. [DOI] [PubMed] [Google Scholar]
- 42.Hotamisligil GS, Peraldi P, Budavari A, Ellis R, White MF, Spiegelman BM. IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-alpha- and obesity-induced insulin resistance. Science. 1996;271:665–668. doi: 10.1126/science.271.5249.665. [DOI] [PubMed] [Google Scholar]
- 43.Zick Y. Role of Ser/Thr kinases in the uncoupling of insulin signaling. Int J Obes Relat Metab Disord. 2003;27(Suppl. 3):S56–S60. doi: 10.1038/sj.ijo.0802503. [DOI] [PubMed] [Google Scholar]
- 44.Kirwan JP, Hauguel-De Mouzon S, Lepercq J, Challier JC, Huston-Presley L, Friedman JE, Kalhan SC, Catalano PM. TNF-alpha is a predictor of insulin resistance in human pregnancy. Diabetes. 2002;51:2207–2213. doi: 10.2337/diabetes.51.7.2207. [DOI] [PubMed] [Google Scholar]
- 45.Kautzky-Willer A, Krssak M, Winzer C, Pacini G, Tura A, Farhan S, Wagner O, Brabant G, Horn R, Stingl H, Schneider B, Waldhausl W, Roden M. Increased intramyocellular lipid concentration identifies impaired glucose metabolism in women with previous gestational diabetes. Diabetes. 2003;52:244–251. doi: 10.2337/diabetes.52.2.244. [DOI] [PubMed] [Google Scholar]
- 46.Oakes ND, Bell KS, Furler SM, Camilleri S, Saha AK, Ruderman NB, Chisholm DJ, Kraegen EW. Diet-induced muscle insulin resistance in rats is ameliorated by acute dietary lipid withdrawal or a single bout of exercise: parallel relationship between insulin stimulation of glucose uptake and suppression of long-chain fatty acyl-CoA. Diabetes. 1997;46:2022–2028. doi: 10.2337/diab.46.12.2022. [DOI] [PubMed] [Google Scholar]
- 47.Savage DB, Petersen KF, Shulman GI. Disordered lipid metabolism and the pathogenesis of insulin resistance. Physiol Rev. 2007;87:507–520. doi: 10.1152/physrev.00024.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ueki K, Fruman DA, Brachmann SM, Tseng YH, Cantley LC, Kahn CR. Molecular balance between the regulatory and catalytic subunits of phosphoinositide 3-kinase regulates cell signaling and survival. Mol Cell Biol. 2002;22:965–977. doi: 10.1128/MCB.22.3.965-977.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ueki K, Algenstaedt P, Mauvais-Jarvis F, Kahn CR. Positive and negative regulation of phosphoinositide 3-kinase-dependent signaling pathways by three different gene products of the p85alpha regulatory subunit. Mol Cell Biol. 2000;20:8035–8046. doi: 10.1128/mcb.20.21.8035-8046.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barbour LA, Shao J, Qiao L, Pulawa LK, Jensen DR, Bartke A, Garrity M, Draznin B, Friedman JE. Human placental growth hormone causes severe insulin resistance in transgenic mice. Am J Obstet Gynecol. 2002;186:512–517. doi: 10.1067/mob.2002.121256. [DOI] [PubMed] [Google Scholar]
- 51.Barbour LA, Mizanoor Rahman S, Gurevich I, Leitner JW, Fischer SJ, Roper MD, Knotts TA, Vo Y, McCurdy CE, Yakar S, Leroith D, Kahn CR, Cantley LC, Friedman JE, Draznin B. Increased P85alpha is a potent negative regulator of skeletal muscle insulin signaling and induces in vivo insulin resistance associated with growth hormone excess. J Biol Chem. 2005;280:37489–37494. doi: 10.1074/jbc.M506967200. [DOI] [PubMed] [Google Scholar]
- 52.Kim YB, Ciaraldi TP, Kong A, Kim D, Chu N, Mohideen P, Mudaliar S, Henry RR, Kahn BB. Troglitazone but not metformin restores insulin-stimulated phosphoinositide 3-kinase activity and increases p110beta protein levels in skeletal muscle of type 2 diabetic subjects. Diabetes. 2002;51:443–448. doi: 10.2337/diabetes.51.2.443. [DOI] [PubMed] [Google Scholar]
- 53.Mauvais-Jarvis F, Ueki K, Fruman DA, Hirshman MF, Sakamoto K, Goodyear LJ, Iannacone M, Accili D, Cantley LC, Kahn CR. Reduced expression of the murine p85alpha subunit of phosphoinositide 3-kinase improves insulin signaling and ameliorates diabetes. J Clin Invest. 2002;109:141–149. doi: 10.1172/JCI13305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Terauchi Y, Tsuji Y, Satoh S, Minoura H, Murakami K, Okuno A, Inukai K, Asano T, Kaburagi Y, Ueki K, Nakajima H, Hanafusa T, Matsuzawa Y, Sekihara H, Yin Y, Barrett JC, Oda H, Ishikawa T, Akanuma Y, Komuro I, Suzuki M, Yamamura K, Kodama T, Suzuki H, Yamamura K, Kodama T, Suzuki H, Koyasu S, Aizawa S, Tobe K, Fukui Y, Yazaki Y, Kadowaki T. Increased insulin sensitivity and hypoglycaemia in mice lacking the p85 alpha subunit of phosphoinositide 3-kinase. Nat Genet. 1999;21:230–235. doi: 10.1038/6023. [DOI] [PubMed] [Google Scholar]
- 55.Chen D, Mauvais-Jarvis F, Bluher M, Fisher SJ, Jozsi A, Goodyear LJ, Ueki K, Kahn CR. p50alpha/p55alpha phosphoinositide 3-kinase knockout mice exhibit enhanced insulin sensitivity. Mol Cell Biol. 2004;24:320–329. doi: 10.1128/MCB.24.1.320-329.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Karlsson HK, Zierath JR, Kane S, Krook A, Lienhard GE, Wallberg-Henriksson H. Insulin-stimulated phosphorylation of the Akt substrate AS160 is impaired in skeletal muscle of type 2 diabetic subjects. Diabetes. 2005;54:1692–1697. doi: 10.2337/diabetes.54.6.1692. [DOI] [PubMed] [Google Scholar]
- 57.Leng Y, Karlsson HK, Zierath JR. Insulin signaling defects in type 2 diabetes. Rev Endocr Metab Disord. 2004;5:111–117. doi: 10.1023/B:REMD.0000021432.84588.f6. [DOI] [PubMed] [Google Scholar]
- 58.Kim YB, Nikoulina SE, Ciaraldi TP, Henry RR, Kahn BB. Normal insulin-dependent activation of Akt/protein kinase B, with diminished activation of phosphoinositide 3-kinase, in muscle in type 2 diabetes. J Clin Invest. 1999;104:733–741. doi: 10.1172/JCI6928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goodyear LJ, Giorgino F, Sherman LA, Carey J, Smith RJ, Dohm GL. Insulin receptor phosphorylation, insulin receptor substrate-1 phosphorylation, and phosphatidylinositol 3-kinase activity are decreased in intact skeletal muscle strips from obese subjects. J Clin Invest. 1995;95:2195–2204. doi: 10.1172/JCI117909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sajan MP, Standaert ML, Miura A, Bandyopadhyay G, Vollenweider P, Franklin DM, Lea-Currie R, Farese RV. Impaired activation of protein kinase C-zeta by insulin and phosphatidylinositol-3,4,5-(PO4)3 in cultured preadipocyte-derived adipocytes and myotubes of obese subjects. J Clin Endocrinol Metab. 2004;89:3994–3998. doi: 10.1210/jc.2004-0106. [DOI] [PubMed] [Google Scholar]
- 61.Bjornholm M, Kawano Y, Lehtihet M, Zierath JR. Insulin receptor substrate-1 phosphorylation and phosphatidylinositol 3-kinase activity in skeletal muscle from NIDDM subjects after in vivo insulin stimulation. Diabetes. 1997;46:524–527. doi: 10.2337/diab.46.3.524. [DOI] [PubMed] [Google Scholar]
- 62.Farese RV, Sajan MP, Yang H, Li P, Mastorides S, Gower WR, Jr, Nimal S, Choi CS, Kim S, Shulman GI, Kahn CR, Braun U, Leitges M. Muscle-specific knockout of PKC-lambda impairs glucose transport and induces metabolic and diabetic syndromes. J Clin Invest. 2007;117:2289–2301. doi: 10.1172/JCI31408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McLachlan KA, Boston R, Alford FP. Impaired non-esterified fatty acid suppression to intravenous glucose during late pregnancy persists postpartum in gestational diabetes: a dominant role for decreased insulin secretion rather than insulin resistance. Diabetologia. 2005;48:1373–1379. doi: 10.1007/s00125-005-1775-6. [DOI] [PubMed] [Google Scholar]
- 64.Peters RK, Kjos SL, Xiang A, Buchanan TA. Long-term diabetogenic effect of single pregnancy in women with previous gestational diabetes mellitus. Lancet. 1996;347:227–230. doi: 10.1016/s0140-6736(96)90405-5. [DOI] [PubMed] [Google Scholar]
- 65.Major CA, deVeciana M, Weeks J, Morgan MA. Recurrence of gestational diabetes: who is at risk? Am J Obstet Gynecol. 1998;179:1038–1042. doi: 10.1016/s0002-9378(98)70211-x. [DOI] [PubMed] [Google Scholar]