Abstract
Background:
Acute bacterial meningitis (ABM) is an important cause of morbidity and mortality throughout the world. It is an acute medical emergency that requires urgent rational antibiotic therapy, especially in neonates and young infants. Determining the pattern and susceptibility of isolates of ABM among children for prompt treatment of this important cause of mortality and morbidity is very important. This study determined the types and the antimicrobial susceptibility pattern of ABM isolates among children at the National Hospital, Abuja.
Materials and Methods:
This is a retrospective study carried out at the National Hospital Abuja (NHA), Nigeria. Laboratory data for a period of 3 years, January 2010-December 2013 were reviewed, and all bacterial isolates and their antibiotics sensitivity testing results for children aged 0-15 years, and other relevant information extracted and analyzed. Study center was the NHA.
Results:
Twenty-eight bacterial pathogens were isolated from a total of 542 cerebrospinal specimens over the study period, giving a yield of 5.2%. The four most common pathogens isolated were Staphylococcus aureus (32.2%), Klebsiella pneumoniae (21.5%), Streptococcus pneumoniae (17.6%), and Escherichia coli (14.3%). Whereas, 28.6% of all the infections occurred in neonates alone, children 2 years and below had 85.7% of all the infections, with male preponderance. Isolates of S. aureus and S. pneumonia tested were both 100% susceptible to amoxicillin-clavulanic acid and Cefuroxime; S. pneumoniae was equally sensitive to Ceftriaxone. K. pneumoniae was 100% sensitive to Imipenem, but 83% to ceftriaxone. 75% of the isolated E. coli strains were sensitive to ceftriaxone, amoxicillin-clavulanic acid, and amikacin, 100% sensitive to imipenem.
Conclusion:
Meningitis in children as seen in the National hospital is almost equally caused by both Gram-positive and Gram-negative organisms, predominantly by S. aureus, S. pneumoniae, K. pneumoniae, and E. coli. Available drugs remain active against these organisms.
Keywords: Acute bacterial meningitis, children, isolates
INTRODUCTION
Acute bacterial meningitis (ABM) is an important cause of morbidity and mortality throughout the world, despite advances in medical treatment.1,2,3 The mortality rate of 2.7% in infants among hospitalized children in Ilorin4 and 3.4% in postneonatal children in a Sokoto Hospital5 both in Nigeria have been reported. It is an acute medical emergency that requires urgent rational antibiotic therapy, especially in neonates and young infants.6 It is among the most common neurological disorders in children in the tropical countries.2 Bacterial meningitis has a global incidence of about 20-100 cases/100,000 live births during the newborn period.7 In the Northern parts of Nigeria, large epidemics of meningitis occur periodically, particularly during the hot, dry season.8,9,10,11 The etiologic agents of meningitis and their antibiotic susceptibility vary from place to place and, therefore, knowledge of the locally predominant organisms in different age groups and their sensitivity pattern is essential for correct and timely management of meningitis. Furthermore, for a potentially fatal infection like childhood meningitis, the need for periodic assessment of the continuing sensitivity of the causative agents to antimicrobial in use is necessary. This is particularly essential, especially where there are no rapid investigative modalities, leaving the clinician with no option but to initiate empirical treatment.
There have been some published studies regarding meningitis in various parts of this country,5,6,12 but there is no available data in Abuja. The objective of this study was, therefore, to analyze the pattern and antimicrobial sensitivity of pathogens isolated from the cerebrospinal fluid (CSF) of children with suspected ABM in National Hospital Abuja (NHA).
MATERIALS AND METHODS
This was a retrospective study done at the NHA, a 200-bed referral tertiary hospital located in Federal Capital Territory of Nigeria. It has well-equipped Special Care Baby Unit, Neonatal Intensive Care Unit, Emergency Pediatric Unit, and In-Patient Pediatric Ward. The records from CSF register of the Medical Microbiology Laboratory of NHA from January 1, 2010, to December 31, 2012, were evaluated. Samples with incomplete data were excluded from the study. In our facility, CSF samples collected in sterile plastic bottles from suspected meningitis patients and submitted at the microbiology laboratory are usually processed as soon as they are received. The macroscopic appearances of the samples are noted, while a well-mixed CSF charged into counting chamber using sterile Pasteur pipette for cell counting is done. Direct smears of specimens are then made on a clean glass slide, fixed and stained by Gram's standard method.13 The remaining CSF samples are then centrifuged inside sterile tubes, and the sediments inoculated onto chocolate, MacConkey, and blood agar plates.14 The plates are then incubated at 37°C in ambient air for 24 h, but chocolate agar plates are incubated in a candle light jar for 24 h. Cultures are examined for growth. If there is no growth, cultures are re-incubated for another 24 h before they are discarded as having no growth. The colonies are identified using standard methods.13,14 Antimicrobial drug susceptibility of the isolates are usually tested by the modified Kirby-Bauer technique and results interpreted according to the Clinical Laboratory Standards Institute guideline.15
RESULTS
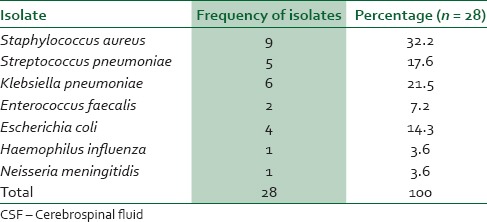
Out of a total of 542 CSF samples submitted and processed, 28 (yield of 5.2%) were culture-positive, only 14 (50%) of the culture-positive samples were turbid in appearance. 16 (57%) of the culture-positives were by culture only and 12 (43%) by direct smear and culture. The most common bacterial isolates were Staphylococcus aureus 9 (32.2%), Streptococcus pneumoniae (17.6%), Klebsiella pneumoniae (21.5%), and Escherichia coli (14.3%) [Table 1].
Table 1.
Isolates from CSF
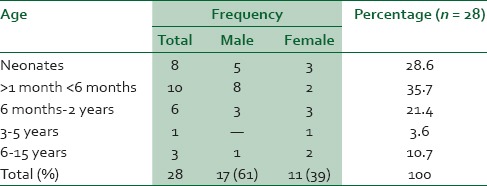
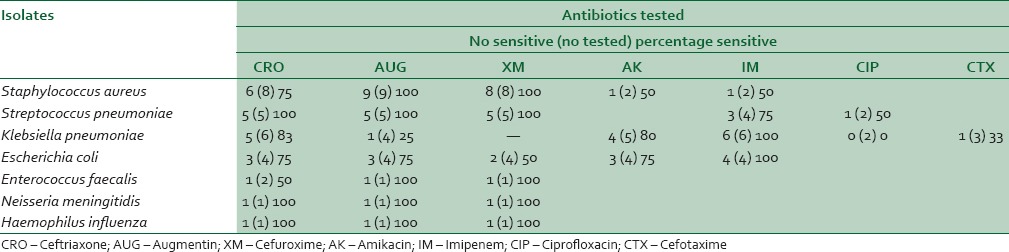
Seventeen (61.1%) were from males and 11 (38.9%) from females. The mean age of patients was 27.3 months, with modal age at > 1 month to <6 age groups [Table 2]. S. aureus and S. pneumoniae tested were both 100% susceptible to amoxicillin-clavulanic acid and cefuroxime; S. pneumoniae was equally sensitive to ceftriaxone.
Table 2.
The age distribution of children with microbiology proven meningitis
K. pneumoniae was 100% sensitive to imipenem but 83% to ceftriaxone. 75% of the isolated E. coli strains were sensitive to ceftriaxone, amoxicillin-clavulanic acid and amikacin, while 100% were sensitive to imipenem [Table 3].
Table 3.
Susceptibility pattern of isolates
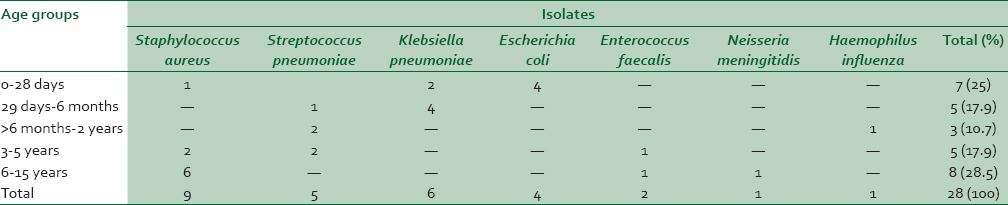
About 89.3% of all infections occurred in children under 5 years, especially in neonates (28.6%), while 10.7% occurred in children 6-15 years. 11 of 12 (91.2%) of all Gram-negative infections occurred in children 2 years and below, while 12 of 16 (75%) of all Gram-positive infections occurred in children 3 years and above [Table 4].
Table 4.
Distribution of isolates according to age groups
DISCUSSION
The CSF culture yield of pathogens of 5.2% in this study is similar to the yield of 6.2% in a similar study in Ibadan.16 However, the prevalence was higher than the ones reported from Shagamu (2.8%),3 Maiduguri (3.5%),17 Enugu (3.1%),18 and more recently from Ilesha (1.6%).4 These differences may be due to differences in hospital practices with respect to infection control, difference in methodology and the detecting systems, as well as access and use of antibiotics prior to sample collection.
This study has also demonstrated that meningitis is more common in males than females. The male preponderance of 1.5: 1 in this study agrees with the finding in Zaria19 of 1.4: 1. This male preponderance may be due to the relative absence of a gene locus for the elaboration of immunoglobulin, which has been documented to be located on the X chromosomes.20 It is also revealed that most Gram-negative bacterial meningitis in children occurred in those below 2 years, while Gram-positive infections occurred in those above 2 years. This finding, which probably reflects the different ecological environment of the children, will be of great guidance in the selection of empiric drug therapy.
Whereas, previous studies have found that ABM in infants accounted for 33% of all cases in children,16,21 our study showed that children under 6 months accounted for 64% of all cases. The incidence of meningitis in infants may be partly due to the vulnerability of their choroid plexus to penetration by bacteria during the septicemic process and to low immunological status.22,23 Although Gram-positive pathogens appeared slightly higher in the etiology of ABM than Gram-negatives (57% vs. 43%), the difference is not statistically significant (P > 0.05). The isolation of S. aureus as the most common pathogen agrees with the finding in a study in India.24 Overall the four most common organisms causing acute bacterial meningitis (ABM) among children in Abuja are S. aureus, K. pneumoniae, S. pneumoniae, and E. coli. These together accounted for 86% of the isolates. This largely contrasts with the pattern in studies done in other parts of the country where S. pneumonia, Neisseria meningitides, Haemophilus influenzae, and E. coli predominate.6,8,12 The reason for this difference cannot be easily explained. The predominance S. aureus, an uncommon agent of ACM, in children of school age may suggest a hematogenous spread to the central nervous system from skin and soft tissue infections. A prospective study will elucidate this further.
The low yield of CSF may be partly due to use of antibiotics prior to presentation and sample collection. The incorporation of newer diagnostic methods such as latex agglutination and polymerase chain reaction will improve the diagnosis.
The high rates of sensitivity of most of the predominant pathogens to amoxicillin-clavulanic acid, cefuroxime, ceftriaxone, amikacin, and imipenem is gladdening and may be due to their restricted use in the hospital. They are also expensive and not easily affordable by a large population of patients. This situation offers clinician a range of choice for empiric treatment in emergency situations like ABM. Institutionalization of rational use of antibiotics, especially in this pediatric group, will, therefore, help prolong the usage lives of these antibiotics.
CONCLUSION
Both Gram-positive and Gram-negative organisms substantially contribute to the etiology of ABM, and locally available antibiotics remain effective against the pathogens. The lack of data, leading to the exclusion of some samples in this study was a significant limitation. A well-designed prospective study will be needed to adequately characterize the etiologies of ABM in children, and also monitor the trend in sensitivity to antibiotics.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bell WE. Bacterial meningitis in children. Selected aspects. Pediatr Clin North Am. 1992;39:651–68. doi: 10.1016/s0031-3955(16)38369-9. [DOI] [PubMed] [Google Scholar]
- 2.Izuora GI. Inflammatory diseases of the central nervous system. In: Azubuike JC, Nkanginieme KE, editors. Paeditrics and Child Health in a Tropical Region. Owerri: African Educational Series; 1999. pp. 362–99. [Google Scholar]
- 3.Olanrewaju DM, Olusanya O, Laditan AA. Acute bacterial meningitis in children. West Afr J Med. 1991;10:405–11. [PubMed] [Google Scholar]
- 4.Fagbule D, Joiner KT. Pattern of childhood mortality at the University of Ilorin teaching hospital. Niger J Paediatr. 1987;4:1–5. [Google Scholar]
- 5.Ibrahim M, Udomah MG, Abduwahab I. Infant mortality at the Usmanu Danfodiyo university teaching hospital, Sokoto. Niger J Paediatr. 1993;20:17–20. [Google Scholar]
- 6.Ogunlesi TA, Okeniyi JA, Oyelami OA. Pyogenic meningitis in Ilesa, Nigeria. Indian Pediatr. 2005;42:1019–23. [PubMed] [Google Scholar]
- 7.World Health Organization. Detecting meningococcal meningitis epidemics in highly endemic African countries. Wkly Epidemiol Rec. 2003;78:294–6. [Google Scholar]
- 8.Alausa KO, Osoba AO. Aetiology of acute bacterial meningitis in Ibadan. Nigerian J Paediatr. 1974;1:57–63. [Google Scholar]
- 9.Baird DR, Whittle HC, Greenwood BM. Mortality from pneumococcal meningitis. Lancet. 1976;2:1344–6. doi: 10.1016/s0140-6736(76)91985-1. [DOI] [PubMed] [Google Scholar]
- 10.Horn DW. The epidemic of cerebrospinal fever in the northern provinces of Nigeria, 1949-1950. J R Sanit Inst. 1951;71:573–89. doi: 10.1177/175791395107100517. [DOI] [PubMed] [Google Scholar]
- 11.Greenwood BM, Bradley AK, Cleland PG, Haggie MH, Hassan-King M, Lewis LS, et al. An epidemic of meningococcal infection at Zaria, Northern Nigeria 1. General epidemiological features. Trans R Soc Trop Med Hyg. 1979;73:557–62. doi: 10.1016/0035-9203(79)90052-x. [DOI] [PubMed] [Google Scholar]
- 12.Mado SM, Aikhionbare HA, Akpede GO. Pattern and antimicrobial sensitivity of pathogens in acute bacterial meningitis beyond neonatal period at Ahmadu Bello University Teaching Hospital (ABUTH) Shika, Zaria. Niger J Paediatr. 2013;40:70–4. [Google Scholar]
- 13.Barrow GI, Feltham RKA. 3rd ed. Cambridge: Cambridge University Press; 1993. Cowan and Steel's Manual for the Identification of Medical Bacteria; p. 156. [Google Scholar]
- 14.Cheesbrough M. Revised Reprint. London: Elsevier Health Sciences; 1989. Medical Laboratory Manual for Tropical Countries Vol. II Microbiology; pp. 160–71. [Google Scholar]
- 15.Wayen, USA: Clinical and Laboratory Standards Institute; 2009. CLSI. Performance Standards for Antimicrobial Susceptibility Testing. CLSI Approved Standard M100-S15. [Google Scholar]
- 16.Alausa OK, Onile BA. The pattern of bacterial meningitis in Ibadan (A 21-month prospective study) Niger Med J. 1984;14:167–70. [Google Scholar]
- 17.Akpede GO, Adeyemi O, Abba AA, Sykes RM. Pattern and antibiotic susceptibility of bacteria in pyogenic meningitis in a children's emergency room population in Maiduguri, Nigeria, 1988-1992. Acta Paediatr. 1994;83:719–23. doi: 10.1111/j.1651-2227.1994.tb13126.x. [DOI] [PubMed] [Google Scholar]
- 18.Ojinaka NC, Iloeje SO. Neurological complications of childhood bacterial meninigitis as seen in Enugu. Niger J Paediatr. 1998;25:53–6. [Google Scholar]
- 19.Mado SM, Aikhionbare HA, Akpede GO. Pattern and antimicrobial sensitivity of pathogens in acute bacterial meningitis beyond neonatal period at Ahmadu Bello University Teaching Hospital (ABUTH) Shika, Zaria. Nigerian Journal of Paediatrics. 2013;40:70–4. [Google Scholar]
- 20.Washburn TC, Medearis DN, Jr, Childs B. Sex differences in susceptibility to infections. Pediatrics. 1965;35:57–64. [PubMed] [Google Scholar]
- 21.Shembesh NM, el Bargathy SM, Rao BN, Kashbur IM. A prospective study of bacterial meningitis in children from North-Eastern Libya. Ann Trop Paediatr. 1998;18:203–7. doi: 10.1080/02724936.1998.11747948. [DOI] [PubMed] [Google Scholar]
- 22.Townsend SM, Pollack HA, Gonzalez-Gomez I, Shimada H, Badger JL. Citrobacter koseri brain abscess in the neonatal rat: survival and replication within human and rat macrophages. Infect Immun. 2003;71:5871–80. doi: 10.1128/IAI.71.10.5871-5880.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffman O, Weber RJ. Pathophysiology and treatment of bacterial meningitis. Ther Adv Neurol Disord. 2009;2:1–7. doi: 10.1177/1756285609337975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fatima K, Meher R, Nazish F, Indu S, Abida M, Razia K. Bacterial meningitis in North India: Trends over a period of eight years. Neurol Asia. 2011;16:47–56. [Google Scholar]


