Abstract
Objective:
Development of dental caries, specifically, white spot lesions (WSLs), continues to be a well-recognized and troubling side effect of orthodontic fixed appliance therapy, despite vast improvement in preventive dental techniques and procedures. The aim of this meta-analysis is to evaluate, determine, and summarize the incidence and prevalence rates of WSLs during orthodontic treatment that have been published in the literature.
Materials and Methods:
According to predetermined criteria, databases were searched for appropriate studies. References of the selected articles and relevant reviews were searched for any missed publications.
Results:
In the 14 studies evaluated for WSLs, the incidence of new carious lesions formed during orthodontic treatment in patients was 45.8% and the prevalence of lesions in patients undergoing orthodontic treatment was 68.4%.
Conclusion:
The incidence and prevalence rates of WSLs in patients undergoing orthodontic treatment are quite high and significant. This widespread problem of WSL development is an alarming challenge and warrants significant attention from both patients and providers, which should result in greatly increased emphasis on effective caries prevention.
Keywords: Demineralization, incidence, orthodontic fixed appliances, prevalence, white spot lesions
INTRODUCTION
White spot lesions (WSLs) are defined as “subsurface enamel porosity from carious demineralization” that presents as “a milky white opacity” when located on smooth surfaces. These are areas of local decalcification of enamel without cavity formation.
Early carious lesions in the enamel are observed clinically as a white opaque spot. The area is slightly softer than the surrounding sound enamel. Two initial stages of enamel demineralization have been observed:
Surface softening- This is characterized by preferential removal of the interprismatic substance, the mineral loss being most pronounced at the enamel surface
Subsurface lesion- The dissolution occurs mainly in the deeper part of the enamel. A porous, but still mineral-rich layer covers the body of the lesion, which is low in mineral. WSL is considered to be the precursor of frank enamel caries.
In orthodontics, it can be attributed to the difficulties in performing oral hygiene procedures on bonded dental arches and the prolonged plaque accumulation on tooth surfaces, which lead to a decrease in pH that tips the demineralization–remineralization balance toward mineral loss (demineralization), which in turn can lead to WSL development and eventually to cavitation and caries extending into the dentin.
The most common negative side effect of orthodontic treatment with fixed appliances is the development of incipient carious lesions around brackets and bands.[1] The irregular surfaces of brackets, bands, wires, and other attachments limit naturally occurring self-cleaning mechanisms, such as movement of the oral musculature and saliva. Since orthodontic appliances make plaque removal more difficult, patients are more susceptible to carious lesions.[2] Certain bacterial groups such as mutans streptococci and lactobacilli, which are present in the plaque, ferment sugars to create an acidic environment which, over time, leads to the development of dental caries.[3]
WSLs are clinical manifestations of early enamel caries. These lesions are characterized by their opacity, mineral loss, and decrease of fluorescence radiance, when compared to healthy enamel surfaces. Many incipient enamel lesions have a white appearance due to an optical phenomenon caused by mineral loss in the surface and sub-surface that alters the refractive index and increases the scattering of light in the affected area, all resulting in greater visual enamel opacity.[1] This is a clinical problem resulting in an unacceptable esthetic presentation that, in some severe cases, may require restorative treatment.[4]
WSLs can become noticeable around the brackets of fixed appliances within 1 month of bracket placement, although the formation of regular caries usually takes at least 6 months.[5,6] These lesions are commonly seen on the buccal surfaces of the teeth, around the brackets, especially in the gingival area.[1,5]
The purpose of this study is to accumulate, summarize, and critically evaluate, in evidence-based manner, the current knowledge from published studies regarding the incidence and prevalence of WSLs and to identify the risk of orthodontic patients developing these lesions.
MATERIALS AND METHODS
A search for relevant clinical studies published in English up to March 2015 was conducted on Medline/PubMed and the Cochrane Library with “orthodontics,” “fixed appliances,” “caries,” “white spot lesions,” “demineralization,” and “decalcification” as the principal search terms. Only human controlled in vivo studies with WSL incidence and prevalence were accepted.
Systematic searches were conducted for published studies. The reference list was manually reviewed. The studies relevant to the analysis were identified and their reference lists were also scanned for additional relevant studies. Studies selected were clinical trials, cohort and cross-sectional studies.
Double publications/duplicates and case reports were discarded. The initial searches revealed 161 papers, but after independent reading of the abstracts by two examiners, 5 abstracts and 38 papers were retrieved in full length and 14 were accepted for this report.
Inclusion criteria
Patients who had undergone fixed orthodontic treatment
Only incidence and prevalence of WSL in patients were evaluated not considering the number of teeth or the teeth surfaces involved
Minimum duration of treatment should be 12 months
No fluoride supplements used during the treatment for control group.
Figure 1.
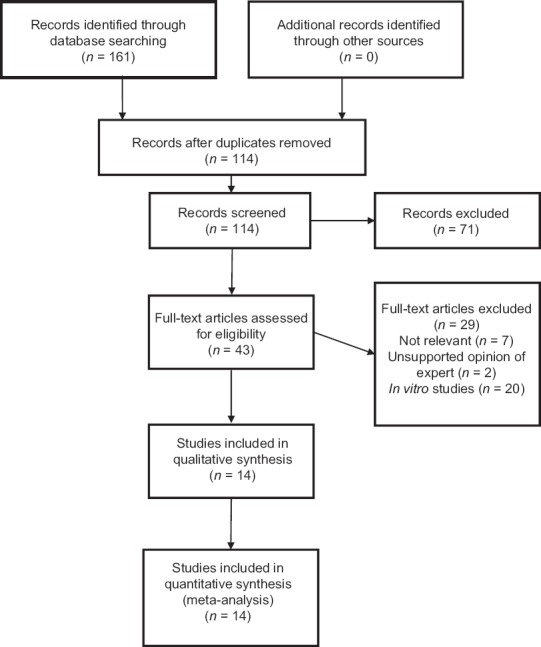
Flowchart of the selection of studies
Data management
Two authors (A. T. and A. P.) independently extracted the rate of incidence and prevalence from the included studies using predefined data extraction forms. Any disagreements were resolved by discussion with the third author (V. S.). The Cohen kappa statistic was used to assess the agreement between the two review authors.
Assessment of publication bias
Publication bias was initially evaluated through visual inspection of funnel plot asymmetry.[7] In addition, publication bias was tested statistically by using the test of Begg and Mazumdar (rank correlation method).[8]
RESULTS
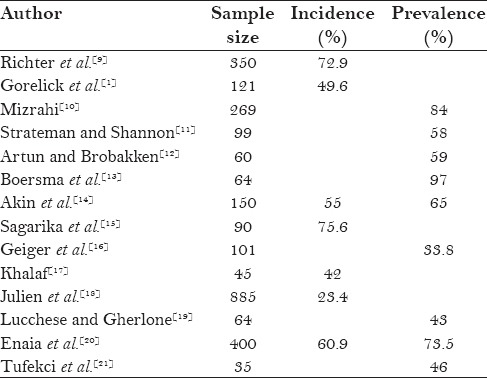
In the 14 studies included in the analysis, a total of 935 patients out of 2041 patients developed new WSLs, which accounted for 45.8% of patients developing new WSL during treatment. A total of 1242 patients were studied for prevalence, of which 850 patients had WSL, suggesting that 68.4% of the patients undergoing orthodontic treatment had WSLs. Table 1 shows the studies and the incidence or prevalence rates for the respective studies.
Table 1.
WSL Incidence and Prevalence rates
DISCUSSION
The study included data regarding the incidence and prevalence of WSLs from 14 studies. In this analysis, 935 patients out of 2041 developed new WSLs during the orthodontic treatment, which accounts to 45.8% of the patients. Eight hundred and fifty patients out of 1242 had WSLs at the time of evaluation, which means 68.4% of patients undergoing orthodontic treatment had WSLs.
Many factors were observed to influence the development of WSLs, which are as follows.
Gender
Khalaf reported that with regards to differences between genders, it was found that males had significantly greater incidence (almost 3 times) of WSLs than females.[17] Boersma et al. found that 40% of the buccal surfaces in males had demineralization, compared with 22% in females.[13] Julien et al. found the percentage of male patients who developed WSLs during treatment to be higher (25%) than the percentage of female patients (22%).[18] Tufekci et al. stated that of the subjects who had at least one WSL, 76% were male.[21] Lucchese and Gherlone found that 55% of patients who had at least one visible WSL were male and 44% were female.[19] Enaia et al. found that male patients tend to develop more severe WSL than female patients.[20]
Sagarika et al. ruled out the role of gender biasing in the process of enamel demineralization.[15] Akin et al. found that gender was not a significant factor in WSL development.[14] Mizrahi reported that following orthodontic treatment, there was still no difference between the sexes with regard to prevalence; however, there was a difference in severity of the opacities. The male patients did experience an increase in the severity of opacities following orthodontic treatment.[10]
These findings differ from those of Gorelick et al., who found the incidence to be 44% for boys and 54% for girls.[1]
This gender difference may be due to the commonly reported better oral hygiene standards in females than in males.[22,23,24]
Age
Khalaf reported that adolescent patients in his study were found to be twice more likely to develop WSLs as adult patients.[17] According to Akin et al., age at the start of treatment and patient's oral hygiene were significant factors in WSL development.[14] Richter et al. also reported that the age at the start of treatment and the patient's oral hygiene were significant factors in WSL development.[9]
Sagarika et al. indicated that the age of the patient does not play a role in the prevalence of WSLs.[15]
Richter et al. found that as age increased, WSL development tended to decrease by 0.59 lesions per age group.[9]
This can be attributed to better oral hygiene maintenance by adult patients than adolescents, and is an important and relevant factor for orthodontists who decide at what age to initiate treatment.
Salivary flow
Gorelick et al., found that occurrence of WSLs on the lingual surface of incisors bonded with canine to canine retainer is nil. They attributed this to the free flow of saliva in that region. This may be a major factor in avoiding decalcification of enamel surface.[1]
Duration of treatment
Khalaf reported that treatment length did impact on the formation of WSLs, and it was found that as the treatment length increased from <24 months to >36 months, the likelihood of formation of WSLs did increase by 3.65 times.[17] Tufekci et al.[21] and Lucchese and Gherlone[19] showed that WSLs can be prevalent in patients undergoing orthodontic treatment for as early as 6 months (38% and 40%, respectively), which increases with longer treatment duration at 12 months (46% and 43%, respectively), supporting the idea that the presence of fixed orthodontic appliances and greater treatment lengths serve as a risk factor for WSL formation. Similar finding was also reported by Julien et al.[18]
According to Richter et al., a trend was detected which indicated that as treatment duration increased, development of WSL also increased.[9] Multiple regression analysis showed that for each month of treatment with full fixed appliances, the number of WSLs increased by an estimated factor of 0.08 lesions per month. Development of WSL continues at a steady rate. After 22 months of treatment, an average of 3.01 surfaces developed WSL; after 33 months, the risk increased to an average of 5.28 new WSLs.[9]
Akin et al. reported that treatment length was not a significant factor in WSL development.[14] Gorelick et al. were unable to find an impact of the treatment length on the prevalence of WSLs.[1]
This might have been because the longer the fixed appliances were in place, the longer the teeth were exposed to cariogenic challenges of increased plaque accumulation.
Use of fluoride during treatment
Khalaf reported that regular use of fluoride mouthwash during the orthodontic treatment did significantly reduce the risk of developing WSLs.[17] Strateman and Shannon reached the same conclusion in their study in which the first group of patients used fluoride gel regularly and the second group used no fluoride. The authors found corresponding incidence rates of WSLs as 27% and 59%, respectively.[11]
Geiger et al. found a 30% reduction in the prevalence and a 25% reduction in the incidence rate of WSLs when orthodontic patients used a fluoride mouth rinse.[16]
Sagarika et al. found that although 0.05% acidulated phosphofluoride mouth rinses were prescribed for the examined test group subjects, it was surprising to observe the high rate of WSL prevalence in the study.[15]
Although use of fluoride applications during orthodontic treatment seems to reduce the incidence of WSLs, it is highly dependent on patient's compliance for the use of these applications.
Teeth involved
Khalaf found that the maxillary anterior teeth were more affected than the mandibular anterior teeth.[17] It was found that the maxillary canines were the most affected teeth, followed by the maxillary lateral incisors. Posterior teeth (the first molars and premolars) were the most affected teeth in the mandibular arch.[17]
Gorelick et al. reported that the maxillary lateral incisors were affected more commonly.[1] Geiger et al. reported that the maxillary lateral incisor and canines were the most common teeth affected.[11] Sagarika et al. found more WSLs seen on maxillary incisors, followed by canines and then the maxillary and mandibular premolars.[15] Julien et al. reported that WSLs were 2.5 times more frequent in the maxillary than in the mandibular arch and that they occurred most frequently on the maxillary laterals, maxillary canines, and mandibular canines.[18]
Lucchese and Gherlone found a high prevalence of WSLs on mandibular first molars and second premolars, followed in decreasing order by first premolars, canines, lateral incisors, and central incisors.[19] In the treated group, a high prevalence of WSLs was observed in the maxilla on the lateral incisors and canines, followed by central incisors, second premolars, and first molars.[19] According to Enaia et al., the maxillary lateral incisors showed higher WSL prevalence or incidence than did the maxillary central incisors.[20] Gorelick et al., found that maxillary incisors and mandibular molars had the highest incidence of WSLs.[1]
Tufekci et al., found no differences in the teeth involved, which could have been due to the fact that the subjects in that sample were examined during treatment and the appliances on their teeth made it more difficult to accurately identify WSLs.[20]
Mizrahi concluded that the maxillary and mandibular first molars were the teeth most commonly affected.[10]
Artun and Brobakken found mandibular canines and premolars to be the most affected teeth instead.[12]
The highest incidence of lesions in maxillary lateral incisors can be attributed to small tooth surface areas between the gingiva and bracket, which is conductive for the retention of plaque and debris leading to increased decalcification in the region.
The distribution pattern of WSLs observed in the maxillary and mandibular teeth may be explained by the different amounts of exposure of saliva to the maxillary anterior teeth in contrast to other areas of the dentition, or simply by poor toothbrushing techniques resulting in the ineffective cleaning of certain teeth.
Surfaces involved
Khalaf reported that WSLs were found in all areas of the maxillary teeth, but almost all WSLs were exclusively recorded on the gingival margins of the mandibular teeth.[17] However, the gingival margin was the most frequently recorded surface location of WSLs on both the maxillary and mandibular teeth.[17] Artun and Brobakken's study has also reported that WSLs commonly affect the gingival areas.[12]
Variables such as geographic and socioeconomic status and private practice versus university settings also might contribute to the differences in the incidences of WSL.
Overall management of WSLs involves methods of both preventing demineralization and encouraging remineralization of existing lesions. Preventive measures are more important due to the challenges of treating patients who develop many WSLs. Successful preventive strategies include patient education, oral health promotion, regular professional oral hygiene visits, and appropriate patient compliance. For efficient caries control in orthodontic patients, the combined use of fluoride and chemical plaque control has been recommended. Caries lesions adjacent to brackets can be reduced or even completely inhibited when a fluoride dentifrice is used with a mouth rinse.[4,5] O’Reilly and Featherstone evaluated the effect of fluoride mouth rinse on demineralization adjacent to orthodontic appliances and showed its effect on inhibiting demineralization.[6] Geiger et al., reported the same result after a longitudinal evaluation of orthodontic patients using fluoride mouth rinse.[16] However, the use of a mouth rinse completely depends on patient compliance, which is frequently low.
For noncompliant patients, appropriate preventive medicaments, such as topical fluorides, can aid in reducing the demineralization of enamel surrounding the orthodontic brackets. Various forms of topical fluoride (toothpaste, mouth rinse, gels, varnishes, fluoride-releasing cements, and fluoride-releasing elastomeric auxiliaries) are the most commonly used caries-preventive protocol during orthodontic treatment for at-risk patients, in addition to patient education and regular hygiene visits. Although fluoride varnish does not totally prevent the formation of WSLs, their incidence can be significantly reduced. In a prospective clinical study, there was a decrease in caries lesions by 44.3% for teeth that had been treated with fluoride varnish during orthodontic treatment.[25] Ogaard et al., evaluated enamel lesion formation with and without fluoride varnish and found a 48% reduction in the depth of lesions with varnish use.[26]
Fluoride-releasing bonding agents were developed to allow for compliance-free, constant exposure to topical fluoride. Studies have shown that fluorapatite formation from either a monthly high dose of topical fluoride application or continually available low doses of fluoride (e.g., from fluoride-containing orthodontic adhesive cements) can be advantageous in reducing enamel decalcification during fixed appliance therapy.[27]
One of the newest modalities in preventive dentistry is the introduction of amorphous calcium phosphate (ACP) into methacrylate composites, gum, pastes, and other dental products. Casein phosphopeptide-ACP (CPP-ACP) has been reported to have topical anticariogenic effects because of its ability to stabilize calcium and phosphate in an amorphous state. CPP-ACP incorporated into dental plaque can significantly increase the levels of plaque calcium and phosphate ions. This mechanism is ideal for the prevention of enamel demineralization because there appears to be an inverse association between plaque calcium and phosphate levels and measured caries experience. The localized CPP-ACP subsequently acts to buffer free calcium and phosphate ions in the plaque fluid, to maintain a state of supersaturation of ACP with respect to enamel mineral, thereby limiting enamel demineralization and enhancing remineralization.[28]
Once the orthodontic treatment is completed and the appliance removed, no further progression of lesions will occur since the cariogenic challenge has ceased.[28] In some cases, WSLs seem to decrease in the first year after debonding.[29] Owing to the results of the classical study by Backer Dirks, it might be assumed that remineralization processes are responsible for the disappearance of the WSLs.[30] However, their disappearance might also be ascribed to attrition by functional wear and toothbrushing. It might be assumed that they diminish as they are brushed away over the years. In this regard, Artun and Thylstrup reported that “primarily the result of surface abrasion with some redeposition of minerals is to be held responsible for the loss of porous tissue and the gradual regression of the WSLs after debonding.”[31] However, the clinical management of visible white spots developed during orthodontic therapy on the facial surfaces is still obscure.
In recent years, the field of orthodontics has seen many recent advances. An intricate issue facing clinical orthodontics that still remains unsolved is the high incidence of post-treatment WSLs. Orthodontic practices and training programs should pay more attention on this preventable condition that affects most orthodontic patients. Despite the high incidence of these lesions associated with orthodontic treatment, fortunately, few of these lesions progress so fast that upon removal of appliance, a restoration is needed. Exposure to healthy saliva results in physiologic rebalance and natural remineralization.
CONCLUSION
Results of this meta-analysis demonstrated that WSL occurrence is common during fixed orthodontic treatment with an incidence and prevalence rate of 45.8% and 68.4%, respectively, indicating the need for special precautionary steps to be taken to prevent the development of WSLs. The widespread problem of WSL development is an alarming challenge and warrants significant attention from both patients and providers, which should result in greatly increased emphasis on effective caries prevention.
Certain factors were found to increase the incidence of WSLs, such as poor oral hygiene, lesser age of the patient at the start of treatment, male patients, and duration of the treatment. Factors like salivary flow and preventive fluoride therapy throughout the treatment duration caused reduction in the incidence of WSLs.
Orthodontists should be aware of the high risk of WSL and decide at the patient level whether it is appropriate to start or continue treatment in patients who are already experiencing enamel demineralization. The risk of developing incipient caries lesions during orthodontic treatment should not be underestimated by orthodontists. High prevalence of WSL in patients undergoing orthodontic treatment indicates the need to evaluate further methods to counter the risk of development of these lesions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–8. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 2.Rosenbloom RG, Tinanoff N. Salivary Streptococcus mutans levels in patients before, during, and after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991;100:35–7. doi: 10.1016/0889-5406(91)70046-Y. [DOI] [PubMed] [Google Scholar]
- 3.Lundström F, Krasse B. Streptococcus mutans and lactobacilli frequency in orthodontic patients: The effect of chlorhexidine treatments. Eur J Orthod. 1987;9:109–16. doi: 10.1093/ejo/9.2.109. [DOI] [PubMed] [Google Scholar]
- 4.Ogaard B. Prevalence of white spot lesions in 19-year-olds: A study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthod. 1989;96:423–7. doi: 10.1016/0889-5406(89)90327-2. [DOI] [PubMed] [Google Scholar]
- 5.Ogaard B, Rølla G, Arends J. Orthodontic appliances and enamel demineralization. Part 1. Lesion development. Am J Orthod Dentofacial Orthop. 1988;94:68–73. doi: 10.1016/0889-5406(88)90453-2. [DOI] [PubMed] [Google Scholar]
- 6.O’Reilly MM, Featherstone JD. Demineralization and remineralization around orthodontic appliances: An in vivo study. Am J Orthod Dentofacial Orthop. 1987;92:33–40. doi: 10.1016/0889-5406(87)90293-9. [DOI] [PubMed] [Google Scholar]
- 7.Light RJ, Pillemer DB. Cambridge, Mass: Harvard University Press; 1984. Summing Up: The Science of Reviewing Research. [Google Scholar]
- 8.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101. [PubMed] [Google Scholar]
- 9.Richter AE, Arruda AO, Peters MC, Sohn W. Incidence of caries lesions among patients treated with comprehensive orthodontics. Am J Orthod Dentofacial Orthop. 2011;139:657–64. doi: 10.1016/j.ajodo.2009.06.037. [DOI] [PubMed] [Google Scholar]
- 10.Mizrahi E. Enamel demineralization following orthodontic treatment. Am J Orthod. 1982;82:62–7. doi: 10.1016/0002-9416(82)90548-6. [DOI] [PubMed] [Google Scholar]
- 11.Stratemann MW, Shannon IL. Control of decalcification on orthodontic patients by daily self-administered application of a water free 0.4% stannous fluoride gel. Am J Orthod. 1974;66:273–9. doi: 10.1016/0002-9416(74)90291-7. [DOI] [PubMed] [Google Scholar]
- 12.Artun J, Brobakken BO. Prevalence of carious white spots after orthodontic treatment with multibonded appliances. Eur J Orthod. 1986;8:229–34. doi: 10.1093/ejo/8.4.229. [DOI] [PubMed] [Google Scholar]
- 13.Boersma JG, van der Veen MH, Lagerweij MD, Bokhout B, Prahl-Andersen B. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: Influencing factors. Caries Res. 2005;39:41–7. doi: 10.1159/000081655. [DOI] [PubMed] [Google Scholar]
- 14.Akin M, Tazcan M, Ileri Z, Basciftci FA. Incidence of white spot lesion during fixed orthodontic treatment. Turkish J Orthod. 2013;26:98–102. [Google Scholar]
- 15.Sagarika N, Suchindran S, Loganathan S, Gopikrishna V. Prevalence of white spot lesion in a section of Indian population undergoing fixed orthodontic treatment: An in vivo assessment using the visual International Caries Detection and Assessment System II criteria. J Conserv Dent. 2012;15:104–8. doi: 10.4103/0972-0707.94572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geiger AM, Gorelick L, Gwinnett AJ, Griswold PG. The effect of a fluoride program on white spot formation during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1988;93:29–37. doi: 10.1016/0889-5406(88)90190-4. [DOI] [PubMed] [Google Scholar]
- 17.Khalaf K. Factors affecting the formation, severity and location of white spot lesions during orthodontic treatment with fixed appliances. J Oral Maxillofac Res. 2014;5:e4. doi: 10.5037/jomr.2014.5104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Julien KC, Buschang PH, Campbell PM. Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod. 2013;83:641–7. doi: 10.2319/071712-584.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lucchese A, Gherlone E. Prevalence of white-spot lesions before and during orthodontic treatment with fixed appliances. Eur J Orthod. 2013;35:664–8. doi: 10.1093/ejo/cjs070. [DOI] [PubMed] [Google Scholar]
- 20.Enaia M, Bock N, Ruf S. White-spot lesions during multibracket appliance treatment: A challenge for clinical excellence. Am J Orthod Dentofacial Orthop. 2011;140:e17–24. doi: 10.1016/j.ajodo.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 21.Tufekci E, Dixon JS, Gunsolley JC, Lindauer SJ. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81:206–10. doi: 10.2319/051710-262.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alcouffe F. Oral hygiene behavior: Differences between men and women. Clin Prev Dent. 1989;11:6–10. [PubMed] [Google Scholar]
- 23.Ostberg AL, Halling A, Lindblad U. Gender differences in knowledge, attitude, behavior and perceived oral health among adolescents. Acta Odontol Scand. 1999;57:231–6. doi: 10.1080/000163599428832. [DOI] [PubMed] [Google Scholar]
- 24.Sakki TK, Knuuttila ML, Anttila SS. Lifestyle, gender and occupational status as determinants of dental health behavior. J Clin Periodontol. 1998;25:566–70. doi: 10.1111/j.1600-051x.1998.tb02489.x. [DOI] [PubMed] [Google Scholar]
- 25.Vivaldi-Rodrigues G, Demito CF, Bowman SJ, Ramos AL. The effectiveness of a fluoride varnish in preventing the development of white spot lesions. World J Orthod. 2006;7:138–44. [PubMed] [Google Scholar]
- 26.Ogaard B, Duschner H, Ruben J, Arends J. Microradiography and confocal laser scanning microscopy applied to enamel lesions formed in vivo with and without fluoride varnish treatment. Eur J Oral Sci. 1996;104:378–83. doi: 10.1111/j.1600-0722.1996.tb00095.x. [DOI] [PubMed] [Google Scholar]
- 27.McNeill CJ, Wiltshire WA, Dawes C, Lavelle CL. Fluoride release from new light-cured orthodontic bonding agents. Am J Orthod Dentofacial Orthop. 2001;120:392–7. doi: 10.1067/mod.2001.118103. [DOI] [PubMed] [Google Scholar]
- 28.Reynolds EC. Remineralization of enamel subsurface lesions by casein phosphopeptide-stabilized calcium phosphate solutions. J Dent Res. 1997;76:1587–95. doi: 10.1177/00220345970760091101. [DOI] [PubMed] [Google Scholar]
- 29.Al-Khateeb S, Forsberg CM, de Josselin de Jong E, Angmar-Månsson B. A longitudinal laser fluorescence study of white spot lesions in orthodontic patients. Am J Orthod Dentofacial Orthop. 1998;113:595–602. doi: 10.1016/s0889-5406(98)70218-5. [DOI] [PubMed] [Google Scholar]
- 30.Backer Dirks O. The clinical testing of agents for the prevention of dental caries. Adv Fluorine Res. 1966;4:1–2. [PubMed] [Google Scholar]
- 31.Artun J, Thylstrup A. Clinical and scanning electron microscopic study of surface changes of incipient caries lesions after debonding. Scand J Dent Res. 1986;94:193–201. doi: 10.1111/j.1600-0722.1986.tb01753.x. [DOI] [PubMed] [Google Scholar]


