Abstract
Background:
To compare 4% articaine and 2% lidocaine local anesthetics in achieving pulpal anesthesia of the lower first permanent molar teeth objectively, and to assess and compare lip and lingual mucosa numbness subjectively.
Materials and Methods:
All subjects received 1.7 ml of any one anesthetic in the mucobuccal fold adjacent to mandibular first molar teeth; the same individuals received the second infiltration at least 1 week after the first. Later, comparisons for pulpal anesthesia, lip and lingual mucosa numbness between these two anesthetics solutions were made.
Results:
Articaine showed significant results with P = 0.006 in achieving pulpal anesthesia objectively, when compared with lidocaine. Articaine also showed very high significant results subjectively with P = 0.0006 in achieving lip numbness, when compared with lidocaine. But the results in achieving lingual mucosa numbness with articaine subjectively was not significant with P = 0.01, when compared with lidocaine.
Conclusion:
Endodontic and operative treatments are one of the most common oral non-surgical procedures done under local anesthesia. The diversity of anesthetic substances currently available on the market requires dental professionals to assess the drug both by its pharmacokinetic and also by its clinical characteristics during dental treatments. Our study used 4% articaine, which is available in the market, for comparison with 2% lidocaine. Further studies are required to use an equal concentration of solutions to achieve more accurate results.
Keywords: Articaine, lidocaine, local anesthetics, pulpal anesthesia
INTRODUCTION
Analgesic therapies for managing painful conditions currently rely on three major classes of drugs: Non-steroidal anti-inflammatory drugs (NSAIDs), opioids, and adjuvants (antidepressants, anticonvulsants, local anesthetics, 2-adrenoceptor agonists).[1] Safe and effective pain control is essential for today's dental practice and local anesthesia plays a fundamental role by reducing the fear, anxiety, and treatment time associated with dental procedures.
Local anesthesia forms the backbone of pain control techniques in dentistry. From cocaine (1884), procaine (1904), to lidocaine (1948), dentistry has been in forefront in seeking to provide patients with pain-free treatment. The primary local anesthetics used in dentistry are classified as amides and esters. Amides are more often used than ester agents since amides produce more rapid and reliable profound surgical anesthesia. New amino ester local anesthetics were synthesized between 1891 and 1930, such as tropocaine, holocaine, benzocaine, and tetracaine. In addition, amino amide local anesthetics were prepared between 1898 and 1972, including procaine, chloroprocaine, cinchocaine, lidocaine, mepivacaine, prilocaine, bupivacaine, etidocaine, and articaine. Still research is continuing to seek safer and more effective local anesthetics.[2,3,4]
Lidocaine was prepared by Nils Lofgren in 1943 and was introduced into market in 1948, and it has become the most common local anesthetic to be used. Because of safety and effectiveness, lidocaine also has become the gold standard for comparison among the newer local anesthetic agents. Lidocaine is an amide with intermediate duration of action.[3]
Carticaine, first prepared by Rusching and colleagues in 1969, had its generic name changed to articaine when it entered clinical practice in Germany in 1976. Its use gradually spread, entering North America in 1983 and the United Kingdom in 1998. As with lidocaine, articaine is also classified under amide group of local anesthetics with intermediate duration of action.[5] Literature reports that patients treated with articaine become “drug free” more quickly than those who receive other local anesthetics.[4]
The advantages of articaine are as follows: Articaine causes a transient and completely reversible state of anesthesia (loss of sensation) during dental procedures; in dentistry, articaine is used both for infiltration and block injections, and with the block technique, it yields the greatest duration of anesthesia; also, in people with hypokalemic sensory overstimulation, lidocaine is not very effective, but articaine works well.[6,7]
Endodontic and operative treatments are among the most common oral non-surgical procedures done under local anesthesia. Various local anesthetic agents like lidocaine, bupivacaine, and prilocaine have been used for the purpose. Articaine has been reported to provide a better local anesthetic effect.[8] It was approved for use in the United States in April 2000 and is marketed as Septocaine (Septodont, New Castle, DE, USA) and as a 4% solution with 1:100,000 epinephrine. Articaine is produced as a 4% local anesthetic solution, similar to prilocaine. This is in contrast to lidocaine, which is a 2% solution. Equal analgesic efficacy along with lower systemic toxicity (i.e., a wide therapeutic range) allows use of articaine in higher concentrations than other amide-type local anesthetics.[9]
Successful pulpal anesthesia is not always achieved in mandibular teeth following regional block anesthesia.[10,11] Labial or lingual infiltration injections with lidocaine are not effective for achieving pulpal anesthesia in mandibular teeth.[12] Adding a labial infiltration of 1.8 ml of 2% lidocaine with 1:100,000 epinephrine to a conventional inferior alveolar nerve block injection increases the success of pulpal anesthesia in mandibular anterior teeth, but not in mandibular molar.[13] On the contrary, an infiltration injection of the mandibular second molar with 4% articaine with 1:200,000 epinephrine successfully achieved pulpal anesthesia in 63% of cases.[12] Perhaps infiltration injection of an articaine solution adjacent to the first molar would be more successful and should be studied experimentally.
A study was conducted to compare 2% lidocaine and 4% articaine in achieving pulpal anesthesia in mandibular molars and it reported statistically significant difference between these solutions in achieving pulpal anesthesia in mandibular molars by buccal infiltration.[14] Similar studies reported a success rate of 75–92% with articaine and 45–67% with lidocaine by single buccal infiltration in permanent mandibular molars.[15]
Articaine is contraindicated in patients allergic to amide-type anesthetics and patients allergic to metabisulfites (preservative present in the formula to extend the life of epinephrine), as there is no cross-allergenicity between sulfites (preservatives), sulfur, and the “sulfa”-type antibiotics. It is contraindicated in patients with hemoglobinopathies (sickle cell disease) and also in patients with idiopathic or congenital methemoglobinemia, but methemoglobinemia is not a concern in the dental practice due to the small volumes of articaine used. Articaine is not contraindicated in patients with sulfa allergies; there is no cross-allergenicity between articaine's sulfur-bearing thiophene ring and sulfonamides.
However, the aim and objective of our study was to compare 4% articaine and 2% lidocaine in achieving pulpal anesthesia of the lower first permanent molar teeth objectively and also to assess and compare lip numbness and lingual mucosa numbness in volunteers subjectively after single buccal infiltration of local anesthesia.
MATERIALS AND METHODS
Study was designed as a prospective randomized double-blind crossover trial, comparing lidocaine 2% (1:100,000 epinephrine) with articaine 4% (1:100,000 epinephrine) [Tables 1 and 2].
Table 1.
Materials used in the study
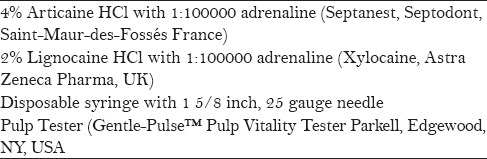
Table 2.
Pharmacology of local anesthetics used
A power calculation indicated that 31 subjects would provide a 90% chance of detecting an effect size of 0.83 (a change of 0.83 standard deviations) in a continuous outcome measure, assuming a significance level of 5% and a correlation of 0.5 between the responses of same subject. Ethical approval for the study and informed written consent from the subjects were obtained.
Subjects with known or suspected allergies, sensitivities to sulfites and amide-type local anesthetics or to any ingredient in the anesthetic solution, concomitant cardiac disease, neurological disease, pregnant women or lactating mothers, subjects with concomitant use of monoamine oxidase inhibitors, tricyclic antidepressants, phenothiazine, vasodepressor drugs, or ergot-type oxytocic drugs, subjects who were on sedatives, who had taken aspirin, acetaminophen, NSAIDs 24 h prior to administration of local anesthetic, or the teeth tested as non-vital were not included in the study.
Thirty-two healthy subjects with age ranging from 15 to 35 years and having initial occlusal caries confirmed by intraoral periapical radiograph were selected as a group. They were treated as Group I to receive 2% lidocaine with 1:100,000 epinephrine (Xylocaine; Astra Zeneca Pharma, UK) in the first visit and the same individuals were treated as Group II to receive 4% articaine with 1:100,000 epinephrine (Septanest; Septodont, Saint-Maur-des-Fossés, France) local anesthesia in the second visit. The subjects were treated by the same operator and dental nurse at two different visits.
The selected subjects received 1.7 ml of any one anesthetic in the mucobuccal fold adjacent to the mandibular first molar in the first visit, and the same individuals received the second infiltration at the same area using a standard dental aspirating syringe at least 1 week after the first visit. The technique was standardized according to Malamed et al.[6] and anesthesia was administered at the rate of 0.9 ml/15 s and was injected over a period of 30 s. Both the subjects, and the dentist and dental nurse were blinded for the drug being used and had no involvement with testing the outcome.
Pulp sensitivity was determined by the dental nurse using an electric pulp tester (Gentle Pulse; Parkell, Edgewood, NY, USA) on the occlusal surface of the mandibular first molar twice before the injection, in order to establish a baseline reading. The same area of the tooth was tested each time and the mean of these two readings was taken as the baseline data. Pulp testing was then repeated once in every 2 min after injection for 30 min. To confirm the validity of reading, a control, unanesthetized tooth on the contralateral side was tested at the same time.
The change in pulp tester readings at the first sensation from the baseline was measured at each time point. Similarly, the numbers of episodes of no response at the maximum stimulation were recorded. In addition to objective assessment of pulpal anesthesia, volunteers were asked to inform the investigator about the feeling of numbness in the lip and lingual mucosa when it appeared.
Statistical analysis
Statistical analysis was performed using Student's t-test. P < 0.05 was considered statistically significant.
RESULTS
The study sample consisted of 32 patients, which was decided according to power calculation. The sample consisted of 7 males (21.9%) and 25 females (78.1%), with the mean age 18.2 years. No adverse events were recorded during any visit.
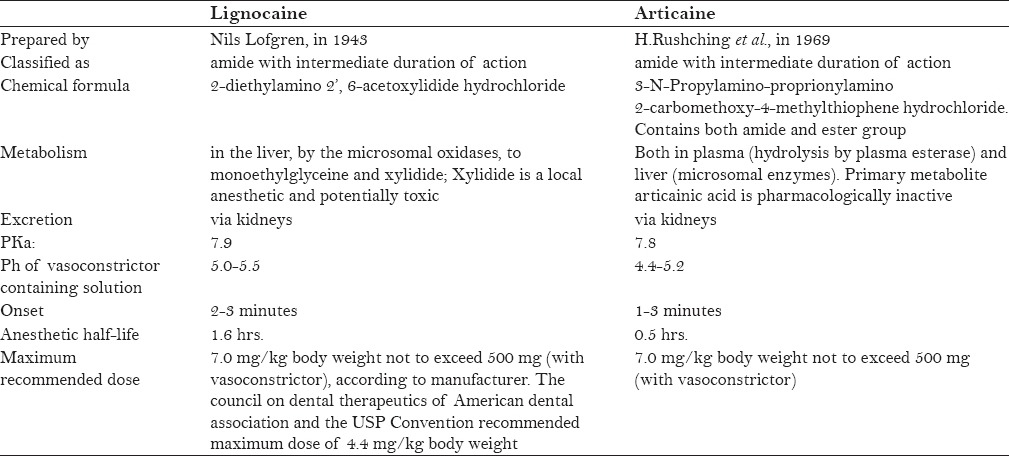
Twenty-eight patients, i.e. 87.5%, experienced anesthetic success (i.e., two or more consecutive episodes of no sensation at maximum stimulation) after 4% articaine injection with a mean time of onset 6.92 min, compared with 17 patients, i.e. 53.1%, after 2% lidocaine injection with a mean time of onset 10.35 min. This showed a high statistical significance with P = 0.006 [Table 3 and Figure 1].
Table 3.
Percentage of success, mean and SD of pulpal anaesthesia of 32 patients in both groups
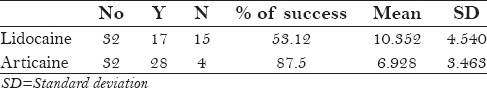
Figure 1.
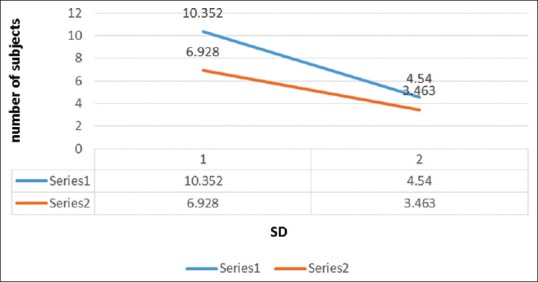
Mean and SD of pulpal anaesthesia
All patients experienced lip numbness after each local anesthetic injection. The onset of lip numbness ranged from 2 to 10 min after articaine with a mean of 3.56 min and SD of 1.66 min. In the lidocaine group, the onset of lip anesthesia ranged from 2 to 8 min with a mean of 4.9 min and SD of 1.36 min. This also showed a very high statistical significance with P = 0.0006 [Table 4 and Figure 2].
Table 4.
Percentage of success, mean and SD of lip numbness of 32 patients in both groups
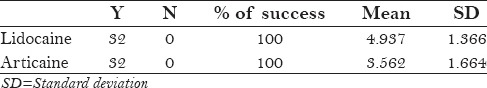
Figure 2.
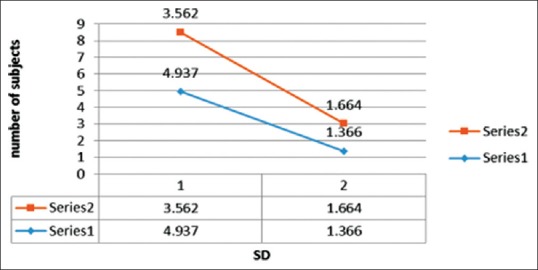
Mean and SD of lip numbness
Lingual mucosa numbness was reported by 15 patients after 2% lidocaine and by 24 patients after 4% articaine buccal infiltration. The mean onset of time was 10.53 min for 2% lidocaine and 9.29 min for 4% articaine. This difference was not significant with P = 0.1 [Tables 5 and 6 and Figure 3].
Table 5.
Percentage of success, mean and SD of lingual mucosa numbness of 32 patients in both groups
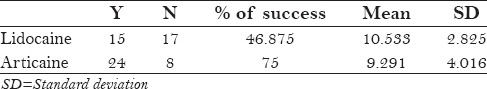
Table 6.
t value and P value of pulpal anaesthesia, lip numbness and lingual mucosa numbness in 32 patients
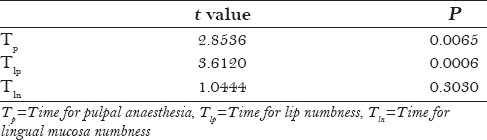
Figure 3.
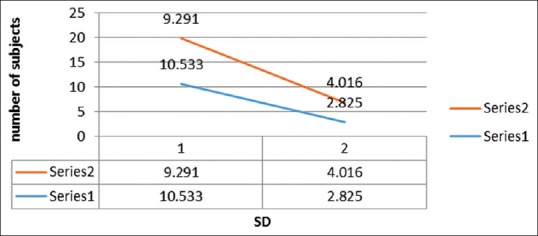
Mean and SD of lingual mucosa numbness
The number of times of no sensation on maximal stimulation in the first molars over the period of the trial was greater for 4% articaine (297) than for 2% lidocaine (157). Equality of proportions was statistically analyzed and was found to be significan [Figures 4 and 5].
Figure 4.
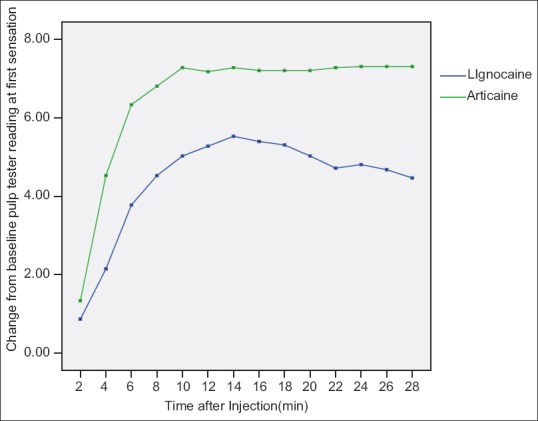
Changes from baseline pulp tester readings at first sensation at time intervals after injection
Figure 5.
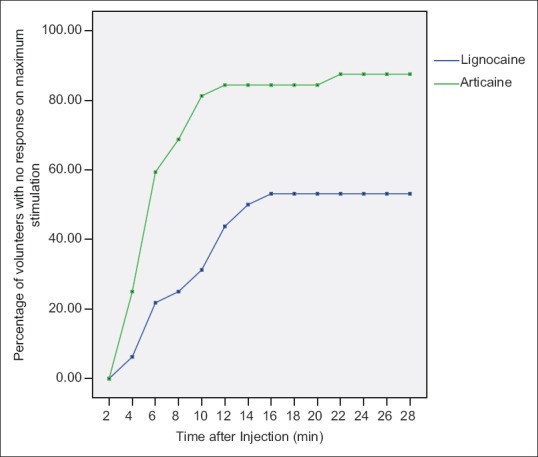
Percentage of patients with no response at maximum stimulation at each interval
The maximum duration of anesthesia possible in this study was 28 min. No patients experienced 28 min of continuous anesthesia in both the groups.
DISCUSSION
Using local anesthetics to control patients’ pain is one of the most important factors for successful treatment. The choice of anesthetic solution should be based on three main clinical considerations: Anesthetic potency, latency (time of onset of anesthesia), and duration of the anesthetic effect. Other important considerations are the pharmacokinetics (absorption, distribution, metabolization, and excretion) and toxicity of the drug.
Articaine, a new amide local anesthetic, was introduced in 1969, and has a reputation of providing an improved local anesthetic effect.[15] Articaine was approved for use in the United States in April 2000. The formulation is known as Septocaine (Septodont) and is available as a 4% solution with 1:100,000 epinephrine. Articaine is classified as an amide, but contains a thiophene ring instead of the benzene ring of other amide local anesthetics.[6] A second molecular difference between articaine and other amide local anesthetics is the extra ester linkage incorporated into the articaine molecule which results in hydrolysis of articaine by plasma esterases.[8]
The use of nerve blocks has several disadvantages when compared to infiltration. The rate of failures reported is approximately 15% and the incidence of adverse effects such as paresthesia, trismus, and hematoma is much greater. Moreover, treatment of only one tooth does not require anesthesia of the entire nerve branch.
Literature reports state that 90–95% of articaine is metabolized in the blood and only 5–10% is broken down in the liver.[9] The plasma half-life has been reported to be as low as 20 min.[16] Both articaine and lidocaine have the same maximum milligram dose of 500 mg (recommended dose of 6.6–7 mg/kg) for the adult patient.[6] Because articaine is marketed as a 4% solution, the maximum manufacturer's dose for a healthy 70 kg adult would be seven cartridges of an articaine solution, compared to 13 cartridges of a 2% lidocaine solution.[8]
In this study, we have compared the pulpal anesthesia of 2% lidocaine and 4% articaine in mandibular first molar buccal infiltration. Thirty-two patients with incipient caries on the mandibular first molar were selected. Injections of anesthetic solution were given on the same area at least 1 week apart. Electronic pulp testing was undertaken at baseline and at 2 min intervals until 30 min post injection. To test the onset and efficacy of pulpal anesthesia, we used an electric pulp tester to measure pain because researches have concluded that electric pulp tester can be a valuable tool in predicting potential anesthetic problems in operative dentistry.[17,18]
A successful outcome was recorded in the absence of pulp sensation on two consecutive maximal pulp tester stimulations; 87.5% of articaine and 53.13% of lidocaine infiltrations were successful. The mean time of onset of pulpal anesthesia was 6.92 min for 4% articaine and 10.35 min for 2% lidocaine. This difference was highly significant with P = 0.006.
Similar studies comparing articaine and lignocaine using buccal infiltration achieved a success rate of 45–57% with lidocaine formulation and 75–92% with articaine formulation. Some reported a success rate of 64.5% for articaine and 38.7% for lidocaine infiltration. Articaine infiltration produced significantly more episodes of no response to maximum stimulation in the first molars than lignocaine.[14,15]
A few studies have investigated the use of infiltration anesthesia in adult mandibular lower incisor following buccal and lingual infiltrations. They reported a success rate of 45% after labial injections of 2% lidocaine with 1:100,000 epinephrine and 50% after lingual infiltrations of the same solutions for lateral incisor pulpal anesthesia. For central incisors, the corresponding success rate were 63% and 47%.[19,20]
Some studies have reported no significant differences between articaine and lidocaine for different intraoral local anesthetic techniques, but some contradict the results.[2,8,14,15,16,18,21] Costa et al., in their study on 20 patients with maxillary posterior teeth infiltration, concluded that articaine produced shorter onset and longer duration of action when compared to lignocaine. Here, in our study, we did not measure the duration of anesthesia; we measured and compared the onset of both solutions. It was found that articaine produced shorter onset (6.92 min) when compared to lidocaine (10.35 min). This difference was highly significant (P = 0.006). To test the onset, duration, and efficacy of pulpal anesthesia, each of these authors used electric pulp tester for measuring pain.[22]
In the present study, we have compared the efficacy of 2% lidocaine and 4% articaine when administered as buccal infiltration in the mandible. We found that 4% articaine produced greater changes from the baseline pulp tester readings than 2% lidocaine, which is in agreement with the results of the studies conducted by Kanaa et al. and Robertson et al.[14,15] Although this difference is worth noting, the important result clinically is no response at maximum stimulation. We used two or more consecutive pulp tester readings at maximum stimulation without sensation as the criterion of success.[2,19,23] This criterion was used by many authors and we obtained greater success in achieving anesthesia in the mandibular permanent first molar probably because the maximum current output of our pulp tester was 47 μa, when compared to 80 μa which was the maximum output of the pulp tester used by Kanaa et al.
Some studies reported a success rate lesser than that reported in this study while using lidocaine.[12] This may be due to testing a different tooth number, i.e., mandibular second molar. The lack of success with lidocaine is because of its lower concentration; this needs to be investigated further.
Some authors have also made a comparative study on the anesthetic efficacy of 4% articaine versus 2% lidocaine, both with epinephrine 1:100,000, in the truncal block of the inferior alveolar nerve during the surgical extraction of impacted lower third molars. The results obtained suggest that 4% articaine offers better clinical performance than 2% lidocaine, particularly in terms of latency and duration of the anesthetic effect.[24] We did not measure duration in our study; therefore, future studies are required to measure duration.
All patients experienced lip numbness after each injection. This was in agreement with the study results of Kanaa et al. Subjective anesthesia of the lingual mucosa was reported in 15 patients of 2% lidocaine group and 24 patients of 4% articaine group. This suggests the limited ability of the anesthetic to diffuse through the entire thickness of mandible, which agrees with the findings of Haas et al.[12] It is worth mentioning that none of our results was influenced by the type or concentration of the vasoconstrictor substance associated with the local anesthetics employed, because both agents contained 1:100,000 epinephrine.
Our success with articaine in achieving pulpal anesthesia in the mandibular first molar was greater (87.5%) than the success rate reported by Kanaa et al. Kanaa et al., reported a success of 64.5% with artcaine and 38.7% with lidocaine. Our study was in agreement with Robertson et al. who reported a success rate of 75–92% with articaine and 45–67% with lidocaine. The higher success rate achieved with articaine in these studies may be due to its higher concentration (4%) when compared to 2% lidocaine.
CONCLUSION
The diversity of anesthetic substances currently available on the market requires dental professionals to assess the drug both by its pharmacokinetic and also by its clinical characteristics during dental treatments. Our study used 4% articaine, which is available in the market, for comparison with 2% lidocaine. Further studies are required to use an equal concentration of both solutions to obtain more accurate results.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare no conflicts of interest.
REFERENCES
- 1.Pozos AJ, Martinez R, Aguirre P, Perez J. The effects of tramadol added to articaine on anesthesia duration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:614–7. doi: 10.1016/j.tripleo.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 2.Berlin J, Nusstein J, Reader A, Beck M, Weaver J. Efficacy of articaine and lidocaine in a primary intraligamentary injection administered with a computer-controlled local anesthetic delivery system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:361–6. doi: 10.1016/j.tripleo.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Covino BG. Pharmacology of local anaesthetic agents. Br J Anaesth. 1986;58:701–16. doi: 10.1093/bja/58.7.701. [DOI] [PubMed] [Google Scholar]
- 4.Hawkins JM, Moore PA. Local anesthesia: Advances in agents and techniques. Dent Clin North Am. 2002;46:719–32. doi: 10.1016/s0011-8532(02)00020-4. [DOI] [PubMed] [Google Scholar]
- 5.Mehta Fali S, Daftary Dinesh K, Billimoria RB, Irani RR. Carticaine in dentistry. J Indian Dent Assoc. 1983;55:501–5. [PubMed] [Google Scholar]
- 6.Malamed SF, Gagnon S, Leblanc D. Efficacy of articaine: A new amide local anesthetic. J Am Dent Assoc. 2000;131:635–42. doi: 10.14219/jada.archive.2000.0237. [DOI] [PubMed] [Google Scholar]
- 7.Vree TB, Gielen MJ. Clinical pharmacology and the use of articaine for local and regional anaesthesia. Best Pract Res Clin Anaesthesiol. 2005;19:293–308. doi: 10.1016/j.bpa.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Malamed SF, Gagnon S, Leblanc D. Articaine hydrochloride: A study of the safety of a new amide local anesthetic. J Am Dent Assc. 2001;132:177–85. doi: 10.14219/jada.archive.2001.0152. [DOI] [PubMed] [Google Scholar]
- 9.Oertel R, Ebert U, Rahn R, Kirch W. The effect of age on pharmacokinetics of the local anesthetic drug articaine. Reg Anesth Pain Med. 1999;24:524–8. doi: 10.1016/s1098-7339(99)90043-3. [DOI] [PubMed] [Google Scholar]
- 10.Pogrel MA. Permanent nerve damage from inferior alveolar nerve blocks - an update to include articaine. J Calif Dent Assoc. 2007;35:271–3. [PubMed] [Google Scholar]
- 11.Rood JP. The analgesia and innervation of mandibular teeth. Br Dent J. 1976;140:237–9. doi: 10.1038/sj.bdj.4803742. [DOI] [PubMed] [Google Scholar]
- 12.Haas DA, Harper DG, Saso MA, Young ER. Lack of differential effect by Ultracaine (articaine) and Citanest (prilocaine) in infiltration anaesthesia. J Can Dent Assoc. 1991;57:217–23. [PubMed] [Google Scholar]
- 13.Haas DA, Lennon D. Local anesthetic use by dentists in Ontario. J Can Dent Assoc. 1995;61:297–304. [PubMed] [Google Scholar]
- 14.Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine and lidocaine mandibular buccal infiltration anesthesia: A prospective randomized double-blind cross-over study. J Endod. 2006;32:296–8. doi: 10.1016/j.joen.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Robertson D, Nusstein J, Reader A, Beck M, McCartney M. The anesthetic efficacy of articaine in buccal infiltration of mandibular posterior teeth. J Am Dent Assoc. 2007;138:1104–12. doi: 10.14219/jada.archive.2007.0324. [DOI] [PubMed] [Google Scholar]
- 16.Oliveira PC, Volpato MC, Ramacciato JC, Ranali J. Articaine and lignocaine efficiency in infiltration anaesthesia: A pilot study. Br Dent J. 2004;197:45–6. doi: 10.1038/sj.bdj.4811422. [DOI] [PubMed] [Google Scholar]
- 17.Certosimo AJ, Archer RD. A clinical evaluation of the electric pulp tester as an indicator of local anesthesia. Oper Dent. 1996;21:25–30. [PubMed] [Google Scholar]
- 18.Claffey E, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of articaine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod. 2004;30:568–71. doi: 10.1097/01.don.0000125317.21892.8f. [DOI] [PubMed] [Google Scholar]
- 19.Yonchak T, Reader A, Beck M, Clark K, Meyers WJ. Anesthetic efficacy of infiltrations in mandibular anterior teeth. Anesth Prog. 2001;48:55–60. [PMC free article] [PubMed] [Google Scholar]
- 20.Meechan JG. Supplementary routes to local anaesthesia. Int Endod J. 2002;35:885–96. doi: 10.1046/j.1365-2591.2002.00592.x. [DOI] [PubMed] [Google Scholar]
- 21.Mikesell P, Nusstein J, Reader A, Beck M, Weaver J. Comparison of articaine and lidocaine for inferior alveolar nerve blocks. J Endod. 2005;31:265–70. doi: 10.1097/01.don.0000140576.36513.cb. [DOI] [PubMed] [Google Scholar]
- 22.Costa CG, Tortamano IP, Rocha RG, Francischone CE, Tortamano N. Onset and duration periods of articaine and lidocaine on maxillary infiltration. Quintessence Int. 2005;36:197–201. [PubMed] [Google Scholar]
- 23.Doğan N, Uçok C, Korkmaz C, Uçok O, Karasu HA. The effects of articaine hydrochloride on wound healing: An experimental study. J Oral Maxillofac Surg. 2003;61:1467–70. doi: 10.1016/j.joms.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 24.Sierra Rebolledo A, Delgado Molina E, Berini Aytís L, Gay Escoda C. Comparative study of the anesthetic efficacy of 4% articaine versus 2% lidocaine in inferior alveolar nerve block during surgical extraction of impacted lower third molars. Med Oral Patol Oral Cir Bucal. 2007;12:E139–44. [PubMed] [Google Scholar]


