Abstract
Background:
There is limited evidence about the distinguished effect of 3D oral health education videos over conventional 2 dimensional projections in improving oral health knowledge. This randomized controlled trial was done to test the effect of 3 dimensional oral health educational videos among first year dental students.
Materials and Methods:
80 first year dental students were enrolled and divided into two groups (test and control). In the test group, 3D animation and in the control group, regular 2D video projections pertaining to periodontal anatomy, etiology, presenting conditions, preventive measures and treatment of periodontal problems were shown. Effect of 3D animation was evaluated by using a questionnaire consisting of 10 multiple choice questions given to all participants at baseline, immediately after and 1month after the intervention. Clinical parameters like Plaque Index (PI), Gingival Bleeding Index (GBI), and Oral Hygiene Index Simplified (OHI-S) were measured at baseline and 1 month follow up.
Results:
A significant difference in the post intervention knowledge scores was found between the groups as assessed by unpaired t-test (p<0.001) at baseline, immediate and after 1 month. At baseline, all the clinical parameters in the both the groups were similar and showed a significant reduction (p<0.001)p after 1 month, whereas no significant difference was noticed post intervention between the groups.
Conclusion:
3D animation videos are more effective over 2D videos in periodontal disease education and knowledge recall. The application of 3D animation results also demonstrate a better visual comprehension for students and greater health care outcomes.
Keywords: 3D animation, knowledge recall, periodontal health
INTRODUCTION
According to the World Health Organization (WHO), health education is any combination of learning experiences designed to help individuals and communities improve their health, by increasing their knowledge or influencing their attitudes. Thus, health education not only plays a very crucial role but also remains as an elementary instrument in health promotion and disease prevention, especially in developing countries. It is important that health education should not just confine to the transmission of information, but should aim to make the target population understand the given information, execute the recommendations, and adapt to healthier lifestyles.[1] However, in clinical practice, it was discerned that doctors tend to undervalue the patient's desire for information and misperceive the process of sharing information.[2] With a shift toward patient-centered care, it becomes important to equip patients with appropriate knowledge and to construct scientific beliefs enabling them to make appropriate healthcare decisions and to rationally redesign their lifestyles.
Oral health education could be comprehended in a similar way, and a shift in the terminology from dental health education to oral health education over the years should be appreciated at this juncture, which emphasizes on the health of the mouth as a whole rather than confining to the teeth. Dental health education has also been subjected to many practical refinements together with theoretical and terminological modifications. One such refinement is the increased utilization of inputs from the fields of education, sociology, and psychology.
The prevalence of periodontal disease is high universally and is a substantial public health problem for countries. The fact that periodontal disease contributes to the global burden of chronic disease makes it a problem of profound importance that has to be addressed.[3] In the first ever national-level epidemiological survey on oral health conducted by the Dental Council of India (DCI), it was identified that the prevalence of periodontal disease was high among the Indian population, which increased with age. The prevalence was highest among those in the age group of 35–44 years, with 89.6% of subjects in this age group identified as having periodontal diseases.[4] It has evolved as a significant public health problem reckoning its impact on the quality of life of individuals and communities. Hence, it becomes exceedingly important for a dentist or a periodontist to corroborate their patient's understanding of the etiology of periodontal diseases, the wide range of treatment choices available, and the sequelae of neglect. Knowledge is an invaluable asset to the patients both for staying healthy and seeking required care in situations of need.
Patients’ adherence to recommendations by a healthcare professional hugely depends on their health literacy.[5] Health literacy also plays a role in the verbal communication between the patient and the healthcare professional, which often gets filled with a lot of intricate medical terminology.[6] Oral health education in clinical practice largely involves display of static pictures and face to face provision of informal education by the oral healthcare professionals. However, there is sound evidence that three-dimensional (3D) animations help the viewers to acquire better understanding of objects with intricate details compared to static orthographic [two-dimensional (2D)] depictions.[7] The greatest advantage with 3D animations is that over-reliance on the health professional–patient communication and its apparent limitations can be partially negotiated, if not completely. It is inferred that periodontal structures and the causes, presenting features, preventive measures, and treatment modalities for periodontal problems, which often are difficult to comprehend in 2D depictions, could be better understood in 3D projections. Nevertheless, there is limited evidence about the distinguished effect of 3D oral health educational videos in improving oral health knowledge of the received. The purpose of this randomized controlled trial was to test the effectiveness of 3D oral health educational videos over conventional 2D projections among the first year dental students in a dental college in South India.
MATERIALS AND METHODS
Study design
This was a parallel, randomized controlled trial with an allocation ratio of 1:1 using computer-generated randomization method. The study protocol was approved by the institutional ethics committee and no alterations to the trial methods were executed. The predefined eligibility criteria remained the same after the commencement of the trial. This randomized controlled trial is reported in compliance with the Consolidated Standards of Reporting Trials (CONSORT) statement. First year dental students who were willing to participate were included in the trial. This study was conducted in a dental college in South India from October 2014 to February 2015. The eligibility criteria for the recruitment of the study sample are as follows: (1)First year dental students who got admission in the 2014–2015 academic year; (2) students who did not receive a formal periodontal health education before; and (3) Students without any systemic problems and vision impairment. Out of 90 students who were evaluated for eligibility, 80 students met the eligibility criteria. These students were randomized and enrolled in the trial. Randomization was done to ensure unbiased allocation of study subjects to the test group and control groups. We believe that there could be extraneous variables, other than the type of intervention, which may influence the final outcome, like the ability of the participants to concentrate during the educational session, IQ levels, previous exposure to basic oral health education, etc. This enunciates the need for randomization. Controlled randomization of study participants was done to ensure equal size of groups and to avail its statistical advantages over simple random allocation.
The participants were distributed into two groups (test and control groups). The participants in the test group were given oral health education pertaining to periodontal anatomy, etiology, presenting conditions, preventive measures, and treatment for periodontal problems using a 3D animation video. Participants in the control group were given the same education using regular 2D video projections. Both the interventions were carried out in a classroom setting and the duration of intervention for both the groups was same (4 min and 15 s). The content of the voice over was repeatedly reviewed by experts for content validity till no further modifications were required. As this was a homotrait (same content), multimethod (different forms) approach, care was taken to ensure complete emphasis to the method of delivery of education (2D or 3D) by matching the voice over and thereby eliminating potential confounding effects.
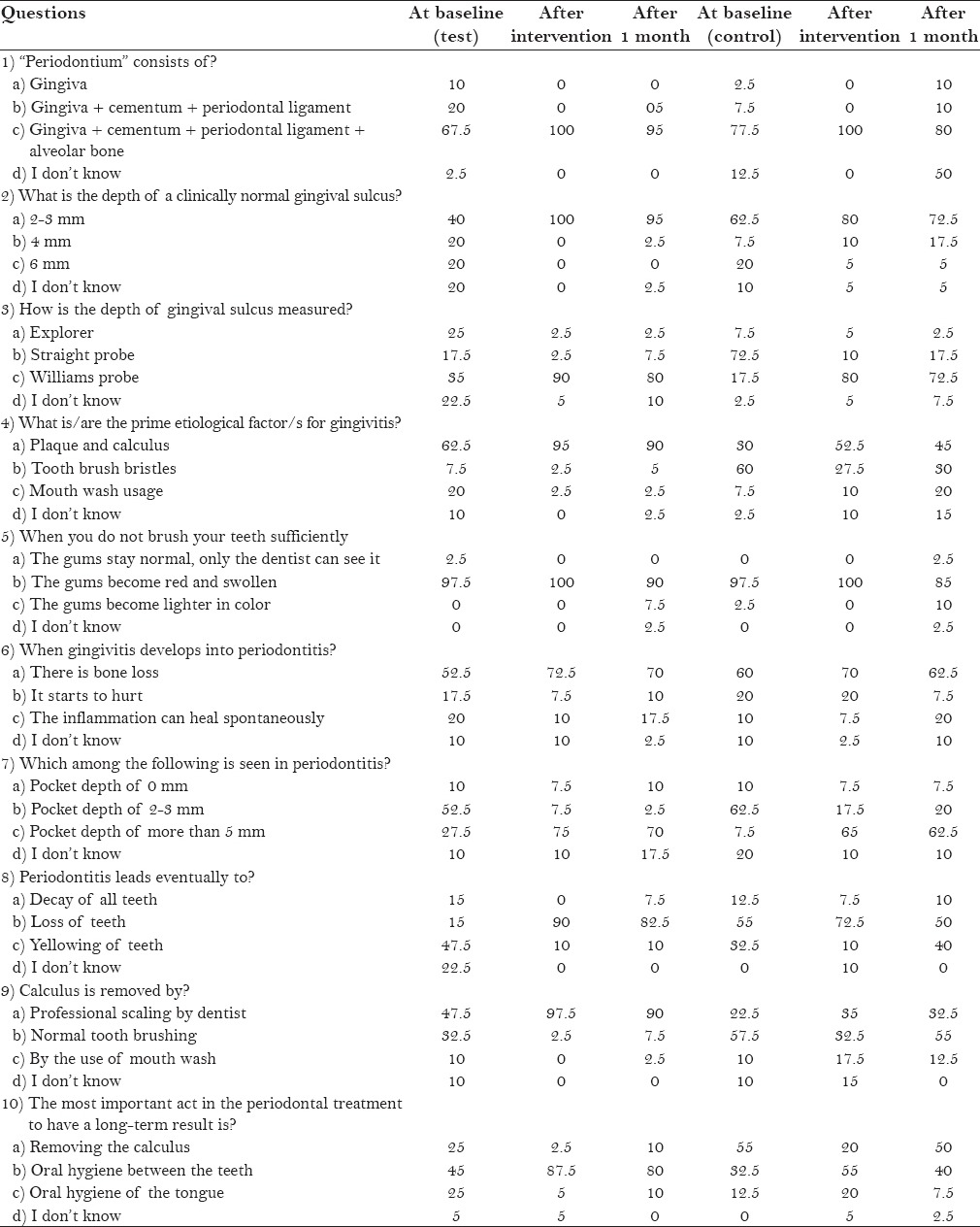
Oral health knowledge, in general, and periodontal knowledge, in particular, was the elementary factor of interest. We used a multiple-choice questionnaire for the assessment of outcome measure [Table 1]. The questionnaire consisted of 10 questions, with each question having four options to choose the answer from. Every question had one correct option, two wrong options, and a “don’t know” option. “Don’t know” was given as an option for every question to ensure complete filling of the questionnaire, as some participants may not want to answer something they do not know, and also to curtail the possibility of correct answers by chance. Without this option, the obligation to choose one of the options may yield good results just by chance. Demographic data on age and gender were also included in the questionnaire. We also assessed the oral hygiene status of the participants at baseline and 1 month post intervention using oral hygiene index simplified (OHI-S),[8] Plaque Index (PI),[9] and the ginigival status of the participants using Gingival Bleeding Index (GBI).[10] These were collectively referred to as oral health status in the context of this article.
Table 1.
Study questionnaire and the percentage of participants choosing correct options in both the groups at baseline and post intervention
The null hypothesis is that there were no differences between the test and control groups with respect to their mean scores in the study questionnaire and the mean scores as recorded by the aforementioned indices post intervention. Differences between the knowledge of the participants and the oral health status in the test and control groups at baseline and post intervention were analyzed using unpaired t-test. Paired t-test was used for analyzing differences between baseline and post intervention scores in both the test and control groups. Descriptive statistics were used and the likelihood of being more knowledgeable post intervention was depicted with odds ratio [95% confidence interval (CI)].
The videos with voice over were assessed for clarity and quality by administering them to five patients attending the outpatient department of the institution who could read, write, and understand English. The pace at which the voice over was recorded was adjusted based on the suggestions received and few sentences were re-recorded owing to dearth of clarity. The intention behind the study was to test the effectiveness of 3D animation videos over conventional 2D videos and the study was considered as an initial move before translating the content of voice over to the regional language and administering it to a larger group of patients. All the participants were administered the questionnaire before receiving the allotted intervention and were clinically examined to record the baseline oral health status. The educational sessions were conducted in silent classrooms using liquid crystal display projectors. Participants in the test and control groups received the intervention at the same time in different classrooms. The same questionnaire was administered immediately post intervention and after 1 month post intervention. The participants had to choose the answers on their own on all three occasions and measures were taken to avoid sharing opinions and views during the time of answering the questionnaire. Clinical examination was conducted 1 month after the intervention by the same examiner who had performed the examination at baseline, to eliminate observational bias.
RESULTS
A total of 90 students were assessed for eligibility. Ten were excluded from the study, and finally 80 participants were randomized and enrolled in the trial to receive the intended interventions.
Demographic characteristics on age and gender are not provided here as all the participants belonged to the same age group and a majority of the participants were females (92.5%). So, a separate analysis based on gender was not considered owing to the small number of male participants in the trial. The analysis was limited to comparisons between the test and the control groups with respect to their baseline and post intervention performances in the study questionnaire and oral health status. The descriptive statistics of the oral health knowledge questionnaire at baseline, immediately post intervention, and 1 month post intervention are given in Table 2. The test and the control groups were not different with respect to their baseline mean knowledge scores (P = 0.092, unpaired t-test). Nevertheless, significant differences in the immediate post intervention and 1 month post intervention scores were found between the groups as assessed by unpaired t-test (P < 0.001).
Table 2.
Descriptive statistics of oral health knowledge scores at baseline, immediately post intervention, and 1 month post intervention in the test (3D) and control (2D) groups
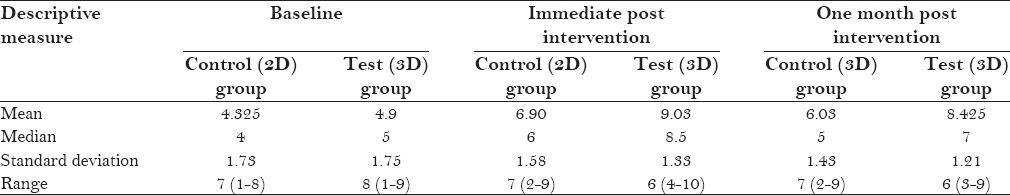
We also analyzed the differences between mean baseline scores and mean post intervention scores in the test and control groups using paired t-tests. There were significant (P < 0.001) differences between the mean scores at baseline and post intervention in both the test and control groups [Table 2].
We calculated the odds ratio to assess the likelihood of choosing a correct answer by the kind of intervention received. The participants in the test group were found to be 3.91 times more likely to choose a correct answer compared to the participants in the control group immediately post intervention and this was statistically significant (95% CI: 2.64–5.81).
The test and control groups were homogenous with respect to their PI scores at baseline. No significant differences in mean PI scores were found between the groups after 1 month. There was significant reduction in the mean PI scores post intervention in both the groups (P < 0.001) [Table 3]. Similar findings were observed with respect to the bleeding index scores within and between the test and control groups (P < 0.001) [Table 3].
Table 3.
Comparative evaluation of PI, BI, OHI-S scores at baseline and 1 month post intervention in the test and control groups
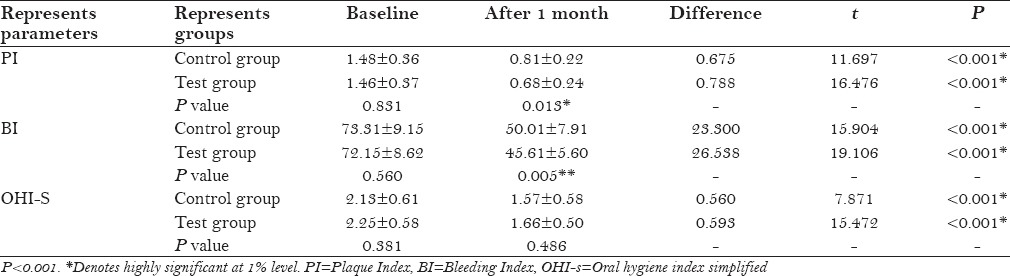
However, there were no differences in the OHI-S scores between the test and control groups both at baseline and post intervention. Significant improvement in oral hygiene was found in the both groups from baseline to post intervention (P < 0.001) [Table 3].
DISCUSSION
It is clear from the results that both the interventions have a profound impact on the periodontal health knowledge of the participants and their oral health status. These results are consistent with a study conducted on 68 periodontitis patients.[11] Participants who had received 3D education showed significantly better improvement compared to those who received 2D interventions, with the exception of OHI-S scores. The baseline scores in the test and control groups were homogenous without significant differences. It was found that the periodontal knowledge scores of the participants had significantly improved with both the interventions. This could be easily understood as transmission of information more likely results in an improvement in knowledge when properly executed. Nevertheless, there were significant differences between the periodontal knowledge scores of the test and control groups after the intervention, which highlights the effectiveness of 3D education over 2D projections.[12]
An improvement in PI scores was also observed from baseline to post intervention. The PI scores in the test group were significantly less compared to those of the control group 1 month after the intervention. The 3D video on mechanical plaque removal might have had a better impact on the participants of the test group than the 2D mechanical plaque control education received by the control group. Brushing endured through time as the most effective method for plaque control and for maintenance of gingival health. Educational videos administered in the study consisted of the brushing technique, and this could have positively influenced a change in the bleeding index of the participants in both the groups from baseline to post intervention. The fact that calculus is so tenacious that it cannot be removed by home-based mechanical oral hygiene measures could have played a role in the OHI-S scores being similar between the test and control groups post intervention. It was inferred that the percentage of participants who got oral prophylaxis done between the baseline and post intervention examinations was relatively comparable.
The periodontal knowledge scores as assessed by a close-ended questionnaire were found to be improved in both the groups. This improvement was not just limited to the data collected immediately after the intervention, but persisted as observed from the data collected 1 month post intervention. These results highlighted knowledge recall, and the recall of knowledge was considerably high among the participants in the test group compared to those in the control group. This increase in post intervention knowledge in the test group has a consistent explanation from the results of a study conducted using 3D multimedia system for patient education.[13] Another finding from the study was improvement in compliance of the participants after the intervention, which is clear from the post intervention oral health status. Regardless of the type of intervention received, participants’ compliance to oral hygiene measures had increased along with the periodontal health knowledge. The reasons for such improvement could be found in the comprehensiveness of the information provided through the interventions, which included the etiology, symptoms, preventive actions, available treatment options, and the sequelae of neglect. These results are in accordance with a study conducted on 30 male patients who were matched for age and education.[14]
There was enough evidence suggesting the advantages of computer-based oral health education over personal communication and printed material.[15] Though the information provided is same, computer-based education does have an extra edge in terms of enabling the patients to visualize the information and to better accumulate this information to the existing knowledge. Such visualization and comprehensive information obviously aid in improvement of knowledge, better retention of the acquired knowledge, realization of the importance of compliance to oral health instructions, and better oral health practices.
English was the medium of communication in the interventions received by the participants. This study should be looked upon as an initial move to test for the effectiveness of 3D periodontal health education over that of 2D education. The ultimate aim of the investigators is to develop a 3D periodontal health educational video in the regional language, based on the findings from this study. This would involve translation, checking for cross-cultural validity, and a pilot study to realize the scope for improvement.[16] The reason for choosing first year dental students was that they were comparable with the general population in terms of their periodontal health knowledge with only a month of experience as a student of dentistry. Also, the interventions may help them to better understand their curriculum and incorporates a sensible view on how to comprehend oral health related problems. Since there was no standardized measure for assessment of periodontal health knowledge, we had designed a questionnaire applicable to the area of the study, which was checked for content validity by experts in the field. However, there is a need to develop a comprehensive, standardized measure to assess periodontal health knowledge of people, and such measures should be thoroughly reviewed for validity and reliability.
CONCLUSION
To sum up, 3D videos serve as an invaluable tool in improving patients’ periodontal health knowledge and understanding of the disease process. They also enable the patients to better comply with instructions, which apparently results in better oral health status. The ultimate objective of oral healthcare professionals is improvement in the health status of their patients, in general, and oral health status, in particular. The 3D periodontal health education videos could help them succeed in their quest.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I thank all the participants for their support in completing the study.
REFERENCES
- 1.Nutbeam D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15:259–67. [Google Scholar]
- 2.Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189–99. [PMC free article] [PubMed] [Google Scholar]
- 3.Petersen PE, Ogawa H. The global burden of periodontal disease: Towards integration with chronic disease prevention and control. Periodontol 2000. 2012;60:15–39. doi: 10.1111/j.1600-0757.2011.00425.x. [DOI] [PubMed] [Google Scholar]
- 4.Bali RK, Mathur VB, Talwar PP, Chanana HB. 1st ed. New Delhi: Dental Council of India and Ministry of Health and Family Welfare, Government of India; 2004. National oral health survey and fluoride mapping 2002-2003 India. [Google Scholar]
- 5.Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, et al. Closing the loop: Physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 6.Jackson LD. Information complexity and medical communication: The effects of technical language and amount of information in a medical message. Health Commun. 1992;4:197–10. [Google Scholar]
- 7.Wu CF, Chiang MC. Effectiveness of applying 2D static depictions and 3D animations to orthographic views learning in graphical course. Comput Educ. 2013;63:28–42. [Google Scholar]
- 8.Greene JC, Vermilion JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:7–13. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 9.Silness J, Loe H. Periodontal diseases in pregnancy. II. Correlation between oral hygiene and periodontal conditions. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 10.Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25:229–35. [PubMed] [Google Scholar]
- 11.Cleeren G, Quirynen M, Ozcelik O, Teughels W. Role of 3D animation in periodontal patient education: A randomized controlled trial. J Clin Periodontol. 2014;41:38–45. doi: 10.1111/jcpe.12170. [DOI] [PubMed] [Google Scholar]
- 12.Hermann M. 3D computer animation – A new medium to optimize preoperative information for patients. Evaluation of acceptance and effectiveness in a prospective randomized study-video versus text. Chirurg. 2002;73:500–7. doi: 10.1007/s00104-001-0416-y. [DOI] [PubMed] [Google Scholar]
- 13.Hu J, Yu H, Shao J, Li Z, Wang J, Wang Y. An evaluation of the dental 3D multimedia system on dentist–patient interactions: A report from China. Int J Med Inform. 2008;77:670–8. doi: 10.1016/j.ijmedinf.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 14.Philippot P, Lenoir N, D’Hoore W, Bercy P. Improving patients’ compliance with the treatment of periodontitis: A controlled study of behavioural intervention. J Clin Periodontol. 2005;32:653–8. doi: 10.1111/j.1600-051X.2005.00732.x. [DOI] [PubMed] [Google Scholar]
- 15.Patel JH, Moles DR, Cunningham SJ. Factors affecting information retention in orthodontic patients. Am J Orthod Dentofacial Orthop. 2008;133(Suppl 4):S61–7. doi: 10.1016/j.ajodo.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 16.Mladenovski A, Kieser JA. The efficacy of multimedia pre-operative information for patients: A pilot study. N Z Dent J. 2008;104:36–43. [PubMed] [Google Scholar]


