Abstract
Objective
The propensity of people vulnerable to suicide to make poor life decisions is increasingly well documented. Do they display an extreme degree of decision biases? The present study used a behavioral decision approach to examine the susceptibility of low-lethality and high-lethality suicide attempters to common decision biases, which may ultimately obscure alternative solutions and deterrents to suicide in a crisis.
Method
We assessed older and middle-aged individuals who made high-lethality (medically serious; N=31) and low-lethality suicide attempts (N=29). Comparison groups included suicide ideators (N=30), non-suicidal depressed (N=53), and psychiatrically healthy participants (N=28). Attempters, ideators, and non-suicidal depressed participants had unipolar non-psychotic major depression. Decision biases included sunk cost (inability to abort an action for which costs are irrecoverable), framing (responding to superficial features of how a problem is presented), under/overconfidence (appropriateness of confidence in knowledge), and inconsistent risk perception. Data were collected between June of 2010 and February of 2014.
Results
Both high- and low-lethality attempters were more susceptible to framing effects, as compared to the other groups included in this study (p≤ 0.05, ηp2 =.06). In contrast, low-lethality attempters were more susceptible to sunk costs than both the comparison groups and high-lethality attempters (p≤ 0.01, ηp2 =.09). These group differences remained after accounting for age, global cognitive performance, and impulsive traits. Premorbid IQ partially explained group differences in framing effects.
Conclusion
Suicide attempters’ failure to resist framing may reflect their inability to consider a decision from an objective standpoint in a crisis. Low-lethality attempters’ failure to resist sunk-cost may reflect their tendency to confuse past and future costs of their behavior, lowering their threshold for acting on suicidal thoughts.
Keywords: Depression, decision-making, suicide, attempted, elderly
INTRODUCTION
Older adults who attempt suicide often regret this decision, describing it as a “bad choice.” A constricted temporal focus on immediate goals and concrete thinking have been theorized to obscure alternatives to suicide in a crisis1, 2. People often proceed with the suicidal plan even after realizing, in the words of Dostoevsky, its “absurdity and monstrosity”3 (see also, attemptsurvivors.com/our-stories/). According to behavioral decision theory, humans aim to be optimal decision makers by making rational choices as proposed by, for example, expected utility theory4. By contrast, suicidal behavior often co-occurs with conditions hallmarked by suboptimal decisions such as gambling and addiction5, 6. While the evidence is mixed7, a number of studies reported that, in the laboratory, suicide attempters perform poorly on gambling tasks8, 9 and describe themselves as poor problem solvers10, 11, suggesting that suicidal behavior is facilitated by poor decision-making.
Behavioral decision research has revealed that people often systematically deviate from normative standards for rational decision-making (for a review of normative decision theory, see Edwards4). For example, they persist with failing plans despite irrecoverable investments, i.e. sunk cost bias12, and make decisions that are influenced by irrelevant variations in how information is presented, i.e. framing effects13. Systematic individual differences in such decision-making biases14 can be captured with a validated measure, the Adult Decision-Making Competence battery of tasks (A-DMC). This measure has reliability across decision-making tasks, and validity for real-world decision outcomes even after controlling for fluid intelligence and socioeconomic status14, 15. However, neither these insights into decision-making biases nor this measure have yet been applied to characterize decision deficits associated with suicidal behavior. Thus, we investigated whether suicide attempters demonstrate exaggerated decision-making biases.
Our study focused on attempted suicide in older- and middle-aged adults, since the suicide rate is high in these age groups16. Additionally, older adults who attempt suicide are more similar, demographically, to those who die by suicide than are younger suicide attempters. Suicide attempts also tend to be more lethal in older adults17. Furthermore, most older adults who attempt suicide suffer from depression18, 19, however, only a minority contemplate suicide, and an even smaller number proceed to act on those thoughts. To characterize the relationship between attempted and/or contemplated suicide and decision-making competence, above and beyond the effects of depression or suicidal ideation, our study groups included older adults with a history of suicide attempt (attempters), those who have contemplated suicide but have never attempted (ideators), depressed individuals with no history of suicide attempt or suicidal ideation (non-suicidal depressed), and psychiatrically healthy older adults. This design allowed us to investigate systematic group differences in the decision-making competence, which could suggest or disprove the possibility that decision biases operate at the final stage of the suicidal process; that of acting on the suicidal ideas.
Moreover, suicide attempts are heterogeneous, ranging from high-lethality, with significant medical damage requiring admission to a medical/surgical unit or treatment in an emergency outpatient department, to low-lethality suicide attempts which are not likely to cause significant medical damage. High- and low-lethality attempters often display distinct clinical and biological profiles20, 21. Earlier studies indicated that low-lethality attempters displayed exaggerated discounting of delayed rewards22, while high-lethality attempters were characterized by deficits in cognitive inhibition23, 24, failure to shift sets25, and interference of social emotions with decision making26. However, it remains an open question how/whether the heterogeneity in the lethality of suicidal behavior maps onto specific decision-making deficits. Tests of biases are one way to capture the decision-making phenotypes of suicide attempters. Thus, our analyses examined decision-making biases in high- and low-lethality suicide attempters separately.
We tested whether older adults who attempted suicide would display lower decision-making competence than the other groups, as seen in lower scores across the following A-DMC tasks:
Resistance to Sunk Costs: measures the ability to discontinue actions where costs are irrecoverable27. Compared to other domains of decision competence, resistance to sunk costs is a more affect-laden process. For example, negative emotions such as anger28 and anxiety29 have been shown to increase sunk-cost bias. In our previous studies, low-lethality suicide attempts were associated with maladaptive impulsive behaviors, such as inability to delay gratification22. Therefore LL attempters can be thought of as generally having a lower threshold for acting on their suicidal thoughts, in contrast to HL attempters, who tend to engage in more premeditation, preparation, and choose more lethal methods. Thus, we investigated whether LL attempters would be more likely to show deficits in this affectively-laden domain of decision competence.
Resistance to Framing Effects: measures the ability to make decisions that are unaffected by normatively meaningless differences in how information is presented. Resisting framing effects is cognitively demanding, as one needs to conceptualize the problem on an abstract level, thus performance is likely affected by cognitive deficits that have been associated with suicide attempts24, 30–32. Therefore, we investigated whether both HL and LL attempter groups would be overly influenced by framing effects.
Under/Overconfidence: assesses the appropriateness of confidence in one’s knowledge. The tendency to overestimate knowledge is sometimes diminished in patients with mood disorders (“depressive realism33”). Given this, and the association of depression with pessimism, we investigated whether non-depressed participants would be more likely to report confidence that is not justified by their level of knowledge.
Consistency in Risk Perception: assesses the ability to follow probability rules when thinking about the likelihood of future events. Given our previous findings that suicide attempters ignored probabilities on a gambling task9, we investigated whether both attempter groups would have deficits in following probability rules as measured by this task.
Finally, we examined whether group differences in decision competence were epiphenomenal (secondary) to other components of vulnerability to suicide. For example, cognitive impairment24, 25, 30, 32 and impulsive-aggressive personality traits34, 35 have been recognized as components of individual vulnerability to suicide (“suicidal diathesis”). Studies have shown a negative correlation between cognitive ability and violations of cost-benefit rules, such as resistance to sunk costs36 and framing errors37. In addition, certain maladaptive personality traits that are over-represented among suicidal people, such as high neuroticism, low conscientiousness, and high impulsivity38, have been associated with framing errors39, 40. Thus, we examined whether group differences in decision-making competence persisted after accounting for cognitive ability, chronic interpersonal difficulties, and impulsivity.
METHOD
Sample and Procedures
The study included 171 participants (age range=42–97, mean= 66.3 sd=9.9). All participants provided written informed consent. Data were collected between June 2010 and February 2014. The University of Pittsburgh Institutional Review Board approved the study.
Suicide attempters (N=60) had engaged in a self-injurious act with the intent to die within a two-week period prior to entering the study, or had a history of past suicide attempt and current suicidal ideation with a plan at the time of study enrollment. Medical seriousness of attempts was assessed using the Beck Lethality Scale (BLS)41. For participants with multiple attempts, data for the highest lethality attempt is presented. Following the literature, high-lethality attempters scored ≥ 4 on the BLS, whereas low-lethality attempters incurred no significant medical damage and scored a 3 or less on the BLS. Current suicidal ideation was assessed using the Beck Scale of Suicidal Ideation42.
Suicide ideators (N=30) endorsed suicidal ideation with a specific plan, but had no lifetime history of suicide attempt. These participants seriously contemplated suicide and communicated some intention to family or medical staff triggering inpatient psychiatric admission or initiation of mental health treatment.
Non-suicidal depressed participants (N=53) had no lifetime history of suicide attempt or suicidal ideation. Participants with passive death wish were excluded from the non-suicidal depressed group.
Suicide attempters, ideators, and non-suicidal depressed participants were diagnosed with unipolar non-psychotic major depression using the Structured Clinical Interview for DSM-IV Axis I Disorders43. Depression severity was measured by the 17-item Hamilton Rating Scale for Depression44. We excluded individuals with clinical dementia (score < 24 on the Mini-Mental State Examination45), and those with a history of neurological disorders, delirium, or sensory disorders that preclude neuropsychological testing. Participants continued to receive psychotropic medications as clinically indicated. We also included 28 non-psychiatric controls, who had no lifetime history of mental health treatment and no lifetime diagnosis of DSM-IV axis I disorders (healthy controls, [HC]).
For demographic and clinical characterization of the sample, see Table 1.
Table 1.
Demographic and Clinical Characteristics (N=171)
| Non-Psychiatric Controls (HC) (N=28) |
Depressed Non-Suicidal (D) (N=53) |
Ideators (I) (N=30) |
Low-Lethality Attempters (LL) (N=29) |
High-Lethality Attempters (HL) (N=31) |
F value/ X2 |
P value | Post-Hoc Comparisons | |
|---|---|---|---|---|---|---|---|---|
| Age | 68.4 (12.0) | 69.4 (8.7) | 65.1 (10.7) | 62.0 (7.4) | 64.0 (9.6) | 3.7 | 0.006 | D>LL |
| Gender (%Male) | 43% | 45% | 60% | 52% | 52% | X2 = 2.3 | 0.68 | -- |
| Race (%White) | 86% | 79% | 87% | 79% | 97% | X2 = 7.2 | 0.51 | -- |
| Years of Education | 14.8 (2.0) | 14.4 (2.6) | 15.0(2.9) | 14.4 (3.1) | 12.8 (3.3) | 2.9 | 0.02 | I>HL |
| Household Income per capita (× 1000) | 24.6 (12.9) | 18.4 (20.3) | 23.4 (28.3) | 17.8 (20.2) | 20.3 (18.6) | 0.59 | 0.67 | -- |
| Hamilton Depression Rating Scale (without suicide items) | 2.3(1.9) | 11.9 (5.2) | 13.4 (6.3) | 17.7 (7.0) | 15.1 (8.4) | 27.0 | p<.001 | HC< D, I, LL, HL D<LL |
| Global cognitive functioning: DRSa total score | 138 (3.4) | 135 (5.3) | 133 (8.5) | 134 (5.5) | 133 (6.6) | 3.2 | 0.015 | HC>HL |
| Lifetime Substance Abuse | - | 5 (10%) | 11 (37%) | 8 (28%) | 9 (29%) | X2 = 9.1 | 0.03 | -- |
| Current Substance Abuse | - | 0 | 7 (23%) | 5 (17%) | 3 (10%) | X2 = 7.4 | 0.06 | -- |
| Current Suicide Ideation | 0.04 (0.2) | 0.2 (0.7) | 15.4 (8.3) | 24.5 (8.4) | 25.8 (3.9) | 199 | p<.001 | HC, D<I, LL, HL I<LL, HL |
| Suicide Intent | - | - | - | 14.9 (5.3) | 19.3 (4.5) | 12 | 0.001 | -- |
| Suicide Intent Planning Subscale | - | - | - | 5.5 (2.9) | 8.0 (2.7) | 11 | 0.002 | -- |
| Age at First Attempt | - | - | - | 47.1 (16.1) | 54.2 (18.3) | 2.4 | 0.13 | -- |
| Number of Attempts | - | - | - | 1.6 (0.9) | 1.7 (1.1) | 0.1 | 0.74 | -- |
| Intensity of Antidepressant Pharmacotherapy during Current Episodeb | - | 3.9 (1.0) | 4.6 (1.7) | 5.0 (2.0) | 6.0 (3.1) | 6.8 | p<.001 | DC, I< HL |
| IIP Interpersonal Sensitivityc | 2.4 (2.2) | 6.0 (3.9) | 9.3 (5.3) | 9.2 (3.9) | 8.4 (4.4) | 14.6 | p<.001 | HC<D, I, LL, HL D<I, LL |
| IIP Interpersonal Ambivalenced | 2.9 (4.2) | 3.7 (3.4) | 5.5 (5.0) | 6.8 (5.3) | 5.7 (5.4) | 3.8 | 0.006 | H<LL D<LL |
| IIP Aggressione | 1.2 (1.5) | 4.3 (3.8) | 6.2 (4.9) | 5.7 (3.5) | 4.7 (5.1) | 6.3 | p<.001 | HC<D, I, LL, HL |
| SPSI Impulsive/Careless Stylef | 1.5 (1.7) | 4.9 (3.6) | 4.7 (3.0) | 6.0 (3.7) | 7.1 (4.7) | 9.6 | p<.001 | HC<D, I, LL, HL D<HL |
| WTARg | 111.8 (8.5) | 106.2 (14.9) | 108.6 (15.2) | 100.2 (15.3) | 98.9 (18.1) | 3.5 | 0.01 | HC >HL |
Mattis Dementia Rating Scale
Threshold greater than 3
Inventory of Interpersonal Problems Interpersonal Sensitivity Subscale
Inventory of Interpersonal Problems Interpersonal Ambivalence Subscale
Inventory of Interpersonal Problems Aggression Subscale
Social Problem Solving Inventory Impulsivity/Carelessness Style Subscale
Wechsler Test of Adult Reading
Gender, race and per capita household income were similar across groups. Non-suicidal depressed participants were older than the suicide attempters. In addition, high-lethality attempters had lower education than non-psychiatric controls and suicide ideators. Consequently, we included age and education in the regression models as covariates.
A-DMC: A-DMC is available online http://www.sjdm.org/dmidi/Adult_-_Decision_Making_Competence.html; for detailed description see14. A research specialist administered the A-DMC task at the participants’ own pace. More on sample items and scoring can be found in the supplemental material. Briefly:
Susceptibility to sunk cost bias is measured by ten items (e.g., You and your friend have driven halfway to a resort. Both you and your friend feel sick. You both feel that you both would have a much better weekend at home. Your friend says it is "too bad" you already drove halfway, because you both would much rather spend the time at home. You agree. Would you be more likely to drive on or turn back?).
Resistance to framing effects is measured by seven-item pairs of attribute framing (e.g., the quality of ground beef labeled 80% lean or 20% fat, advising a family member about a cancer treatment with a 50% success rate or a 50% failure rate) and seven-item pairs measuring risky-choice framing tasks. The positive frames and negative frames appear in separate sets with different item orders and are separated by other A-DMC tasks.
Under/overconfidence: Participants indicate whether statements are true or false (e.g., Alcohol causes dehydration, True or False?), then assess their confidence in that answer on a scale from 50% (just guessing) to 100% (absolutely sure). The overall score reflects mean confidence minus percent correct across items. Overall, a decision maker who answers 70% of items correctly should express 70% confidence.
Consistency in Risk Perception: Twenty items ask participants to judge the chance of an event (e.g., What is the probability that you will get into a car accident while driving during the next year? What is the probability that your driving will be accident-free during the next year?) on a linear scale ranging from 0% (no chance) to 100% (certainty). Scoring is the percentage of consistent risk judgments across related events.
Global cognitive ability was assessed with the Mattis Dementia Rating Scale (DRS)46. Scores on the DRS range from 0–144, with lower scores indicating more impairment; its subscales assess Initiation/Perseveration, Attention, Construction, Conceptualization, and Memory. The Wechsler Test of Adult Reading (WTAR) was used as an estimate for premorbid intelligence47.
Impulsivity was assessed with the Social Problem Solving Inventory (SPSI) Impulsivity/Carelessness subscale48.
Chronic interpersonal problems were measured by the Inventory of Interpersonal Problems (IIP-15)49, 50, which assesses interpersonal sensitivity, ambivalence, and aggression indicative of a dysfunctional personality.
Data analyses: We first examined group differences in overall decision-making competence using a MANOVA with four normalized A-DMC subscale scores jointly considered as dependent variables. This analysis was repeated while taking into account possible confounders (demographic characteristics and global cognitive ability). To examine group differences in specific domains of decision-making, we performed follow-up ANOVAs using each of the four A-DMC subscales – as dependent variables. Taking advantage of our 5-group design, we followed up by systematically testing group differences reflecting presumed effects of depression, suicidal ideation, suicide attempt, and attempt lethality using a Helmert contrast (comparing healthy controls vs. all depressed, non-suicidal depressed vs. all suicidal (ideators, HL and LL), suicide ideators vs. all attempters, low-lethality vs. high-lethality attempters). The second model also included demographic characteristics to test whether group differences were robust to the inclusion of these covariates. A third model included all the above characteristics as well as the DRS score. Finally, in exploratory analyses, we tested potential explanatory variables (impulsivity, interpersonal functioning, depression severity, history of substance abuse, premorbid IQ) that may have accounted for group differences in decision competence.
RESULTS
Group differences in overall decision competence
A multivariate ANOVA, using the scores on the four A-DMC subscales as dependent variables, indicated significant group differences in decision-making competence (Wilks’ lambda = .83, F[16,516.94] = 2.06, p=0.009, ηp2=0.05), which remained after controlling for demographic characteristics (group: Wilks’ lambda = .81, F[16,489.44] = 2.23, p<0.01, ηp2=0.05; age: ηp2=0.04; sex: ηp2=0.07; race: ηp2=0.06; education: ηp2=0.05), and for global cognitive ability (group: Wilks’ lambda = .82, F[16,480.28] = 2.04, p=0.01, ηp2=0.05; age: ηp2=0.04; sex: ηp2=0.07; race: ηp2=0.06; education: ηp2=0.05; global cognitive ability: ηp2=0.07).
Group differences across domains
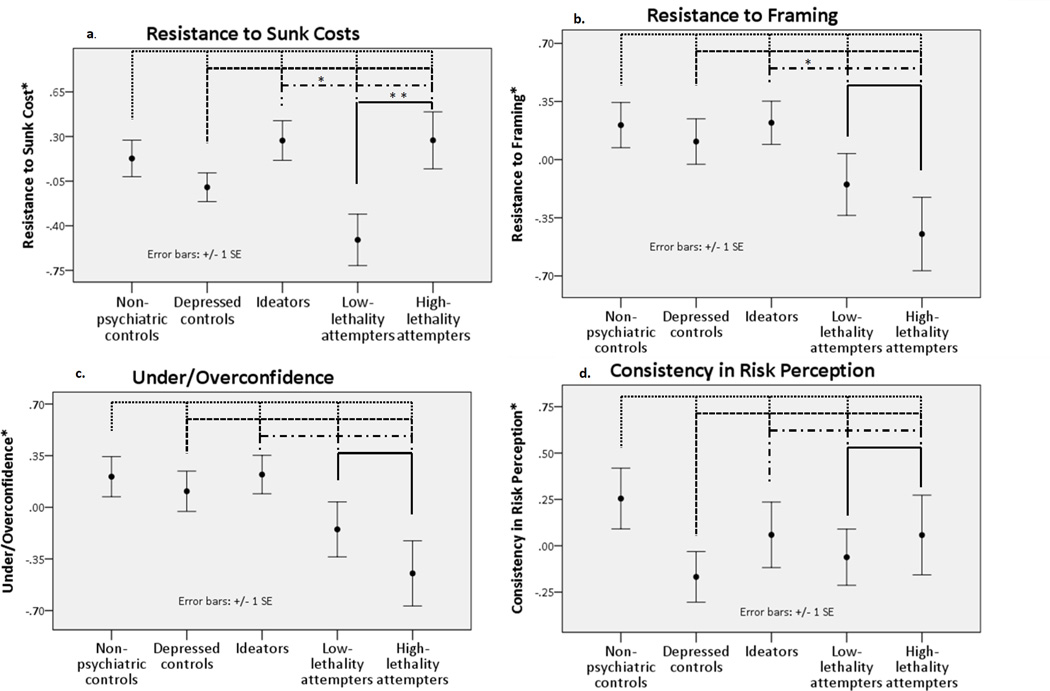
Next, we conducted separate univariate ANOVAs on each of the four A-DMC subscales. There were significant mean group differences in Resistance to Sunk Costs (see Table 2a). While all depressed participants did not differ from healthy controls (p=0.07) and all participants with suicidal ideation did not differ from non-suicidal depressed (p=0.96), suicide attempters were more susceptible to sunk cost than suicide ideators (p=0.04). Low-lethality attempters were more susceptible to sunk cost than high-lethality attempters (p<0.002; Figure 1a).
Table 2.
| a. Results: Resistance to Sunk Cost | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group differences in Resistance to Sunk Cost persist after accounting for demographic factors (Model 2) and global cognition (Model 3) | |||||||||||||
| Group Status | d.f | Gender | Race | Education (years) |
DRS | R-Squared | Adjusted R2 |
||||||
| F | η2 | F | η2 | F | η2 | F | η2 | F | η2 | ||||
| Model 1 | 4.2** | .09 | 4 | -- | -- | -- | -- | 0.09 | 0.07 | ||||
| Model 2 | 3.9** | .09 | 4 | .72 | .00 | 1.8 | .02 | 1.6 | .01 | -- | 0.13 | 0.08 | |
| Model 3 | 3.8** | .09 | 4 | 1.3 | .01 | 1.2 | .02 | .36 | .00 | 7.9** | .05 | 0.17 | 0.12 |
| b. Results: Resistance to Framing | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group differences in Resistance to Framing persist after accounting for demographic factors (Model 2) and global cognition (Model 3) | |||||||||||||||
| Group Status |
d.f | Gender | Race | Education Years |
DRS | Age | R-Squared | Adjusted R2 |
|||||||
| F | η2 | F | η2 | F | η2 | F | η2 | F | η2 | F | η2 | ||||
| Model 1 | 2.8* | .06 | 4 | -- | -- | -- | -- | -- | 0.06 | 0.04 | |||||
| Model 2 | 3.4* | .08 | 4 | 2.0 | .01 | 7.3*** | 08 | 5.4* | .03 | -- | 5.8* | 04 | 0.23 | 0.19 | |
| Model 3 | 3.2* | .07 | 4 | 2.0 | .01 | 7.1*** | 08 | 5.0* | .03 | .01 | .00 | 4.7* | 03 | 0.23 | 0.18 |
Observation N=171, DRS: Mattis Dementia Rating Scale,
p ≤ 0.01
Observations: N=171, DRS: Mattis Dementia Rating Scale,
p ≤ 0.05,
p ≤ 0.001
Figure 1.
Mean group differences in separate decision-making competencies as reflected by the Adult Decision-Making Competence battery of tasks. Lower scores represent worse performance. Helmert contrasts were performed to investigate the effect of depression, suicide ideation, suicide attempt, and attempt lethality.
* Mean standardized residual, adjusted for age, gender, race, education, and global cognition measured by DRS.
The vertical bars denote the standard errors of these estimates. *p ≤ .05 **p ≤ .005
There was also a significant mean difference in Resistance to Framing Effects across the groups (see Table 2b). While all depressed participants did not differ from healthy controls (p=.15) and all participants with suicidal ideation did not differ from non-suicidal depressed (p=.44), suicide attempters were more susceptible to framing effects than suicide ideators (p<.01; Figure 1b). There was no effect of attempt lethality (p=.23).
Contrary to our expectation that depressed participants were more likely to recognize the extent of their knowledge, we failed to find significant group differences in Under/Overconfidence (F[4,166]=1.4, p=0.23; Figure 1c). An additional analysis examining confidence after controlling for knowledge51 (i.e. whether one is more or less confident than his knowledge would justify) similarly failed to find any group differences (F[4,165]=2.1, p=0.09). There were also no group differences in Consistency of Risk Perception among the groups (F [4,166]=1.9, p=0.11; Figure 1d).
Group differences in Resistance to Sunk Cost and Framing Effects, adjusting for possible confounders
Group differences in Resistance to Sunk Cost scores remained significant after accounting for age, gender, race, and education (see Table 2a). Poorer global cognition (lower DRS scores) was associated with poorer resistance to sunk cost, (F[9, 161]= 3.6, p<0.001, ηp2=0.05) but even after its inclusion in the model, group differences remained (F[4, 161] = 3.8, p<0.01, ηp2=0.09).
Similarly, group differences remained significant when IQ (WTAR scores) (available on 150/171 participants) was added to the model (group: F[4,139] = 2.69, p = .03, ηp2 = .08, WTAR: F[1,139] = 4.29, p = .04, ηp2 = .03).
Group differences in Resistance to Framing Effects remained significant in the model including age, race, gender, and education (Supplementary eTable 1a), F[4, 161]= 3.4, p=0.01, ηp2=0.08), while age, race, and education explained additional variance (F[9, 161]= 5.3 p<0.01, ηp2=.23). Including global cognition did not explain any additional or unique variance. However, when premorbid IQ was included in the model, group differences were no longer significant (added to the full model with age, sex, race, education, DRS, group: F[4,139] = 2.01, p = .10, ηp2 = .06, WTAR: F(1,139) = 1.71, p = .19, ηp2 = .01).
Additional sensitivity analyses and Correlations with the A-DMC subscales and clinical and cognitive variables are reported in the Supplemental material.
Exploratory analyses
We tested whether group differences in decision-making competence were explained by maladaptive personality traits, particularly impulsivity. Because participants reporting higher interpersonal ambivalence also displayed somewhat lower resistance to both sunk cost and framing (Supplementary eTable 1a), we included these variables in our analyses of group differences. After accounting for age, gender, race, and education, interpersonal ambivalence explained no additional variance in resistance to sunk cost (F[4,155]=1.56, p=0.21, ηp2=0.01), but predicted lower resistance to framing (F[4,155]=5.91, p=0.02, ηp2=0.04), with group differences remaining significant. Impulsivity (SPSI Impulsive/Careless subscale) did not explain additional unique variance in resistance to sunk costs or shared variance with group. Impulsivity explained a small proportion of variance in resistance to framing shared with group, but did not increase the total variance explained. Group differences remained significant. We performed additional analyses to account for depression severity. HAM-D 16 scores (without the suicide item) did not explain any additional variance in resistance to framing or in sunk cost (p>.61, ηp2 <.01) when added to the full model (age, sex, education, DRS, group, WTAR). In participants with major depression, lifetime history of substance use disorders did not explain any additional variance in resistance to framing (p=.54, ηp2 =.01), when added to the full model. It did predict lower resistance to sunk cost (F(2,91) = 3.58, p = .03, ηp2 = .07)), but significant group differences remained (F(3,91) = 3.13, p = .029, ηp2 = .09)).
DISCUSSION
We found significant group differences in overall decision-making competence. Subsequent analyses revealed that suicide attempters were more susceptible to framing effects than non-psychiatric controls, depressed non-suicidal individuals, and ideators, a difference partially explained by premorbid IQ. Low-lethality attempters were more susceptible to sunk cost than non-psychiatric controls, suicide ideators, and high-lethality attempters.
What are the psychological underpinnings of susceptibility to sunk cost? When compared to other decision-making abilities, resistance to sunk cost appears to rely less on fluid intelligence14. Rather, it is impaired in individuals prone to regret and rumination about losses52. Inability to resist sunk costs can be thought of as a form of entrapment53. To the extent that these group differences in the ability to resist sunk costs from the past can be generalized to the suicidal crisis, suicide attempters’ decisions may be driven by their stronger focus on painful past experiences.
We found that suicide attempters were susceptible to framing bias. The ability to resist framing effects is exemplified by giving the same response to a pair of equivalent prospects, e.g., one presented in a gain and another in a loss frame54. Suicide attempters were impaired on this cognitively demanding task. Susceptibility to framing effects was modestly correlated with age, global cognition, IQ, ambivalence in interpersonal relationships, and impulsive/careless social problem-solving style. Of these, only IQ partially explained the group differences in susceptibility to framing effects; results from large epidemiological studies demonstrate a relationship between IQ and death by suicide and suicide attempt55, 56. It is possible that the inability to conceptualize the problem at a higher abstract level inhibits the search for alternative solutions in a suicidal crisis.
Decision making is often thought of as a balance between deliberative and affective processes. From this perspective, diminished ability to resist sunk costs and framing effects may be particularly detrimental in the face of extreme affects57, propelling a suicidal crisis.
Our prediction that depressed participants’ would differentially recognize the extent of their knowledge compared to non-psychiatric controls was not supported. It is possible, however, that our measure of general knowledge was not sensitive enough to capture domain-specific misjudgment of confidence. For example, overconfidence has been related to perceived knowledge in gambling58 and substance use15 in samples characterized by those risky behaviors. Tasks that assess knowledge about depressive illness and/or self-efficacy may be more sensitive indicators of confidence misjudgment in depressed individuals than general knowledge questions.
Consistency in Risk Perception was relatively similar among the groups and modestly correlated with interpersonal aggression but not with cognitive abilities. Those who indicated higher interpersonal aggression perceived risk less consistently. Impulsive-aggressive traits are more pronounced among younger suicidal individuals34, who may show a greater impairment in this domain.
Our results resonate with the entrapment theory of suicide53, and the conceptualization of suicidal crisis as a state of entrapment and ruminative flooding59, indicating that the experience of entrapment may be shaped by an excessive focus on past losses and an inability to flexibly conceptualize one’s situations. Even more relevant to our results is Baumeister’s escape theory where death is sought to end “aversive […] awareness of one’s painful life situation.1” It is easy to see how excessive attention to sunk costs – irrecoverable losses – would contribute to such an aversive self-awareness.
We found that older people with a history of suicide attempts display heterogeneity in decision competence that somewhat mirrors the clinical presentation of the attempt. Decision-making abilities of suicide ideators, on the other hand, were more similar to that of non-suicidal depressed controls than to suicide attempters, suggesting that decision biases may operate at the final stage of the suicidal process, that of acting on suicidal ideas.
Our study is limited by a cross-sectional design. We focused on older adults with unipolar depression, as it is the most common antecedent of late-life suicide18, 60.Although we found group differences in decision-making competence, we were unable to directly study the application of decision-making competence during the suicidal crisis, which would be possible only with a prospective design.
It is also unclear to what extent our findings can be generalized to other populations. In addition, we were not able to explore potential life-span changes in decision-making skills.
Future research may take a more integrative perspective by examining how susceptibility to biases, such as those described here, relate to altered decisions and behavior in a suicidal crisis, and neural signals during decision-making and learning tasks, by looking specifically at the interaction between emotional states and decision-making outcomes in suicide attempters (e.g., Eldar & Niv, 201461).
In summary, attempted suicide appears to be associated with specific decision biases. Poor decisions can also result in an accumulation of financial, occupational, or interpersonal problems that in turn precipitate the suicidal crisis. Individual differences in decision-making competence may guide intervention. Decision-making competence can be improved62, offering a possible avenue for preventing the escalation of a suicidal crisis. One way to address this vulnerability in psychotherapy with suicidal individuals is mindfulness meditation, provided that these skills can be applied in a suicidal crisis. Mindfulness meditation has been shown to improve resistance to sunk-cost bias through decreased focus on past and future and decreased negative affect63. Another approach would be a modification of Cognitive Behavioral Therapy, which has been successfully used in suicidal patients64, specifically targeting the tendency to dwell on irrecoverable losses. While the role of framing effects in suicidal behavior is presently less clear, a case can be made for fostering a strategic approach to decisions in learning-based therapies.
Supplementary Material
CLINICAL POINTS.
People vulnerable to suicide make poor life decisions. Yet, we know little about their decision-making competence.
We found that suicide attempters are less likely to avoid common decision biases than control groups. Namely they lacked a flexible and critical mind to avoid the effect of framing and were excessively focused on past negative experiences. Improving decision competence could be a goal of psychotherapy with suicide attempters.
Acknowledgment
The authors would like to thank Natalie Truty, B.S., Laura Kenneally, B.S, and Jonathan Wilson, B.S. of the University of Pittsburgh Medical Center for their assistance in data collection as well as in the preparation of this manuscript.
Financial support provided by NIA K18 AG042166, NIMH R01 MH085651, MH100095, and K23 MH086620 (Bethesda, MD; USA), the American Foundation for Suicide Prevention (New York, New York; USA), and the European Union Seventh Framework Programme (FP7-People-2013-CIG-618522).
Footnotes
Data have not previously been presented.
The authors have nothing to disclose.
References
- 1.Baumeister RF. Suicide as Escape from Self. Psychol Rev. 1990 Jan;97(1):90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- 2.Ringel E. The presuicidal syndrome. Suicide Life Threat Behav. 1976;6(3):131–149. [PubMed] [Google Scholar]
- 3.Dostoevsky F. Crime and Punishment: The Russian Messenger. 1866 [Google Scholar]
- 4.Edwards W. The theory of decision making. Psychol Bull. 1954;51(4):380. doi: 10.1037/h0053870. [DOI] [PubMed] [Google Scholar]
- 5.Manning V, Koh PK, Yang Y, et al. Suicidal ideation and lifetime attempts in substance and gambling disorders. Psychiatry Research. doi: 10.1016/j.psychres.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 6.Dougherty DM, Mathias CW, Marsh DM, Moeller FG, Swann AC. Suicidal behaviors and drug abuse: impulsivity and its assessment. Drug Alcohol Depend. 2004;76(Supplement 1):S93–S105. doi: 10.1016/j.drugalcdep.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Gorlyn M, Keilp JG, Oquendo MA, Burke AK, Mann JJ. Iowa Gambling Task performance in currently depressed suicide attempters. Psychiatry research. 2013;207(3):150–157. doi: 10.1016/j.psychres.2013.01.030. [DOI] [PubMed] [Google Scholar]
- 8.Jollant F, Bellivier F, Leboyer M, et al. Impaired decision making in suicide attempters. Am J Psychiatry. 2005 Mar;162(2):304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- 9.Clark L, Dombrovski AY, Siegle GJ, et al. Impairment in risk-sensitive decision-making in older suicide attempters with depression. Psychol Aging. 2011;26(2):321–330. doi: 10.1037/a0021646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gibbs LM, Dombrovski AY, Morse J, Siegle GJ, Houck PR, Szanto K. When the solution is part of the problem: problem solving in elderly suicide attempters. Int J Geriatr Psychiatry. 2009 Dec;24(12):1396–1404. doi: 10.1002/gps.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D'Zurilla TJ, Chang EC, Nottingham EJt, Faccini L. Social problem-solving deficits and hopelessness, depression, and suicidal risk in college students and psychiatric inpatients. J Clin Psychol. 1998 Dec;54(8):1091–1107. doi: 10.1002/(sici)1097-4679(199812)54:8<1091::aid-jclp9>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 12.Arkes HR, Blumer C. The psychology of sunk cost. Organizational behavior and human decision processes. 1985;35(1):124–140. [Google Scholar]
- 13.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211(4481):453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- 14.Bruine de Bruin W, Fischhoff B, Parker A. Individual Differences in Adult Decision-Making Competence. J Pers Soc Psychol. 2007;92(5):938–956. doi: 10.1037/0022-3514.92.5.938. [DOI] [PubMed] [Google Scholar]
- 15.Parker AM, Fischhoff B. Decision-making competence: External validation through an individual-differences approach. J Behav Decis Making. 2005 Jan;18(1):1–27. [Google Scholar]
- 16.Centers for Disease Control and Prevention NCfIPaC. National Suicide Statistics At A Glance. [cited 2013 August 9];2012 May 11; 2012; Available from: http://www.cdc.gov/violenceprevention/suicide/statistics/aag.html#C.
- 17.De Leo D, Padoani W, Scocco P, et al. Attempted and completed suicide in older subjects: results from the WHO/EURO Multicentre Study of Suicidal Behaviour. Int J Geriatr Psychiatry. 2001 Mar;16(3):300–310. doi: 10.1002/gps.337. [DOI] [PubMed] [Google Scholar]
- 18.Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry. 1996 Aug;153(8):1001–1008. doi: 10.1176/ajp.153.8.1001. [DOI] [PubMed] [Google Scholar]
- 19.Waern M, Runeson BS, Allebeck P, et al. Mental disorder in elderly suicides: a case-control study. Am J Psychiatry. 2002 Mar;159(3):450–455. doi: 10.1176/appi.ajp.159.3.450. [DOI] [PubMed] [Google Scholar]
- 20.Leyton M, Paquette V, Gravel P, et al. alpha-[11C]Methyl-L-tryptophan trapping in the orbital and ventral medial prefrontal cortex of suicide attempters. Eur Neuropsychopharmacol. 2006 Apr;16(3):220–223. doi: 10.1016/j.euroneuro.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Oquendo MA, Placidi GP, Malone KM, et al. Positron emission tomography of regional brain metabolic responses to a serotonergic challenge and lethality of suicide attempts in major depression. Arch Gen Psychiatry. 2003 Jan;60(1):14–22. doi: 10.1001/archpsyc.60.1.14. [DOI] [PubMed] [Google Scholar]
- 22.Dombrovski AY, Szanto K, Siegle GJ, et al. Lethal Forethought: Delayed Reward Discounting Differentiates High- and Low-Lethality Suicide Attempts in Old Age. Biol Psychiatry. 2011;70(2):138–144. doi: 10.1016/j.biopsych.2010.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richard-Devantoy S, Annweiler C, Beauchet O, Camus V, Le Gall D, Garre JB. P03-470 - Cognitive inhibition in suicidal depressed elderly. European Psychiatry. 2011;26(1):1640. doi: 10.4088/JCP.10l06797. 2011. [DOI] [PubMed] [Google Scholar]
- 24.Keilp JG, Sackeim HA, Brodsky BS, Oquendo MA, Malone KM, Mann JJ. Neuropsychological dysfunction in depressed suicide attempters. Am J Psychiatry. 2001;158(5):735–741. doi: 10.1176/appi.ajp.158.5.735. [DOI] [PubMed] [Google Scholar]
- 25.McGirr A, Dombrovski AY, Butters M, Clark L, Szanto K. Deterministic learning and attempted suicide among older depressed individuals: Cognitive assessment using the Wisconsin Card Sorting Task. J Psychiatr Res. 2012 Feb;46(2):226–232. doi: 10.1016/j.jpsychires.2011.10.001. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Szanto K, Clark L, Hallquist M, Vanyukov P, Crockett M, Dombrovski A. The cost of social punishment and high-lethality suicide attempts. Psychol Aging. 2014 Mar;29(1):84–94. doi: 10.1037/a0035339. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brockner J, Rubin JZ. Entrapment in escalating conflicts: A social psychological analysis. New York: Springer-Verlag; 1985. [Google Scholar]
- 28.Coleman MD. Sunk cost, emotion, and commitment to education. Current Psychology. 2010;29(4):346–356. [Google Scholar]
- 29.Moon H, Hollenbeck JR, Humphrey SE, Maue B. The tripartite model of neuroticism and the suppression of depression and anxiety within an escalation of commitment dilemma. J Pers. 2003;71(3):347–368. doi: 10.1111/1467-6494.7103004. [DOI] [PubMed] [Google Scholar]
- 30.Keilp JG, Sackeim HA, Mann JJ. Correlates of trait impulsiveness in performance measures and neuropsychological tests. Psychiatry Res. 2005 Jun 30;135(3):191–201. doi: 10.1016/j.psychres.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 31.Richard-Devantoy S, Berlim M, Jollant F. A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychol Med. 2013:1–11. doi: 10.1017/S0033291713002304. [DOI] [PubMed] [Google Scholar]
- 32.Gujral S, Dombrovski AY, Butters M, Clark L, Reynolds CF, 3rd, Szanto K. Impaired Executive Function in Contemplated and Attempted Suicide in Late Life. Am J Geriatr Psychiatry. 2013 Feb 6; doi: 10.1016/j.jagp.2013.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alloy LB, Abramson LY. Cognitive processes in depression. 1 Jan 1988 ed. New York, NY: Guilford Press (New York, NY, US); 1988. Depressive realism: Four theoretical perspectives; pp. 223–265. [Google Scholar]
- 34.McGirr A, Renaud J, Bureau A, Seguin M, Lesage A, Turecki G. Impulsive-aggressive behaviours and completed suicide across the life cycle: a predisposition for younger age of suicide. Psychol Med. 2008 Mar;38(3):407–417. doi: 10.1017/S0033291707001419. [DOI] [PubMed] [Google Scholar]
- 35.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999 Feb;156(2):181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 36.Larrick RP, Nisbett RE, Morgan JN. Who uses the cost-benefit rules of choice? Implications for the normative status of microeconomic theory. Organizational Behavior and Human Decision Processes. 1993;56(3):331–347. [Google Scholar]
- 37.Stanovich KE. Who is rational?: Studies of individual differences in reasoning. Psychology Press; 1999. [Google Scholar]
- 38.Baud P. Personality traits as intermediary phenotypes in suicidal behavior: Genetic issues. American Journal of Medical Genetics Part C: Seminars in Medical Genetics. 2005;133C(1):34–42. doi: 10.1002/ajmg.c.30044. [DOI] [PubMed] [Google Scholar]
- 39.Soane E, Chmiel N. Are risk preferences consistent?: The influence of decision domain and personality. Personality and Individual Differences. 2005;38(8):1781–1791. [Google Scholar]
- 40.Lauriola M, Russo PM, Lucidi F, Violani C, Levin IP. The role of personality in positively and negatively framed risky health decisions. Personality and individual differences. 2005;38(1):45–59. [Google Scholar]
- 41.Beck AT, Beck R, Kovacs M. Classification of suicidal behaviors: I. Quantifying intent and medical lethality. Am J Psychiatry. 1975 Mar;132(3):285–287. doi: 10.1176/ajp.132.3.285. [DOI] [PubMed] [Google Scholar]
- 42.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979 Apr;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 43.First MS, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I Disorders - Patient Edition (SCID-I/P) Version 2.0. 1995 [Google Scholar]
- 44.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960 Feb;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 46.Mattis S. Psychological Assessment Resources. Odessa, FL: 1988. Dementia Rating Scale (DRS): Professional Manual. [Google Scholar]
- 47.Wechsler D. The Wechsler Test of Adult Reading: WTAR. San Antonio: Psychological Corporation; 2001. [Google Scholar]
- 48.D'Zurilla TJ, Nezu AM. Development and preliminary evaluation of the Social Problem-Solving Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1990;2(2):156–163. [Google Scholar]
- 49.Horowitz LM, Rosenberg SE, Baer BA, Ureño G, Villaseñor VS. Inventory of interpersonal problems: Psychometric properties and clinical applications. J Consult ClinPsychol. 1988 Dec;56(6):885–892. doi: 10.1037//0022-006x.56.6.885. 1988. [DOI] [PubMed] [Google Scholar]
- 50.Pilkonis PA, Kim Y, Proietti JM, Barkham M. Scales for personality disorders developed from the Inventory of Interpersonal Problems. J Personal Disord. 1996;10(4):355–369. [Google Scholar]
- 51.Parker AM, Stone ER. Identifying the effects of unjustified confidence versus overconfidence: Lessons learned from two analytic methods. J Behav Decis Making. 2014;27(2):134–145. doi: 10.1002/bdm.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.van Putten M, Zeelenberg M, van Dijk E. Who throws good money after bad? Action vs. state orientation moderates the sunk cost fallacy. Judgment and Decision Making. 2010;5(1):33–36. [Google Scholar]
- 53.Williams JMG, Crane C, Barnhofer T, Duggan D. Psychology and suicidal behaviour: elaborating the entrapment model. In: Hawton K, editor. Prevention and Treatment of Suicidal Behaviour: From Science to Practice. 1 ed. USA: Oxford University Press; 2005. pp. 71–89. [Google Scholar]
- 54.Levin IP, Gaeth GJ, Schreiber J, Lauriola M. A new look at framing effects: Distribution of effect sizes, individual differences, and independence of types of effects. Organizational Behavior and Human Decision Processes. 2002;88(1):411–429. [Google Scholar]
- 55.Andersson L, Allebeck P, Gustafsson JE, Gunnell D. Association of IQ scores and school achievement with suicide in a 40-year follow-up of a Swedish cohort. Acta Psychiatrica Scandinavica. 2008;118(2):99–105. doi: 10.1111/j.1600-0447.2008.01171.x. [DOI] [PubMed] [Google Scholar]
- 56.Gunnell D, Löfving S, Gustafsson JE, Allebeck P. School performance and risk of suicide in early adulthood: Follow-up of two national cohorts of Swedish schoolchildren. J Affect Disord. 2011;131(1–3):104–112. doi: 10.1016/j.jad.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 57.Peters E, Hess TM, Västfjäll D, Auman C. Adult age differences in dual information processes: Implications for the role of affective and deliberative processes in older adults' decision making. Perspectives on Psychological Science. 2007;2(1):1–23. doi: 10.1111/j.1745-6916.2007.00025.x. [DOI] [PubMed] [Google Scholar]
- 58.Goodie AS. The role of perceived control and overconfidence in pathological gambling. Journal of Gambling Studies. 2005;21(4):481–502. doi: 10.1007/s10899-005-5559-1. [DOI] [PubMed] [Google Scholar]
- 59.Yaseen ZS, Gilmer E, Modi J, Cohen LJ, Galynker II. Emergency Room Validation of the Revised Suicide Trigger Scale (STS-3): A Measure of a Hypothesized Suicide Trigger State. PLoS ONE. 2012;7(9) doi: 10.1371/journal.pone.0045157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52(3):193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- 61.Eldar E, Niv Y. Interaction between emotional state and learning underlies mood instability. Nature communications. 2015;6 doi: 10.1038/ncomms7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jacobson D, Parker A, Spetzler C, et al. Improved Learning in US History and Decision Competence with Decision-Focused Curriculum. PloS one. 2012;7(9):e45775. doi: 10.1371/journal.pone.0045775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hafenbrack AC, Kinias Z, Barsade SG. Debiasing the Mind Through Meditation Mindfulness and the Sunk-Cost Bias. Psychological Science. 2014;25(2):369–376. doi: 10.1177/0956797613503853. [DOI] [PubMed] [Google Scholar]
- 64.Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.