Abstract
Background
Attention bias towards threat is associated with anxiety in older youth and adults and has been linked with violence exposure. Attention bias may moderate the relationship between violence exposure and anxiety in young children. Capitalizing on measurement advances, the current study examines these relationships at a younger age than previously possible.
Methods
Young children (mean age 4.7, ±0.8) from a cross-sectional sample oversampled for violence exposure (N = 218) completed the dot-probe task to assess their attention biases. Observed fear/anxiety was characterized with a novel observational paradigm, the Anxiety Diagnostic Observation Schedule. Mother-reported symptoms were assessed with the Preschool-Age Psychiatric Assessment and Trauma Symptom Checklist for Young Children. Violence exposure was characterized with dimensional scores reflecting probability of membership in two classes derived via latent class analysis from the Conflict Tactics Scales: Abuse and Harsh Parenting.
Results
Family violence predicted greater child anxiety and trauma symptoms. Attention bias moderated the relationship between violence and anxiety.
Conclusions
Attention bias towards threat may strengthen the effects of family violence on the development of anxiety, with potentially cascading effects across childhood. Such associations may be most readily detected when using observational measures of childhood anxiety.
Keywords: attention bias, violence, harsh parenting, early childhood, anxiety, fear
Introduction
Although young children’s exposure to family violence may profoundly affect their mental health (Bayer et al., 2011; Ferguson, 2013; Shonkoff, 2011), only a subset of children exposed to violence or trauma develops problems. Studies of older children and adults have shown that those who devote disproportionate attention orienting or ‘attention biases’ towards potential threats are at increased risk for anxiety and post-traumatic stress symptoms (Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & van, 2007; Pine, 2007). New approaches to treatment involving retraining of attention biases show promise for reducing anxiety and underscore the importance of understanding the how attention bias may influence the development of anxiety (Bar-Haim, Morag, & Glickman, 2011; Shechner et al., 2012). Young, violence-exposed children with anxiety may exhibit attention biases. However, virtually no research examines associations between attention bias and anxiety before school-age (Bar-Haim et al., 2007; Perez-Edgar et al., 2011; Shechner et al., 2012), even though anxiety often emerges in this developmental period (Egger & Angold, 2006). While there are many forms of traumatic exposure, violence is a promising focus for initial investigation due to its prevalence in families with young children (Ferguson, 2013). The current study investigates the relationships among family violence, attention bias to threat, and anxiety in a community-based sample of preschool-age children, oversampled for family violence.
Measurement advances have led to research on the prevalence of impairing anxiety in young children (Egger & Angold, 2006) and studies that have documented increased risk for anxiety and trauma-related symptoms in young children who have experienced family violence (Briggs-Gowan et al., 2010; Ferguson, 2013; Levendosky, Bogat, & Martinez-Torteya, 2013). Typically, individuals show rapid, reflexive, early orienting towards extreme threats (LeDoux, 2000). However, some individuals devote disproportionate attention to milder threats, such as mere pictures of angry faces, and the term ‘attention bias’ refers to this tendency (Bar-Haim et al., 2007). Attention bias can be thought of as excessive vigilance toward threats and may be assessed by standard attention-capture paradigms, such as the dot-probe task (Shechner et al., 2012). Attention bias towards threat is commonly associated with a range of childhood anxiety disorders (Bar-Haim et al., 2007; Perez-Edgar et al., 2011; Waters, Henry, Mogg, Bradley, & Pine, 2010). It also has been linked with PTSD in adults and children (Bar-Haim et al., 2007; Moradi, Neshat-Doost, Teghavi, Yule, & Dalgleish, 1999; Pine et al., 2005; Swartz, Graham-Bermann, Mogg, Bradley, & Monk, 2011). Such biases towards threat may increase the perception of the environment as dangerous, serving to maintain, amplify, or promote anxiety (Bar-Haim et al., 2007). If they manifest in young children exposed to family violence, these biases could amplify risk for developing anxiety and post-traumatic stress symptoms.
Pollak and others have documented disruptions in processing of emotion, especially anger, among children exposed to adversity (Pollak, 2008, 2012). In adverse family environments, attention bias towards threat may serve an adaptive survival function by quickly alerting children to signs of possible danger, while also elevating their risk for anxiety (Pollak, 2012). Attention biases have been identified in a few existing studies of children who have experienced family violence (Pine et al., 2005; Shackman, Shackman, & Pollak, 2007; Swartz et al., 2011) or negative, harsh parenting (Gulley, Oppenheimer, & Hankin, 2014). One such study found that the relationship between family violence and children’s anxiety was stronger at higher levels of attention bias (Gulley et al., 2014). In general, such studies have focused on extreme exposure (e.g. substantiated physical abuse) and thus, the threshold is unclear at which violence exposure is linked to attention biases.
Studying anxiety in young children exposed to violence presents particular challenges. Because fears and anxieties are common in early childhood (Spence, Rapee, McDonald, & Ingram, 2001), studies must distinguish normative variation from clinically-concerning anxiety (Wakschlag et al., 2008). In addition, while parental reports are an essential source of information, such reports can be biased, particularly when parents are coping with their own trauma exposure (Kassam-Adams, Garcia-Espana, Miller, & Winston, 2006). In other areas of psychopathology, ratings during standardized clinical observations have demonstrated incremental utility over parent reports for early detection (Wakschlag et al., 2008). The current study uses such ratings in a novel paradigm designed to elicit fear and anxiety in the context of parent-child interactions (Briggs-Gowan, Mian, Carter, & Wakschlag, 2011).
We investigate attention bias as a possible mechanism in developmental pathways to anxiety in young children exposed to family violence. We hypothesize that exposure to family violence relates to both anxiety (Hypothesis 1) and attention bias towards threat in young children (Hypothesis 2). We further hypothesize that attention bias toward threat correlates with anxiety (Hypothesis 3) and amplifies the relationship between violence exposure and anxiety (Hypothesis 4).
Method
Participants
Participants were part of an Intensive Sub-study sample of 497 that was originally drawn via a stratified random sampling plan from a survey sample of 1,857 3–5-year-olds recruited from pediatric practices (Nichols et al., In press; Wakschlag et al., 2014). See online supplementary Figure S1 for sampling and participation details. The subsample was restricted to children without significant delays or neurodevelopmental conditions and their English-speaking, biological mothers. We oversampled children with (a) disruptive behavior (DB) above the 80th percentile on the Multidimensional Assessment Profile of Disruptive Behavior (Wakschlag et al., 2014) and (b) children of mothers who reported past-year intimate partner violence (IPV) so that these children could be followed up for a larger study of developmental risk. The analytic sample for this paper includes 218 children who met all eligibility criteria for the Intensive Sub-study, participated in the second of two laboratory visits when the dot-probe was administered, and had usable data for the dot-probe and key mother-reported variables (please see SuppFig1). Children younger than 4 years were excluded because they generally could not provide usable data; only one study has reported findings from the dot-probe with children as young as 4 years (Swartz et al., 2011). These 218 represent 69.4% of children (n=314) who attended at least one laboratory visit, were 4+ years of age, and met eligibility criteria. Compared with the original survey sample, these 218 were similar in sex, race/ethnicity, single parenting and poverty, p > .05, but as expected by design higher in DB and IPV (p < .05) (SuppFig1). These children were comparable to the remainder of the Intensive sample on all variables.
Children were 48–84 months old (48% 4-year-olds, 41% 5-year-olds, 11% 6-year-olds+). They were ethnically diverse (47% African American/Black, 32% Hispanic, 20% non-Hispanic White, 2% Other) and evenly distributed in sex (49% boys). Forty-eight percent lived in poverty and 36% of children lived in single parent homes. Employing methods described in the Measures, 10% experienced probable abuse, 58% harsh parenting, and 32% non-harsh parenting. Average non-verbal reasoning on the Differential Abilities Scale was 101.7 (Standard Deviation (SD) = 17.51).
Procedures
Participants attended two three-hour laboratory visits. Mothers were compensated for participation and transportation. Study protocols were approved by institutional review boards. Mandated procedures for reporting suspected abuse, neglect and imminent harm were followed. Mothers provided informed consent. Staff monitored children for fatigue and distress, provided breaks, and discontinued assessments when appropriate.
Measures
Attention Bias
The computerized affective dot-probe task was administered to children. Each trial began with the presentation of a 500-ms central fixation cross. This was followed by the 500-ms presentation of a pair of faces (NimStim, Face Stimulus Set) that appeared to the right and left side of the fixation cross, centered at +/−4.1° of horizontal visual angle eccentricity from the cross. Face pairs were photographs of emotional expressions of the same person (Angry-Neutral, Happy-Neutral, Neutral-Neutral). The task is depicted in Figure S2. Inclusion of happy faces offered a test of the specificity of any observed biases to threatening stimuli. The location (left/right) for each type of emotional stimulus was counterbalanced. Immediately after the face-pair a target (coin) appeared on the left or right side of the screen. Children were told that the [point of the game was to catch as many coins as quickly as they could] and that they [would get a prize for doing a good job]. Using a button box, they were asked to indicate as quickly and accurately as possible with their left or right index finger the side on which the coin appeared. They were told that they would also see faces, but that the game was about catching the coins. The coin remained on the screen until a button was pressed. Every 90 trials, children were given a break during which they ‘earned’ gold coins to place in a piggybank. All children received prizes. There were 10 practice trials with the possibility of repeating the practice block twice. Administration was discontinued if 70% accuracy was not reached in the practice. Bias scores were calculated as the difference between reaction times (RTs) for incongruent (coin appeared on the same side as the neutral face) and congruent (coin appeared on the same side as the emotion), such that positive bias was towards the emotion and negative was towards the neutral face.
Children completed either the standard 180 trial dot-probe (72 Angry/Neutral, 72 Happy/Neutral, 36 Neutral/Neutral trials) or an extended 360 trial version (144 Angry/Neutral, 144 Happy/Neutral, 72 Neutral/Neutral). Children who completed the long version did so as part of an event-related potential study; data are not included here because only a subset yielded usable data (n = 151). Task version was a covariate in all models. There were no differences in accuracy, RTs, or bias scores between the two versions, t(1,216) = 0.44–1.52, ns, or when the two halves of the long version were compared, t(1,148) = 0.08–0.48, ns.
Incorrect responses may occur due to extraneous factors (e.g., inattention, incomplete viewing of stimuli, or temporary lapse of task understanding) or could occur if children with particularly strong biases press the button on the wrong side. As it is impossible to determine the reason for such errors, we followed the standard approach used in the field by removing incorrect trials (Pine et al., 2005). RTs were removed for trials that were <200 ms, >7000 ms, or >2.5 SD from the individual child’s MN RT across conditions. Data were not used if there were fewer than 9 RTs per emotion condition or accuracy was below 65% (n = 34). Review for outliers (+/−3.5 SD from the sample mean) identified one outlier on 3 emotion conditions; child was excluded. Two outliers on angry bias and 1 on happy bias were reined in by assigning values at 3.5 SD from the mean. Analytic models employed continuous bias scores and tertile groupings (Toward, No/Low Bias, Away); consistent with previous studies (Perez-Edgar et al., 2011). Please see Table 1 for descriptive statistics.
Table 1.
Descriptive Statistics
| N | MN | STD | |
|---|---|---|---|
| Dot-probe | |||
| Accuracy | 218 | 90.9% | (8.1%) |
| Neutral RT | 218 | 1068.4 | (355.0) |
| Angry RT | 218 | 1061.7 | (333.6) |
| Happy RT | 218 | 1052.6 | (340.4) |
| Angry Bias | 218 | −6.8 | (110.3) |
| Happy Bias | 218 | −1.5 | (109.4) |
| Angry Bias Tertiles | |||
| Away | 71 | −118.3 | 95.4 |
| No/Low | 73 | −1.4 | 16.1 |
| Towards | 74 | 94.7 | 68.0 |
| Happy Bias Tertiles | |||
| Away | 72 | −110.8 | 88.9 |
| No/Low | 72 | 1.7 | 14.9 |
| Towards | 74 | 101.8 | 71.3 |
| Symptoms | |||
| TSCYC | |||
| Total Trauma | 149 | 56.9 | (14.3) |
| Dissociation | 151 | 53.7 | (12.5) |
| PAPA | |||
| Specific Phobia Responses | 218 | 0.3 | (0.3) |
| Fear (Social, Separation, Panic, Agoraphobia) | 218 | 1.5 | (1.7) |
| GAD | 218 | 1.6 | (1.4) |
| Depression/Dysthymia | 218 | 1.6 | (1.5) |
| Anx-DOS (Observed) | |||
| Fear/Anxiety Composite | 201 | 3.4 | (3.1) |
Child-directed Violence
Mothers completed a modified Conflict Tactics Scales Parent-Child (Straus, Hamby, Finkelhor, Moore, & Runyan, 1998) about their behavior and their partner’s behavior toward the child in the context of parenting over the child’s lifetime. Items reflecting severe physical abuse (e.g., burning) were excluded because they are rarely endorsed and can result in under-reporting. Posterior probabilities (PP) for Probable Abuse and Harsh Parenting were derived from a latent class analysis (LCA) of these items (Grasso, Briggs-Gowan, Henry, & Wakschlag, 2014). PPs are continuous dimensional scores that reflect the probability that a child falls in a given class. PPs were used to better differentiate statistically between severe and milder forms of aggression relative to traditional subscale scores, which treat items as equivalent regardless of severity. The LCA used dichotomous items indicating behavior displayed by one or both parent. A 3-class solution was the best fit for the data, log-likelihood=−2102, Bayesian Information Criterion (BIC)=4438, Lo-Mendell-Rubin adjusted likelihood ratio compared with a 2-class model, p<.01. The three groups identified were: Probable Abuse, which had high probability of exposure to mild to severe forms of verbal and physical violence, including a number of severely violent behaviors (e.g., hit with a fist or object, kicked); Harsh (but not abusive) Parenting, which had high probability of exposure to harsh parenting (e.g., spanking, threatening to spank), but low probability of severe physical violence; and Low, which had low probability of exposure to all behaviors except shouted at child. PPs for Probable Abuse and Harsh Parenting were used.
Intimate Partner Violence
Intimate partner violence (IPV) was assessed with mothers’ reports on 15 items from the partner version of the Conflict Tactics Scale (Straus, Hamby, Boney-McCoy, & Sugarman, 1996). Severe behaviors (e.g., sexual assault) were excluded, as described above. An LCA of these items identified a 3-class solution, log-likelihood=−2043, BIC=4368, Lo-Mendell-Rubin adjusted likelihood ratio compared to the 2-class model, p<.01 (Grasso et al., 2014). Identified groups included: High IPV, with high probability of a range of mild to severe verbal and physical violence; Moderate IPV, with high probability of exposure to non-physical and verbal violence, but low probability of exposure to physical violence; and Low IPV, with low probability (<0.5) of exposure to all indicators. PPs for high and moderate IPV were used.
Child Anxiety
The protocol provided developmentally-sensitive assessment of a full range of anxiety and trauma-related symptoms. These were assessed by developmentally-appropriate mother-report tools, the Preschool Age Psychiatric Assessment (PAPA) (Egger et al., 2006) and Trauma Symptom Checklist for Young Children (TSCYC) (Briere et al., 2001), and by a novel developmentally-sensitive direct observation, clinical paradigm, the Anxiety Diagnostic Observation Schedule (Anx-DOS) (Briggs-Gowan et al., 2011).
The PAPA, a DSM-IV-based semi-structured diagnostic interview for 2- to 5-year-olds, was administered by trained research assistants. Reliability of administration and scoring was monitored for 20% of interviews by an expert clinical psychologist (Percent Agreement = 81%-98%). Data were reduced by grouping ‘internalizing’ symptoms along fear and distress lines (Clark & Watson, 2006). A fear composite score was calculated as the mean of social phobia, separation, agoraphobia, and panic symptom criteria. As specific phobias have limited symptom criteria to contribute to such a composite, mean avoidance reaction across multiple phobia types was analyzed separately. Distress was assessed with symptom totals for generalized anxiety and depression/dysthymia; a composite variable was not created given our specific interest in anxiety. The PTSD section was administered. However, as in another of our studies (Briggs-Gowan et al., 2010), rates were too low to include in analyses, perhaps because PTSD symptoms are queried only if the respondent reports that an event caused a change in the child.
The Total and Dissociation Scales of the TSCYC were used. The total score is the summary of Arousal, Avoidance, and Intrusion scales (Cronbach α = 0.71–0.81). TSCYC data are available for a subset because it was added late due to concern about under-identification of PTSD by the PAPA.
Children and their mothers were observed during the Anx-DOS, a direct observation paradigm that uses two ‘presses’ to elicit clinically-salient behaviors. The presses were a remote-controlled tarantula, operated by the examiner in another room, which children are instructed to touch, and an opaque mystery jar that children were instructed to reach into to get a prize. The Anx-DOS is similar to traditional behavioral inhibition paradigms in assessing fearful and anxious/distressed behaviors via direct observation. However, behavioral inhibition paradigms typically utilize event-based coding (e.g. latency to touch) and focus on the occurrence of a behavior per se (e.g., Perez-Edgar et al., 2011). In contrast, consistent with other diagnostic observation systems (Lord et al., 1989; Wakschlag et al., 2008), the Anx-DOS utilizes global coding to capture qualitative differences in defining features of the clinical phenotype of anxious behavior in a developmentally-sensitive manner, assessing emotional expressions and behaviors along a clinical continuum from normal to atypical (0: no evidence; 1: mild/normative; 2: of concern; 3: atypical). Independent coders rated physical avoidance of the press, emotional expressions of fear/arousal, and exaggerated startle. A fear/anxiety composite score, calculated by summing these three codes, had strong internal consistency (α = .84) and inter-rater reliability (MN Intraclass r = .86). Composite scores >7 require multiple clinically-concerning codes and are considered ‘clinical.’ Data for 17 children were uncodable due to technical or administration errors.
Developmental Level
The Differential Ability Scales-Second Edition (DAS-II) (Elliott, 1983) Picture Similarities subscale provided a measure of developmental level.
Analytic Approach
Multiple linear regression and analysis of covariance (ANCOVA) models were examined with PROC SURVEYREG in SAS 9.0. All models included child age, sex, race/ethnicity, task version, and developmental level as covariates. The first set of linear regressions tested whether family violence (posterior probabilities for Probable Abuse and Harsh Parenting) was related to child anxiety (Hypothesis 1). The second set of linear regressions tested whether family violence was associated with attention bias towards threat (angry faces) (Hypothesis 2). The third analysis employed a series of ANCOVAs to test whether child anxiety was associated with attention bias towards angry faces, with children grouped across bias tertiles according to their relative bias scores: children with relative Bias Away from angry faces; children with No/Low Bias; and children with relative Bias Towards angry faces (Hypothesis 3); to be consistent with Hypothesis 4, bias was the independent variable. Finally, the hypothesis that attention bias towards threat would moderate the relationship between violence and anxiety was tested with interaction effects in linear regressions (Hypothesis 4). To evaluate the specificity of attention biases to angry faces, these analyses were repeated for biases related to happy faces. All analyses also were repeated with IPV variables as independent variables. Model estimation procedures accounted for the complex stratified sampling design. The survey design-based estimator (available in SAS) employed in these analyses accounts for the stratification and unequal probabilities of selection in the sample design. All analyses employed sampling weights that account for both unequal probabilities of selection and differential non-response rates.
Results
Family violence will be associated with anxiety (Hypothesis 1)
Family violence was associated with child anxiety (Table 2). The term ‘probable abuse’ was used to indicate exposure to all forms of aggression including severe behaviors (e.g., hitting/kicking, threatening to send the child away); probable abuse was associated with mothers’ reports of children’s specific phobias, distress and trauma symptoms, but not their reports of other fear symptoms or observed fear/anxiety on the Anx-DOS. In contrast, harsh parenting reflected more moderate violence (e.g., spanking, yelling) than probable abuse. Harsh parenting correlated significantly with specific phobias and depression/dysthymia symptoms. Moderate and high IPV were not associated with any symptom measure, B=−.06−.15, ns, except for TSCYC Dissociation (B=.19 and .24, p<.05, respectively).
Table 2.
Associations between violence and child anxiety/distress
| Mother-reported Symptoms | Observed | ||||||
|---|---|---|---|---|---|---|---|
| PAPA Fear | PAPA Distress | TSCYC | Anx-DOS | ||||
| Specific Phobias |
Other Fears |
GAD | Dep/Dys | Total Score |
Dissociation | Fear/Anxiety | |
| Harsh Parenting1 |
0.24** | 0.16 | 0.04 | 0.20** | 0.18 | 0.14 | 0.13 |
| Probable Abuse1 |
0.15* | 0.07 | 0.22* | 0.20** | 0.20* | 0.24* | 0.15 |
Note. Values are standardized Β from regressions representing exposure-symptom relationships after controlling for covariates. These are interpreted similar to correlation coefficients.
LCA posterior probability score.
p<.05,
p<.01
Family violence will be associated with attention bias towards threat (Hypothesis 2)
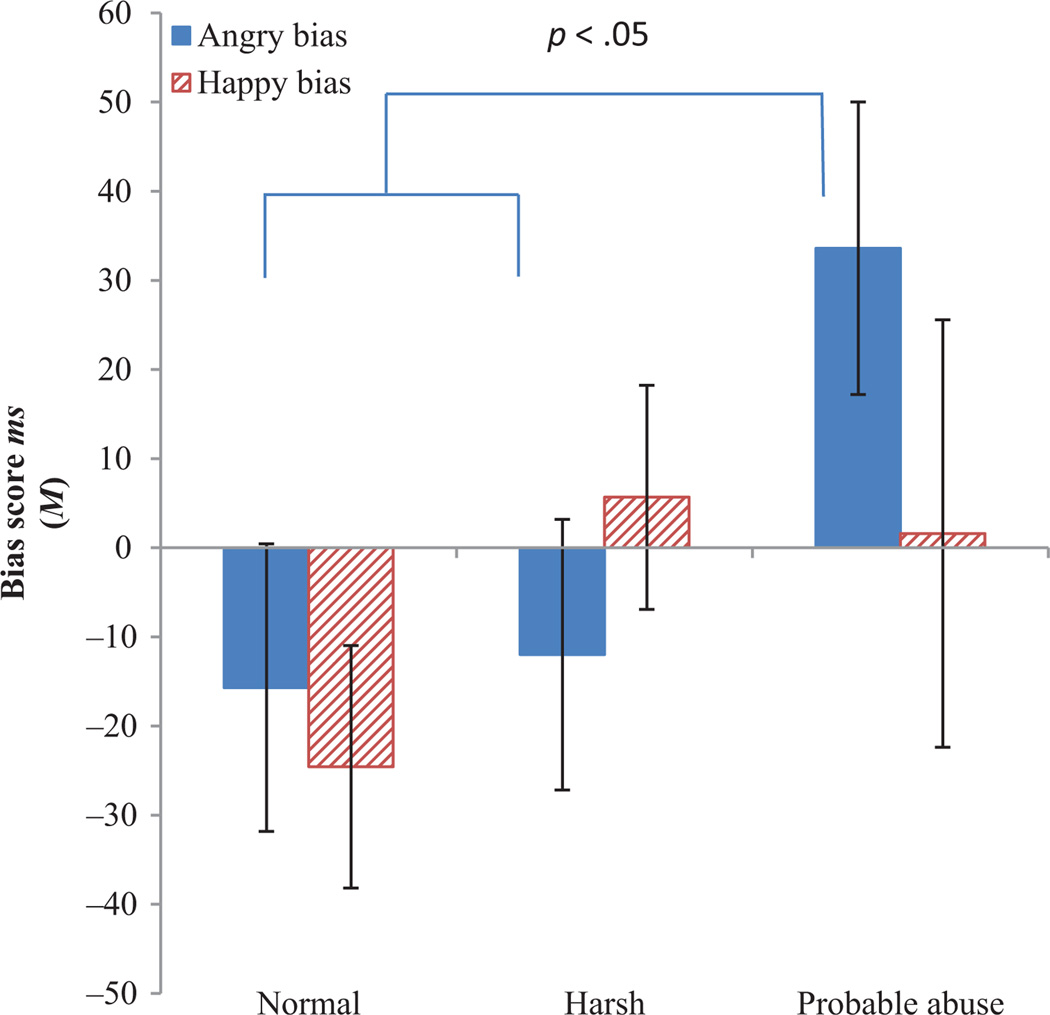
A linear regression predicting continuous bias scores indicated that Abuse was positively associated with attention bias towards angry/threat faces (Table 3). To better illustrate this association, we also used ANCOVA to test for differences in angry bias across the Probable Abuse, Harsh Parenting, and Non-harsh LCA groups. There was a significant main effect of group (p < .05) and a significant planned contrast effect indicating greater angry bias in the Abuse group relative to the other groups combined (p < .05) (see Figure 1). Pairwise comparisons between the Abuse group and each of the other groups were non-significant after Bonferroni correction (p < .10). Angry bias was not associated with moderate (B = .04) or high IPV (B=.12, p < .06). However, high IPV was associated with bias toward happy faces, B = .23, p < .01.
Table 3.
Family violence and attention bias
| Prediction of Bias Towards Angry | Prediction of Bias Towards Happy | |||||
|---|---|---|---|---|---|---|
| Std. Est. | Std. Error | F | Std. Est. | Std. Error | F | |
| Age | −0.16 | 1.15 | 3.69 | 0.14 | 1.43 | 1.46 |
| Sex | −0.01 | 21.22 | 0.03 | −0.12 | 17.23 | 2.26 |
| Race | −0.19 | 6.28 | 3.04 | 0.03 | 5.03 | 0.10 |
| Version | 0.07 | 23.84 | 0.46 | −0.04 | 20.24 | 0.20 |
| Non-verbal reasoning | 0.20 | 0.69 | 4.08* | −0.09 | 0.67 | 0.69 |
| Harsh Parenting1 | 0.04 | 24.44 | 0.16 | 0.14 | 20.96 | 2.58 |
| Probable Abuse1 | 0.12 | 24.33 | 4.96* | 0.09 | 29.31 | 1.38 |
LCA posterior probability score.
p<.05
Figure 1.
Attention bias towards threat and probable abuse. ANCOVA indicated a main effect of group for angry bias, F (2,218) = 3.15, P < .05. A planned contrast test indicated greater bias in the Abuse group compared with the Normal and Harsh groups, F(1,218) = 6.25, P < .05. There were no effects for happy bias
Attention bias towards threat will be associated with anxiety (Hypothesis 3)
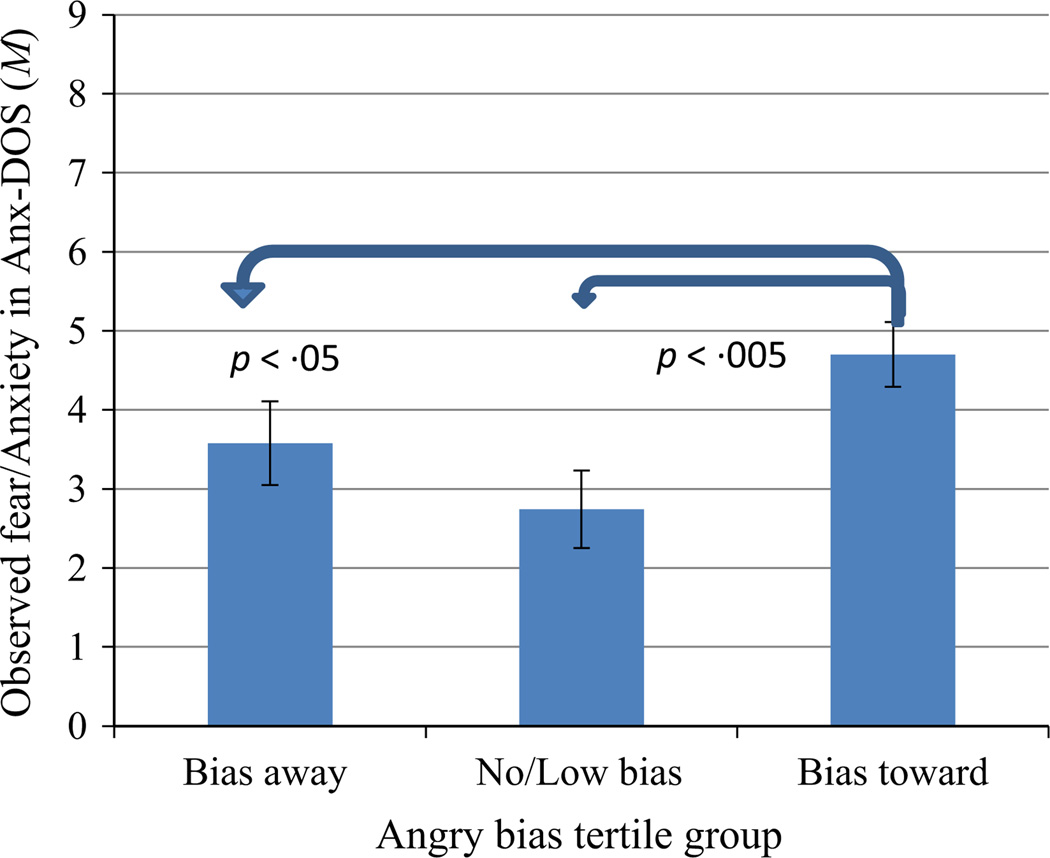
The relationship between child anxiety and attention bias was examined in a series of ANCOVAs that tested for differences in anxiety across the bias tertile groups. These groups were based on children’s relative positions on the angry bias distribution (Bias Away, Bias Towards, or No/Low Bias). The ANCOVAs for mothers’ reports of child anxiety indicated no significant effects of bias group, although the specific phobia model was in the expected direction, F(2,218) = 3.00, p < .10. In contrast, there was a significant main effect of angry bias on observed fear/anxiety in the Anx-DOS (p < .002) and higher anxiety in the Bias Towards group than the Bias Away (p < .05) and No/Low Bias (p<.005) groups (Figure 2). (A linear regression employing continuous bias scores revealed the same pattern).
Figure 2.
Attention bias towards threat and observed fear/anxiety. ANCOVA indicated a significant effect of angry bias group on observed fear/anxiety in the Anx-DOS, F(2,201) = 6.35, P < .002. Bonferroni-adjusted pairwise comparisons indicated greater fear/anxiety in children with relative Bias Towards threat compared with those with No/Low Bias (P < .005) or Bias Away from threat (P < .05)
For a clinical perspective, an Ad Hoc test revealed that Anx-DOS scores were in the clinical range in 27% of the Bias Towards group and 13% of remaining children, Rao-Scott X2 = 11.12, p < .005. Happy bias was not related to anxiety.
Attention bias moderates associations between violence and anxiety (Hypothesis 4)
Angry bias statistically moderated the relationship between Abuse and observed fear/anxiety. The first step of a linear regression included continuous scores for angry bias, Harsh Parenting, and Probable Abuse. Only angry bias was associated with observed anxiety, Fangrybias(1,201) = 5.15, p < .03; Fabuse(1,201) = 2.09, ns, Fharsh(1,201) = 1.00, ns. The second step, which tested for moderation, the interaction between angry bias and Abuse was significant, F(1,201) = 6.18, standardized B = .15, p < .02. A separate model revealed a similar pattern for high IPV and GAD symptoms, with a significant interaction between IPV and angry bias, F(1,180) = 8.48, B = .14, p < .005. Thus, the relations between family violence and these forms of anxiety/fear were stronger at higher levels of attention bias towards threat. No moderation by happy bias was observed.
Discussion
There are several main findings from the current study. First, child-directed violence was associated with both children’s anxiety symptoms and attention biases. Second, children’s attention bias towards anger was related to their anxiety symptoms and, third, also moderated the violence exposure-anxiety relationship. In other words, children who had stronger attentional biases towards anger showed stronger associations between violence exposure and anxiety.
Children who were direct victims of more severe violence were identified as suffering from ‘probable abuse.’ This ‘probable abuse’ group was reported by their mothers as manifesting higher levels of specific phobia, generalized anxiety and trauma symptoms, relative to other children. Severe intimate partner violence was associated with dissociative symptoms. This expands what is known about the relationship between severe violence exposure and anxiety in preschool-aged children. Harsh (but not abusive) parenting was associated only with specific phobias and depression/dysthymia. Notably, severe direct exposure to violence also was associated with greater attention bias towards threat. This extends to preschool-aged children patterns that have previously been observed only in older children (Gulley et al., 2014; Shackman et al., 2007). Together, these past studies and the current findings suggest that exposure to family violence may alter children’s patterns of attention and lead to increased vigilance towards threats in their environments. However, all of these studies were cross-sectional and must be interpreted cautiously. In adults, longitudinal studies have indicated increases in attention bias towards threat following violence exposure, such as experiencing combat (Wald et al., 2013). Thus, prospective research may reveal similar violence-related processes in children.
Moreover, attention bias towards anger in the dot-probe was associated with observed fear/anxiety in the Anx-DOS. Children with a greater bias towards threat were significantly more likely to display fear, physical avoidance, and startle responses than other children. In contrast, attention bias was not associated with mother-reported anxiety. This lack of association may reflect general limitations of parental reports of children’s internalizing symptoms (De Los Reyes, Thomas, Goodman, & Kundey, 2013; Kassam-Adams et al., 2006) or of DSM symptom-based measures for capturing aspects of anxiety that can be associated with underlying neural processes (Insel et al., 2010). This greater correspondence between the Anx-DOS and the dot-probe also could reflect the fact that both capture children’s responses to acute threats and are directly-observed behaviors.
Finally, attention bias moderated the relationship between probable abuse and observed anxiety and between severe IPV and generalized anxiety symptoms. This adds to a recent study in which attention bias moderated the association between negative, harsh parenting and anxiety in school-age children (Gulley et al., 2014). In both that prior study and in ours, exposed children with bias towards threat tended to display greater fear/anxiety than exposed children without such bias. As both were cross-sectional, we cannot establish whether attention bias promoted, exacerbated or sustained children’s anxiety. However, an earlier study suggests that bias may indeed contribute to the persistence or onset of anxiety in young children– bias towards threat at age 5 moderated the relationship between behavioral inhibition and social withdrawal, with greater bias towards threat associated with more withdrawal in children who were behaviorally inhibited as toddlers (Perez-Edgar et al., 2011).
Strengths and limitations
Strengths of this study are the use of a multi-method developmentally-adapted protocol with preschoolers and the enriched community-based design, which increased power to test study hypotheses while retaining generalizability to non-referred children. However, the cross-sectional design prevents us from establishing causal patterns. Additionally, the lack of temperament data prevents us from examining how behavioral inhibition may influence patterns in this sample. Finally, the lack of PTSD symptoms is only partially addressed by the addition of the trauma symptom survey.
Summary
This study demonstrates the presence of attention bias to threat in very young children who have experienced relatively severe child-directed violence in the context of parenting. Children with stronger attentional biases towards threats also displayed heightened fear/anxiety in response to proximal threats in our observational paradigm. This convergence of behaviors across two separate paradigms suggests a general pattern of heightened responses to threats that may represent early vulnerability for anxiety. The relationship between family violence exposure and fear/anxiety also was stronger at higher levels of attention bias towards threat. If evident in a longitudinal design, such a pattern would suggest that attention bias is a mechanism through which early exposures influence developmental pathways for anxiety and trauma-related psychopathologies. Finally, findings suggest the potential for innovative methods to identify young children at high risk for anxiety and to intervene with novel interventions, such as attention bias modification training (Bar-Haim et al., 2011; Shechner et al., 2012), to deflect negative trajectories before the onset of impairing anxiety.
Supplementary Material
Keypoints.
This is the first study to support attention bias to threat as a moderator of the relationship between early adversity (violence) and anxiety in young children. Anxiety was particularly pronounced in children exposed to violence who also displayed attention bias towards threat. Children who devote disproportionate attention to detecting potentially threatening stimuli in their environment may be at high risk for developing anxiety early in life.
A picture is worth a thousand words - Observed behavior but not maternal reports were associated with attention bias. Clinically, this underscores the value of supplementing maternal reports with observation, and especially with paradigms that help to distinguish clinically-concerning anxiety from more normative fears and anxieties.
Findings also contribute to a growing evidence base that young children who experience more severe and frequent violence manifest fear, anxiety and distress, underscoring the need for preventive and intervention efforts targeting this high-risk population.
Acknowledgements
Financial support for the study was provided by grants from the National Institute of Mental Health (U01MH090301; R01MH082830). The authors thank Jackie Kestler and Kimberly McCarthy for their hard work and dedication to supporting this study.
Footnotes
The authors have declared that they have no competing or potential conflicts of interest.
Supporting Information
Additional Supporting Information is provided along with the online version of this article.
Figure S1. Sampling Design
Figure S2. Affective Dot Probe Task
References
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van IJzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychological Bulletin. 2007;133(1):1–24. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y, Morag I, Glickman S. Training anxious children to disengage attention from threat: a randomized controlled trial. Journal of Child Psychology & Psychiatry. 2011;52(8):861–869. doi: 10.1111/j.1469-7610.2011.02368.x. [DOI] [PubMed] [Google Scholar]
- Bayer JK, Ukoumunne OC, Lucas N, Wake M, Scalzo K, Nicholson JM. Risk factors for childhood mental health symptoms: national longitudinal study of Australian children. Pediatrics. 2011;128(4):e865–e879. doi: 10.1542/peds.2011-0491. [DOI] [PubMed] [Google Scholar]
- Briere J, Johnson K, Bissada A, Damon L, Crouch J, Gil E, et al. The Trauma Symptom Checklist for Young Children (TSCYC): reliability and association with abuse exposure in a multi-site study. Child Abuse & Neglect. 2001;25(8):1001–1014. doi: 10.1016/s0145-2134(01)00253-8. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Clark R, Augustyn M, McCarthy KJ, Ford JD. Exposure to potentially traumatic events in early childhood: differential links to emergent psychopathology. Journal of Child Psychology and Psychiatry. 2010;51(10):1132–1140. doi: 10.1111/j.1469-7610.2010.02256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Mian N, Carter AS, Wakschlag LS. The Anxiety Dimensional Observation Schedule (Anx-DOS), Version 1.0. Northwestern University; 2011. [Google Scholar]
- Clark LA, Watson D. Distress and fear disorders: an alternative empirically based taxonomy of the "mood" and "anxiety" disorders. British Journal of Psychiatry. 2006;189:481–483. doi: 10.1192/bjp.bp.106.03825. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Thomas SA, Goodman KL, Kundey SM. Principles underlying the use of multiple informants' reports. Annual Review of Clinical Psychology. 2013;9:123–149. doi: 10.1146/annurev-clinpsy-050212-185617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychology & Psychiatry. 2006;47(3–4):313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A. Test-Retest Reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Elliott C. Differential Abilities Scales: Introductory and technical handbook. New York: Psychological Corporation; 1983. [Google Scholar]
- Ferguson CJ. Spanking, corporal punishment and negative long-term outcomes: a meta-analytic review of longitudinal studies. Clinical Psychology Review. 2013;33(1):196–208. doi: 10.1016/j.cpr.2012.11.002. [DOI] [PubMed] [Google Scholar]
- Grasso DJ, Briggs-Gowan MJ, Henry DB, Wakschlag LS. Latent class analysis of child directed and witnessed family violence among preschool children and associated risk. 2014 [Google Scholar]
- Gulley LD, Oppenheimer CW, Hankin BL. Associations among negative parenting, attention bias to anger, and social anxiety among youth. Developmental Psychology. 2014;50(2):577–585. doi: 10.1037/a0033624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N, Garcia-Espana JF, Miller VA, Winston F. Parent-child agreement regarding children's acute stress: the role of parent acute stress reactions. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(12):1485–1493. doi: 10.1097/01.chi.0000237703.97518.12. [DOI] [PubMed] [Google Scholar]
- LeDoux JE. Emotion circuits in the brain. Annual Review of Neuroscience. 2000;23:155–184. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- Levendosky AA, Bogat GA, Martinez-Torteya C. PTSD symptoms in young children exposed to intimate partner violence. Violence Against Women. 2013;19(2):187–201. doi: 10.1177/1077801213476458. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, Goode S, Heemsbergen J, Jordan H, Mawhood L, et al. Autism diagnostic observation schedule: a standardized observation of communicative and social behavior. Journal of Autism and Developmental Disorders. 1989;19(2):185–212. doi: 10.1007/BF02211841. [DOI] [PubMed] [Google Scholar]
- Moradi AR, Neshat-Doost HT, Teghavi R, Yule W, Dalgleish T. Performance of children of adults with PTSD on the stroop color-naming task: a preliminary study. Journal of Traumatic Stress. 1999;12(4):663–671. doi: 10.1023/A:1024721218869. [DOI] [PubMed] [Google Scholar]
- Nichols S, Briggs-Gowan MJ, Estabrook R, Burns J, Kestler J, Berman G, et al. Punishment insensitivity in early childhood: A developmental, dimensional approach. Journal of Abnormal Child Psychology. In press doi: 10.1007/s10802-014-9950-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Edgar K, Reeb-Sutherland BC, McDermott JM, White LK, Henderson HA, Degnan KA, et al. Attention biases to threat link behavioral inhibition to social withdrawal over time in very young children. Journal of Abnormal Child Psychology. 2011;39(6):885–895. doi: 10.1007/s10802-011-9495-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pine DS. Research review: a neuroscience framework for pediatric anxiety disorders. Journal of Child Psychology and Psychiatry. 2007;48(7):631–648. doi: 10.1111/j.1469-7610.2007.01751.x. [DOI] [PubMed] [Google Scholar]
- Pine DS, Mogg K, Bradley BP, Montgomery L, Monk CS, McClure E, et al. Attention bias to threat in maltreated children: implications for vulnerability to stress-related psychopathology. American Journal of Psychiatry. 2005;162(2):291–296. doi: 10.1176/appi.ajp.162.2.291. [DOI] [PubMed] [Google Scholar]
- Pollak SD. Mechanisms linking early experience and the emergence of emotions: Illustrations from the study of maltreated children. Current Directions in Psychological Science. 2008;17(6):370–375. doi: 10.1111/j.1467-8721.2008.00608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak SD. The Role of Parenting in the Emergence of Human Emotion: New Approaches to the Old Nature-Nurture Debate. Parenting Science and Practice. 2012;12(2–3):232–242. doi: 10.1080/15295192.2012.683363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shackman JE, Shackman AJ, Pollak SD. Physical abuse amplifies attention to threat and increases anxiety in children. Emotion. 2007;7(4):838–852. doi: 10.1037/1528-3542.7.4.838. [DOI] [PubMed] [Google Scholar]
- Shechner T, Britton JC, Perez-Edgar K, Bar-Haim Y, Ernst M, Fox NA, et al. Attention biases, anxiety, and development: toward or away from threats or rewards? Depress Anxiety. 2012;29(4):282–294. doi: 10.1002/da.20914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP. Protecting brains, not simply stimulating minds. Science. 2011;333(6045):982–983. doi: 10.1126/science.1206014. [DOI] [PubMed] [Google Scholar]
- Spence SH, Rapee R, McDonald C, Ingram M. The structure of anxiety symptoms among preschoolers. Behav Res Ther. 2001;39(11):1293–1316. doi: 10.1016/s0005-7967(00)00098-x. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: development and psychometric data for a national sample of American parents. Child Abuse and Neglect. 1998;22(4):249–270. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Swartz JR, Graham-Bermann SA, Mogg K, Bradley BP, Monk CS. Attention bias to emotional faces in young children exposed to intimate partner violence. Journal of Child and Adolescent Trauma. 2011;4:109–122. [Google Scholar]
- Wakschlag LS, Briggs-Gowan MJ, Choi SW, Nichols SR, Kestler J, Burns JL, et al. Advancing a multidimensional, developmental spectrum approach to preschool disruptive behavior. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(1):82–96. doi: 10.1016/j.jaac.2013.10.011. e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Briggs-Gowan MJ, Hill C, Danis B, Leventhal BL, Keenan K, et al. Observational Assessment of Preschool Disruptive Behavior, Part II: validity of the Disruptive Behavior Diagnostic Observation Schedule (DB-DOS) Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(6):632–641. doi: 10.1097/CHI.0b013e31816c5c10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wald I, Degnan KA, Gorodetsky E, Charney DS, Fox NA, Fruchter E, et al. Attention to threats and combat-related posttraumatic stress symptoms: prospective associations and moderation by the serotonin transporter gene. JAMA Psychiatry. 2013;70(4):401–408. doi: 10.1001/2013.jamapsychiatry.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters AM, Henry J, Mogg K, Bradley BP, Pine DS. Attentional bias towards angry faces in childhood anxiety disorders. J Behav Ther Exp Psychiatry. 2010;41(2):158–164. doi: 10.1016/j.jbtep.2009.12.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.