Abstract
The nursing outcomes of hospitalized patients whose plans of care include death anxiety, which is a diagnosis among patients at the end-of-life, are obscure. The authors of the current article applied data mining techniques to nursing plan-of-care data for patients diagnosed with death anxiety, as defined by North American Nursing Diagnosis Association International, from four different hospitals to examine nursing care outcomes and associated factors. Results indicate that <50% of patients met the expected outcome of comfortable death. Gerontology unit patients were more likely to meet the expected outcome than patients from other unit types, although results were not statistically significant. Younger patients (i.e., age <65) had a lower chance of meeting the outcome compared with older patients (i.e., age ≥65) (χ2(1) = 9.266, p < 0.004). Longer stays improved the chances of meeting the outcome (χ2(2) = 6.47, p < 0.04). Results indicate that death anxiety outcomes are suboptimal and suggest the need to better educate clinicians about diagnosing and treating death anxiety among patients who face the end-of-life transition.
The official North American Nursing Diagnosis Association International (NANDA-I) definition for death anxiety is a “vague uneasy feeling of discomfort or dread generated by perceptions of a real or imagined threat to one's existence” (2007, pp. 11-12); it is characterized by fear of suffering, powerlessness, and the impact of one's death on others. Death anxiety has also been described as apprehension arising from one's death awareness (Abdel-Khalek, 2005). Reduction of death anxiety is important to achieving comfort and respectful death goals. Because hospitals in the United States typically focus on preserving life, one important research question is: Do nurse clinicians diagnose death anxiety, and are desired outcomes of care achieved in hospitalized patients who are near the end of life (EOL)?
The phenomenon of death anxiety has been well studied and is supported by a rich scientific literature, predominantly from the field of psychology (Abdel-Khalek, 2005; Depaola, Griffin, Young, & Neimeyer, 2003; Keller, Sherry, & Piotrowski, 1984). However, some literature on death anxiety also originates from the field of nursing (Kisvetrová, Klugar, & Kabelka, 2013; Lehto & Stein, 2009). Research has shown that when death is integrated as a core part of being, it is perceived as less threatening (Lehto & Stein, 2009); therefore, individuals experience less death anxiety. Older adult study participants have reported lower death anxiety than middle-aged participants (Bengtson, Cuellar, & Ragan, 1977; Feifel & Branscomb, 1973; Fortner & Neimeyer, 1999; Keller et al., 1984), but findings from cohort studies indicate that the age-related decrease in death anxiety stabilizes rather than continuing within the older adult population (Fortner & Neimeyer, 1999). Levels of death anxiety are less in individuals with committed religious beliefs and practices as compared with those without religious beliefs (Alvarado, Templer, Bresler, & Thomas-Dobson, 1995), and they are higher in older women than in older men or younger women and men (Depaola et al., 2003).
The science related to the phenomenon of death anxiety has generally been informed by individuals self-rating their death anxiety using Likert-type scales (Abdel-Khalek, 1998; Wen, 2010; Wittkowski, 2001). Study populations have typically included college students (Keller et al., 1984; Schwartz, Mazor, Rogers, Ma, & Reed, 2003) and/or family members recruited by college students (Wittkowski, 2001), churchgoers (Wen, 2010), and hospice nurses (Schwartz et al., 2003). However, investigators have rarely studied a population with advanced illness or at EOL (Lo et al., 2011). Studies specific to the nursing literature most frequently depict the phenomenon of death anxiety in terms of nurses’ death anxiety versus patients’ death anxiety; in addition, they measure how that anxiety influences patient care (Peters et al., 2013). In one nursing study, investigators used a quantitative survey to examine spiritual support care activities that Czech nurses offered to patients at the EOL (Kisvetrová et al., 2013). In another study, Grossman (2007) examined nursing documentation of EOL patient symptoms, interventions, and responses in two long-term care facilities before and after participation in a nursing education program on pain and symptom management. However, the authors of the current article found no studies that analyzed the outcomes of care provided to hospitalized patients diagnosed with death anxiety at the EOL.
Although death anxiety is one of the nursing diagnoses defined by NANDA-I (2003), a second notable gap in the literature is the lack of studies focused on patients diagnosed with death anxiety using data available in health records. This gap may be due, in part, to the lack of quality informatics tools for recording this diagnosis and the associated interventions and outcomes in a retrievable and analyzable format. Practice-based evidence has the potential to increase the understanding of clinical phenomena related to death anxiety as it is diagnosed and treated in real-world settings. Such evidence, along with evidence from randomized controlled studies, has the potential to generalize to the larger population (Benson & Hartz, 2000).
Using an existing, valid, and highly reliable electronic health record (EHR) data set coded with standardized nursing terminologies (Keenan et al., 2012), the current study aimed to (a) examine the care outcomes for hospitalized EOL patients whose plans of care included the NANDA-I diagnosis death anxiety and (b) identify patient- and nurse-related factors associated with the outcomes. The importance of this work was its potential to identify the anomalies and hidden correlations related to outcomes of hospitalized patients associated with the nursing diagnosis death anxiety.
METHOD
Design
The authors of the current article conducted a data mining study of an existing data set. The data were obtained as part of routine clinical practice (Keenan et al., 2012). Specifically, RNs from four study hospitals consistently documented patient problems, interventions, and outcomes using standardized terminologies in the Hands-On Automated Nursing Data System (HANDS), an EHR system designed specifically to record nursing care provided to patients. Diagnoses were based on NANDA-I (2003) terminologies, as well as outcomes on the Nursing Outcome Classification (NOC; Moorhead, Johnson, & Maas, 2004) and interventions on the Nursing Interventions Classification (NIC; Dochterman & Bulechek, 2004) terminologies. Availability of these data made it possible to examine outcomes for patients who were diagnosed with death anxiety, based on the NANDA-I definition, when they were near death.
The original study was approved by the Institutional Review Board (IRB) at the University of Illinois at Chicago (UIC) and participating institutions. The analysis reported in the current article did not involve human subjects because the data set is de-identified, as determined by the IRB at the UIC.
Setting
The data were collected from nine medical-surgical units located in four unique Midwestern hospitals (Keenan et al., 2012). The clinical specialties represented in the nine units are depicted in Table 1.
TABLE 1.
Clinical Specialties of Units Studied by Hospital Type
| EOL Patients With Death Anxiety Diagnosis | |||||
|---|---|---|---|---|---|
| Hospital | Unit | Total EOL Patients (N = 1,453) (n[%]) | Total (N = 462) (n[%]) | Cared for by Experienced Nurses (n[%]) | Cared for by Less Experienced Nurses (n[%]) |
| LCH1 | General Medical | 173 (11.9) | 9 (1-9) | 9 (100) | 0 (0) |
| Medical ICU | 148 (10.2) | 2 (0.4) | 1 (50) | 1 (50) | |
| Gerontology | 472 (32.5) | 296 (64.1) | 157 (53) | 139 (47) | |
| UH | Cardiac Surgical | 46 (3.2) | 8 (1.7) | 7 (87.5) | 1 (12.5) |
| Neurosurgical | 87 (6) | 34 (7.4) | 25 (73.5) | 9 (26.5) | |
| Cardiac ICU | 153 (10.5) | 11 (2.4) | 6 (54.5) | 5 (45.5) | |
| LCH2 | Medical Gerontology | 103 (7.4) | 32 (6.9) | 22 (68.8) | 10 (31.2) |
| General Medical | 144 (9.9) | 36 (7.8) | 17 (47.2) | 19 (52.8) | |
| SCH | Medical Surgical | 122 (8.4) | 34 (7.4) | 22 (64.7) | 12 (35.3) |
Note. EOL = end-of-life; LCH1 = large community hospital 1; ICU = intensive unit; UH = university hospital; LCH2 = large community hospital 2; SCH = small community hospital. Nurses who have at least 2 years of experience at their current position are considered to be experienced nurses. All other nurses with <2 years of experience are considered to be less experienced nurses.
Sample
The authors derived the data for this secondary analysis study from a primary data set gathered on 42,403 medical-surgical care episodes (34,927 unique patients). Each hospitalization of a patient on a study unit corresponds to one episode, which is defined as a continuous patient stay on a single hospital unit. A patient was identified as an EOL patient from the larger dataset using one or more of the following indicators on a plan of care (POC) within the patient's episode:
Discharge status = expired OR hospice home care OR discharged to hospice medical facility OR
NOC = dignified life closure OR comfortable death OR
NIC = dying care
A total of 1,453 unique EOL patients were included in the study, with some participants represented in multiple episodes. In the analysis, the authors considered only the last episode for each patient; therefore, each patient is represented only once in the analytic dataset. Previous episodes for those with multiple episodes were not included to avoid violation of the independence assumption required by the data mining techniques. The authors would have adopted more complicated analytical tools, such as multilevel modeling, to include these episodes if a substantial number of them had occurred; however, only eight patients experienced more than one episode. Therefore, including these few episodes would have provided minimal gain.
The mean age of patients was 75 (SD = 14.1 years). Of the study participants, 462 patients, whose episodes included multiple POCs that were updated each shift, were diagnosed with death anxiety by the nurses providing care to them. The authors excluded patients with only one POC because at least two POCs were needed to compute patients’ progress toward the expected outcome. All of the results presented in the current article are based on the study of the POCs for these 462 patients.
The admitting nurse created an admission shift HANDS POC for each patient, which included the nursing diagnoses, outcomes (i.e., current rating of the nursing outcomes in the POC and expected rating at discharge), and interventions applicable to the patient's condition. At every handoff thereafter, the POC was updated with new content, and all outcomes were rated (in the case of a new NOC) or re-rated (in the instances when the NOC was added to a previous POC) for each outcome included on the plan. The NANDA-I diagnosis of death anxiety was assigned only to patients who were assessed by RNs as exhibiting the signs and symptoms of the diagnosis (Table 2). To facilitate the validity of RN diagnosis, information containing the pertinent attributes of each NANDA-I diagnosis was made immediately available through decision support information buttons in HANDS. Therefore, diagnoses were not assigned automatically to patients, but rather the HANDS software provided robust decision support to help the RNs, who had extensive training and validation prior to using HANDS, locate and select the appropriate diagnoses for each patient. Validity and reliability of the trained RNs’ use of the standardized terms are reported elsewhere (Keenan et al., 2012).
TABLE 2.
NANDA-I Death Anxiety Diagnosis
| Death Anxiety (1998, 2006a) |
| Definition: Vague uneasy feeling of discomfort or dread generated by perceptions of a real or imagined threat to one's existence. |
| Defining characteristics |
| • Reports concerns of overworking the caregiver |
| • Reports deep sadness |
| • Reports fear of developing terminal illness |
| • Reports fear of loss of mental abilities when dying |
| • Reports fear of pain related to dying |
| • Reports fear of premature death |
| • Reports fear of the process of dying |
| • Reports fear of prolonged dying |
| • Reports fear of suffering related to dying |
| • Reports feeling powerless over dying |
| • Reports negative thoughts related to death and dying |
| • Reports worry about the impact of one's own death on significant others |
| Related factors |
| • Anticipating adverse consequences of general anesthesia |
| • Anticipating impact of death on others |
| • Anticipating pain |
| • Anticipating suffering |
| • Confronting reality of terminal disease |
| • Discussions on topic of death |
| • Experiencing dying process |
| • Near death experience |
| • Nonacceptance of own mortality |
| • Observations related to death |
| • Perceived proximity of death |
| • Uncertainty about an encounter with a higher power |
| • Uncertainty about the existence of a higher power |
| • Uncertainty about life after death |
| • Uncertainty of prognosis |
Note. NANDA-I = North American Nursing Diagnosis Association International.
Years denote when death anxiety was defined and redefined, respectively.
Reprinted with permission (NANDA-I, 2007, pp. 11-12).
Procedure and Measures
The authors used the HANDS (Keenan et al., 2012) database, which contains historic episodes of nursing POCs collected between 2005 and 2008. HANDS is an electronic application and database that nurses used to enter and track patients’ clinical diagnoses, outcomes, and interventions across episodes of care. An episode consisted of the POCs that nurses documented at every formal handoff (e.g., admission, shift-change update, discharge) in the HANDS software for a period of 1 year (i.e., 4 units) or 2 years (i.e., 5 units). The diagnoses, interventions, outcome ratings recorded every shift, patient characteristics, and characteristics of the nurse providing care were all linked at the shift level. All patients on these units for the duration of the study were participants in the original study, and therefore, their POC data reside in the database. Therefore, the EOL patients included in the current study were a subset of all patients whose data were collected on these nine units and who met the designated EOL criteria. For a majority of patients, their POCs were updated every 8 to 12 hours. Thus, the main attributes (i.e., variables) available in the database for each POC include patient demographics, nurse demographics, all nursing diagnoses, the associated outcomes, and their ratings at the time; interventions are also included, all of which are coded with standardized terminologies approved by the American Nurses Association. Nursing diagnoses were coded with NANDA-1 (2003) terms, outcomes were coded using terms and rating scales from the NOC (Moorhead et al., 2004), and interventions were coded with terms from the NIC (Dochterman & Bulechek, 2004). An expected outcome rating (i.e., goal at discharge from the unit, where 1 represents the lowest or worst outcome and 5 represents the highest or best outcome) for each NOC was recorded only on the POC when the NOC was first entered. The RN entered a patient's discharge disposition into the database at the end of each episode.
Analysis
The authors applied multiple data mining techniques on a targeted dataset consisting of only those episodes that included death anxiety among EOL patients. However, to reduce clutter in the data and analysis, the NANDA-I diagnoses other than death anxiety, as well as the NIC interventions that appeared in the EOL episodes, were clustered into domains and classes. Instead of applying data-dependent clustering, the authors used the nursing literature to cluster the NANDA-I diagnoses and NIC interventions. According to the NANDA-I system, multiple NANDA-I (2003) diagnoses and NIC interventions (Dochterman & Bulechek, 2004) have been logically and thematically grouped into classes, and multiple classes have been further grouped into domains. The NANDA-I diagnoses that appeared in the authors’ sample of episodes belonged to 12 different NANDA-I domains. However, only four of the 12 were used in the analysis. The remaining eight domains were not studied due to low frequency of episodes that contained NANDA-I diagnoses belonging to those domains. In addition, the authors included only five of 23 NANDA-I classes from the four domains based on the frequency distribution. Similarly, of the seven NIC domains, the authors used three domains, and of the 27 NIC classes, they included five classes, based on the frequency distribution. Table 3 illustrates the relationships among the NIC domains, classes, and terms (i.e., labels). The table also provides the NOC met ratio (i.e., the ratio of episodes where the NOC was met to the total number of episodes in a given analysis, reported as a percentage value) when the NIC was used with NOC: Comfortable Death. As is noted, the NIC: Dying Care was used in 398 episodes, but the corresponding NOC-expected rating was met only in approximately 47.4% of episodes. In the association mining analysis, the authors used the NIC Behavioral, Family, and Physiological: Basic domains to represent NIC labels belonging to these three domains that were in patient episodes. The other domains were not used because of low frequency. For the classwise analysis, the authors used the Coping Assistance, Physical Comfort Promotion, Life Span Care, Immobility Management, and Self-Care Facilitation classes.
Table 3.
NICs for NOC: Comfortable Death Frequency Table with NOC met %, and NIC domains and classes.
| NIC Domain Names | NIC Class Names | NIC Label Name | Episode Count | NOC Met (%age) |
|---|---|---|---|---|
| Behavioral | Behavior Therapy | Music Therapy | 3 | 66.7 |
| Mutual Goal Setting | 3 | 33.3 | ||
| Communication Enhancement | Active Listening | 21 | 57.1 | |
| Coping Assistance | Dying Care | 398 | 47.4 | |
| Emotional Support | 47 | 51.1 | ||
| Spiritual Support | 23 | 47.8 | ||
| Touch | 10 | 30.0 | ||
| Coping Enhancement | 5 | 20.0 | ||
| Grief Work Facilitation | 5 | 60.0 | ||
| Counseling | 2 | 50.0 | ||
| Humor | 1 | 100 | ||
| Security Enhancement | 1 | 0 | ||
| Physical Comfort Promotion | Calming Technique | 26 | 57.7 | |
| Anxiety Reduction | 22 | 45.5 | ||
| Simple Relaxation Therapy | 2 | 0 | ||
| Family | Information Management | Referral | 1 | 0 |
| Life Span Care | Family Support | 74 | 49.3 | |
| Caregiver Support | 18 | 33.3 | ||
| Respite Care | 7 | 42.9 | ||
| Family Process Maintenance | 6 | 66.7 | ||
| Health System | Health System Mediation | Visitation Facilitation | 5 | 20.0 |
| Health System Guidance | 1 | 100 | ||
| Patient Rights Protection | 1 | 0 | ||
| Physiological: Basic | Immobility Management | Bed Rest Care | 53 | 39.6 |
| Positioning | 1 | 0 | ||
| Physical Comfort Promotion | Pain Management | 75 | 54.7 | |
| Simple Massage | 1 | 0 | ||
| Self-Care Facilitation | Self-Care Assistance | 26 | 53.8 | |
| Bathing | 12 | 58.3 | ||
| Feeding | 1 | 100 | ||
| Physiological: Complex | Drug Management | Analgesic Administration | 19 | 47.4 |
| Medication Administration | 14 | 7.1 | ||
| Medication Management | 11 | 54.5 | ||
| Patient-Controlled Analgesia (PCA) Assistance | 7 | 42.9 | ||
| Respiratory Management | Oxygen Therapy | 2 | 50.0 | |
| Respiratory Monitoring | 1 | 0 | ||
| Skin/Wound Management | Skin Surveillance | 2 | 50.0 | |
| Tissue Perfusion Management | Circulatory Care: Venous Insufficiency | 1 | 100 |
The authors applied association rule mining techniques to the clustered data set. Association rule mining aims to extract interesting correlations or frequent patterns in the database. Association rule mining is used to discover association rules based on predefined minimum support and confidence. The support of an item set X is defined as the proportion of transactions in the data set, which contain the item set. Confidence of the rule X → Y (X implies Y) is defined as the proportion of support of X and Y over the support of X. Due to the limited size of the death anxiety EOL dataset, the application of classification technique was not deemed suitable.
The analysis of the data was performed for different outcomes related to the death anxiety diagnosis across all units and for each individual unit. The authors considered patient age, length of stay (LOS), discharge status, unit, and nurse experience to determine whether any of these factors played a role in a patient meeting or not meeting the expected outcome. Patient age, LOS, and nurse experience were continuous variables that were first discretized before data mining could be performed. For example, the authors divided patients into four age groups (i.e., 18 to 49, 50 to 64, 65 to 84, and 85 and older) based on theoretical and data frequency distribution. The authors did not encounter any data quality issues in the current study; thus, no episodes were excluded due to data quality.
For nurse experience, the authors considered a nurse with experience of at least 2 years to be an experienced nurse, and nurses with less than 2 years of experience were considered inexperienced. The episode was categorized as care provided by an experienced nurse if more than 50% of the nurses providing care in that episode had more than 2 years of experience.
The authors calculated LOS for each episode by summing the number of hours for all of the shifts in the episode. They divided the LOS into three categories: short (<48 hours), medium (48 to 119 hours), and long (120 hours or more). For each episode, the authors studied the related NOC outcomes and NIC intervention classes and examined whether NOC outcomes related to death anxiety met the expected outcomes.
The expected outcome was met if the NOC rating in the last POC of a given episode was greater than or equal to the expected rating established on the POC, to which the NOC was first added within an episode.
RESULTS
Among the 462 patients that had NANDA-I death anxiety diagnoses, the average age was 78 (SD = 12.9 years). Approximately 4.5% of patients were ages 18 to 49, 9.5% were 50 to 64, 47.2% were 65 to 84, and 38.8% were 85 or older.
For patients with a NANDA-I death anxiety diagnosis, the average LOS was 113 hours (SD = 117 hours) compared with LOS of 103 hours (SD = 108 hours) for all EOL patients. Approximately 25.3% of patients with death anxiety experienced a stay of less than 48 hours, 36.4% stayed 48 to 120 hours, and 38.7% had a stay exceeding 120 hours. Approximately 54.5% of the EOL patients with death anxiety died in the hospital, 24.9% were discharged to hospice, and 20.6% were transferred to other units. Of the patients with gender information, 10% were male and 14.3% were female. The gender information was absent for approximately 75% of patients because it was not a required data entry field in the HANDS software, and for the current study, HANDS was not directly interfaced to the EHR.
Table 1 shows, by study unit, the number of patients and the number of nurses by their experience levels. Of the patients diagnosed with death anxiety, most (i.e., approximately 64%) were admitted to the large community hospital 1 gerontology unit, whereas none of the other units had more than 10% of patients with death anxiety.
Figure 1 shows the five most frequent NOC outcomes related to the NANDA-I death anxiety diagnosis and frequency, as well as the percentages of the episodes for which each of the NOC outcomes was met and the percentages of the episodes for which each of the NOC outcomes was not met. A total of 438 episodes with the NANDA-I death anxiety diagnosis occurred; these episodes also included the NOC: Comfortable Death outcome, of which 47% met the expected outcome. The second most common NOC was Dignified Life Closure, in which the expected outcome was met in approximately 48% of episodes. Of the five NOC outcomes, NOC: Fear Level was the only one for which the expected outcome was met for more than 50% (i.e., approximately 53%) of the episodes. NOC: Pain Control was less commonly found with the NANDA-I death anxiety diagnosis, as it was present in only 16 of 462 patients, with approximately 44% of patients meeting the expected outcome. NOC: Coping was the least common, present in only 14 of 462 patients, with approximately 36% meeting the expected outcome (Figure 1). Although nurses used multiple NOC outcomes to evaluate the impact of nursing care on death anxiety, only the NOC: Comfortable Death outcome occurred with sufficient frequency to warrant additional analysis. The following analysis will therefore focus on the NOC: Comfortable Death outcome.
Figure 1.

Percentage of expected NOC ratings met and not met for different NOCs related to the NANDA-I death anxiety diagnosis.
Note. NOC = Nursing Outcome Classification; NANDA-I = North American Nursing Diagnosis Association International. The numbers inside the bars represent the number of episodes.
For patients with death anxiety, it was discovered that the chance of meeting the expected outcome for NOC: Comfortable Death increased with a longer LOS. Figure 2 presents the relationship between the LOS and the NOC: Comfortable Death outcome related to the NANDA-I death anxiety diagnosis. The percentage of episodes where the NOC expected outcome was met increased as the LOS increased. The chi-square test showed that for patients with death anxiety, the chance of meeting the expected NOC: Comfortable Death outcome rating improved as the LOS increased (χ2(2) = 6.47, p < 0.04).
Figure 2.

Relationship of NOC: Comfortable Death outcome with length of stay of hospitalized patients.
Note. NOC = Nursing Outcome Classification. The numbers inside the bars represent the number of episodes.
The data were also analyzed to determine if patient age had any impact on the outcome. As shown in Figure 3, it was observed that younger patients (age <65) had a low NOC met ratio (i.e., 29%), compared with older patients (age ≥65), for whom the expected NOC met ratio was approximately 50%. A chi-square test indicated that the difference was statistically significant (χ2(1) = 9.266, p < 0.004).
Figure 3.

Relationship of NOC: Comfortable Death outcome with patient age.
Note. NOC = Nursing Outcome Classification. The numbers inside the bars represent the number of episodes.
From a review of the data by unit, it was observed that most patients (71.2%) diagnosed with death anxiety received care on gerontology units (Table 1). In addition, those EOL patients receiving care from experienced nurses were more likely (54.8%) to meet the NOC: Comfortable Death expected outcome, compared with EOL patients receiving care from inexperienced nurses (48%) on the gerontology units. However, the chi-square test revealed that the difference by nurse experience was not statistically significant (p < 0.28). Figure 4 shows the percentage of expected NOC ratings being met and not met by nurse experience level for the two gerontology units combined.
Figure 4.

Percentages of expected NOC outcome ratings met and not met by nurse experience for gerontology units (combined) for NOC: Comfortable Death outcome.
Note. NOC = Nursing Outcome Classification. The numbers inside the bars represent the number of episodes.
Figure 5 shows the expected NOC rating not met ratio compared among unit types and the discharge status of patients. The expected NOC rating met ratio was above 50% only for patients who died while on the two gerontology units. Patients on the gerontology units who were discharged to hospice had an expected NOC rating met ratio of approximately 45%. The expected NOC rating met ratio for other units was lower than 50%, regardless of the discharge status. As mentioned previously, for patients on gerontology units only, the patients who died had a greater chance of meeting the expected rating for NOC: Comfortable Death compared with patients who were discharged to hospice. The chi-square test showed that the difference was close to being statistically significant (χ2(1) = 2.57, p < 0.09).
Figure 5.
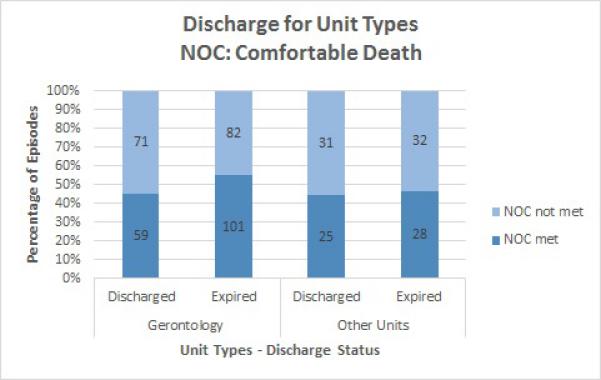
Percentages of expected NOC outcome ratings met and not met by type of unit and discharge status for NOC:Comfortable Death outcome.
Note. NOC = Nursing Outcome Classification. The numbers inside the bars represent the number of episodes.
From Figures 2 and 3, it can be noted that an increase in LOS and age improved the NOC outcomes. To determine if any dependence existed between age and LOS (to see whether older adults who tend to stay longer had better NOC outcomes), a correlation test was run. The results showed that no dependence existed between the two variables, with a correlation coefficient of 0.04.
Results from the association rule mining (using NANDA-I domains or classes, NIC domains or classes, and the NOC: Comfortable Death outcome) to determine hidden patterns in the data with a minimum level of support (i.e., 15%) indicated that no rules existed for which confidence levels were adequate. All rules that emerged had a confidence level of 0.64 or lower.
DISCUSSION
In the current study, the authors examined the outcomes of a diagnosis of death anxiety among hospitalized EOL patients using an electronic tool that allows analyses of the clinical problem (i.e., diagnosis), the interventions used to address it, and the related outcomes. The initial examination revealed findings that both support and conflict with previous literature. The most promising finding is that the longer the LOS on a unit, the more likely a patient diagnosed with death anxiety was to achieve desired outcomes. This finding indicates the potential importance of providing an environment, not necessarily in a hospital setting, that is consistent and supportive of the dying process. With additional data and further analyses enabled by informatics tools such as HANDS, sufficient data may be found to demonstrate the unequivocal importance of keeping EOL patients out of hospitals whenever possible to help each patient realize a comfortable death, especially when the patient preference is to die at home, as is the preference for most Americans (Hall, Levant, & DeFrances, 2013).
The finding that one gerontology unit in a large community hospital was responsible for more than six of 10 diagnoses of death anxiety is important. Differences in nursing care by hospitals are well known (DeCato et al., 2013; Friedenberg, Levy, Ross, & Evans, 2012), but documentation of differences in EOL care by unit is a less-studied phenomenon because data are not readily available and in an easily analyzable format. The current study's finding that the one gerontology unit of nine total units was responsible for 32% of the EOL patients and 64% of the death anxiety diagnoses deserves additional research, as the current analyses cannot explain the differences in frequency of assigning this diagnosis by unit. It is possible that the nurses who developed starter unit templates for care included a death anxiety POC template, making it easier for these unit nurses to recognize and focus on death anxiety in their hospitalized EOL patients. Another possible reason may be that nurses on the gerontology unit are more familiar and accustomed to using palliative care services, which may also account for the trend in better death anxiety outcomes for patients who died on the gerontology unit. In addition, by nature of gerontology units, the patients are older and more likely to be facing EOL than on other units. Although a number of other explanations are possible, additional research is needed to explicate them. As stated previously, gerontology unit patients who died had a greater chance of meeting the expected rating for the NOC: Comfortable Death compared with patients who were discharged to hospice. This finding may be attributed to the fact that once the nurses realized that the patient was dying and no plan to discharge to hospice existed, they took responsibility for this particular NOC rather than assuming the hospice team would assume responsibility of it after discharge.
The high frequency of patients not meeting their expected outcomes related to death anxiety is an important finding that indicates a need to improve nursing practice at EOL. Patients whose LOS was 5 days or longer had a better chance of meeting the expected outcome related to death anxiety than those with a shorter LOS. In addition, only 29% of younger adult patients met their expected outcomes. The current study's findings related to age are consistent with prior death anxiety research focused on age (Bengtson et al., 1977; Feifel & Branscomb, 1973; Fortner & Neimeyer, 1999; Keller et al., 1984); however, the authors were not able to examine the data by gender as others have examined (Depaola et al., 2003). This study limitation is not resolvable for this data set. The authors did not identify other research related to LOS and its association with death anxiety outcomes. The findings have important implications for improving the care of hospitalized patients facing EOL. For example, consultation with the palliative care team should be considered soon after admission, as palliative care specialists may help all team members focus on treatments that will improve the rate of meeting the expected outcomes related to death anxiety.
RECOMMENDATIONS
Because approximately 50% of patients with death anxiety did not meet the expected outcomes of care and because more experienced gerontology nurses had better outcomes and gerontology units achieved slightly better outcomes (i.e., 51% versus 46% in other units, though not statistically significant), a need exists for general efforts aimed at improving the nursing care provided to EOL patients. As such, the authors recommend implementing educational programs that help all nurses who care for EOL patients understand the critical needs of patients who are dying and nurses’ primary clinical role when EOL patients are hospitalized. Programs such as the End-of-Life Nursing Consortium (Grant et al., 2013) and Toolkit for Nurturing Excellence at End of Life (https://research.nursing.uic.edu/Tneel/index.aspx; Wilkie, Judge, Wells, & Berkley, 2001) are packaged so they can be brought to the clinical teaching environment and delivered to clinicians at the bedside to enhance their ability to care for EOL patients.
IMPLICATIONS FOR PRACTICE
The finding that the expected outcomes for most of the NOCs related to death anxiety had a low percentage of being met indicates the need for increasing nurses’ knowledge about ways to reduce a patient's death anxiety and is a key implication of the current study's findings.
In conjunction with the palliative care consultations, another implication is a need to coordinate care with hospice services to facilitate either an expedient transition back to home or, if no other option is available, a respectful and comfortable death in the hospital. Hospice and palliative care services are excellent resources for bedside nurses to use and from which to be educated about their roles in providing a comfortable and respectful death.
A final implication follows from the finding that outcomes were significantly better for patients with longer LOSs and may relate to the need for continuity in caring for patients at EOL. The authors have not completed the analysis of the data set for continuity of care outcomes; however, they plan to do so, and they hypothesize that better death anxiety outcomes will be observed when continuity of care is optimal for EOL patients. HANDS provides an opportunity to observe indicators of nurses developing therapeutic relationships with dying patients, a key component of continuity of care. For example, the authors expect death anxiety outcomes to improve as nurses both perform the tasks of nursing and serve as a caring, therapeutic presence, using techniques such as the NIC: Active Listening and NIC: Calming Techniques, as well as comfort measures such as NIC: Massage and NIC: Therapeutic Touch. However, from the association data mining, the authors did not find any domains or classes of NICs associated with death anxiety outcomes. Reasons for this finding are unclear but may relate to the low frequency of a heterogeneous group of interventions and the relatively small sample for data mining techniques. In future research, additional exploration of the data set may yield additional insights about the influence of interventions on death anxiety outcomes.
CONCLUSION
The current study demonstrated that practice-based data, which are captured in a structured format as part of daily nursing practice caring for patients facing the EOL transition, offer important insights to guide practice improvement efforts and the identification of additional research priorities. The research team will continue to mine the data available in the HANDS database to gain additional insights about effective care for hospitalized dying patients.
Acknowledgments
The HANDS software, used to collect the original data in the research reported in the current article, is owned and distributed by HealthTeamIQ, LLC. Dr. Keenan is President and CEO of HealthTeamIQ, LLC. The remaining authors have disclosed no potential conflicts of interest, financial or otherwise. This research was supported by grant 1R01 NR012949 from the National Institutes of Health, National Institute for Nursing Research (NINR). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NINR. The authors thank Kevin Grandfield, Publication Manager, Department of Biobehavioral Health Science, College of Nursing, University of Illinois at Chicago, for his editorial assistance.
REFERENCES
- Abdel-Khalek AM. Single- versus multi-item scales in measuring death anxiety. Death Studies. 1998;22:763–772. doi: 10.1080/074811898201254. [DOI] [PubMed] [Google Scholar]
- Abdel-Khalek AM. Death anxiety in clinical and non-clinical groups. Death Studies. 2005;29:251–259. doi: 10.1080/07481180590916371. [DOI] [PubMed] [Google Scholar]
- Alvarado KA, Templer DI, Bresler C, Thomas-Dobson S. The relationship of religious variables to death depression and death anxiety. Journal of Clinical Psychology. 1995;51:202–204. doi: 10.1002/1097-4679(199503)51:2<202::aid-jclp2270510209>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Bengtson VL, Cuellar JB, Ragan PK. Stratum contrasts and similarities in attitudes toward death. Journal of Gerontology. 1977;32:76–88. doi: 10.1093/geronj/32.1.76. doi:10.1093/geronj/32.1.76. [DOI] [PubMed] [Google Scholar]
- Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. New England Journal of Medicine. 2000;342:1878–1886. doi: 10.1056/NEJM200006223422506. doi:10.1056/NEJM200006223422506. [DOI] [PubMed] [Google Scholar]
- DeCato TW, Engelberg RA, Downey L, Nielsen EL, Treece PO, Back AL, Curtis JR. Hospital variation and temporal trends in palliative and end-of-life care in the ICU. Critical Care Medicine. 2013;41:1405–1411. doi: 10.1097/CCM.0b013e318287f289. doi:10.1097/CCM.Ob0l3e318287f289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depaola SJ, Griffin M, Young JR, Neimeyer RA. Death anxiety and attitudes toward the elderly among older adults: The role of gender and ethnicity. Death Studies. 2003;27:335–354. doi: 10.1080/07481180302904. [DOI] [PubMed] [Google Scholar]
- Dochterman J, Bulechek GM. Nursing interventions classification (NIC) 4th ed. Mosby; St. Louis, MO: 2004. [Google Scholar]
- Feifel H, Branscomb AB. Who's afraid of death? Journal of Abnormal Psychology. 1973;81:282–288. doi: 10.1037/h0034519. doi:l0.1037/h0034519. [DOI] [PubMed] [Google Scholar]
- Fortner BV, Neimeyer RA. Death anxiety in older adults: A quantitative review. Death Studies. 1999;23:387–411. doi: 10.1080/074811899200920. [DOI] [PubMed] [Google Scholar]
- Friedenberg AS, Levy MM, Ross S, Evans LE. Barriers to end-of-life care in the intensive care unit: Perceptions vary by level of training, discipline, and institution. Journal of Palliative Medicine, 15,404-411. 2012 doi: 10.1089/jpm.2011.0261. doi:10.1089/jpm.2011.0261. [DOI] [PubMed] [Google Scholar]
- Grant M, Wiencek C, Virani R, Uman G, Munevar C, Malloy P, Ferrell B. End-of-life care education in acute and critical care: The California ELNEC project. AACN Advanced Critical Care. 2013;24:121–129. doi: 10.1097/NCI.0b013e3182832a94. doi:l0.1097/NCI.Ob013e3182832a94. [DOI] [PubMed] [Google Scholar]
- Grossman S. Educating RNs regarding palliative care in long-term care generates positive outcomes for patients with end-stage chronic illness. Journal of Hospice & Palliative Nursing. 2007;9:323–328. doi: 10.1097/0l.NJH.0000299316.45256.f3. [Google Scholar]
- Hall MJ, Levant S, DeFrances CJ. Trends in inpatient hospital deaths: National Hospital Discharge Survey, 2000-2010. National Center for Health Statistics Data Brief. 2013;118:1–8. Retrieved from http://www.cdc.gov/nchs/data/databriefs/db 118.pdf. [PubMed] [Google Scholar]
- Keenan GM, Yakel E, Yao Y, Xu D, Szalacha L, Tschannen D, Wilkie DJ. Maintaining a consistent big picture: Meaningful use of a Web-based POC EHR system. International Journal of Nursing Knowledge. 2012;23:119–133. doi: 10.1111/j.2047-3095.2012.01215.x. doi:10.111llj.2047-3095.2012.01215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller JW, Sherry D, Piotrowski C. Perspectives on death: A developmental study. Journal of Psychology. 1984;116:137–142. doi: 10.1080/00223980.1984.9923628. [DOI] [PubMed] [Google Scholar]
- Kisvetrová H, Klugar M, Kabelka L. Spiritual support interventions in nursing care for patients suffering death anxiety in the final phase of life. International Journal of Palliative Nursing. 2013;19:599–605. doi: 10.12968/ijpn.2013.19.12.599. [DOI] [PubMed] [Google Scholar]
- Lehto RH, Stein KF. Death anxiety: An analysis of an evolving concept. Research and Theory for Nursing Practice. 2009;23:23–41. doi: 10.1891/1541-6577.23.1.23. [DOI] [PubMed] [Google Scholar]
- Lo C, Hales S, Zimmermann C, Gagliese L, Rydall A, Rodin G. Measuring death-related anxiety in advanced cancer: Preliminary psychometrics of the Death and Dying Distress Scale. Journal of Pediatric Hematology Oncology. 2011;33(Suppl. 2):S140–S145. doi: 10.1097/MPH.0b013e318230e1fd. doi: 10.1097/MPH.Ob013e3 18230e1fd. [DOI] [PubMed] [Google Scholar]
- Moorhead S, Johnson M, Maas M. Nursing outcomes classification (NOC) (Iowa Outcomes Project) 3rd ed. Mosby; St. Louis, MO: 2004. [Google Scholar]
- North American Nursing Diagnosis Association International . NANDA-1 nursing diagnoses: Definitions and classification, 2003-2004. Author; Philadelphia, PA: 2003. [Google Scholar]
- North American Nursing Diagnosis Association International . Nursing diagnoses: Definitions & classification, 2007-2008. 1st ed. Author; Oxford, UK: 2007. [Google Scholar]
- Peters L, Cant R, Payne S, O'Connor M, McDermott F, Hood K, Shimoinaba K. How death anxiety impacts nurses' caring for patients at the end-of-life: A review of literature. The Open Nursing journal. 2013;7:14–21. doi: 10.2174/1874434601307010014. doi:10.2174/187443460ll307010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz CE, Mazor K, Rogers J, Ma Y, Reed G. Validation of a new measure of concept of a good death. Journal of Palliative Medicine. 2003;6:575–584. doi: 10.1089/109662103768253687. [DOI] [PubMed] [Google Scholar]
- Wen Y-H. Religiosity and death anxiety. The Joumal of Human Resource and Adult Learning. 2010;6(2):31–37. [Google Scholar]
- Wilkie DJ, Judge MK, Wells MJ, Berkley IM. Excellence in teaching end-of-life care: A new multimedia toolkit for nurse educators. Nursing and Health Care Perspectives. 2001;22:226–230. [PubMed] [Google Scholar]
- Wittkowski J. The construction of the multidimensional orientation toward dying and death inventory (MODDI-F). Death Studies. 2001;25:479–495. doi: 10.1080/07481180126858. [DOI] [PubMed] [Google Scholar]


