Abstract
Objective
To develop and evaluate a Critical Warzone Experiences (CWE) scale, a brief measure of warzone experiences associated with the development of posttraumatic stress disorder (PTSD), anxiety, and depression.
Method
The psychometric properties of the CWE were evaluated across three independent samples of Iraq/Afghanistan veterans (combined N = 392).
Results
Despite its brevity (7 items), the CWE exhibited good internal consistency (average α = .83), good temporal stability (1-year test-retest reliability = .73), and a clear unidimensional factor structure in Study 1. Study 2 confirmed the CWE’s factor structure through confirmatory factor analysis, and structural equation modeling demonstrated a strong association between the CWE and post-deployment mental health, β = .49, p < .001. Study 3 provided further support for the validity of the CWE by demonstrating that it was associated with PTSD diagnosis, clinician-rated PTSD symptom severity, and global functional impairment in an independent sample of Iraq/Afghanistan veterans (average validity coefficient = .59).
Conclusion
While replication of these findings in more diverse samples is needed, the preliminary evidence from these studies indicates that the CWE is a brief, reliable, and valid measure of critical warzone experiences among Iraq/Afghanistan war veterans.
In the aftermath of the Vietnam War, researchers began to intensively study the manner in which combat experiences might contribute to posttraumatic stress disorder (PTSD) and other types of mental health problems. As a result, several measures of combat exposure were created, including the widely-used 7-item Combat Exposure Scale (CES; Keane et a., 1989), which was validated with Vietnam veterans. More recently, considerably longer measures of combat exposure and other types of deployment experiences (e.g., post-battle experiences) have been developed, including the U.S. Army and Marine Corps Mental Health Advisory Team’s Combat Experiences Scale (MHAT-CES).
The MHAT-CES has been used in numerous studies of Iraq/Afghanistan veterans (e.g., Booth-Kewley, Larson, Highfill-McRoy, Garland, & Gaskin, 2010; Castro, Bienvenu, Hufmann, & Adler, 2000; Hoge et al., 2004; Hoge, Milliken, Auchterlonie, & Hoge, 2007; Meyer et al., 2013; Morissette et al., 2011; Wright, Cabrera, Eckford, Adler, & Bliese, 2012), including Hoge and colleagues’ (2004) seminal study on mental health problems among Iraq/Afghanistan veterans. Despite the widespread use of the MHAT-CES in published studies of Iraq/Afghanistan veterans, there has been significant variability in the manner in which this measure has been administered. Whereas some studies used versions of the MHAT-CES that contained as many as 44 items and assessed a broad range of warzone experiences (Wright et al., 2011), others used versions with as few as three items and limited content coverage (Hoge et al., 2006; Milliken et al., 2007). Recently, Guyker and colleagues (2013) conducted the first full-scale psychometric study of the MHAT-CES and developed a 28-item version. The authors conducted an exploratory factor analysis and identified three subscales, which they labeled as “Exposure to Combat Environment” (17 items), “Direct Engagement” (7 items), and “Nearness to Serious Injury/Death of Others” (4 items). Internal consistency for the three MHAT-CES subscales identified through factor analysis was good (.94 for Exposure to Combat Environment, .81 for Direct Engagement, and .82 for Nearness to Serious Injury/Death of Others). In addition, supportive evidence was obtained for the internal and external validity of the three subscales. However, the authors acknowledged that the three factors were not clearly distinguishable from each other, noting that the correlations between the three subscales and measures of PTSD, anxiety, and depression were quite similar, raising concerns about their usefulness. Moreover, given the success of the much briefer CES developed for use with Vietnam veterans (Keane et al., 1989), an additional question is whether it is necessary for the MHAT-CES to use four times as many items (i.e., 28 items) as the original CES to assess critical warzone experiences.
Similar concerns can be raised in relation to the Deployment Risk and Resilience Inventory (DRRI; King, King, Vogt, Knight, & Sampler, 2006) and the more recently published Deployment Risk and Resilience Inventory-2 (DRRI-2; Vogt et al., 2013). A clear advantage of the DRRI/DRRI-2 measures is that they have been developed in a systematic fashion and have been validated with Iraq and Afghanistan veterans; however, like the MHAT-CES, the two key DRRI/DRRI-2 scales assessing critical warzone experiences, the Combat Experiences (CE) and Aftermath of Battle (AB) subscales, include a total of 30 items, far more than the original CES. In addition, as with the MHAT-CES, the discriminant validity of the CE and AB subscales is unclear. For example, the DRRI-2 manual reports that the CE and AB subscales have nearly identical correlations with self-reported PTSD symptom severity (.45, .43, respectively), self-reported depression symptom severity (.20, .22, respectively), and self-reported anxiety symptom severity (.23, .22, respectively; Vogt et al., 2012), again raising concerns about the utility of multiple, lengthier scales of warzone experiences.
Objective of the Present Research
The objective of the present research was to develop a brief, reliable, valid, and unidimensional measure of critical warzone experiences for use with Iraq/Afghanistan veterans. We were particularly interested in developing a brief measure that would be strongly associated with the development of PTSD, anxiety, and depression, while also exhibiting good reliability and factor structure. To achieve this objective, we conducted three studies aimed at evaluating a 7-item version of the MHAT-CES that we refer to hereafter as the Critical Warzone Experiences (CWE) scale. The primary objective of Study 1 was to develop the CWE and evaluate its internal consistency, test-retest reliability, factor structure, and concurrent validity with other measures of warzone experiences. The primary objectives of Studies 2 and 3 were to assess the validity of the CWE in relation to our key clinical outcomes of PTSD, anxiety, and depression symptomatology. An additional goal of Study 2 was to use confirmatory factor analysis (CFA) to further examine the factor structure of the CWE. An additional goal of Study 3 was to examine the relationship between the CWE and PTSD diagnosis, clinician-rated PTSD symptom severity scores, and global functional impairment.
Study 1
Participants
Study 1 was comprised of 130 Iraq/Afghanistan veterans enrolled for healthcare within the Department of Veterans Affairs (VA). Veterans with mental health conditions were oversampled to ensure adequate representation. Exclusion criteria included: (1) diagnoses of schizophrenia, another psychotic disorder, or bipolar disorder; (2) current suicidality or homicidality warranting immediate crisis intervention; or (3) recently beginning psychiatric medications or psychotherapy (in order to limit symptom fluctuations related to stopping or starting psychiatric medication or therapy). Veterans with other psychiatric diagnoses were eligible. The majority of participants were male (85%) and had served in the Army (82%). Approximately 63% of the sample was Caucasian and 18% African American. With respect to ethnicity, 26% of participants identified as Latino. Participants’ average age was 38.0 years (SD = 10.8).
Procedures
All procedures were approved by the local Institutional Review Board (IRB) prior to data collection. Veterans completed a baseline assessment as part of a larger longitudinal study that included both a diagnostic interview and completion of self-report measures. A subset of participants (n = 67) completed an annual assessment that included re-administration of the CWE. Interviews were conducted by doctoral-level psychologists or master’s level assessment technicians who completed intensive assessment training. Consensus on all diagnoses was reached with a doctoral-level clinical psychologist with significant PTSD assessment experience.
Measures
A 33-item version of the MHAT-CES similar to the one used by Guyker and colleagues (2013) to develop their 28-item version of the measure was administered to participants and used to develop the CWE, as described in more detail below. As the DRRI-2 was not yet published, the original DRRI (King et al., 2006) CE and AB subscales were used to measure combat experiences and post-battle experiences, respectively, in order to assess the concurrent validity of the CWE. The Clinician Administered PTSD Scale (CAPS; Blake et al., 1995) and PTSD Checklist-Military Version (PCL-M; Weathers et al., 1993) assessed PTSD symptom severity, according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV; APA, 2000). The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) assessed depression symptom severity, and the Depression-Anxiety-Stress Scales (DASS; Lovibond & Lovibond, 1995) assessed severity of depression, anxiety, and stress.
Measure Development
Given our objectives, we made an a priori decision that we would ideally like the measure to contain seven or fewer items in keeping with other brief measures of combat exposure (cf. Keane et al. 1989). Because our primary focus was on developing a measure with high predictive validity, we initially examined the relationship between the 33 MHAT-CES items and the measures of PTSD, depression, and anxiety. We then selected the seven items that had the highest average correlation to represent the seven most critical warzone experiences in relation to PTSD, depression, and anxiety. Next, we examined how well these seven items represented the three MHAT-CES factors identified by Guyker and colleagues (2013) to ensure adequate content validity. This content analysis revealed that the seven items we selected to comprise the CWE included three items from the 17-item MHAT-CES “Exposure to Combat Environment” subscale, three items from the 7-item MHAT-CES “Direct Engagement” subscale, and one item from the 4-item MHAT-CES “Nearness to Serious Injury/Death of Others” subscale (Appendix A). Thus, the proportion of items from the original MHAT-CES subscales and the abbreviated CWE was similar, with 86% of the items for both measures coming from the “Exposure to Combat Environment” and “Direct Engagement” subscales and 14% of the items coming from the “Nearness to Serious Injury/Death of Others” subscale. Having identified seven items with seemingly good predictive and content validity, we proceeded to examine the reliability, factor structure, and concurrent validity of the CWE.
Results
Internal consistency for the CWE was good (α = .80), especially considering its brevity. One-year test-retest reliability for the CWE was also high, r = .73, p < .001, indicating that CWE scores were relatively stable over a long period of time. With respect to concurrent validity, the CWE was strongly associated with both the DRRI-CE, r = .76, p < .001, and the DRRI-AB, r = .72, p < .001, providing good support for its convergent validity.
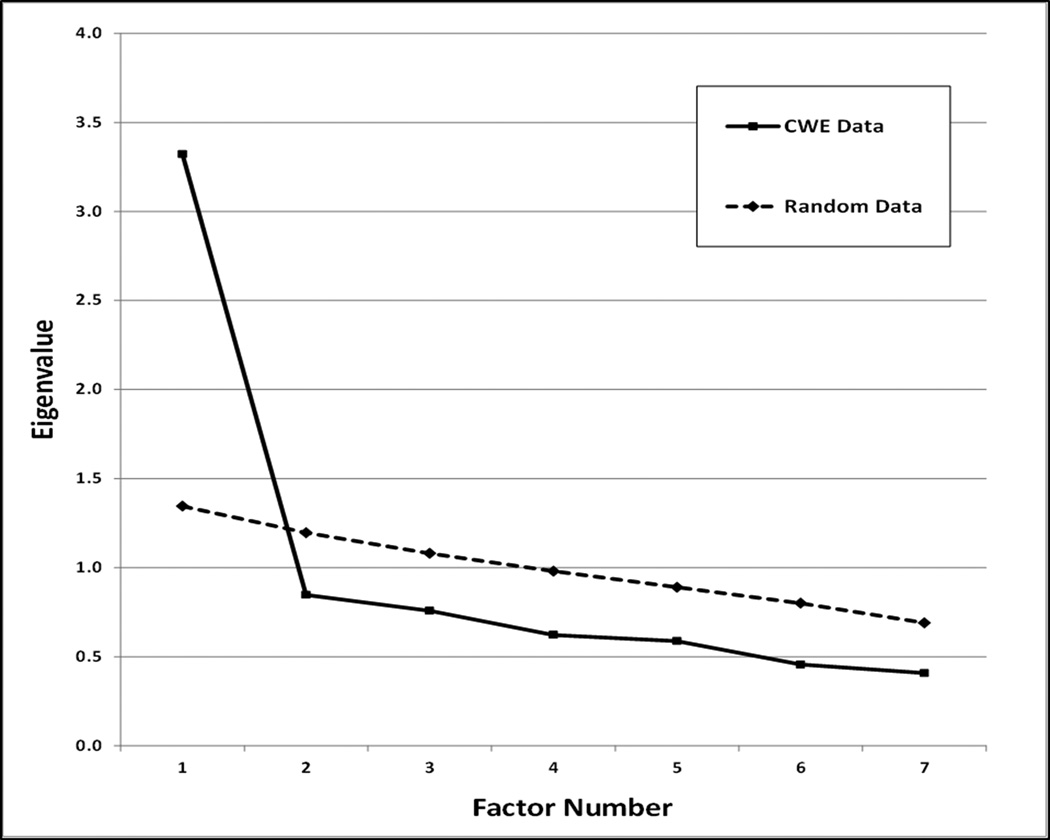
Next, principal component analysis (PCA) was used to explore the factor structure of the CWE. As can be seen in Figure 1, parallel analysis (Horn, 1965) indicated that a single factor should be extracted from the PCA. Examination of the scree plot also supported a one factor solution (Brown, 2006; Cattell, 1966). The single factor extracted from the PCA accounted for approximately 47% of the variance in the scale. Factor loadings are presented in Table 1. In general, factor loadings were high, ranging from .64 (“Saved life of a civilian or soldier”) to .73 (“Seeing ill/injured women or children and unable to help”). The average factor loading was .69.
Figure 1.
Results of the parallel analysis of the Critical Warzone Experiences (CWE) scale from Study 1 (N = 130).
Table 1.
Factor Loadings for the Critical Warzone Experiences (CWE) Scale from Studies 1 and 2
| Factor Loadings from the Principal Component Analysis in Study 1 (N = 130) | ||
| Item | Factor Loading |
|
| 1 | Seeing ill/injured women/children who you were unable to help | .73 |
| 2 | Had a buddy shot or hit who was near you | .71 |
| 3 | Being in threatening situations where you were unable to respond because of rules of engagement | .70 |
| 4 | Witnessing violence within local population or between ethnic groups | .70 |
| 5 | Being directly responsible for the death of an enemy combatant | .69 |
| 6 | Being wounded/injured | .65 |
| 7 | Saved the life of a soldier or civilian | .64 |
| Factor Loadings from the Confirmatory Factor Analysis in Study 2 (N = 212) | ||
| Item | Factor Loading |
|
| 1 | Seeing ill/injured women/children who you were unable to help | .71 |
| 2 | Had a buddy shot or hit who was near you | .79 |
| 3 | Being in threatening situations where you were unable to respond because of rules of engagement | .68 |
| 4 | Witnessing violence within local population or between ethnic groups | .76 |
| 5 | Being directly responsible for the death of an enemy combatant | .77 |
| 6 | Being wounded/injured | .56 |
| 7 | Saved the life of a soldier or civilian | .53 |
Note: All factor loadings shown are fully standardized and statistically significant at p < .01.
Finally, consistent with our item selection strategy, we found that the CWE was positively associated with total symptom severity scores on the CAPS, r = .46, p < .001; PCL-M, r = .47, p < .001; BDI-II, r = .39, p < .001; DASS-D, r = .41, p < .001; DASS-A, r = .42, p < .001; and DASS-S, r = .41, p < .001.
Discussion
The most important findings from Study 1 were that the CWE demonstrated good internal consistency, good temporal stability, and good factor structure. While the magnitude of the CWE’s correlations with the measures of PTSD, anxiety, and depression was also encouraging, we recognized that these correlations may have been artificially inflated due to our selection strategy. Accordingly, we conducted two additional studies to assess the validity of the CWE in two independent samples of Iraq/Afghanistan veterans.
Study 2
Participants
Study 2 was comprised of 212 unique Iraq/Afghanistan veterans. Inclusion/exclusion criteria were identical to those used in Study 1. The majority of participants were male (61%) and had served in the Army (86%). Approximately half (53%) of the participants were Caucasian; 39% were African American. In addition, 16% of participants identified as Latino. Participants’ mean age was 38.8 years (SD = 9.4).
Procedures and Measures
All procedures were approved by the local Institutional Review Board (IRB) prior to data collection. Participants completed the CWE, PCL-M, BDI-II, and DASS in private rooms at a VA Medical Center.
Results
Internal consistency for the CWE was again good (α = .85) in Study 2. In addition, to further examine the factor structure of the CWE, we fit a one-factor CFA model at the item level. The following fit indices were used to evaluate model fit: Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), and Standardized Root Mean Square Residual (SRMR). In general, models that fit data well should have non-significant chi-square statistics, RMSEA values near or below .06, CFI and TLI values near or above .95, and SRMR values near or below .10 (Kline, 2011; Hu & Bentler, 1999). Examination of the fit indices from the CFA revealed that the proposed one-factor model fit the data fairly well, falling within the range of values generally accepted to indicate close fit, χ2 (14) = 23.184, p = .057, RMSEA = .056, CFI = .983, TLI = .975, SRMR = .027. Factor loadings were also high in Study 2 (Table 1), ranging from .53 to .79. As in Study 1, the average factor loading was .69.
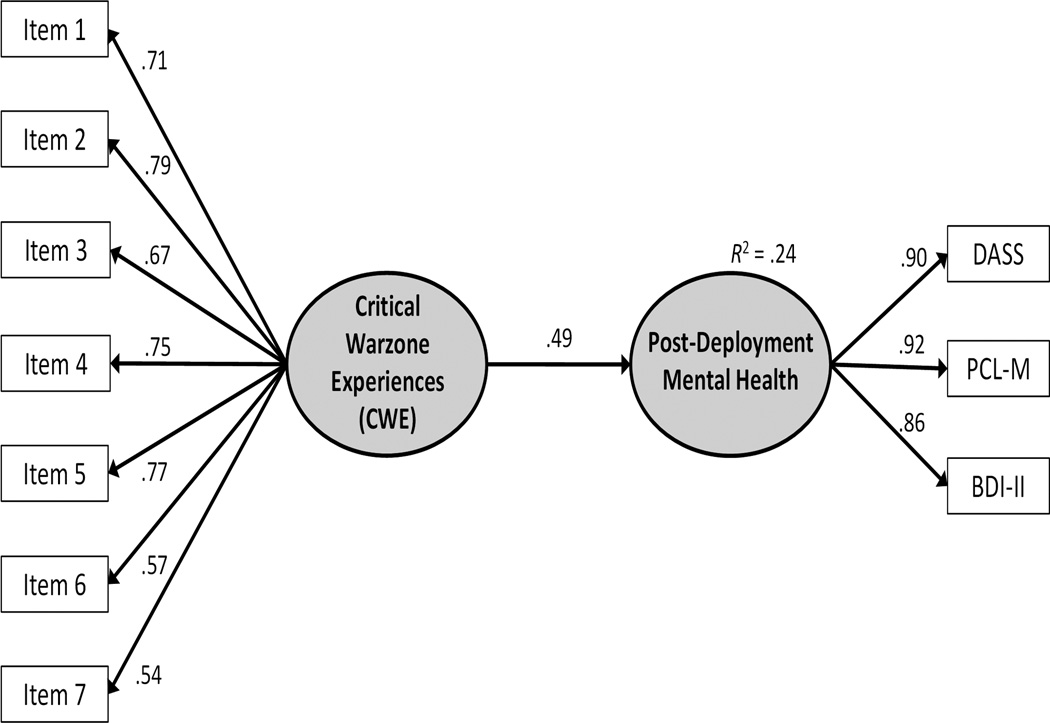
Next, structural equation modeling (SEM) was used to assess the predictive validity of the CWE in relation to PTSD, anxiety, and depression symptoms. In this model, total scores from the PCL-M, BDI-II, and DASS were used to create a post-deployment mental health factor. In turn, this factor was regressed onto the CWE factor (Figure 2). The SEM model exhibited relatively close fit to the data, χ2 (34) = 65.755, p = .0009, RMSEA = .066, CFI = .970, TLI = .961, SRMR = .047. Moreover, the CWE latent factor was strongly associated with the post-deployment mental health latent variable, β = .49, p < .001, R2 = 24%, supporting the predictive validity of the CWE.
Figure 2.
Structural equation model in sample 2 (N = 212). All parameters shown are fully standardized and statistically significant (p < .01). Model fit statistics: χ2 (34) = 65.755, p = .0009, RMSEA = .066, CFI = .970, TLI = .961, SRMR = .047. DASS = 21-item Depression-Anxiety-Stress Scales; PCL-M = PTSD Checklist – Military Version; BDI-II = Beck Depression Inventory – II.
Discussion
Study 2 used CFA and SEM to further examine the psychometric properties of the CWE in an independent sample of Iraq/Afghanistan veterans. Within this framework, the CWE continued to demonstrate good internal consistency and good factor structure. In addition, Study 2 provided clear evidence that the CWE was associated with the key clinical outcomes of PTSD, depression, and anxiety; however, Study 2 was also limited by the fact that all of the measures were self-report instruments.
Study 3
Participants
Study 3 was comprised of 50 unique Iraq/Afghanistan veterans who participated in a larger study concerning the genetics of PTSD. All participants were male, as that was an eligibility criterion for the larger study. In addition, participants were not required to be on a stable dose of medication or psychotherapy to participate in the study. Otherwise, inclusion/exclusion criteria were similar to those used in Studies 1 and 2. The majority of participants (82%) had served in the Army. Fifty percent of the sample met lifetime criteria for a diagnosis of PTSD on the CAPS; 32% met criteria for current PTSD. The majority of the sample was either Caucasian (62%) or African American (34%). Approximately 8% of the sample identified as Latino. Participants’ mean age was 39.7 years (SD = 9.8).
Procedures and Measures
All procedures were approved by the local Institutional Review Board (IRB) prior to data collection. PTSD diagnosis and symptom severity were assessed with the CAPS (Blake et al., 1995). Current PTSD was defined as meeting full criteria within the past month, whereas lifetime PTSD was based on a 30-day period when participants reported experiencing their highest level of military-related PTSD symptoms. Participants also completed the PCL-M, BDI-II, and DASS, in addition to the 36-item self-report version of the World Health Organization Disability Assessment Schedule - II(WHODAS-II; Üstün et al., 2010). The WHODAS-II was used to assess global functional impairment during the previous 30 days.
Results
Internal consistency for the CWE remained high in Study 3 (α = .85) despite the small sample size. Correlations between the CWE and the different symptom severity measures were substantially higher than the correlations observed in Studies 1 and 2. Specifically, the CWE was significantly and positively correlated with the CAPS, r = .71, p < .001; PCL-M, r = .56, p < .001; DASS-Depression, r = .51, p < .001; DASS-Anxiety, r = .57, p < .001; DASS-Stress, r = .58, p < .001; and BDI-II, r = .61, p < .001. The CWE was also significantly correlated with total functional impairment scores on the WHODAS-II, r = .56, p < .001. The CWE’s average validity coefficient across these measures was .59. Similar to Keane et al. (1989), we examined differences in CWE scores by PTSD status. As expected, CWE scores were significantly higher, t = 2.48 (46), p = .017, M diff = 4.7, among veterans currently diagnosed with PTSD, M = 8.9, SD = 8.7, compared with veterans who did not meet current criteria for PTSD, M = 4.2, SD = 4.5. Similarly, veterans who met lifetime criteria for PTSD, M = 8.0, SD = 7.4, reported significantly higher CWE scores, t = 2.57 (46), p = .014, M diff = 4.5, compared with veterans who had never met criteria for PTSD, M = 3.5, SD = 4.5.
Discussion
Study 3 provided additional support for the reliability, as the CWE continued to exhibit good internal consistency. Most notable, however, were the strong associations between the CWE and all of the clinical measures examined, including PTSD diagnosis, clinician-rated PTSD symptom severity, and global functional impairment.
General Discussion
The present research focused on the development and evaluation of a 7-item version of the MHAT-CES which we refer to as the CWE. The CWE appears to possess a number of desirable qualities that we hope will lead to its systematic use in future research and clinical work with returning Iraq/Afghanistan veterans. For example, while the CWE is brief and only takes 1–2 minutes complete, it exhibited good internal consistency across three different samples of Iraq/Afghanistan veterans (average α = .83). The CWE also exhibited good temporal stability (1-year test-retest reliability = .73) and a clear unidimensional factor structure in Studies 1 and 2, demonstrating an average factor loading of .69 across studies.
Most notable, though, were the strong mental health validity coefficients observed for the CWE across all three samples. For example, because of the item selection strategy we employed, we expected that the magnitude of the validity coefficients for the CWE would be artificially inflated and larger than the effects typically observed for a measure of combat exposure in Study 1. This expectation was confirmed, as the average validity coefficient for the CWE (.43) was higher than the average validity coefficient for both the DRRI-CE (.38) and the DRRI-AB (.29) in Study 1; however, in Study 2, we observed that the effect of the CWE on the post-deployment mental health latent variable was even stronger (β = .49, p < .001, R2 = 24%).
Study 3 provided the strongest evidence of the CWE’s association with post-deployment mental health, in which the average validity coefficient for the CWE was .59. To put the magnitude of the latter effect into perspective, Vogt and colleagues (2012) reported in the DRRI-2 manual that the average validity coefficient for both the DRRI-2-CE and the DRRI-2-AB subscales was .29 using three self-report measures of PTSD, depression, and anxiety. In contrast, the CWE—which contains a 75% reduction in items compared with these two scales—had a correlation of .71 with the CAPS, the gold-standard clinician-based interview of PTSD symptom severity.
Thus, while preliminary, the findings from Studies 2 and 3 provide strong support for our item-selection strategy and suggest that the CWE does, in fact, capture seven of the most critical warzone experiences with respect to the development of PTSD, depression, and anxiety among returning Iraq/Afghanistan era veterans. As such, we believe that the CWE can be an important addition to research assessment batteries in studies of Iraq/Afghanistan veterans, providing significant predictive power for relatively little burden. In particular, we believe that the CWE could work well in large epidemiological studies of Iraq/Afghanistan veterans where it is imperative to keep the total number of items in assessment batteries to a minimum. In addition, while preliminary, the CWE’s strong association with PTSD diagnosis, clinician-based symptom severity scores, and a measure of functional impairment suggests that the CWE could also eventually become a useful assessment tool in clinical settings as well.
Study Limitations and Future Directions
Several limitations of the present research should be noted. First, each of the three samples was comprised of Iraq/Afghanistan veterans enrolled within the VA healthcare system, one of which (Study 3) was comprised entirely of male veterans. Thus, additional research with more diverse samples of Iraq/Afghanistan veterans is needed to foster generalizability of the findings to non-treatment seeking veterans and female veterans. It should also be noted that while the CWE was developed and evaluated among Iraq/Afghanistan-era veterans, its items are not specific to these conflicts and may have utility among veterans from a variety of eras. Thus, additional research with veterans from others eras is also warranted.
A second limitation of the present research concerns its focus on PTSD, anxiety, and depression. Because high rates of these conditions are frequently observed among returning Iraq/Afghanistan veterans and because these are the conditions that combat exposure has previously been most strongly associated with, the present research primarily focused on these clinical outcomes. However, there are many other conditions that are significant concerns for returning veterans, including alcohol misuse (e.g., Calhoun, Elter, Jones, Kudler, & Straits-Troster, 2008), suicide (e.g., Kang & Bullman, 2008), traumatic brain injury (Morissette et al., 2011), and violence (e.g., MacManus et al., 2012). Additional research into the relationship between the CWE and such other key outcomes is needed. Finally, although we found good test-retest reliability over a one-year period, it must be noted that as with other retrospective measures of combat exposure, the CWE is subject to recall bias. Prospective research with military personnel prior to their deployments will be necessary to truly assess the impact of combat exposure on long term mental health outcomes.
Summary and Conclusions
In sum, combat exposure and other warzone experiences have been repeatedly associated with PTSD and other mental health disorders among returning veterans (cf. Brewin, Andrews & Valentine, 2000; Ozer, Best, Lipsey & Weiss, 2003). However, there is currently little consensus among researchers about how to measure this key construct among returning Iraq/Afghanistan veterans. The current set of studies provides evidence that the CWE is a brief measure of critical warzone experiences with predictive validity in relation to PTSD, anxiety, and depression symptoms that may be as high, or higher than, other lengthier measures of warzone experiences. The CWE also possesses good internal consistency, good test-retest reliability, and good factor structure. While replication of these findings in more diverse samples is needed, the preliminary evidence gathered from these three studies suggests that the CWE is a significant advancement in the measurement of critical warzone experiences.
Acknowledgments
This research was supported by a Career Development Award-2 (1IK2CX000525-01A1) to Dr. Kimbrel from the Clinical Science Research and Development Service of the Department of Veterans Affairs (VA) Office of Research and Development (ORD), a VA VISN 17 New Investigator Award to Dr. Kimbrel entitled “Genetic and Environmental Effects on PTSD, Depression, and Alcohol Misuse”, a Merit Award (I01RX000304) to Dr. Morissette from the Rehabilitation Research and Development Service of the VA ORD, the VA VISN 17 Center of Excellence for Research on Returning War Veterans, the Central Texas Veterans Health Care System, the Durham Veterans Affairs Medical Center, the VA Mid-Atlantic Mental Illness Research, Education, and Clinical Center, and the Department of Veterans Affairs Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Appendix A
CRITICAL WARZONE EXPERIENCES (CWE) SCALE
| How often did you experience the following during combat? | Never | 1 time | 2–4 times | 5–9 times | 10+ times |
|---|---|---|---|---|---|
| 1. Seeing ill/injured women/children who you were unable to help1 | O | O | O | O | O |
| 2. Had a buddy shot or hit who was near you2……………………….. | O | O | O | O | O |
| 3. Being in threatening situations where you were unable to respond because of rules of engagement1…………………………………… | O | O | O | O | O |
| 4. Witnessing violence within local population or between ethnic groups1 | O | O | O | O | O |
| 5. Being directly responsible for the death of an enemy combatant2……. | O | O | O | O | O |
| 6. Being wounded/injured2……………………………………………… | O | O | O | O | O |
| 7. Saved the life of a soldier or civilian3…………………………………. | O | O | O | O | O |
Scoring: Sum the items using the following values to obtain the total score: Never = 0; 1 time = 1; 2–4 times = 2; 5–9 times = 4; 10+ times = 5.
Note:
Included on the Mental Health Advisory Team – Combat Experiences Scale (MHAT-CES) “Exposure to Combat Environment” subscale;
Included on the MHAT-CES “Direct Engagement” subscale;
Included on the MHAT-CES “Nearness to Serious Injury/Death of Others” subscale.
References
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Booth-Kewley S, Larson GE, Highfill-McRoy RM, Garland CF, Gaskin TA. Correlates of posttraumatic stress disorder symptoms in Marines back from war. Journal of Traumatic Stress. 2010;23:69–77. doi: 10.1002/jts.20485. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine J. Meta-analysis of risk factors for PTSD in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. New York: Guilford; 2006. [Google Scholar]
- Calhoun PS, Elter J, Jones E, Kudler H, Straits-Troster K. Hazardous alcohol use and receipt of risk-reduction counseling among U.S. veterans of the wars in Iraq and Afghanistan. Journal of Clinical Psychiatry. 2008;69:1686–1693. doi: 10.4088/jcp.v69n1103. [DOI] [PubMed] [Google Scholar]
- Castro CA, Bienvenu RV, Hufmann AH, Adler AB. Soldier dimensions and operational readiness in U.S. Army forces deployed to Kosovo. International Review of the Armed Forces Medical Services. 2000;73:191–200. [Google Scholar]
- Cattell RB. The scree test for the number of factors. Multivariate Behavioral Research. 1966;1:245–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- Guyker WM, Donnelly K, Donnelly JP, Dunnam M, Warner GC, Kittleson J, Meier ST. Dimensionality, reliability, and validity of the Combat Experiences Scale. Military Medicine. 2013;178:377–384. doi: 10.7205/MILMED-D-12-00223. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association. 2006;295:1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Horn JL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30:179–185. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kang HK, Bullman TA. Risk of suicide among US veterans after returning from the Iraq or Afghanistan war zones. Journal of the American Medical Association. 2008;300:652–653. doi: 10.1001/jama.300.6.652. [DOI] [PubMed] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, Mora CA. Clinical evaluation of a measure to assess combat exposure. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1:53–55. [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, Sampler RE. Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychology. 2006;18(2):89–120. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling (3rd ed) New York: Guilford; 2011. [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- MacManus D, Dean K, Bakir MA, Iversen AC, Hull L, Fahy T, Fear NT. Violent behaviour in U.K. military personnel returning home after deployment. Psychological Medicine. 2012;42:1663–1673. doi: 10.1017/S0033291711002327. [DOI] [PubMed] [Google Scholar]
- Meyer EC, Morissette SB, Kimbrel NA, Kruse MI, Gulliver SB. Acceptance and Action Questionnaire – II scores as a predictor of posttraumatic stress disorder symptoms among war Veterans. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:521–528. [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. Journal of the American Medical Association. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Morissette SB, Woodward M, Kimbrel NA, Meyer EC, Kruse MI, Dolan S, Gulliver SB. Deployment-related TBI, persistent post-concussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabilitation Psychology. 2011;56:340–350. doi: 10.1037/a0025462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey T, Weiss D. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Üstün TB, Chatterji S, Kostanjsek N, Rehm J, Kennedy C, Epping-Jordan J, Pull C in collaboration with WHO/NIH Joint Project. Developing the World Health Organization Disability Assessment Schedule 2.0. Bulletin of the World Health Organization. 2010;88:815–823. doi: 10.2471/BLT.09.067231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt D, Smith BN, King LA, King DW, Knight J, Vasterling JJ. Deployment Risk and Resilience Inventory-2 (DRRI-2): An updated tool for assessing psychosocial risk and resilience factors among service members and veterans. Journal of Traumatic Stress. 2013;26:710–717. doi: 10.1002/jts.21868. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist (PCL): Reliability, validity, and diagnostic utility; Poster presented at the 9th annual meeting of the International Society of Traumatic Stress Studies; San Antonio, TX.1993. [Google Scholar]
- Wright KM, Cabrera OA, Eckford RD, Adler AB, Bliese PD. The impact of predeployment functional impairment on mental health after combat. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4:260–269. [Google Scholar]