Abstract
The aim of the study is to assess the prognostic value of different volume-based calculations of tumor metabolic activity in the initial assessment of patients with high-grade bone sarcomas (BS) and soft tissue sarcomas (STS) using F-18 FDG PET/CT.
A single-site, retrospective study from 2002 to 2012 including 92 patients with histologically verified high-grade BS (N = 37) or STS (N = 55). All patients underwent a pretreatment F-18 FDG PET/CT scan. Clinical data were registered. Measurements of the accuracy of metabolic tumor volume with a preset threshold of 40% of the maximum standardized uptake value of primary tumor (MTV40%) and total lesion glycolysis (TLG) as prognostic variables and identification of optimal discriminating cut-off values were performed through ROC curve analysis. Patients were grouped according to the cut-off values. All deaths were considered an event in survival analysis. Kaplan–Meier survival estimates and log-rank test were used to compare the degree of equality of survival distributions. Prognostic variables with related hazard ratios (HR) were assessed using Cox proportional hazards regression analysis.
Forty-one of 92 patients died during follow-up (45%; 12 BS and 29 STS). Average survival for included patients was 6.5 years (95% CI 5.8–7.3 years) and probability of 5-year survival was 52%. There was a high-significant accuracy of TLG and MTV40% as prognostic variables when looking on all patients and during subgroup analysis. AUCs were higher for TLG than for MTV40%. TLG above optimal cut-off value was the only variable which was independently prognostic for survival throughout multivariate regression analysis of all included patients (P = 0.01, HR 4.78 [95% CI 1.45–15.87]) and subgroup analysis (BS: P = 0.04, HR 11.11 [95% CI 1.09–111.11]; STS: P < 0.05, HR 3.37 [95% CI 1.02–11.11]). No significant results were demonstrated for MTV40%.
Volume-based F-18 FDG PET/CT imaging markers in terms of pretreatment estimation of TLG provide supplemental prognostic information to histologic grading, with significant independent properties for prediction of overall survival in patients with high-grade BS or STS.
INTRODUCTION
Bone and soft tissue sarcomas (BS and STS) are a rare, diverse group of tumors, which exhibit mesenchymal differentiation. Sarcomas only comprise ∼1% of all cancers.1 However, with relatively high reported 5-year mortality rates up to 50%2 and extensive diversity in terms of tumor histology, metastatic potential, and outcome,1,3,4 diagnosis and treatment of these patients are challenging. Thus, it becomes obvious that correct staging of disease in these patients has an essential role in predicting clinical outcome and guiding treatment. For prediction of prognosis, both the Musculoskeletal Tumor Society (MSTS)5 and the American Joint Committee of Cancer (AJCC) staging system 6,7 for malignant primary bone and soft-tissue lesions are implemented in the clinical routine. Even though these guidelines include a number of tumor features, nodal status, and distant organ metastasis, the issue of a substantial variety in patient outcome—even within the same tumor grade—cannot be ignored. Correct tumor grading requires representative tissue from the least differentiated area in the tumor, which may not be achieved in heterogeneous tumors. In addition, tumor grading depends on the pathologist's judgment and is a subjective variable. Metabolic imaging with positron emission tomography (PET) applying the fluorine-18 radiolabeled glucose analog fluoro-2-deoxy-D-glucose (F-18 FDG) might overcome these shortcomings and has gained a supplemental role to histological characteristics in the assessment of patients with sarcoma. This imaging modality exerts properties in terms of assessing tumor behavior, as it allows noninvasive, 3-dimensional visualization and quantification of tumor glucose metabolism in vivo.8,9
Pretreatment semiquantitative estimation of primary tumor glucose metabolism using the maximum standardized uptake value (SUVmax) normalized to body weight has been suggested being a significant prognostic factor for overall and progression-free survival in sarcoma patients.10–18 As SUVmax purely represents the maximum value of a single voxel in the acquired imaging data, it does not reflect important prognostic tumor properties such as tumor heterogeneity as well as tumor size and burden. Volume-based F-18 FDG PET imaging markers in terms of metabolic tumor volume (MTV) and total lesion glycolysis (TLG) have been introduced to overcome the obvious limitations of SUVmax, with several studies reporting significant prognostic properties in terms of prediction of treatment response and survival in a diversity of solid tumors.19–23 In patients with bone and soft-tissue sarcoma, the amount of clinical evidence is minimal and conflicting.11,12,15,24 Consequently, it has proven difficult to standardize the implementation of this quantification tool in the diagnostic work-up and follow-up of patients with sarcoma.25,26
The present study compares the prognostic value of volume-based semi-quantitative calculations of tumor metabolic activity as determined by MTV and TLG using F-18 FDG PET/computed tomography (CT) in the initial assessment of patients with histologically verified high-grade bone or soft-tissue sarcoma.
METHODS
Study Population and Design
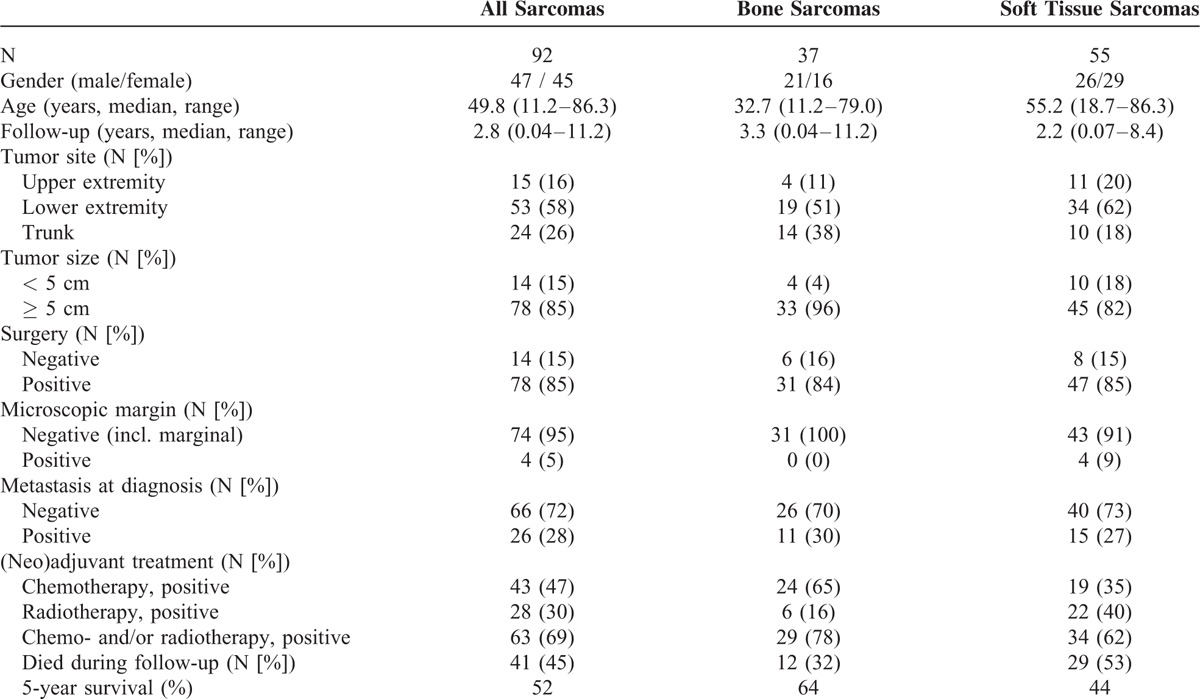
A single-site, retrospective study from July 1st 2002 to December 31st 2012 including 92 consecutive patients, with clinical characteristics and study design as previously reported27 (47 men; 45 women; median age 49.8 [11.2–86.3] years; Table 1). The patients were referred for further evaluation and/or surgical treatment and were included in the study according to the following criteria: first, histologically verified high-grade BS (N = 37) or STS (N = 55) according to either the French Federation of Cancer Centers Sarcoma Group (FNCLCC) grading system (STS)28 or the grading recommendations of the College of American Pathologists (BS),29 second, no previous history of malignancy, third, underwent an on-site pre-operative 18F-FDG PET/CT scan for staging, and fourth, a minimum follow-up period of 1 year for survived patients. Medical records, imaging examinations, and histopathology were reviewed. The histological classification of the included bone sarcomas was: osteosarcoma N = 20, Ewing sarcoma N = 6, chondrosarcoma N = 5, others N = 6. Regarding the included soft tissue sarcomas the histological subtypes were distributed as follows: myogenic sarcoma N = 16, synovial sarcoma N = 9, malignant peripheral nerve sheath tumor N = 6, liposarcoma N = 5, angiosarcoma N = 4, myxofibrosarcoma N = 3, undifferentiated pleomorphic sarcoma N = 2, others N = 10. Only patients with Ewing sarcoma/primitive neuroectodermal tumor (PNET) and osteosarcoma received preoperative chemotherapy (these patients also received postoperative chemotherapy). No pre-PET chemotherapy was allowed. The treatment protocol, which also included radiotherapy for prevention of local recurrence in patients with marginal or intralesional tumor resection, was not changed during the study period. The study was approved by the Danish Data Protection Agency (journal number 2011-41-5734).
TABLE 1.
Clinical Characteristics. Previously Reported by Andersen et al 201527
F-18 FDG PET/CT: Acquisition and Analysis
Routine F-18 FDG PET/CT was performed with dedicated PET/CT scanners (GE Discovery LS, GE Healthcare, Waukesha, WI; Siemens Biograph Sensation 16, Siemens Biograph 40 TruePoint, Siemens Biograph 64 TruePoint, Siemens Biograph mCT-S 64, Siemens Medical Solutions, Knoxville, TN). Patients fasted for a minimum of 6 h before FDG injection. Before June 1st 2010 a dose of 400 MBq F-18 FDG was injected intravenously 60 min before the scan; hereafter a dose of 4 MBq/kg body weight was used. The PET emission scan was performed for 2.5 to 5 min per bed position depending on the scanner type and the body mass index of the patients. Patients were scanned from the base of the skull to the distal side of the tumor, at least including the proximal femora. Covering the same area, a contrast-enhanced CT was performed (500 mL Ioxitalamat solution 12.6 mg/mL administered orally 30 min before the scan and intravenous Optiray® 300 mg/mL at 1.5–2.5 mL/s with a delay of 60–80 s). CT data were used for attenuation correction of the PET emission data. No separate low-dose CT scan for attenuation correction was performed in order to reduce the risk of movement artifacts due to a prolonged examination time.30 The acquired PET and CT data were reconstructed in 3 dimensions. During the study period our institution switched from a standard iterative reconstruction (AW-OSEM: 4 iterations and 8 subsets with 4 mm Gaussian postfilter) of PET images toward using a Point Spread Function reconstruction (3 iterations and 21 subsets followed by a 2 mm Gaussian postfilter). Images (PET, CT, and fused) were reviewed applying a dedicated workstation and software (syngo® via, Siemens Healthcare, Forchheim, Germany). Interpretations were done by a specialist in nuclear medicine and a specialist in diagnostic radiology in consensus. A volume of interest (VOI) was drawn including primary tumor (Figure 1), and SUV normalized to body weight was calculated as the VOI activity (MBq/mL) / (injected dose [MBq] / body weight [g]). SUVmax was the single maximum pixel value in the VOI. An isoactivity contour was automatically drawn in the VOI using a preset margin threshold of 40% of SUVmax (metabolic tumor volume [MTV40%]). TLG was defined as MTV40% multiplied with the mean SUV of the MTV40%.19
FIGURE 1.
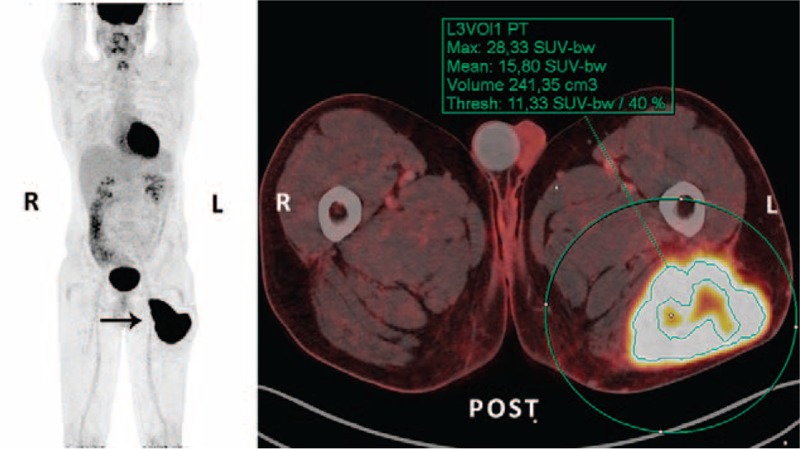
36-year-old male with high-grade soft tissue sarcoma (subclassification not possible; tumor grade III [FNCLCC grading system]) located in the posterior musculature on the left femur (arrow). The patient underwent a preoperative F-18 FDG PET/CT scan for staging, which showed no metastatic disease. For volume-based calculations of tumor metabolic activity, a volume-of-interest (VOI) was manually drawn on the acquired PET images (green circle), and estimation of the maximum standardized uptake value of primary tumor was performed (SUVmax 28.33 g/mL). Dedicated software and a preset threshold of 40% of SUVmax of primary tumor (SUV 11.33 g/mL) was used to define the metabolic tumor volume (irregular green shape; MTV40% 241.35 mL), and the mean standardized uptake value of the MTV40% was determined (SUVmean 15.80 g/mL). The 2 latter variables were used for calculation of total lesion glycolysis (TLG = MTV40% × [SUVmean of the MTV40%] = 3813.33 g). A wide resection of tumor (12 × 7 × 10 cm) was achieved. No adjuvant therapy was administered. One year after surgery the patient presented with metastatic disease and he died 2 months later. CT = computed tomography, F-18 = fluorine-18, FDG = fluoro-2-deoxy-D-glucose, FNCLCC = French Federation of Cancer Centers Sarcoma Group, MTV = metabolic tumor volume, PET = positron emission tomography, SUVmax = maximum standardized uptake value, TLG = total lesion glycolysis, VOI = volume of interest.
Clinical Endpoints
Overall survival was set as the primary endpoint. Survival time was defined as the period from the date of the pretreatment F-18 FDG PET/CT scan to the date of death; for survived patients the date on which data regarding patient survival were obtained from the Danish Centralized Civil Register (April 11th 2014).
STATISTICS
Statistical analyses were performed using IBM® SPSS® Statistics 19.0 (SPSS Inc., IBM, Somers, NY) and MedCalc® version 12.7.1.0 (MedCalc Software, Ostend, Belgium) on data registered in the following groups: (1) all included patients, (2) patients with BS, (3) patients with STS. Measurements of the accuracy of MTV40% and TLG as prognostic variables and identification of optimal discriminating cut-off values were performed through receiver operating characteristic (ROC) curve analysis with use of the Youden Index algorithm. Patients were grouped according to the cut-off values. All deaths (N = 41) were considered an event in the survival analysis and the patients were censored at the end of their follow-up. Kaplan–Meier survival estimates and the log-rank test were used to compare the degree of equality of survival distributions. Prognostic variables with related hazard ratios (HR) were assessed applying Cox proportional hazards regression analysis. The following categorical variables were included: gender, tumor size, surgery, metastasis at diagnosis, MTV40%, and TLG. P values < 0.05 were considered statistically significant.
RESULTS
Clinical characteristics are presented in Table 1. The median follow-up period was 2.8 years (range 0.04–11.2 years). A total of 41 of 92 patients died during follow-up (45%; 12 BS and 29 STS patients). Average survival for all included patients was 6.5 years (95% CI 5.8–7.3 years) and the probability of 5-year survival was 52%. There was a significant difference (P < 0.05) in both probability of 5-year survival and average survival between patients with BS (64%; 7.8 years [95% CI 6.2–9.4 years]) and STS (44%; 4.5 years [95% CI 3.5–5.5 years]).
ROC Curve Analysis
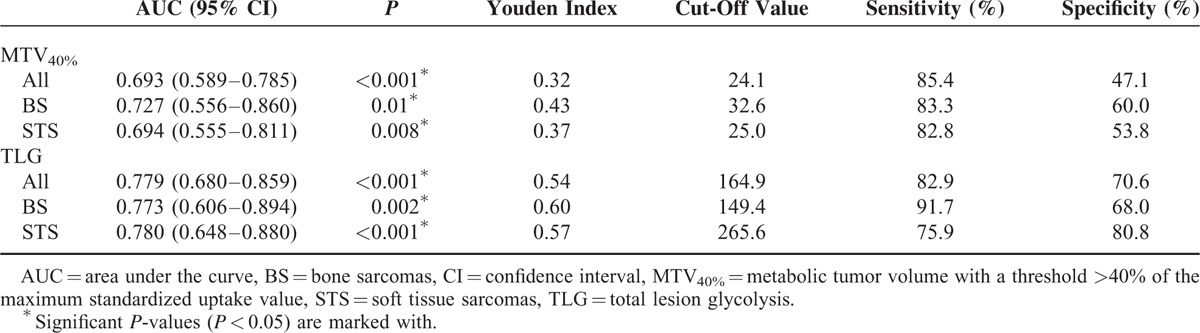
ROC curve analysis of overall survival with area under the curve (AUC) data and optimal discriminating cut-off values are presented in Figure 2 and Table 2. The AUCs were significant for both MTV40% (P < 0.001) and TLG (P < 0.001) when looking on all patients as well as during subgroup analysis of patients with BS or STS. The AUCs were consistently higher for TLG compared to MTV40% (all patients: 0.779 vs 0.693; BS: 0.773 vs 0.727; STS: 0.780 vs 0.694).
FIGURE 2.
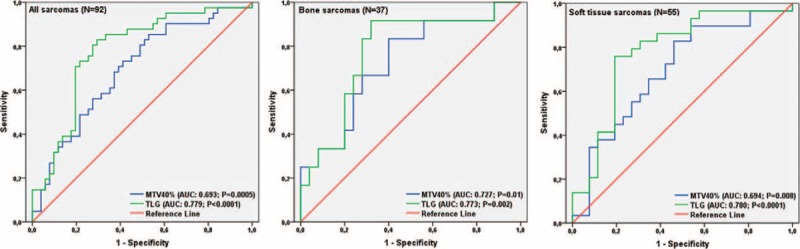
ROC curve analysis of all included patients (N = 92) and subgroups of patients with BS (N = 37) or STS (N = 55), with measurements of the accuracy of metabolic tumor volume with a preset threshold of 40% of the maximum standardized uptake value of primary tumor (MTV40%) and total lesion glycolysis (TLG) as prognostic variables. BS = bone sarcoma, MTV = metabolic tumor volume, ROC = receiver operating characteristic, STS = soft tissue sarcoma, TLG = total lesion glycolysis.
TABLE 2.
ROC Curve Analysis
Kaplan–Meier Survival Estimates
Kaplan–Meier survival data for ungrouped data and grouped data according to the estimated optimal cut-off values are presented in Figure 3 and Table 3. When dividing all patients into 2 groups below and above cut-off value for MTV40% (24.1), 6 out of 30 and 35 out of 62 patients died during follow-up, respectively. Probabilities of 5-year survival were 79% and 40%, and average survival was 9.1 years (95% CI 7.5–10.6 years) and 5.4 years (95% CI 4.1–6.6 years) in the 2 groups (P = 0.004). When dividing all patients into 2 groups below and above the cut-off value for TLG (164.9), 7 out of 43 and 34 out of 49 patients died during follow-up. Probabilities of 5-year survival were 83% and 24%, and average survival was 9.5 years (95% CI 8.3–10.6 years) and 3.6 years (95% CI 2.5–4.6 years), respectively (P < 0.001).
FIGURE 3.
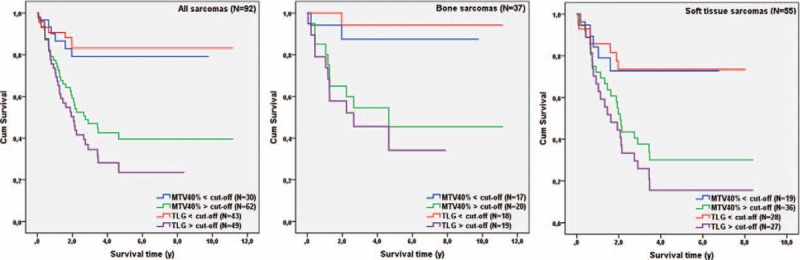
Kaplan–Meier survival curves for all included patients (N = 92) and subgroups of patients with BS (N = 37) or STS (N = 55). Data were grouped according to the optimal discriminating cut-off value for MTV40% and TLG determined with ROC curve analysis. BS = bone sarcoma, MTV = metabolic tumor volume, ROC = receiver operating characteristic, STS = soft tissue sarcoma, TLG = total lesion glycolysis.
TABLE 3.
Survival Data (Ungrouped and Grouped Data [Above/Below Optimal Cut-Off Value])
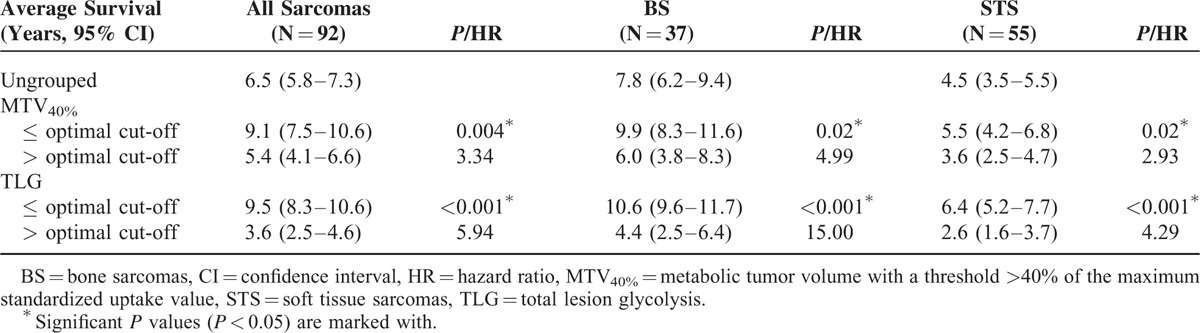
When analyzing data from patients with BS, 2 out of 17 and 10 out of 20 patients died during follow-up, when patients were grouped according to the optimal cut-off value for MTV40% (32.6). Estimated 5-year survival was 87% below cut-off and 46% above, with an average survival of 9.9 years (95% CI 8.3–10.6 years) and 6.0 years (95% CI 3.8–8.3 years), respectively (P = 0.02). When grouping patients with BS below and above the optimal cut-off value for TLG (149.4), probabilities of 5-year survival were 94% (1 out of 18 patients died during follow-up) and 34% (11 out of 19 patients died during follow-up), respectively. There was a significant difference in average survival (10.6 years [95% CI 9.6–11.7 years] below cut-off vs 4.4 years [95% CI 2.5–6.4 years] above cut-off; P < 0.001).
In subgroup analysis of patients with STS probabilities of 5-year survival, when data was grouped below (5 out of 19 patients died during follow-up) and above (24 out of 36 patients died during follow-up) the optimal cut-off values for MTV40% (25.0) were 73% and 30%, respectively. Significant differences in average survival were registered, as average survival was 5.5 years (95% CI 4.2–6.8 years) below the cut-off value and 3.6 years (95% CI 2.5–4.7 years) above (P = 0.02). Regarding TLG, probabilities of 5-year survival below and above the optimal cut-off value (265.6) were 74% and 16%, respectively. Totally 7 out of 28 and 22 out of 27 patients died during follow-up, respectively. Average survival was 6.4 years (95% CI 5.2–7.7 years) below cut-off and 2.6 years (95% CI 1.6–3.7 years) above (P < 0.001).
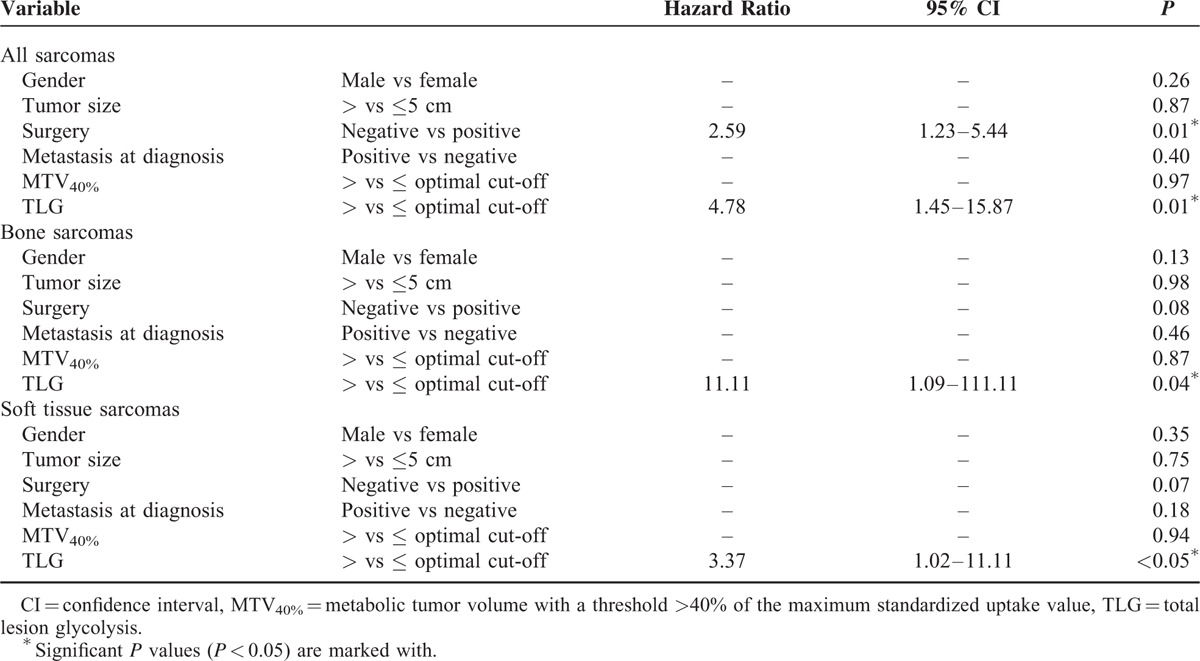
Prognostic Values of MTV40% and TLG
Data from Cox proportional hazards regression analysis with variables affecting overall survival in multivariate analyses are presented in Table 4. TLG above the optimal discriminating cut-off value was the only variable which was significant as a prognostic variable for survival throughout analysis of all included patients (P = 0.01, HR 4.78 [95% CI 1.45–15.87]) as well as subgroup analysis of patients with BS (P = 0.04, HR 11.11 [95% CI 1.09–111.11]) or STS (P < 0.05, HR 3.37 [95% CI 1.02–11.11]). No significant results were demonstrated for MTV40%. Performed surgery was significant as prognostic variable when analyzing all included patients (P = 0.01; HR: 2.59 [95% CI 1.23–5.44]) but not during subgroup analysis.
TABLE 4.
Variables Affecting Overall Survival in Multivariate Analyses
DISCUSSION
The main finding of the present study is the identification of pretherapeutic estimation of TLG using F-18 FDG PET/CT as an independent prognostic variable for overall survival both in patients with high-grade BS and STS. We have previously reported the shortcomings of the prognostic use of SUVmax and tumor-to-background uptake ratio in the same study cohort, especially in subgroup analysis of patients with high-grade BS.27 The volume-based F-18 FDG PET imaging markers MTV and TLG attempt to overcome the limitations of SUVmax, by including several important prognostic tumor characteristics, such as heterogeneity, size, and burden; that is, an inclusion of the total volume and total activity of metabolically active tumor cells. This theoretical advantage has been verified by several studies reporting significant prognostic properties in terms of prediction of treatment response and survival in a diversity of solid tumors.19–23
In patients with STS, reported data regarding the application of TLG and MTV are conflicting. One study reported the superiority of TLG to SUVmax as a reliable predictor of progression-free survival in STS.11 However, their clinical endpoint differed from our study, and their inclusion of patients in terms of histologic tumor grading was more heterogeneous. Our study is in discrepancy with a study by Hong et al,15 which concluded that the aforementioned volume-based F-18 FDG PET imaging markers may not provide additional prognostic information in patients with STS. They explained their results as a possible consequence to tumor necrosis (87% of included patients had tumor necrosis), which lowers the values of volume-based F-18 FDG PET imaging markers, but does not affect the maximum value in a single voxel (ie, SUVmax). We did not include this variable in our study. Their study population also differed to the present study, as patients with low-grade STS were included.
Costelloe et al12 were the first reporting data on the prognostic value of volume-based FDG imaging markers in osteosarcoma, where high TLG before chemotherapy was associated with poor survival. Our results are in accordance with this, even though our study cohort embraces all high-grade bone sarcomas and not only osteosarcomas. However, Byun and co-workers24 failed to demonstrate an independent prognostic value of pretherapeutic estimation of TLG in AJCC stage II osteosarcomas of the extremities. Instead, MTV with a fixed SUV threshold of 2.0 was predictive of metastasis-free survival in their cohort, which is in conflict with the results presented in the present study. This underlines the need for standardization in the estimation of volume-based FDG PET imaging markers, especially in such a heterogeneous group of tumors as sarcomas. In our study, measurements of the accuracy of MTV40% as prognostic variable for overall survival were in general lower than for TLG, and importantly, MTV40% did not have independent predictive value for overall survival in multivariate regression analyses. This is in accordance with the majority of the aforementioned studies of patients with STS or BS, and could be explained by the limitation of MTV to reflect the most malignant/metabolic active cell component of the tumor.
In an oncological setting, the introduction of FDG PET has achieved considerable impact, as the possibility of noninvasive estimation of tumor metabolic activity is attractive in terms of treatment guidance. In many cases, it also supports the predication of patient outcome. Concerns regarding the statistical weakness of quantitative F-18 FDG PET imaging markers have been introduced, including poor reproducibility of tumor volume estimates used for calculation of both MTV and TLG.31 Despite this and the fact that we in the present study used several PET/CT scanners and there were slight on-site changes in the F-18 FDG PET/CT scan protocol in terms of reconstruction algorithm and injected dose of the tracer during the inclusion period, we consider our results to be valid.32
Due to the unspecific nature of the radiolabeled glucose analog FDG, one of the limitations of this tracer is to discriminate inflammatory tissue from malignant tissue. Consequently, incorrect delineation of tumor boundaries may occur. We did not predefine a standardized method to delineate the tumor in our study, which may result in an inaccurate estimation of volume-based F-18 FDG PET imaging markers. Most reports regarding the prognostic value of F-18 FDG PET imaging markers in terms of survival of patients with sarcomas are limited by the low incidence of these tumors and their retrospective design, that also being the case in our study. In an optimal setting, a prospective study, which also takes the heterogeneity in tumor origin and localization, intra- and intertumoral properties, as well as tumor size and burden into account, is warranted. However, one of the strengths of the present study is the ability to identify prognostic variables supplemental to tumor grading—also during subgroup analyses—as it includes a relatively large number of patients with histologically verified high-grade BS or STS only.
In this study, which includes patients with histologically verified high-grade bone or soft tissue sarcomas, volume-based F-18 FDG PET/CT imaging markers in terms of pretreatment quantification of total lesion glycolysis provide supplemental predicative information to histologic grading. We conclude that estimation of total lesion glycolysis has the potential to be recognized as an independent prognostic marker for overall survival in this group of patients. In the current setting, we do not recommend the use of estimated metabolic tumor volume with a margin threshold of 40% of the maximum standardized uptake value of primary tumor for survival prognostics. Further studies should focus on the clinical utility of volume-based F-18 FDG PET imaging markers, especially TLG.
Footnotes
Abbreviations: AJCC = American Joint Committee of Cancer, AUC = area under the curve, BS = bone sarcoma, CI = confidence interval, CT = computed tomography, F-18 = fluorine-18, FDG = fluoro-2-deoxy-D-glucose, FNCLCC = French Federation of Cancer Centers Sarcoma Group, HR = hazard ratio, MSTS = Musculoskeletal Tumor Society, MTV = metabolic tumor volume, PET = positron emission tomography, PNET = primitive neuroectodermal tumor, ROC = receiver operating characteristic, STS = soft tissue sarcoma, SUVmax = maximum standardized uptake value, TLG = total lesion glycolysis, VOI = volume of interest.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Fletcher CDM, Bridge JA, Hogendoorn PCW, et al. World Health Organisation Classification of Tumours of Soft Tissue and Bone. 4th edLyon: IARC Press; 2013. [Google Scholar]
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics. CA Cancer J Clin 2012; 62:10–29. [DOI] [PubMed] [Google Scholar]
- 3.Coindre JM, Terrier P, Guillou L, et al. Predictive value of grade for metastasis development in the main histologic types of adult soft tissue sarcomas: a study of 1240 patients from the French Federation of Cancer Centers Sarcoma Group. Cancer 2001; 91:1914–1926. [DOI] [PubMed] [Google Scholar]
- 4.Skubitz KM, D’Adamo DR. Sarcoma. Mayo Clin Proc 2007; 82:1409–1432. [DOI] [PubMed] [Google Scholar]
- 5.Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res 1980; 153:106–120. [PubMed] [Google Scholar]
- 6.Edge S, Byrd DR, Compton CC, Greene FL, Trotti A. AJCC: Soft tissue sarcoma. AJCC Cancer Staging Manual. 7th ed2010; New York, NY: Berlin, Springer, 291-298. [Google Scholar]
- 7.Edge S, Byrd DR, Compton CC, Greene FL, Trotti A. AJCC: Bone. AJCC Cancer Staging Manual. 7th ed2010; New York, NY: Berlin, Springer, 281-290. [Google Scholar]
- 8.Benz MR, Tchekmedyian N, Eilber FC, et al. Utilization of positron emission tomography in the management of patients with sarcoma. Curr Opin Oncol 2009; 21:345–351. [DOI] [PubMed] [Google Scholar]
- 9.Gambhir SS. Molecular imaging of cancer with positron emission tomography. Nat Rev Cancer 2002; 2:683–693. [DOI] [PubMed] [Google Scholar]
- 10.Brenner W, Conrad EU, Eary JF. FDG PET imaging for grading and prediction of outcome in chondrosarcoma patients. Eur J Nucl Med Mol Imaging 2004; 31:189–195. [DOI] [PubMed] [Google Scholar]
- 11.Choi ES, Ha SG, Kim HS, et al. Total lesion glycolysis by 18F-FDG PET/CT is a reliable predictor of prognosis in soft-tissue sarcoma. Eur J Nucl Med Mol Imaging 2013; 40:1836–1842. [DOI] [PubMed] [Google Scholar]
- 12.Costelloe CM, Macapinlac HA, Madewell JE, et al. 18F-FDG PET/CT as an indicator of progression-free and overall survival in osteosarcoma. J Nucl Med 2009; 50:340–347. [DOI] [PubMed] [Google Scholar]
- 13.Eary JF, O'Sullivan F, Powitan Y, et al. Sarcoma tumor FDG uptake measured by PET and patient outcome: a retrospective analysis. Eur J Nucl Med Mol Imaging 2002; 29:1149–1154. [DOI] [PubMed] [Google Scholar]
- 14.Fuglo HM, Jorgensen SM, Loft A, et al. The diagnostic and prognostic value of (1)(8)F-FDG PET/CT in the initial assessment of high-grade bone and soft tissue sarcoma. A retrospective study of 89 patients. Eur J Nucl Med Mol Imaging 2012; 39:1416–1424. [DOI] [PubMed] [Google Scholar]
- 15.Hong SP, Lee SE, Choi YL, et al. Prognostic value of 18F-FDG PET/CT in patients with soft tissue sarcoma: comparisons between metabolic parameters. Skeletal Radiol 2014; 43:641–648. [DOI] [PubMed] [Google Scholar]
- 16.Schuetze SM, Rubin BP, Vernon C, et al. Use of positron emission tomography in localized extremity soft tissue sarcoma treated with neoadjuvant chemotherapy. Cancer 2005; 103:339–348. [DOI] [PubMed] [Google Scholar]
- 17.Schwarzbach MH, Hinz U, Dimitrakopoulou-Strauss A, et al. Prognostic significance of preoperative [18-F] fluorodeoxyglucose (FDG) positron emission tomography (PET) imaging in patients with resectable soft tissue sarcomas. Ann Surg 2005; 241:286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skamene SR, Rakheja R, Dalhstrom KR, et al. Metabolic activity measured on PET/CT correlates with clinical outcomes in patients with limb and girdle sarcomas. J Surg Oncol 2014; 109:410–414. [DOI] [PubMed] [Google Scholar]
- 19.Larson SM, Erdi Y, Akhurst T, et al. Tumor treatment response based on visual and quantitative changes in global tumor glycolysis using PET-FDG imaging. The visual response score and the change in total lesion glycolysis. Clin Positron Imaging 1999; 2:159–171. [DOI] [PubMed] [Google Scholar]
- 20.Lee JW, Kang CM, Choi HJ, et al. Prognostic value of metabolic tumor volume and total lesion glycolysis on preoperative 18F-FDG PET/CT in patients with pancreatic cancer. J Nucl Med 2014. [DOI] [PubMed] [Google Scholar]
- 21.Liao S, Penney BC, Wroblewski K, et al. Prognostic value of metabolic tumor burden on 18F-FDG PET in nonsurgical patients with non-small cell lung cancer. Eur J Nucl Med Mol Imaging 2012; 39:27–38. [DOI] [PubMed] [Google Scholar]
- 22.Pak K, Cheon GJ, Nam HY, et al. Prognostic value of metabolic tumor volume and total lesion glycolysis in head and neck cancer: a systematic review and meta-analysis. J Nucl Med 2014. [DOI] [PubMed] [Google Scholar]
- 23.Zhang H, Wroblewski K, Liao S, et al. Prognostic value of metabolic tumor burden from F-FDG PET in surgical patients with non-small-cell lung cancer. Acad Radiol 2013; 20:32–40. [DOI] [PubMed] [Google Scholar]
- 24.Byun BH, Kong CB, Park J, et al. Initial metabolic tumor volume measured by 18F-FDG PET/CT can predict the outcome of osteosarcoma of the extremities. J Nucl Med 2013; 54:1725–1732. [DOI] [PubMed] [Google Scholar]
- 25.Casali PG, Blay JY. Soft tissue sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2010; 21 Suppl 5:v198–v203. [DOI] [PubMed] [Google Scholar]
- 26.Hogendoorn PC, Athanasou N, Bielack S, et al. Bone sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2010; 21 Suppl 5:v204–v213. [DOI] [PubMed] [Google Scholar]
- 27.Andersen KF, Fuglo HM, Rasmussen SH, et al. Semi-quantitative calculations of primary tumor metabolic activity using F-18 FDG PET/CT as a predictor of survival in 92 patients with high-grade bone or soft tissue sarcoma. Medicine (Baltimore) 2015; 94:e1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guillou L, Coindre JM, Bonichon F, et al. Comparative study of the National Cancer Institute and French Federation of Cancer Centers Sarcoma Group grading systems in a population of 410 adult patients with soft tissue sarcoma. J Clin Oncol 1997; 15:350–362. [DOI] [PubMed] [Google Scholar]
- 29.Rubin BP, Antonescu CR, Gannon FH, et al. Protocol for the examination of specimens from patients with tumors of bone. Arch Pathol Lab Med 2010; 134:e1–e7. [DOI] [PubMed] [Google Scholar]
- 30.Berthelsen AK, Holm S, Loft A, et al. PET/CT with intravenous contrast can be used for PET attenuation correction in cancer patients. Eur J Nucl Med Mol Imaging 2005; 32:1167–1175. [DOI] [PubMed] [Google Scholar]
- 31.Wahl RL, Jacene H, Kasamon Y, et al. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med 2009; 50 Suppl 1:122S–150S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adams MC, Turkington TG, Wilson JM, et al. A systematic review of the factors affecting accuracy of SUV measurements. AJR Am J Roentgenol 2010; 195:310–320. [DOI] [PubMed] [Google Scholar]


