Abstract
As pelvic fractures in children and adolescents are very rare, the surgical management is not well delineated nor are the postoperative complications. The aim of this study using the prospective data from German Pelvic Trauma Registry study was to evaluate the various treatment approaches compared to adults and delineated the differences in postoperative complications after pelvic injuries.
Using the prospective pelvic trauma registry established by the German Society of Traumatology and the German Section of the Arbeitsgemeinschaft für Osteosynthesefragen (AO), International in 1991, patients with pelvic fractures over a 12-year time frame submitted by any 1 of the 23 member level I trauma centers were reviewed.
We identified a total of 13,525 patients including pelvic fractures in 13,317 adults and 208 children aged ≤14 years and compared these 2 groups. The 2 groups’ Injury Severitiy Score (ISS) did not differ statistically. Lethality in the pediatric group was 6.3%, not statistically different from the adults’ 4.6%. In all, 18.3% of the pediatric pelvic fractures were treated surgically as compared to 22.7% in the adult group. No child suffered any thrombosis/embolism, acute respiratory distress syndrome (ARDS), multiorgan failure (MOF), or neurologic deficit, nor was any septic MOF detected. The differences between adults and children were statistically significant in that the children suffered less frequently from thrombosis/embolism (P = 0.041) and ARDS and MOF (P = 0.006).
This prospective multicenter study addressing patients with pelvic fractures reveals that the risk for a thrombosis/embolism, ARDS, and MOF is significant lower in pediatric patients than in adults. No statistical differences could be found in the ratios of operative therapy of the pelvic fractures in children compared to adults.
INTRODUCTION
Trauma remains the leading cause of death in children.1 Injuries in the pelvic region in children and adolescents are rare: the incidence is between 2.4% and 7.5%.2–4 The main causes of injury are high-energy trauma2 associated with concomitant injuries to other regions (neurovascular and musculoskeletal structures, abdominal trauma, injuries to the central nerve system, etc.).5
A postmortem study of trauma patients showed a high rate of pelvic fracture-related deaths and a high incidence of pelvic fractures.6–8 An analysis from the American National Inpatient Pediatric Database revealed that children with pelvic injuries presented 5.2 concomitant injuries on average.9
A summary of the present literature shows that 83.3% of all pediatric pelvic injuries were due to high-energy trauma. The United States analysis also reveals that a pedestrian being struck by a car was the mechanism in 57.8%, a motor vehicle passenger was injured in 17.8%, a bicyclist in 4.9%, and a motorcyclist in 0.6%. A fall from a height was responsible for causing a pediatric pelvic fracture in 9.2%. Crush injuries (2.2%), injuries sustained during sport activities (2.1%), and farm accidents (0.5%) were uncommon.10 A key prognostic injury mechanism is the history of roll-over or crush (Injury Severitiy Score [ISS] up to 40 points, 86.6% associated injuries, 20% mortality rate >70% local complication rate).11
The ligaments of the children's pelvic are relatively stronger, and growth centers are present which together with the sacroiliac joints and pubic symphysis enable significant absorption capacity.10 Their pelvis is thus more elastic and more cartilaginous than that of adults.12 This elasticity results primarily in plastic deformation when the pelvic bone absorbs an impact13 which enables the pelvic anatomy's potential to be entirely restored, but not normally to the preinjury point. Due to this elasticity, the intrapelvic viscera are insufficiently protected, and intrapelvic organ injuries can occur in the absence of pelvic fractures or dislocations.14 Therefore, even simple or minimally displaced fractures are usually the result of a high-energy trauma, accompanied by the significant risk of additional intrapelvic and intraabdominal injuries.14 This leads to a relatively high incidence of isolated pubic rami fractures or iliac wing fractures.15–25
In contrast, complete disruption of the anterior and posterior pelvis or a complex pelvic injury can present a high risk factor for morbidity and mortality.26,27
Polytraumatized children should undergo computer tomography scans to rule out both pelvic fractures and associated nonmusculoskeletal injuries.28
The majority of pediatric pelvic fractures heal with no sequelae. Delayed union, pseudarthrosis, and persisting ligamentous instability are very rare.29 Complex pelvic traumas are associated in 31% of cases in conjunction with a higher rate of complications such as chronic back pain, persisting length discrepancy of the legs, difficulty urinating, and malfunction of the anal sphincter.27 Pelvic asymmetry can occur in children because of injury to the triradiate epiphysis; their mortality rate after pelvic fractures is around 5% (compared to 11%–18% in adults).2,3
The aim of this study based on a review of prospectively collected registry data was to evaluate the epidemiological data on children over a lengthy interval and to analyze how often and which emergency procedures were done to treat their pelvic fracture, as well as the postoperative complications these children suffered. Moreover, we were able to examine the clinical follow-up in a small subgroup of children to compare with a group of adults’ follow-up. Our a priori hypothesis was that there are relevant differences between the pelvic fractures in children compared to adults in terms of their epidemiological data, treatment methods, clinical outcomes, and types and rates of complications.
METHODS
This study is based on data from the prospective pelvic trauma registry introduced by the German Society of Traumatology and the German Section of Arbeitsgemeinschaft für Osteosynthesefragen/Association of the Study of Internal Fixation International in 1991.26,30–32 The registry provides data on all patients with pelvic fractures treated from January 1991 to December 1993, from January 1998 to December 2000, and from January 2004 to December 2012 at any 1 of the about 23 level I trauma centers contributing to the registry. In the years missing between the 3 time periods, the register was inactive and no data were collected. Moreover, the number of contributing hospitals has changed overtime. Data acquisition and analysis were done in accordance with ethical guidelines and approved by our institutional review board. The trial was registered at the German Clinical Trials Register (DRKS no. 00000488).
Data were collected and processed using a standardized data sheet. For this purpose, we engaged a secured internet interface hosted by a professional academic provider (www.memdoc.org, Institute for Evaluative Research in Medicine, Bern, Switzerland). Registration occurred as soon as possible after the patient's admission and was updated consistently during follow-up by a trauma surgeon or study nurse. All selected items were exported from the original datasets into a Microsoft Excel (Microsoft Corp, Redmond, WA) document for the purpose of evaluation and statistical analysis. These items included age, gender, ISS, Hannover Polytrauma Score, fracture type, need for emergency measures, mortality, cause of death, and need for operative stabilization. The majority of the participating institutions (listed under Acknowledgments) fulfilled the requirements of a level I trauma center according to the classification of the American College of Surgery33 and German Trauma Society.34
All fractures were classified in each case by experienced orthopedic/trauma surgeons. Classifications were based on plain radiographs and computer tomography scans routinely used. Moreover, doubtful cases were discussed in regular meetings conducted by the working group on a 4-time annual basis to minimize interobserver bias. Pelvic ring fractures were classified using Tile classification system adopted by the Orthopaedic Trauma Association.35 Stable pelvic ring fractures were classified as type A, fractures with only rotational instability as type B, and fractures with both rotational and translational instability as type C injuries. We defined type B and C injuries presenting major visceral, neurovascular, or soft-tissue injuries as complex pelvic injuries.36,37 We assessed patients on whether they had sustained isolated pelvic ring fractures or pelvic ring fractures with additional injuries to other body regions. We applied the ISS and Hannover Polytrauma Score to assess the severity of injuries.38,39
The complications evaluated were divided into postoperative complications such as thrombosis and embolism, acute respiratory distress syndrome (ARDS), multi-organ failure (MOF), neurologic deficit (occurring during clinical treatment and not associated with the initial trauma; the point of time, or if an injury was surgery-associated not specifiable by the available data), postoperative bleeding and hematoma, wound infections, and seroma. The diagnosis of each complication was confirmed by a representative from that specific discipline (neurology, anesthesiology, and vascular specialist).
Whenever we had access to patients’ follow-up data, we applied the evaluated EuroQoL-5D (EQ-5D) and Merle d’Aubigné and Postel score.
The EQ-5D score measures disease-nonspecific quality of life based on the EQ-5D index (ranges from −0.6 to 1, where 1 is the best imaginable health); it is designed primarily for self-completion by respondents and is ideal for use in postal surveys. It is cognitively simple, takes only a few minutes to complete, and instructions to respondents are included in the questionnaire.40
The EQ-5D is suitable and validated for the use of pediatrics.41 Even though 2010 the EQ-5D-Y (a child-friendly version of the EQ-5D) was introduced the authors preferred to have on consistent questionnaire.42 There are no specific questionnaires for specific pelvic fractures in children, so the authors believe that this questionnaire was the best suitable for the investigation and was suitable and validated. Moreover, the clinical problems after pelvic fractures are very similar to patients suffering acetabular fractures.
The Merle d’Aubigné and Postel score is considered easy to understand and simple to administer and measures hip function via a score (ranges between 0 and 18, where 0 is the worst and 18 the best function).43
Our data were analyzed using WinStat 2009 (Bad Krozingen, Germany) for Microsoft Excel (Microsoft Corp, Redmond, WA) and statistical test as the Chi-square test and Mid-P-exact tests were used when appropriate. The alpha was set to 0.05 throughout the study.
RESULTS
We identified a total of 13,525 patients including pelvic fractures in 13,317 adults and 208 children aged ≤14 years and compared these 2 groups. The time periods and numbers of adults versus children identified were: years 1991 to 1993 (n = 1722/57), years 1998 to 2000 (n = 2569/47), and years 2004 to 2012 (n = 9234/104).
Mean age in the pediatric group was 9.3 years (±4.2) with a mean ISS of 16.7 (±15) points. Mean age in the adult group was 53.5 years (±23.5) with a mean ISS of 15 (±15) points (ISS: P > 0.05). The adults’ mean age rose overtime (mean age: 48, 53 and 59 years) (P < 0.001), whereas we observed no statistical difference in the children's mean age overtime (P > 0.05) (Fig. 1).
FIGURE 1.
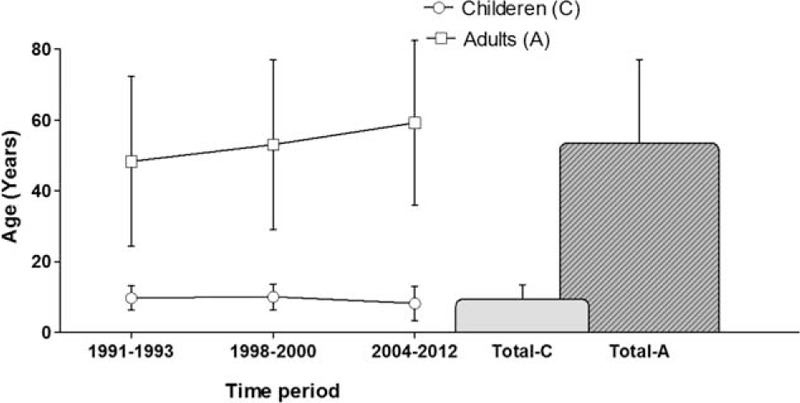
Development of mean age of the pediatric and adult groups since 1991. Mean age in the pediatric group was 9.3 years (±4.2) with a mean Injury Severitiy Score (ISS) of 16.7 (±15) points. Mean age in the adult group was 53.5 years (±23.5) with a mean ISS of 15 (±15) points (ISS: P > 0.05). The adults’ mean age rose over time (mean age: 48, 53, and 59 years) (P < 0.001), whereas we observed no statistical difference in the children's mean age overtime (P > 0.05).
We conducted a further analysis of the gender ratio of these patients and observed a continuous trend in the adult group, namely a significantly decreasing gender ratio with a nearly equal ratio of 1.03 in the latest investigation period (P < 0.001). However, in the pediatric group, many more boys suffered pelvic fractures – we noted a ratio of 1.48 from 2004 to 2012 with an overall rate of 58% boys and 42% girls; there was no statistical difference in the gender ratio in the pediatric group's 3 time periods (P > 0.05) (Fig. 2).
FIGURE 2.
Development of the gender ratio of children and adults. We conducted a further analysis of the gender ratio of these patients, which revealed a continuous trend in the group of adults, namely a significantly decreasing gender ratio with a nearly equal ratio of 1.03 in the latest investigation period (P < 0.001). However, in the pediatric group, many more boys suffered pelvic fractures, at a ratio of 1.48 from 2004 to 2012 with an overall rate of 58% boys and 42% girls; there was no statistical difference in the gender ratio in the pediatric group's 3 time periods (P > 0.05).
Table 1 summarizes the fracture classification in both groups, classified in Tile A, B, and C fractures,35 isolated acetabulum fractures (Iso Ac.), combined fractures of the acetabulum with an additional Tile A or B fracture type (Ac + Tile A/B), and complex fractures of the pelvis. Complex fractures were defined as pelvic fractures with additional injury to pelvic organs, vessels, and open fractures. The distribution of complex fractures among the children and adults was statistically not significantly different (P > 0.05). However, the distribution according to the Tile classification did differ significantly because of the much higher rate of acetabular fractures among the adults (P < 0.001) (Table 1).
TABLE 1.
Summarizes the Fracture Classification in Both Groups, Classified in Tile A, B, and C fractures,35 Isolated Acetabulum Fractures (Iso Ac.), Combined Fractures of the Acetabulum With an Additional Tile A or B Fracture Type (Ac + Tile A/B) and Complex Fractures of the Pelvis

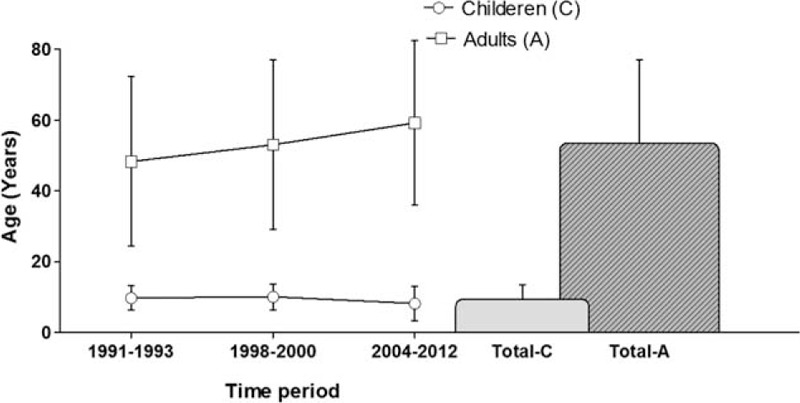
Figure 3 illustrates the ratios of operative therapy of the pelvic fractures. A total of 18.3% of the pediatric pelvic fractures were treated operatively, while 22.7% of the adults’ fractures were treated surgically. The other patients were treated conservatively; we detected no statistical difference between the adults and children in this regard (P > 0.05). What is remarkable is that in the initial time period (1/1991–12/1993), very few children underwent surgery compared to the adults. However, the rate of operative therapy from the 2nd and 3rd time period (1/1998–12/2000 and 1/2004–12/2012) is similar in both groups (Fig. 3).
FIGURE 3.
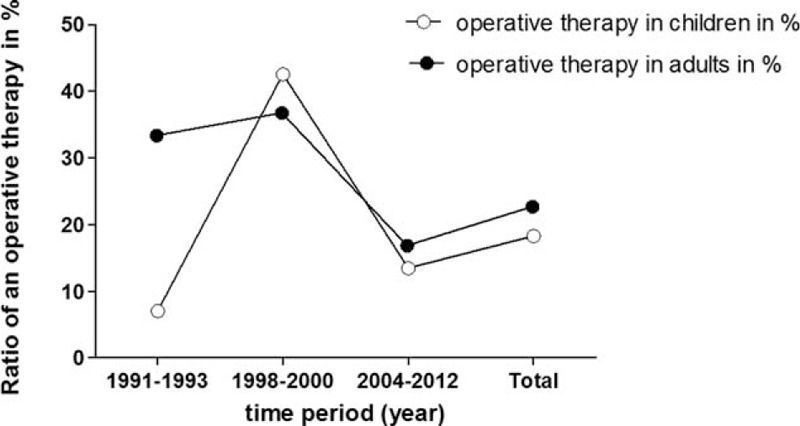
The ratio of an operative therapy of children and adults. In Figure 3 illustrates the ratios of operative therapy of the pelvic fractures. A total of 18.3% of the pediatric pelvic fractures were treated operatively, while 22.7% of the adults’ fractures were treated surgically. The other patients were treated conservatively; we detected no statistical difference between the adults and children in therapy terms (P > 0.05). What is remarkable is that in the very 1st time period, very few children underwent surgery compared to the adults. However, from the second time period, the rate of operative therapy is similar in both groups.
Almost all the children who had undergone emergency surgery (15.4%) required subsequent therapy; the emergency interventions performed (in order of frequency) were:
Surgical emergency procedures with 8.7% external fixator (as “effective treatment” in 7.7%), 6.7% laparotomy, 1.4% emergency operation, and 0.5% pelvic C-clamp.
Not surgical procedures with 1% pelvic compression with a cloth, 1% pelvic binder.
A total of 18.8% of the adults in our survey had to undergo emergency surgery - their procedures were:
Surgical emergency procedures with 3% laparotomy, 1.9% emergency operation, 1.5% pelvic C-clamp, and 0.4% angioembolization.
We observed no statistical group difference in terms of emergency procedures (P < 0.05).
Table 2 summarizes the postoperative complications. No child suffered a thrombosis/embolism, ARDS, or a neurologic deficit. Two children suffered from “multi-organ failure” (MOF): one died after a severe craniocerebral injury and the other, after severe blood loss in the thorax and abdomen. These MOFs were thus not “septic” in nature. The differences between adults and children were statistically significant in terms of thrombosis/embolism (P = 0.041) and ARDS and MOF (P = 0.006). No children suffered a neurologic deficit, whereas 2% of the adults did (P = 0.015). No group differences were detected in terms of bleeding/hematoma or infect/seroma (P > 0.05) (Table 2).
TABLE 2.
Summarizes Postoperative Complications

Lethality after suffering a pelvic fracture was not statistically significant, namely 13 children (6.3%) and 619 patients among the adults (4.6%) (P > 0.05).
Clinical follow-up is shown in Figure 4 and is based on data from just 10 children (most from examinations in our clinic) 3.3 (±0.9) years after trauma and from data available from the registry of 631 adults who had undergone follow-up 2.5 (±1.7) years after trauma. The EQ5D score represents quality of life and the Merle d’Aubigne Score patient functionality. The 10 children we analyzed had significantly better results in the follow-up investigations according to both scores (P < 0.05) (Fig. 4).
FIGURE 4.
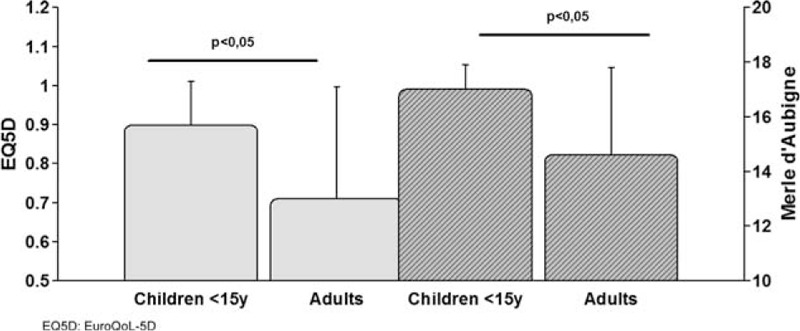
Clinical follow-up after pelvic fracture. Clinical follow-up is shown in Figure 4 and is based on data from 10 children (most from examinations in our clinic) 3.3 (±0.9) years after trauma and from available data in the registry of 631 adults who had undergone follow-up 2.5 (±1.7) years after trauma. The EQ5D score represents quality of life and the Merle d’Aubigne Score represents patient functionality. The 10 analyzed children had significantly better results in the follow-up investigations according to both scores (P < 0.05).
DISCUSSION
In investigating the prospective pelvic trauma registry introduced by the German Society of Traumatology and the German Section of Arbeitsgemeinschaft für Osteosynthesefragen/Association of the Study of Internal Fixation International, it was the aim of this study to analyze epidemiological results and differences between adults and children suffering a pelvic trauma in terms of emergency operative procedures, postoperative complications, and clinical follow-up examinations. According to a recently published review, only 1 publication44 has so far reported on more pediatric patients under investigation in a study.45 Gänsslen analyzed an overall mean age of 9 years in 10 analyzed studies and found a mean ISS of 15.7 points in 5 studies, and male predominance at a male/female ratio of approximately 1.4:1, all factors that resemble our investigation's findings.10 In analyzing the fracture types in different studies, Gänsslen cites a 60% to 80% rate of type A fractures, 10% to 35% type B injuries, and 10% to 16% type C injuries. Our results confirm his forecast for the German population in the last 2 decades. Type A are stable, type B are partially unstable injuries with partial posterior, rotational instability after antero-posterior or lateral compression, and type C are unstable injuries with combined anterior and posterior, vertical instability. Another commonly accepted classification of children's pelvic fracture is the Torode classification.25
For the children's analysis, we opted for the classic age cut-off at 14 years, as the epiphyseal plate in the acetabulum closes between 14 and 16 years.46 Mean age in the pediatric group we analyzed was 9.3 years (±4.2). Another review summarized 10 studies on pediatric pelvic fractures and identified a mean age of 9 years, similar to our data.10
Several alternatives and approaches for the operative treatment of pelvic fractures in children have been published, describing a wide (0.6%–30%) range of surgical interventions and reporting comparable rates of external and internal fixation.10 With the knowledge that conservatively treated displaced pelvic fractures in children can lead to pelvic asymmetry and poor clinical outcomes, more authors have focused on operative stabilization of the pelvic ring.22,25,47–49 The standard indications for the operative fixation of pelvic fractures are:
Concomitant therapy when open-wound treatment is necessary.
Additional hemorrhage control during resuscitation.15
Prevention of deformity in severely displaced fractures.6,50–52
The optimization and enhancement of patient mobility in particular situations (eg, polytrauma).
Therefore, only displaced fractures require surgical reduction and stabilization15,25,43,52,53 and only case descriptions are reported in the literature.13
Several emergency devices are currently available to stabilize an instable pelvis. Antishock trousers are no longer recommended in adults because of the high rate of complications.54 The application of pelvic slings, pelvic bed sheets, or a pelvic binder at the scene or in the emergency ward may be useful tools and treatment options for pediatric patients with an instable pelvic fracture.55 As our registry findings also reveal, stabilization with external fixation is the most common stabilization technique for pediatric pelvic fractures.17,38,47,49,51,54,56,57 After external fixation was applied, McIntyre et al58 detected a 60% rate of controlled bleeding in his cohort. The pelvic C-clamp is an adequate tool and can be used to stabilize the posterior pelvic ring, as another author mentions.59 Definitive reduction and internal fixation in acute management is only recommended when the patients are in stable condition. Feasible approaches for fixation are symphyseal plating, anterior plating of the SI-joint, and application of transiliosacral screws.60
Accepted methods to control pelvic hemorrhage are angiography or embolization and pelvic packing. Angiography and embolization to stabilize hemodynamics in pediatric patients with pelvis fractures can succeed, but reported time intervals between admission and the start of embolization range from 12 to 15 hours in an international study, and only 62 minutes in a German study.61,62 Another trauma-registry study reports the incidence of angiographic interventions as approximately 5% – a potential treatment strategy to stabilize hemodynamics.4 External fixation was the most often applied method in children and adults; however, the advantage at a younger age is that it is more frequently administered as definitive care.
Taking this study's data and the literature into account, external fixation seems to be an appropriate and minimally invasive treatment for most unstable pelvic fractures in children. Nevertheless, binding an unstable pelvic fracture (ie, in a preclinical or emergency room context) and angioembolization in the first hours of clinical stabilization are also treatment options for children.
We observed a significantly lower incidence of thrombosis, ARDS, and MOF in the pediatric group compared to adults. The “typical” complications in adults were almost nonexistent among the children.
The incidence of ARDS in the overall pediatric population is relatively low, with estimates ranging between 2.963 and 1264–66 cases/100,000 children per year. The mortality rate in recently published studies from the USA and China are between 18% and 43% depending on the population and disease.64,67 Data from North America show mortality gradually dropping from 35% in the years 1996–1997 to 26% between 2004 and 2005.67 Even in very large studies, the main risk factors to develop an ARDS are pneumonia, aspiration, sepsis, near drowning, concomitant cardiac disease, and “others”; however, suffering a trauma or even polytrauma goes unmentioned.68
Venous thromboembolism (VTE) is an often-reported and major source of morbidity in critically ill trauma adult patients. In a pediatric population, Vavilala et al69 found that older children with high Injury Severity Scores, major vascular injury, craniotomy, or venous catheters are at risk for VTE.
Although trauma is noted as a risk factor in almost every reported series of pediatric patients with VTE, the rate of VTE specific to the pediatric trauma population is not well established. The reported incidence of VTE in the overall pediatric trauma population ranges from 0.02% to 0.33%69–76 and appears stable overtime.71
Evidence-based guidelines provide clear recommendations for VTE prophylaxis in adults who suffer major trauma.77–79 The initiation of low-dose unfractionated heparin or LMWH with intermittent pneumatic compression is recommended to begin within 24 to 48 hours of injury, unless contraindicated. In the presence of contraindications such as uncontrolled bleeding, presence of an epidural catheter, or severe coagulopathy, mechanical prophylaxis is suggested, and pharmacologic anticoagulation should begin once the bleeding risk has subsided. The recommended duration of VTE prophylaxis for patients with spinal cord injury is 3 months. Duration of prophylaxis is not clearly stated for other types of trauma; however, patients requiring major orthopedic surgery are recommended to receive prophylaxis for up to 35 days from the date of surgery, as opposed to only 10 to 14 days. For patients with isolated lower-leg injuries requiring leg immobilization, VTE prophylaxis is not recommended. Nor are screening ultrasounds recommended. The aforementioned guidelines make no recommendations for treating pediatric trauma patients.18,77,79
The data on medical or physical VTE prophylaxis in children and the newborn are insufficient.80 In adolescents in early puberty (≥Stadium Tanner II), the expositional and dispositional risk factors should be evaluated as they are in adults.80–82
Pelvic fractures in children are extremely rare, and they appear to becoming even less frequent over the most recent decades.
The fact that our study employs a prospective multicentre registry is both strength and weakness. On the one hand, including patients from several institutions best reflects a country's therapeutic reality. On the other hand, we relied on 21 to 27 active level I trauma centers contributing to the registry, and it goes without saying that treatment protocols depend on each institution's environment.
CONCLUSION
The severity of injury seems to be similar in adults and children who suffer a pelvic fracture. In our registry patients, emergency procedures were performed in 15.4% of the children, and their risk for thrombosis/embolism, ARDS, and MOF was significant lower. Children seem to enjoy a better clinical outcome than adults according to the long time follow-up investigations we had access to. The reason for this probably has to do with poorly understood differences in the child's immune system.
Acknowledgments
Over the past 20 years, the members of the Pelvic Trauma Working Group of the German Trauma Association have invested much time and effort in scientific projects, as well as in teaching and improving the standards of care for patients with pelvic and acetabular fractures in Germany. This study and all other achievements would not have been possible without their commitment during the different study periods. Hospitals contributing to the German Pelvic Trauma Registry Initiative are: AZ Groeninge (Belgien); BG Kliniken Bergmannstrost, Halle; BG Unfall Klinik – Tuebingen; BG Unfallklinik, Ludwigshafen; BG Unfallklinik, Murnau; BWK Ulm; Charité – Campus Virchow Klinikum; Diakonissenkrankenhaus, Flensburg; Friederikenstift, Hannover; Klinikum Ludwigsburg; Klinikum der Universität Regensburg, Regensburg; Klinikum rechts der Isar, München; Klinikum, Augsburg; Klinikum, Dortmund; Klinikum, Nürnberg; Klinikum, Schwerin; Kreisklinik, Biberach; Medizinische Hochschule, Hannover; RWTH University Hospital; SKM, Koblenz; STER ANTWERP (Belgien); Städt. Klinikum, Braunschweig; Städtisches Klinikum, Karlsruhe; Univerisitätsklinik, Magdeburg; Universität, Kiel; Universitätklinik, Mainz; Universitätsklinik Halle; Universitätsklinik, Freiburg; Universitätsklinik, Jena; Universitätsklinik, Münster; Universitätskliniken Saarland; Universitätsklinikum AöR, Leipzig; Universitätsklinikum Hamburg-Eppendorf, Hamburg; Universitätsklinikum, Ulm; and Westpfalz-Klinikum, Kaiserslautern. “The article processing charge was funded by the German Research Foundation (DFG) and the Albert Ludwigs University Freiburg in the funding programme Open Access Publishing.”
Footnotes
Abbreviations: AO = Arbeitsgemeinschaft für Osteosynthesefragen, ARDS = acute respiratory distress syndrome, EQ-5D = EuroQoL-5D, ISS = Injury Severitiy Score, MOF = multiorgan failure, PTS = Hannover Polytrauma Score, VTE = venous thromboembolism.
The article processing charge was funded by the German Research Foundation (DFG) and the Albert Ludwigs University Freiburg in the funding programme Open Access Publishing.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Snyder CL, Jain VN, Saltzman DA, et al. Blunt trauma in adults and children: a comparative analysis. J Trauma 1990; 30:1239–1245. [DOI] [PubMed] [Google Scholar]
- 2.Schlickewei W, Keck T. Pelvic and acetabular fractures in childhood. Injury 2005; 36 Suppl 1:A57–63. [DOI] [PubMed] [Google Scholar]
- 3.Ismail N, Bellemare JF, Mollitt DL, et al. Death from pelvic fracture: children are different. J Pediatr Surg 1996; 31:82–85. [DOI] [PubMed] [Google Scholar]
- 4.Demetriades D, Karaiskakis M, Velmahos GC, et al. Pelvic fractures in pediatric and adult trauma patients: are they different injuries? J Trauma 2003; 54:1146–1151.discussion 51. [DOI] [PubMed] [Google Scholar]
- 5.Widmann R. Fractures of the Pelvis Rockwood CA WK. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 6.Keshishyan RA, Rozinov VM, Malakhov OA, et al. Pelvic polyfractures in children. Radiographic diagnosis and treatment. Clin Orthop Relat Res 1995; 320:28–33. [PubMed] [Google Scholar]
- 7.Schmal H, Klemt C, Haag C, et al. [Complex pelvic injury in childhood]. Unfallchirurg 2002; 105:748–754. [DOI] [PubMed] [Google Scholar]
- 8.Nabaweesi R, Arnold MA, Chang DC, et al. Prehospital predictors of risk for pelvic fractures in pediatric trauma patients. Pediatr Surg Int 2008; 24:1053–1056. [DOI] [PubMed] [Google Scholar]
- 9.Galano GJ, Vitale MA, Kessler MW, et al. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J Pediatr Orthop 2005; 25:39–44. [DOI] [PubMed] [Google Scholar]
- 10.Gansslen A, Hildebrand F, Heidari N, et al. Pelvic ring injuries in children. Part I: epidemiology and primary evaluation. A review of the literature. Acta Chir Orthop Traumatol Cech 2012; 79:493–498. [PubMed] [Google Scholar]
- 11.Mosheiff R, Suchar A, Porat S, et al. The “crushed open pelvis” in children. Injury 1999; 30 Suppl 2:B14–B18. [PubMed] [Google Scholar]
- 12.Currey JD, Butler G. The mechanical properties of bone tissue in children. J Bone Joint Surg Am 1975; 57:810–814. [PubMed] [Google Scholar]
- 13.Stuhler T, Stankovic P, Krause P, et al. [Pelvic fractures in children: clinic, late results, biomechanic (author's transl)]. Arch Orthop Unfallchir 1977; 90:187–198. [DOI] [PubMed] [Google Scholar]
- 14.Offiah A, van Rijn RR, Perez-Rossello JM, et al. Skeletal imaging of child abuse (non-accidental injury). Pediatr Radiol 2009; 39:461–470. [DOI] [PubMed] [Google Scholar]
- 15.Blasier RD, McAtee J, White R, et al. Disruption of the pelvic ring in pediatric patients. Clin Orthop Relat Res 2000; 376:87–95. [DOI] [PubMed] [Google Scholar]
- 16.Chia JP, Holland AJ, Little D, et al. Pelvic fractures and associated injuries in children. J Trauma 2004; 56:83–88. [DOI] [PubMed] [Google Scholar]
- 17.Grisoni N, Connor S, Marsh E, et al. Pelvic fractures in a pediatric level I trauma center. J Orthop Trauma 2002; 16:458–463. [DOI] [PubMed] [Google Scholar]
- 18.Junkins EP, Furnival RA, Bolte RG. The clinical presentation of pediatric pelvic fractures. Pediatr Emerg Care 2001; 17:15–18. [DOI] [PubMed] [Google Scholar]
- 19.Junkins EP, Jr, Nelson DS, Carroll KL, et al. A prospective evaluation of the clinical presentation of pediatric pelvic fractures. J Trauma 2001; 51:64–68. [DOI] [PubMed] [Google Scholar]
- 20.Lane-O’Kelly A, Fogarty E, Dowling F. The pelvic fracture in childhood: a report supporting nonoperative management. Injury 1995; 26:327–329. [DOI] [PubMed] [Google Scholar]
- 21.Musemeche CA, Fischer RP, Cotler HB, et al. Selective management of pediatric pelvic fractures: a conservative approach. J Pediatr Surg 1987; 22:538–540. [DOI] [PubMed] [Google Scholar]
- 22.Rieger H, Brug E. Fractures of the pelvis in children. Clin Orthop Relat Res 1997; 336:226–239. [DOI] [PubMed] [Google Scholar]
- 23.Silber JS, Flynn JM, Koffler KM, et al. Analysis of the cause, classification, and associated injuries of 166 consecutive pediatric pelvic fractures. J Pediatr Orthop 2001; 21:446–450. [PubMed] [Google Scholar]
- 24.Spiguel L, Glynn L, Liu D, et al. Pediatric pelvic fractures: a marker for injury severity. Am Surg 2006; 72:481–484. [PubMed] [Google Scholar]
- 25.Torode I, Zieg D. Pelvic fractures in children. J Pediatr Orthop 1985; 5:76–84. [DOI] [PubMed] [Google Scholar]
- 26.Hauschild O, Strohm PC, Culemann U, et al. Mortality in patients with pelvic fractures: results from the German pelvic injury register. J Trauma 2008; 64:449–455. [DOI] [PubMed] [Google Scholar]
- 27.Meyer-Junghanel L, Gansslen A, Pohlemann T, et al. [Treatment outcome after complex pelvic trauma in children]. Unfallchirurg 1997; 100:225–233. [DOI] [PubMed] [Google Scholar]
- 28.Zwingmann J, Schmal H, Sudkamp NP, et al. [Injury severity and localisations seen in polytraumatised children compared to adults and the relevance for emergency room management]. Zentralbl Chir 2008; 133:68–75. [DOI] [PubMed] [Google Scholar]
- 29.Holden CP, Holman J, Herman MJ. Pediatric pelvic fractures. J Am Acad Orthop Surg 2007; 15:172–177. [DOI] [PubMed] [Google Scholar]
- 30.Zwingmann J, Sudkamp NP, Benjamin K, et al. Intra- and postoperative complications of navigated and conventional techniques in percutaneous iliosacral screw fixation after pelvic fractures: results from the German Pelvic Trauma Registry. Injury 2013; 44:1765–1772. [DOI] [PubMed] [Google Scholar]
- 31.Pohlemann T, Tosounidis G, Bircher M, et al. The German Multicentre Pelvis Registry: a template for an European Expert Network? Injury 2007; 38:416–423. [DOI] [PubMed] [Google Scholar]
- 32.Lehmann W, Hoffmann M, Fensky F, et al. What is the frequency of nerve injuries associated with acetabular fractures? Clin Orthop Relat Res 2014; 472:3395–3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aprahamian C, Wolferth CC, Jr, Darin JC, et al. Status of trauma center designation. J Trauma 1989; 29:566–570. [DOI] [PubMed] [Google Scholar]
- 34.Siebert H. [White book of severely injured – care of the DGU. Recommendations on structure, organization and provision of hospital equipment for care of severely injured in the Federal Republic of Germany]. Unfallchirurg 2006; 109:815–820. [DOI] [PubMed] [Google Scholar]
- 35.Tile M. Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg 1996; 4:143–151. [DOI] [PubMed] [Google Scholar]
- 36.Bosch U, Pohlemann T, Haas N, et al. [Classification and management of complex pelvic trauma]. Unfallchirurg 1992; 95:189–196. [PubMed] [Google Scholar]
- 37.Culemann U, Tosounidis G, Reilmann H, et al. [Injury to the pelvic ring. Diagnosis and current possibilities for treatment]. Unfallchirurg 2004; 107:81–1169.quiz 82–3. [DOI] [PubMed] [Google Scholar]
- 38.Baker SP, O’Neill B, Haddon W, Jr, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974; 14:187–196. [PubMed] [Google Scholar]
- 39.Sudkamp N, Haas N, Flory PJ, et al. [Criteria for amputation, reconstruction and replantation of extremities in multiple trauma patients]. Chirurg 1989; 60:774–781. [PubMed] [Google Scholar]
- 40.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001; 33:337–343. [DOI] [PubMed] [Google Scholar]
- 41.Ravens-Sieberer U, Wille N, Badia X, et al. Feasibility, reliability, and validity of the EQ-5D-Y: results from a multinational study. Qual Life Res 2010; 19:887–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wille N, Badia X, Bonsel G, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010; 19:875–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.D’Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am 1954; 36-A:451–475. [PubMed] [Google Scholar]
- 44.Vitale MG, Kessler MW, Choe JC, et al. Pelvic fractures in children: an exploration of practice patterns and patient outcomes. J Pediatr Orthop 2005; 25:581–587. [DOI] [PubMed] [Google Scholar]
- 45.Gansslen A, Hildebrand F, Heidari N, et al. Pelvic ring injuries in children. Part II: treatment and results. A review of the literature. Acta Chir Orthop Traumatol Cech 2013; 80:241–249. [PubMed] [Google Scholar]
- 46.Weinberg AM, Tscherne H. Unfallchirurgie im Kindesalter. Pohlemann T, Gänsslen A, Partenheimer A. eds. Berlin Heidelberg New York: Springer; 2006. [Google Scholar]
- 47.Baskin KM, Cahill AM, Kaye RD, et al. Closed reduction with CT-guided screw fixation for unstable sacroiliac joint fracture-dislocation. Pediatr Radiol 2004; 34:963–969. [DOI] [PubMed] [Google Scholar]
- 48.Karunakar MA, Goulet JA, Mueller KL, et al. Operative treatment of unstable pediatric pelvis and acetabular fractures. J Pediatr Orthop 2005; 25:34–38. [DOI] [PubMed] [Google Scholar]
- 49.Stiletto RJ, Baacke M, Gotzen L. Comminuted pelvic ring disruption in toddlers: management of a rare injury. J Trauma 2000; 48:161–164. [DOI] [PubMed] [Google Scholar]
- 50.Bryan WJ, Tullos HS. Pediatric pelvic fractures: review of 52 patients. J Trauma 1979; 19:799–805. [DOI] [PubMed] [Google Scholar]
- 51.Reef R. The use of external fixation devices in the management of severe lower-extremity trauma and pelvic injuries in children. Clin Orthop 1984; 188:21–33. [PubMed] [Google Scholar]
- 52.Schwarz N, Posch E, Mayr J, et al. Long-term results of unstable pelvic ring fractures in children. Injury 1998; 29:431–433. [DOI] [PubMed] [Google Scholar]
- 53.Heeg M, Klasen HJ. Long-term outcome of sacroiliac disruptions in children. J Pediatr Orthop 1997; 17:337–341. [PubMed] [Google Scholar]
- 54.Gansslen A, Giannoudis P, Pape HC. Hemorrhage in pelvic fracture: who needs angiography? Curr Opin Crit Care 2003; 9:515–523. [DOI] [PubMed] [Google Scholar]
- 55.Simpson T, Krieg JC, Heuer F, et al. Stabilization of pelvic ring disruptions with a circumferential sheet. J Trauma 2002; 52:158–161. [DOI] [PubMed] [Google Scholar]
- 56.Engelhardt P. [Malgaigne pelvic ring injury in childhood]. Orthopäde 1992; 21:422–426. [PubMed] [Google Scholar]
- 57.Rangger C, Gabl M, Dolati B, et al. [Pediatric pelvic fractures]. Unfallchirurg 1994; 97:649–651. [PubMed] [Google Scholar]
- 58.McIntyre RC, Jr, Bensard DD, Moore EE, et al. Pelvic fracture geometry predicts risk of life-threatening hemorrhage in children. J Trauma 1993; 35:423–429. [DOI] [PubMed] [Google Scholar]
- 59.Holt GE, Mencio GA. Pelvic C-clamp in a pediatric patient. J Orthop Trauma 2003; 17:525–527. [DOI] [PubMed] [Google Scholar]
- 60.Routt ML, Jr, Nork SE, Mills WJ. High-energy pelvic ring disruptions. Orthop Clin North Am 2002; 33:59–72.viii. [DOI] [PubMed] [Google Scholar]
- 61.Qasim ZA, Masood R, Mateen MA. Successful use of angiographic embolization to control hemorrhage from blunt pelvic trauma in a pediatric patient. JPMA J Pak Med Assoc 2004; 54:32–33. [PubMed] [Google Scholar]
- 62.Westhoff J, Laurer H, Wutzler S, et al. [Interventional emergency embolization for severe pelvic ring fractures with arterial bleeding. Integration into the early clinical treatment algorithm]. Unfallchirurg 2008; 111:821–828. [DOI] [PubMed] [Google Scholar]
- 63.Erickson S, Schibler A, Numa A, et al. Acute lung injury in pediatric intensive care in Australia and New Zealand: a prospective, multicenter, observational study. Pediatr Crit Care Med 2007; 8:317–323. [DOI] [PubMed] [Google Scholar]
- 64.Zimmerman JJ, Akhtar SR, Caldwell E, et al. Incidence and outcomes of pediatric acute lung injury. Pediatrics 2009; 124:87–95. [DOI] [PubMed] [Google Scholar]
- 65.Dahlem P, van Aalderen WM, Hamaker ME, et al. Incidence and short-term outcome of acute lung injury in mechanically ventilated children. Eur Resp J 2003; 22:980–985. [DOI] [PubMed] [Google Scholar]
- 66.Kneyber MC, Brouwers AG, Caris JA, et al. Acute respiratory distress syndrome: is it underrecognized in the pediatric intensive care unit? Intens Care Med 2008; 34:751–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hu X, Qian S, Xu F, et al. Incidence, management and mortality of acute hypoxemic respiratory failure and acute respiratory distress syndrome from a prospective study of Chinese paediatric intensive care network. Acta Paediatr 2010; 99:715–721. [DOI] [PubMed] [Google Scholar]
- 68.Flori HR, Glidden DV, Rutherford GW, et al. Pediatric acute lung injury: prospective evaluation of risk factors associated with mortality. Am J Resp Crit Care Med 2005; 171:995–1001. [DOI] [PubMed] [Google Scholar]
- 69.Vavilala MS, Nathens AB, Jurkovich GJ, et al. Risk factors for venous thromboembolism in pediatric trauma. J Trauma 2002; 52:922–927. [DOI] [PubMed] [Google Scholar]
- 70.Candrilli SD, Balkrishnan R, O’Brien SH. Effect of injury severity on the incidence and utilization-related outcomes of venous thromboembolism in pediatric trauma inpatients. Pediatr Crit Care Med 2009; 10:554–557. [DOI] [PubMed] [Google Scholar]
- 71.Askegard-Giesmann JR, O’Brien SH, Wang W, et al. Increased use of enoxaparin in pediatric trauma patients. J Pediatr Surg 2012; 47:980–983. [DOI] [PubMed] [Google Scholar]
- 72.McBride WJ, Gadowski GR, Keller MS, et al. Pulmonary embolism in pediatric trauma patients. J Trauma 1994; 37:913–915. [DOI] [PubMed] [Google Scholar]
- 73.Cook A, Shackford S, Osler T, et al. Use of vena cava filters in pediatric trauma patients: data from the National Trauma Data Bank. J Trauma 2005; 59:1114–1120. [DOI] [PubMed] [Google Scholar]
- 74.Cyr C, Michon B, Pettersen G, et al. Venous thromboembolism after severe injury in children. Acta Haematol 2006; 115:198–200. [DOI] [PubMed] [Google Scholar]
- 75.O’Brien SH, Candrilli SD. In the absence of a central venous catheter, risk of venous thromboembolism is low in critically injured children, adolescents, and young adults: evidence from the National Trauma Data Bank. Pediatr Crit Care Med 2011; 12:251–256. [DOI] [PubMed] [Google Scholar]
- 76.Truitt AK, Sorrells DL, Halvorson E, et al. Pulmonary embolism: which pediatric trauma patients are at risk? J Pediatr Surg 2005; 40:124–127. [DOI] [PubMed] [Google Scholar]
- 77.Gould MK, Garcia DA, Wren SM, et al. Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141 (2 Suppl):e77S–e227S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141 (2 Suppl):e278S–e325S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rogers FB, Cipolle MD, Velmahos G, et al. Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma 2002; 53:142–164. [DOI] [PubMed] [Google Scholar]
- 80.AWMF. S3-Leitlinie Polytrauma/Schwerverletzten-Behandlung 2011. [Google Scholar]
- 81.Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Childhood 1970; 45:13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Childhood 1969; 44:291–303. [DOI] [PMC free article] [PubMed] [Google Scholar]


