Abstract
Study Objective
We sought to (1) define the high-risk elderly trauma patient based on prognostic differences associated with different injury patterns and (2) derive alternative field trauma triage guidelines that mesh with national field triage guidelines to improve identification of high-risk elderly patients.
Methods
This was a retrospective cohort study of injured adults ≥ 65 years transported by 94 EMS agencies to 122 hospitals in 7 regions from 1/1/2006 through 12/31/2008. We tracked current field triage practices by EMS, patient demographics, out-of-hospital physiology, procedures and mechanism of injury. Outcomes included Injury Severity Score ≥ 16 and specific anatomic patterns of serious injury using Abbreviated Injury Scale score ≥ 3 and surgical interventions. In-hospital mortality was used as a measure of prognosis for different injury patterns.
Results
33,298 injured elderly patients were transported by EMS, including 4.5% with ISS ≥ 16, 4.8% with serious brain injury, 3.4% with serious chest injury, 1.6% with serious abdominal-pelvic injury and 29.2% with serious extremity injury. In-hospital mortality ranged from 18.7% (95% CI 16.7–20.7) for ISS ≥ 16 to 2.9% (95% CI 2.6–3.3) for serious extremity injury. The alternative triage guidelines (any positive criterion from the current guidelines, GCS ≤ 14 or abnormal vital signs) outperformed current field triage practices for identifying patients with ISS ≥ 16: sensitivity (92.1% [95% CI 89.6–94.1%] vs. 75.9% [95% CI 72.3–79.2%]), specificity (41.5% [95% CI 40.6–42.4%] vs. 77.8% [95% CI 77.1–78.5%]). Sensitivity decreased for individual injury patterns, but was higher than current triage practices.
Conclusions
High-risk elderly trauma patients can be defined by ISS ≥ 16 or specific non-extremity injury patterns. The field triage guidelines could be improved to better identify high-risk elderly trauma patients by EMS, with a reduction in triage specificity.
INTRODUCTION
Injuries in older adults are common and often involve use of emergency medical services (EMS).1,2 Current field trauma triage processes fail to identify a large proportion of seriously injured older patients, many of whom are transported to non-trauma hospitals (termed “under-triage”). 3–8 This mismatch between patient need and hospital capability is a disparity in care that can result in worse clinical outcomes.9,10 As the population of older adults in the U.S. continues to increase, under-triage and resulting disparities in trauma care are likely to become further exaggerated unless system-level changes are implemented. While the national field triage guidelines have been modified in an effort to close this gap,11 little evidence exists that these changes have been successful and out-of-hospital research on injured older adults remains sparse.
Elderly trauma patients are unique compared to younger patients. They can incur life-threatening injuries from low velocity mechanisms (e.g., ground-level fall12,13) and have a much higher prevalence of comorbid conditions and frailty compared to younger patients. Older adults take more medications (including medications potentially worsening injury14,15) and have different physiologic responses to injury.16,17 They often have more complex medical and surgical decision-making than younger patients,18 including end-of-life considerations. Thus, the one-size-fits-all approach to field triage guidelines may be inadequate for injured elderly patients. Previous studies have explored elderly-specific triage criteria,19–21 although there is a need to pull these modifications together in a manner that allows integration with the current national triage guidelines and to compare with current triage processes. Defining “serious injury” in older adults also remains unclear, as definitions used for younger populations may not be appropriate.
Using a large multi-site cohort of injured adults ≥ 65 years transported by EMS, we sought to: (1) define the high-risk injured older adult using prognostic differences associated with different injury patterns; and (2) derive alternative field trauma triage guidelines that mesh with current national guidelines to improve identification of high-risk elderly trauma patients. This study builds upon recent work developing triage guidelines specific to injured older adults.19–21 Sixteen Institutional Review Boards at 7 sites approved this protocol and waived the requirement for informed consent.
MATERIALS and METHODS
Study Design
This was a multi-site retrospective cohort study.
Study Setting
The study included injured older adults who were evaluated by 94 EMS agencies transporting to 122 hospitals (including 15 Level I, 8 Level II, 3 Level III, 4 Level IV, 1 Level V and 91 community/private/federal hospitals) in 7 regions across the Western U.S. from January 1, 2006 through December 31, 2008. The 7 regions included: Portland, OR/Vancouver, WA (4 counties); King County, WA; Sacramento, CA (2 counties); San Francisco, CA; Santa Clara, CA (2 counties); Denver County, CO; and Salt Lake City, UT (4 counties). Regions were based on EMS agency service areas, typically including a central metropolitan region and some surrounding rural areas.
Selection of Participants
The study sample included all injured adults ≥ 65 years transported by EMS to an acute care hospital (trauma and non-trauma centers) with a matched hospital record available. This cohort of patients approximates the group of older adults to whom field triage guidelines are routinely applied and includes patients with mild, moderate and serious injuries of all types. We restricted the sample to patients ≥ 65 years due to the high rate of under-triage in this age group,4,5,8 large trauma-related mortality,22,23 high prevalence of comorbidities and medication use, and previous research suggesting that the importance of individual triage criteria changes when older adults are defined as ≥ 65 years versus ≥ 55 years.19 We excluded inter-hospital transfers without an initial EMS presentation, non-transported patients and deaths in the field.
Measurements
We included the following out-of-hospital variables in the analysis: age; sex; initial out-of-hospital physiology (Glasgow Coma Scale [GCS] score, systolic blood pressure [SBP], respiratory rate and heart rate); need for assisted ventilation (bag-valve mask ventilation, intubation, supraglottic airway or cricothyrotomy); 23 field trauma triage criteria currently in use at these sites; mechanism of injury (15 categories); hospital destination; and EMS reason for selecting a particular hospital. We also captured a composite, dichotomous measure of field triage to reflect actual triage practices by EMS personnel. To minimize misclassification bias, field triage status was compiled from multiple data sources, including EMS charts, matched trauma registry records and matched EMS phone records from base hospitals. For purposes of the analysis, we collapsed EMS reason for hospital selection to a dichotomous term of patient choice versus other reasons, based on previous research suggesting that patients requesting particular hospitals may have better prognosis.24 We categorized acute care hospitals as major trauma centers (Level I and II trauma hospitals) based on American College of Surgeons accreditation status and state designation versus non-trauma hospitals.
Outcomes
We used Abbreviated Injury Scale (AIS) scores25 to create 5 definitions of “serious injury” (AIS ≥ 3) and considered in-hospital mortality as a marker of prognosis to compare definitions. The definitions included: Injury Severity Score (ISS) ≥ 16;26 serious traumatic brain injury (TBI, maximum head AIS ≥ 3 or any intra-cranial procedure); serious chest injury (maximum thoracic AIS ≥ 3 or thoracic surgery); serious abdomen-pelvic injury (maximum abdominal-pelvic AIS ≥ 3, therapeutic laparotomy or pelvic surgery); and serious extremity injury (maximum upper or lower extremity AIS ≥ 3 or orthopedic surgery on the extremities). Surgical procedures in each of the body regions were included to account for major interventional procedures reflecting serious injuries, in addition to standard AIS scoring. The region-specific surgical procedures were coded based on ICD9-CM procedure codes in the brain, thoracic, abdominal-pelvic and extremity regions that indicated invasive operative management. In addition, operative procedures captured through standardized trauma registry data fields and mapped to these anatomic regions were also used to supplement ICD9-CM procedure codes for surgical interventions. For each of the anatomic regions, we also evaluated isolated serious injury (defined as an AIS ≥ 3 and/or major surgical intervention for a single anatomic region, but with an ISS < 16).
Hospital records from trauma registries, emergency department (ED) databases and discharge databases were used to generate injury severity measures, surgical procedures and in-hospital mortality. These records were matched to EMS records using probabilistic linkage (LinkSolv v8.2, Strategic Matching, Inc.). We have validated the use of record linkage methodology for matching ambulance records to trauma registry data27 and have rigorously evaluated and described use of these methods in the current database.28 Because ISS is not included in administrative data sources, we used a mapping function (ICDPIC .ado Stata module) to generate ISS from ICD-9-CM diagnosis codes,29 which we have validated against manually abstracted ISS values.30
Data Analysis
We used descriptive statistics to characterize the cohort and describe injury patterns for the sample. We then used classification and regression tree (CART) analysis31 to derive an alternative set of field triage guidelines to identify high-risk older adults (v. 8.2, Salford Systems, San Diego, CA). CART uses binary recursive partitioning to create decision trees that optimize the identification of a subgroup of patients through a series of splits in the data based on potential predictor variables, pre-specified misclassification costs and tree complexity parameters. We randomly-selected 60% of the sample to derive and cross-validate32 the decision tree, and then used the remaining 40% to internally validate the tree. We employed ISS ≥ 16 as the primary outcome to develop the decision rule, but also derived decision trees using the anatomic-specific definitions of serious injury for comparison. Thirty-three variables were considered as potential predictors: patient demographics; individual triage criteria; dichotomous field triage status using current guidelines; physiologic measures; need for assisted ventilation (bag-mask ventilation or attempted intubation); mechanism of injury; and patient choice for hospital destination. We tested trees with and without patient choice included as a predictor to determine the role of this factor in field triage. Misclassification costs were selected to generate a tree targeted to national benchmarks for triage sensitivity (≥ 95%) and specificity (≥ 65%).33 We combined the most consistent portions of decision trees developed using ISS ≥ 16 and the anatomic-specific outcomes into a composite set of triage guidelines appropriate for field use, then tested the accuracy of the composite rule using the validation sample.
We used multiple imputation34 to handle missing data for key variables, including: GCS (21%); SBP (7%); respiratory rate (10%); heart rate (7%); assisted ventilation (2%); mechanism of injury (30%); reason for destination selection (36%); gender (1%); and hospital type (< 1%). The use of multiple imputation in handling missing trauma data has been validated35 and rigorously evaluated in this database.28 We used flexible chains regression models for multiple imputation (IVEware, Survey Methodology Program, Survey Research Center, Institute for Social Research, University of Michigan, MI)36 with generation of 10 multiply imputed datasets, each analyzed independently and combined using Rubin’s rules to appropriately account for variance within- and between-datasets.34
We used SAS (v. 9.2, SAS Institute, Cary, NC) for database management and descriptive statistics.
RESULTS
There were 33,298 injured adults ≥ 65 years transported by EMS during the study period with a matched hospital record available. The sample included 1,507 (4.5%) patients with ISS ≥ 16, 1,599 (4.8%) with serious TBI, 1,135 (3.4%) with serious chest injury, 521 (1.6%) with serious abdominal-pelvic injury and 9,732 (29.2%) with serious extremity injury. One thousand thirteen (3.0%) patients died following EMS transport. The majority of the sample (80%) was injured by falls. Descriptive characteristics of the sample are presented in Table 1.
Table 1.
Characteristics of injured patients 65 years and older transported by EMS in 7 regions (n = 33,298).
| Demographics: | |
| 65 – 74 years | 8,448 (25.4%) |
| 75 – 84 years | 12,588 (37.8%) |
| ≥85 years | 12,262 (36.8%) |
| Female | 22,587 (67.8%) |
| Out-of-hospital physiology and procedures: | |
| SBP < 100 mmHg | 1,274 (3.8%) |
| GCS 13 – 15 | 32,035 (96.2%) |
| GCS 9 – 12 | 840 (2.5%) |
| GCS ≤ 8 | 423 (1.3%) |
| Assisted ventilation or intubation attempt | 209 (0.6%) |
| Mechanism of Injury: | |
| Gunshot wound | 40 (0.1%) |
| Stabbing | 69 (0.2%) |
| Assault | 188 (0.6%) |
| Fall | 26,503 (79.6%) |
| Motor vehicle crash | 3,309 (9.9%) |
| Pedestrian vs. auto | 418 (1.3%) |
| Bicycle | 107 (0.3%) |
| Other | 2,664 (8.0%) |
| EMS triage and transport: | |
| ≥1 field triage criterion | 8,382 (25.2%) |
| Helicopter scene transport | 43 (0.1%) |
| Inter-hospital transfer after initial EMS transport | 1,017 (3.1%) |
| Final care in Level I or II trauma center | 9,063 (27.2%) |
| EMS reason for hospital selection: | |
| Patient or family choice | 24,058 (72.3%) |
| Hospital proximity | 3,630 (10.9%) |
| Specialty hospital | 2,676 (8.0%) |
| Ambulance diversion | 682 (2.1%) |
| On-line medical control or MD request | 428 (1.3%) |
| Other | 1,826 (5.5%) |
| Injury severity, hospital procedures and mortality: | |
| ISS 0 – 8 (minor injury) | 24,624 (74.0%) |
| ISS 9 – 15 (moderate injury) | 7,167 (21.5%) |
| ISS ≥ 16 (serious injury) | 1,507 (4.5%) |
| Serious TBI | 1,599 (4.8%) |
| Serious chest injury | 1,135 (3.4%) |
| Serious abdominal-pelvic injury | 521 (1.6%) |
| Serious extremity injury | 9,732 (29.2%) |
| Major non-orthopedic surgery | 1,372 (4.1%) |
| Orthopedic surgery | 9,112 (27.4%) |
| Blood transfusion | 4,923 (14.8%) |
| In-hospital mortality | 1,013 (3.0%) |
ISS = Injury Severity Score; SBP = systolic blood pressure (in mmHg); GCS = Glasgow Coma Scale score; EMS = emergency medical services; ISS = Injury Severity Score; TBI = traumatic brain injury.
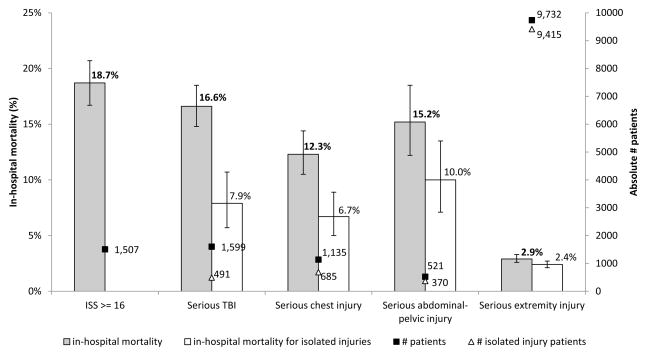
We identified differences in the proportion of patients meeting each of the five definitions of serious injury and their associated mortality (Figure 1). Injury Severity Score ≥ 16 had the highest in-hospital mortality (18.7%, 95% CI 16.7–20.7), though patients with serious brain, chest and abdominal-pelvic injury patterns had only slightly lower mortality (12.3%–16.6%). Patients with serious extremity injuries were common and often presented as an isolated injury; this injury pattern had the lowest mortality (2.9%, 95% CI 2.6–3.3). Patients with isolated serious injury were less common overall and had lower associated in-hospital mortality than polytrauma patients; for patients with serious extremity injury, these differences were minimal.
Figure 1.
Frequency and mortality for different definitions of “serious injury” in injured patients over 65 years transported by EMS (n = 33,298).
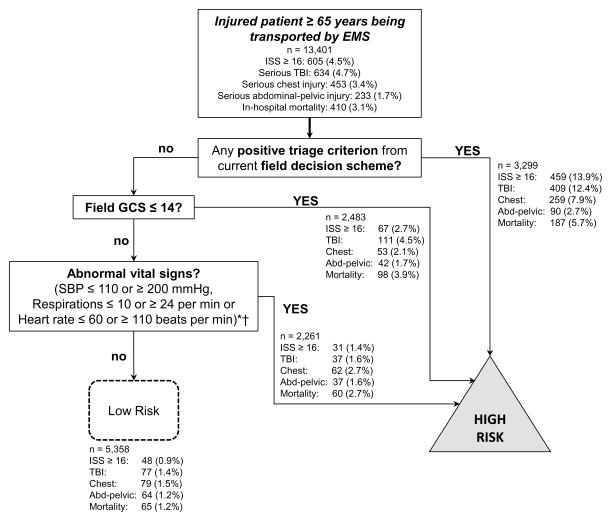
We used 19,897 patients to derive the alternative triage guidelines and 13,401 patients to validate their diagnostic accuracy compared to current triage guidelines. The alternative triage guidelines included: any positive triage criterion from the current guidelines; GCS ≤ 14; and abnormal vital signs (Figure 2). Compared to current field triage practices (sensitivity 75.9%, 95% CI 72.3–79.2%; specificity 77.8%, 95% CI 77.1–78.5%), the alternative guidelines had higher sensitivity (92.1%, 95% CI 89.6–94.1%) and lower specificity (41.5%, 95% CI 40.6–42.4%), as demonstrated in Table 2. Using area under the curve, the current guidelines generally had higher discrimination in correctly classifying older adults with and without serious injuries, despite having lower sensitivity. The vital sign parameters proposed in Figure 2 are broader than current field triage physiologic criteria (GCS ≤ 14 vs. GCS ≤ 13; SBP ≤ 110 or ≥ 200 vs. SBP < 90; respiratory rate ≤ 10 or ≥ 24 vs. respiratory rate < 10 or > 29) and include heart rate (≤ 60 or ≥ 110), which is not a current triage criterion. Most patients in the sample identified solely by the abnormal vital signs step had a single vital sign abnormality. In simulating use, the alternative guidelines would have identified an additional 98 patients with ISS ≥ 16 (67% reduction in under-triage), while targeting an additional 4,645 patients without serious injuries for transport to major trauma centers (164% increase in over-triage). The alternative triage guidelines were less sensitive for identifying patients with anatomic-specific serious injuries, yet they did improve upon the deficits in identifying such patients by current triage guidelines (Table 2).
Figure 2.
Alternative out-of-hospital method for identifying older adults with Injury Severity Score ≥ 16 (validation sample n = 13,401).
*Including high-risk mechanism (fall, motor vehicle occupant, auto vs. pedestrian/bicycle, significant medical illness, or suffocation) as a separate triage criterion following the “abnormal vital signs” step increased sensitity (99.8%) with a severe decrease in specificity (1.6%). Coupling abnormal vital signs with high-risk mechanisms at this step slightly decreased sensitivity (90.4%), but increased specificity (48.5%).
†Patient choice (patients requesting a specific hospital) was considered as an additional predictor in decision rule derivation. This factor was not predictive of patients with ISS ≥ 16 or serious chest injuries. However, the lack of patient choice (hospitals selected by EMS for reasons other than patient choice) increased the probability of having serious abdominal injury and serious TBI. This factor may represent another aspect to consider in the out-of-hospital risk assessment of older patients.
Table 2.
Accuracy measures of the alternative triage guidelines compared to current triage guidelines for identifying seriously injured patients 65 years and older (validation sample n = 13,401).
| Current triage guidelines | Alternative triage guidelines | |
|---|---|---|
| ISS ≥ 16: | n = 605 | |
| Sensitivity | 75.9% (72.5–79.3%) | 92.1% (89.8–94.5%) |
| Specificity | 77.8% (77.1–78.5%) | 41.5% (40.6–42.4%) |
| AUC | 0.77 (0.75– 0.79) | 0.67 (0.66–0.68) |
| # patients under-triaged | 146 | 48 |
| # patients over-triaged | 2,840 | 7,485 |
| Serious TBI: | n = 634 | |
| Sensitivity | 64.5% (60.8–68.2%) | 87.9% (85.2–90.5%) |
| Specificity | 77.4% (76.6–78.1%) | 41.4% (40.5–42.2%) |
| AUC | 0.71 (0.69–0.73) | 0.65 (0.63–0.66) |
| # patients under-triaged | 225 | 77 |
| # patients over-triaged | 2,890 | 7,485 |
| Serious chest injury: | n = 453 | |
| Sensitivity | 57.2% (52.6–61.7%) | 82.6% (79.0–86.3%) |
| Specificity | 76.5% (75.8–77.3%) | 40.8% (39.9–41.6%) |
| AUC | 0.67 (0.65–0.69) | 0.62 (0.60–0.64) |
| # patients under-triaged | 194 | 79 |
| # patients over-triaged | 3,040 | 7,668 |
| Serious abdominal-pelvic injury: | n = 233 | |
| Sensitivity | 38.6% (32.4–44.9%) | 72.5% (66.2–78.8%) |
| Specificity | 75.6% (74.9–76.4%) | 40.2% (39.4–41.1%) |
| AUC | 0.57 (0.54–0.60) | 0.56 (0.53–0.60) |
| # patients under-triaged | 143 | 64 |
| # patients over-triaged | 3,209 | 7,874 |
Parentheses represent 95% confidence intervals. ISS = Injury Severity Score; TBI = traumatic brain injury; AUC = area under the curve.
DISCUSSION
Our findings suggest that it is possible to improve the identification of high-risk older adults in the out-of-hospital setting, although over-triage would be expected to increase with changes to field triage practices. We also demonstrate that a global measure of injury severity (ISS ≥ 16) and specific injury patterns (serious brain, chest and abdomen-pelvic injuries) are all associated with substantial mortality and thus may be used to define the high-risk subset of injured older adults. Patients with serious extremity injuries generally had isolated injuries and low mortality, representing an ineffective target for field triage.
We demonstrate that elderly-specific triage guidelines can be applied to the current national triage guidelines. Because the national guidelines are designed for application to all age groups, integrating age-specific triage guidelines without adding undue complexity to the algorithm is a potential challenge. The current national triage guidelines include certain criteria specific to older adults (e.g., “Older adults –SBP < 110 might represent shock after age 65 years”),11 yet these criteria represent a small portion of the algorithm and it is unclear if they have had any meaningful effect on reducing under-triage. The decision scheme developed here is designed for application following completion of the standard triage guidelines, which may allow more straightforward implementation and EMS training without adversely affecting use of the triage algorithm for younger patients. This integration could be further simplified by changing the GCS criterion for all ages to ≤ 14 from the current GCS ≤ 13, as previous research has suggested that this modification would reduce under-triage among all age-groups37 and is of particular value among injured older adults.19–21
We were not able to develop a triage algorithm that had 95% sensitivity,33 without a major decrease in specificity. The inverse relationship between triage sensitivity and specificity has been previously demonstrated.37 Some iterations of the decision tree included high-risk mechanisms of injury (e.g., falls) to further increase sensitivity, though because 80% of patients were injured by falls, such a criterion resulted in an unacceptable drop in specificity. Furthermore, while the alternative triage guidelines were relatively sensitive in identifying patients with ISS ≥ 16, they were less sensitive in identifying patients with specific types of serious injuries. The alternative guidelines improved the identification of older adults with serious injuries, although the overall diagnostic accuracy (as measured through the area under the curve) decreased compared to current triage practices, reflecting major decrements in specificity. These findings demonstrate the challenge in attempting to reach the national target for under-triage – the ability to correctly classify both seriously and non-seriously injured patients may actually decrease in order to reach this target. This trade-off is important for trauma systems and broader healthcare communities to consider. The ability to identify a higher proportion of high-risk patients without a marked decrease in specificity may require additional variables (e.g., point-of-care biomarkers) or more targeted field assessment (e.g., physical exam findings) to raise sensitivity, while preserving specificity and guideline discrimination. Despite these limitations, the alternative triage guidelines identified more high-risk patients than current guidelines, with the opportunity to improve early clinical management to reduce morbidity and mortality among patients with specific injury patterns.
Although our results and those from other recent studies20,21 suggest that methods exist to better identify high-risk injured older adults, this is just the first step in matching patient need with hospital capability. Following field identification of high-risk patients, selection of a hospital destination can be affected by patient choice,24 hospital proximity, provider training, provider experience, weather and geography, and other factors. Even with effective triage guidelines that identify high-risk elders, any of these factors can potentially disrupt the triage process and create mismatches between patient need and hospital capability. We explored the role of patient choice in field triage, but found inconsistent results. While patient choice has been associated with better prognosis24 and therefore could theoretically serve as another factor to consider during field triage, including this measure in field triage guidelines raises potential difficulties related to its subjective nature and variability between individual patients.
Importantly, before adopting and implementing any new guidelines, two factors should be considered. First, because we found that application of our alternative guidelines would increase over-triage, there are potential cost and resource implications for the healthcare system that must be considered. Previous research has suggested that up to 40% of acute care costs among injured patients served by EMS are attributable to low-risk patients being transported to major trauma centers.38 Before adopting new triage guidelines that may further increase over-triage, formal study of these implications (including costs) should be conducted. One such study is currently underway. Second, the role of major trauma centers in caring for older injured adults remains unclear, as research on the survival benefit of providing care for injured older adults in major trauma centers remains mixed.39–41 Discrepancies between studies are likely explained in part due to differences in how “serious injury” is defined (AIS ≥ 339 vs. ISS ≥ 1641 vs. ICD-9 diagnoses with severe mortality risk40). Resource-based measures (e.g., need for surgical intervention, major blood transfusion) are difficult to use as triage targets among older adults due to differences in medical and surgical decision-making regarding procedural interventions18 and aggressiveness of care compared to younger patients.
In previous studies comparing appropriately-triaged and under-triaged older adults with serious injuries, there were no significant survival differences up to 60 days post-injury41 and under-triaged patients appeared to have better prognosis than seriously injured adults transported to major trauma centers.24 As suggested by these studies, there are likely unobserved factors associated with triage that can influence outcome. Simply reducing under-triage may not necessarily translate into improved outcomes among seriously injured older adults. The complex interplay of these factors among injured older adults and their relation to revising field trauma triage requires additional research.
We used a retrospective cohort for this project and restricted the sample to patients who matched to a hospital record, both of which may have introduced bias to the analysis. Our data did not provide information on comorbidities, pre-injury medications, baseline mentation, intoxication or end-of-life preferences, all of which can play important roles in out-of-hospital decision-making. The vital sign values we used in the decision rule were sharpened versions of cut-points we previously developed in a sample of injured adults ≥ 55 years,19 plus heart rate. While the previous study showed only modest improvement in sensitivity among a sample that included patients ≥ 55 years,19 the current study was restricted to patients ≥ 65 years, with greater gains in sensitivity. Whether these findings reflect true age-based differences or otherwise are unclear. We also assumed that all older adults meeting the alternative triage criteria would be transported to major trauma centers, although actual EMS adherence to the guidelines may be lower. For these reasons, the guidelines developed in this study require prospective evaluation and assessment during actual out-of-hospital use. The intent with this study was not necessarily to create the definitive decision tool for identifying high-risk elderly trauma patients, but rather to develop a potential instrument to reduce under-triage that could interface with the national guidelines and deepen the evidence base on this topic.
Under-triage of older adults remains incompletely understood and is likely related to more than just field triage guidelines, many of which we were unable to account for in this study. It is unlikely that simply revising the national triage guidelines will completely resolve discrepancies in under-triage and the resulting disparities in trauma care among older adults. However, the ability to effectively identify older adults with serious injuries shortly after injury is an important first step in providing more effective and comprehensive care for injured elders.
CONCLUSIONS
Our findings suggest that the field triage guidelines could be improved to better identify older adults with serious injuries, with resulting increases in over-triage. Seriously injured elders may be defined using a traditional global anatomic measure of injury severity (ISS ≥ 16) or specific injury patterns involving the brain, chest or abdominal-pelvic regions.
Acknowledgments
We acknowledge and thank all the participating EMS agencies, EMS medical directors, trauma registrars, and state offices that supported and helped provide data for this project.
SOURCE of FUNDING
This project was supported by the Robert Wood Johnson Foundation Physician Faculty Scholars Program; the Oregon Clinical and Translational Research Institute (grant #UL1 RR024140); UC Davis Clinical and Translational Science Center (grant #UL1 RR024146); Stanford Center for Clinical and Translational Education and Research (grant #1UL1 RR025744); University of Utah Center for Clinical and Translational Science (grant #UL1-RR025764 and C06-RR11234); and UCSF Clinical and Translational Science Institute (grant #UL1 RR024131). All Clinical and Translational Science Awards are from the National Institutes of Health National Center for Advancing Translational Sciences. The study sponsors were not involved with study design, data collection, analysis, writing or decision to submit the manuscript for publication.
Footnotes
No authors have any financial or personal conflicts of interest that might bias this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wang HE, Mann NC, Jacobson KE, et al. National characteristics of emergency medical services responses in the United States. Prehosp Emerg Care. 2013;17:8–14. doi: 10.3109/10903127.2012.722178. [DOI] [PubMed] [Google Scholar]
- 2.Albert MLAJ. NCHS data brief, no 130. Hyattsville, MD: National Center for Health Statistics; 2013. Emergency department visits by persons aged 65 and over: United States, 2009–2010. [PubMed] [Google Scholar]
- 3.Newgard C, Zive D, Rea T, et al. A Multi-Site Assessment and Validation of the ACSCOT Trauma Triage Criteria for Identifying Seriously Injured Children and Adults [Abstract] Ann Emerg Med. 2010;56:S28. [Google Scholar]
- 4.Nakamura Y, Daya M, Bulger EM, et al. Evaluating age in the field triage of injured persons. Ann Emerg Med. 2012;60:335–45. doi: 10.1016/j.annemergmed.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang DC, Bass RR, Cornwell EE, Mackenzie EJ. Undertriage of elderly trauma patients to state-designated trauma centers. Archives of surgery. 2008;143:776–81. doi: 10.1001/archsurg.143.8.776. discussion 82. [DOI] [PubMed] [Google Scholar]
- 6.Lehmann R, Beekley A, Casey L, Salim A, Martin M. The impact of advanced age on trauma triage decisions and outcomes: a statewide analysis. American journal of surgery. 2009;197:571–4. doi: 10.1016/j.amjsurg.2008.12.037. discussion 4–5. [DOI] [PubMed] [Google Scholar]
- 7.Cox S, Morrison C, Cameron P, Smith K. Advancing age and trauma: Triage destination compliance and mortality in Victoria, Australia. Injury. 2014;45:1312–9. doi: 10.1016/j.injury.2014.02.028. [DOI] [PubMed] [Google Scholar]
- 8.Xiang H, Wheeler KK, Groner JI, Shi J, Haley KJ. Undertriage of major trauma patients in the US emergency departments. Am J Emerg Med. 2014;32:997–1004. doi: 10.1016/j.ajem.2014.05.038. [DOI] [PubMed] [Google Scholar]
- 9.Haas B, Gomez D, Zagorski B, Stukel TA, Rubenfeld GD, Nathens AB. Survival of the fittest: the hidden cost of undertriage of major trauma. J Am Coll Surg. 2010;211:804–11. doi: 10.1016/j.jamcollsurg.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Haas B, Stukel TA, Gomez D, et al. The mortality benefit of direct trauma center transport in a regional trauma system: a population-based analysis. The journal of trauma and acute care surgery. 2012;72:1510–5. doi: 10.1097/TA.0b013e318252510a. discussion 5–7. [DOI] [PubMed] [Google Scholar]
- 11.Sasser SM, Hunt RC, Faul M, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recommendations and reports : Morbidity and mortality weekly report Recommendations and reports / Centers for Disease Control. 2012;61:1–20. [PubMed] [Google Scholar]
- 12.Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;50:116–9. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Spaniolas K, Cheng JD, Gestring ML, Sangosanya A, Stassen NA, Bankey PE. Ground level falls are associated with significant mortality in elderly patients. J Trauma. 2010;69:821–5. doi: 10.1097/TA.0b013e3181efc6c6. [DOI] [PubMed] [Google Scholar]
- 14.Nishijima DK, Shahlaie K, Sarkar K, Rudisill N, Holmes JF. Risk of unfavorable long-term outcome in older adults with traumatic intracranial hemorrhage and anticoagulant or antiplatelet use. Am J Emerg Med. 2013;31:1244–7. doi: 10.1016/j.ajem.2013.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fortuna GR, Mueller EW, James LE, Shutter LA, Butler KL. The impact of preinjury antiplatelet and anticoagulant pharmacotherapy on outcomes in elderly patients with hemorrhagic brain injury. Surgery. 2008;144:598–603. doi: 10.1016/j.surg.2008.06.009. discussion -5. [DOI] [PubMed] [Google Scholar]
- 16.Martin JT, Alkhoury F, O’Connor JA, Kyriakides TC, Bonadies JA. ‘Normal’ vital signs belie occult hypoperfusion in geriatric trauma patients. The American surgeon. 2010;76:65–9. [PubMed] [Google Scholar]
- 17.Heffernan DS, Thakkar RK, Monaghan SF, et al. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma. 2010;69:813–20. doi: 10.1097/TA.0b013e3181f41af8. [DOI] [PubMed] [Google Scholar]
- 18.Oresanya LB, Lyons WL, Finlayson E. Preoperative assessment of the older patient: a narrative review. JAMA. 2014;311:2110–20. doi: 10.1001/jama.2014.4573. [DOI] [PubMed] [Google Scholar]
- 19.Newgard CD, Richardson D, Holmes JF, et al. Physiologic field triage criteria for identifying seriously injured older adults. Prehosp Emerg Care. 2014;18:461–70. doi: 10.3109/10903127.2014.912707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Werman HA, Erskine T, Caterino J, Riebe JF, Valasek T Members of the Trauma Committee of the State of Ohio EMSB. Development of statewide geriatric patients trauma triage criteria. Prehospital and disaster medicine. 2011;26:170–9. doi: 10.1017/S1049023X11006315. [DOI] [PubMed] [Google Scholar]
- 21.Ichwan B, Darbha S, Shah MN, et al. Geriatric-specific triage criteria are more sensitive than standard adult criteria in identifying need for trauma center care in injured older adults. Ann Emerg Med. 2015;65:92–100. e3. doi: 10.1016/j.annemergmed.2014.04.019. [DOI] [PubMed] [Google Scholar]
- 22.Caterino JM, Valasek T, Werman HA. Identification of an age cutoff for increased mortality in patients with elderly trauma. Am J Emerg Med. 2010;28:151–8. doi: 10.1016/j.ajem.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 23.Johnson CL, Margulies DR, Kearney TJ, Hiatt JR, Shabot MM. Trauma in the elderly: an analysis of outcomes based on age. The American surgeon. 1994;60:899–902. [PubMed] [Google Scholar]
- 24.Newgard CD, Mann NC, Hsia RY, et al. Patient choice in the selection of hospitals by 9-1-1 emergency medical services providers in trauma systems. Acad Emerg Med. 2013;20:911–9. doi: 10.1111/acem.12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abbreviated Injury Scale (AIS) 2005 Manual. Barrington, IL: Association for the Advancement of Automotive Medicine; 2005. [Google Scholar]
- 26.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. [PubMed] [Google Scholar]
- 27.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 28.Newgard C, Malveau S, Staudenmayer K, et al. Evaluating the use of existing data sources, probabilistic linkage, and multiple imputation to build population-based injury databases across phases of trauma care. Acad Emerg Med. 2012;19:469–80. doi: 10.1111/j.1553-2712.2012.01324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark DEOT, Hahn DR. ICDPIC: Stata Module to provide methods for translating International Classification of Diseases (Ninth Revision) Diagnosis Codes into standard injury categories and/or scores. Boston: Boston College, Department of Economics; 2009. [Google Scholar]
- 30.Fleischman RMN, Wang NE, Hsia RY, Rea TD, Liao M, Holmes JF, Newgard CD. Validating The Use Of ICD9 Codes To Generate Injury Severity Score: The ICDPIC Mapping Procedure[Abstract] Acad Emerge Mead. 2012;19:S314. [Google Scholar]
- 31.Breiman LFJ, Stone CJ, Olshen RA. Classification and regression trees. New York: Chapman & Hall; 1984. [Google Scholar]
- 32.Stone M. Cross-validatory choice and the assessment of statistical predictions. J Roy Statist Soc Ser B. 1974;36:111–47. [Google Scholar]
- 33.Resources for the Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2014. [Google Scholar]
- 34.Rubin D. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons, Inc; 1987. [Google Scholar]
- 35.Newgard CD. The validity of using multiple imputation for missing out-of-hospital data in a state trauma registry. Acad Emerg Med. 2006;13:314–24. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 36.Raghunathan T, Lepkowski, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27:85–95. [Google Scholar]
- 37.Newgard CD, Hsia RY, Mann NC, et al. The trade-offs in field trauma triage: a multiregion assessment of accuracy metrics and volume shifts associated with different triage strategies. The journal of trauma and acute care surgery. 2013;74:1298–306. doi: 10.1097/TA.0b013e31828b7848. discussion 306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Newgard CD, Staudenmayer K, Hsia RY, et al. The cost of overtriage: more than one-third of low-risk injured patients were taken to major trauma centers. Health Aff (Millwood) 2013;32:1591–9. doi: 10.1377/hlthaff.2012.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 40.Pracht EE, Langland-Orban B, Flint L. Survival advantage for elderly trauma patients treated in a designated trauma center. J Trauma. 2011;71:69–77. doi: 10.1097/TA.0b013e31820e82b7. [DOI] [PubMed] [Google Scholar]
- 41.Staudenmayer KL, Hsia RY, Mann NC, Spain DA, Newgard CD. Triage of elderly trauma patients: a population-based perspective. J Am Coll Surg. 2013;217:569–76. doi: 10.1016/j.jamcollsurg.2013.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]