Abstract
Objective
To assess the impact of surgery for BPH on use of medication (5-ARIs, alpha blockers, antispasmodics), we assessed pre- and post-operative medication utilization among surgically treated men.
Materials and Methods
Using the Truven Health Analytics MarketScan® Commercial Claims Database, we defined a cohort of men < 65 years of age who had surgical therapy for BPH with either TURP or laser procedures from 2007 through 2009. Primary outcomes included freedom from medical or surgical intervention by 4 months after surgery (chi-square and multivariable logistic regression) and subsequent use of medical or surgical intervention in initial responders (Kaplan-Meier and multivariable Cox regression).
Results
We identified 6430 patients treated with either TURP (3096) or laser procedure (3334) for BPH. Pre-surgical antispasmodic use was associated with the highest risk of medication use at 4 months after surgery (OR 5.19; CI 3.16 to 8.53 versus no medication use prior to surgery). At three years after surgery, 6% (95% CI 4–8%) of laser and 4% (95% CI 2–5%) of TURP treated patients had repeat surgical intervention, and both laser and TURP treated patients had an estimated new use of medication rate of 22% (95% CI 18–25% laser and 20–25% TURP). The strongest predictor of intervention after surgery was pre-operative antispasmodic use (HR 2.49; 95% CI 1.41 to 4.43).
Conclusions
Our results show a need for effective patient counseling about continued or new use of medical therapy after laser and TURP procedures. However, most patients experience durable improvement after surgical intervention for BPH.
Keywords: Benign Prostatic Hyperplasia, Lower urinary tract symptoms, Transurethral Resection of the Prostate, Laser Vaporization, Laser Ablation, Medical Therapy for lower urinary tract symptoms
Introduction
For most men with moderately to severely symptomatic lower urinary tract symptoms due to prostatic enlargement, surgical intervention provides excellent symptomatic relief. Over 70% of men undergoing surgery for LUTS with an enlarged prostate undergo TURP or laser therapy.1 Regardless of modality, excellent improvements in urinary flow, symptom scores, and PVR are seen,2–5 and the results appear to be durable in single institution series beyond 5 years6 and randomized trials out to 2 years.7,8
Despite these excellent results, the use of medical therapy for BPH both before and after surgical intervention has not been well characterized. Most patients, and urologists, see surgical intervention as definitive therapy for LUTS due to BPH that should preclude the need for additional medical therapy. Furthermore, medical therapy for BPH is a significant expense for patients and insurers, and successful elimination of these medications is a goal for many patients. Thus, the effectiveness of the procedure should include a measure of whether medication therapy was used after surgery.
To better inform patients and their providers on the effectiveness of surgery for LUTS, we undertook a study of medication use before and after surgical intervention for BPH. First, we asked whether men discontinued pre-operative BPH medication use in the immediate post-operative period, and if discontinuation rates varied between TURP and laser procedures. Second, we determined the rate of initiation of new medication, or receipt of surgical therapy, over longer follow up after surgery. We hypothesized that, consistent with prior population based studies,9,10 laser procedures would be associated with increased rates of retreatment compared to TURP.
Patients and Methods
Patient Population
Using the Truven Health Analytics MarketScan® Commercial Claims Database, a database of commercially insured patients, we identified a cohort of men < 65 years of age, who had surgical therapy for LUTS with either TURP or laser procedures from 2007 through 2009. This database contains all inpatient claims, outpatient claims, and medication data for patients while they have commercial insurance (from any insurance company) through their employer. Men over the age of 65 were not included from this database, as the data for these men may be incomplete due to Medicare being the primary insurance with the commercial insurance as the secondary coverage. Follow-up records were available through 2010.
Surgical procedures were identified from outpatient and physicians claims data using Common Procedural Terminology codes 52647 and 52648 (laser), and 52450 and 52601 (TURP). Inpatient surgical procedures were identified using International Classification of Disease 9th edition (ICD-9-CM) procedure codes 60.21 (laser) and 60.0, 60.00, 60.2, 60.20, and 60.29 (TURP). In cases where both CPT and ICD-9 codes were available, the CPT code was used to identify the procedure. All men were required to have an ICD-9 diagnosis consistent with BPH or lower urinary tract symptoms (594.1, 599.6, 600.0, 600.2, 600.9, 788.2, 788.21, 788.29, 788.41, 788.42, 788.43, 788.61, 788.62). To help ensure patients were not receiving therapy for complications from prior surgery or for other diagnoses, we excluded men who had surgical therapy in the year prior to the index procedure, or who had a diagnosis consistent with bladder cancer, prostate cancer, Parkinson’s disease, multiple sclerosis, hemi paralysis, paralysis syndrome, or cerebrovascular disease in the year prior to the index procedure. We did not include men with laser enucleation procedures (CPT code 52649).
Medication Utilization
We assessed outpatient medication use related to LUTS: 5-alpha reductase inhibitors (finasteride, dutasteride), alpha-blockers (doxazosin, terazosin, tamsulosin, alfuzosin, silodosin), and antispasmodics (oxybutynin, tolterodine, solifenacin, trospium, fesoterodine, darifenacin, propiverine)]. The data set includes filled prescriptions for medications. Pre-operative medical therapy was defined as medication possession rate of greater than 80% in the year prior to surgery. We also explored using active medication at the time of BPH related surgery as the marker of medication use, but we found no difference in percentage of men on medication at the time of surgery. We then examined the data for new filled prescriptions for BPH related medication after surgery. We required all men to have at least 4 months of insurance coverage after surgical intervention for assessment of post intervention medications use.
Effectiveness of Surgical Intervention
We developed a combined outcome for effectiveness of surgery including use of medical therapy related to LUTS or repeat surgery. Repeat surgery was identified from inpatient and outpatient claims for surgery related to BPH or complications of prior surgery using procedure codes (Appendix 1). We examined the data for use of medications or surgery up to four-months after surgery. This four-month window was used to allow discontinuation of 90-day supplied pre-operative medical therapy. By this measure of short-term effectiveness we identified a group who underwent early medical or surgical reintervention and, conversely, a group of initial responders (no early reintervention).
The long-term effectiveness of surgical intervention was similarly assessed by the combined endpoint of surgical intervention and new medical therapy starting 4 months after surgery among the group of initial responders. Men were censored at loss of their insurance coverage or at the end of the data.
Statistical Analysis
We assessed for differences in baseline characteristics between patients receiving TURP and laser therapy through chi-square testing for categorical variables and t-test for continuous variables.
Types of medications used by TURP and laser patients were compared before and 4 months after surgery by chi-square testing. We then assessed the impact of type of medication used prior to surgery, patient age, comorbidity, the year of the procedure, and type of surgery on short-term success through logistic regression analysis.
Comorbidity was defined based on inpatient and outpatient claims for the year prior to the index surgery.11 Interactions between medication use and surgical procedure were tested and no significant results were found. Thus, we report the primary effects only.
Among initial responders, we assessed the long-term effectiveness of laser and TURP procedures through competing risk analysis accounting for surgical and medical interventions after therapy. We then examined factors associated with starting new medications or having repeat surgery including medication use prior to surgery, patient age, comorbidity, and the year of the procedure, and type of surgery with Cox proportional hazards regression analysis.
Results
We identified 6430 patients who were treated with either TURP (3096 patients) or a laser procedure (3334 patients) for BPH from 2007–2009 (Appendix 2). Patient age (p = 0.56), year of surgery (p = 0.93), and comorbidity (p = 0.05) were not significantly different between patients treated with TURP and laser therapy. We found no difference in the proportion of patients using BPH medication in the year prior to surgery (49% TURP, 48% laser), however laser-treated patients used slightly more alpha-blocker (34.1% versus 32.6%) and anti-spasmodic medications (1.2% versus 0.9%) while TURP patients had higher use of 5-alpha reductase inhibitors (7.9% versus 6.2%) (p = 0.025 for all categories).
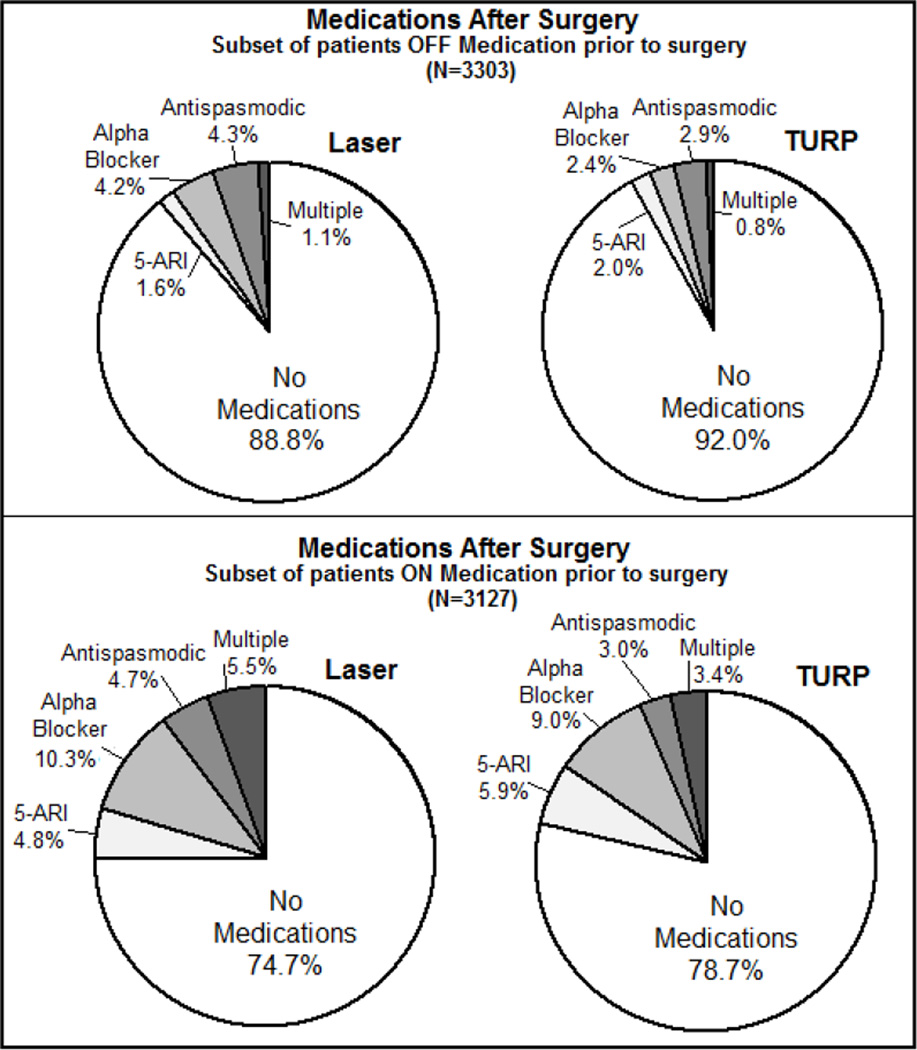
At four months after surgery, TURP patients were less likely to be on medical therapy than patients treated with laser procedures (15% versus 18%; p < 0.001). Distributions and types of medication for LUTS after surgery stratified by pre-operative medication use are shown in Figure 1. Among patients who were not on medication prior to surgery, 89% of those treated with laser procedures remained off medication at 4 months after surgery compared to 92% of those treated with TURP (p = 0.006). Antispasmodic medication was the most common type of medication used after surgery (4.3% laser and 2.9% TURP) among patients off medication before surgery. Among men on BPH medication pre-operatively, those treated with laser therapy were less likely than those treated with TURP to be off medical therapy at 4 months post-operatively (74.7% compared to 78.7% p = 0.001). Alpha-blocker medications were the most common medication used in both groups. Repeat surgery within 4 months of the initial procedure occurred in a small percentage of patients (4% TURP and 4% laser).
Figure 1. Medication use four months after laser and TURP procedures.
TURP patients were more likely to be off medication after surgery than were laser patients regardless of medication use prior to surgery. Patients requiring new medication after surgery were split between use of alpha-blocker medication and antispasmodics. Patients continuing medication after surgery were commonly using alpha-blocker medications. Antispasmodic use was higher in laser treated patients and 5-alpha reductase inhibitor use was higher in TURP treated patients.
After controlling for potential confounding (Table 1) laser procedures remained significantly associated with a higher probability of retreatment by four months after surgery (OR 1.28; 95% CI 1.13 to 1.45). However, prior medication use was associated with much higher risks of retreatment, with pre-surgical antispasmodic use associated with the highest risk of continued or new therapy (OR 5.19 CI 3.16 to 8.53 versus no medication use prior to surgery). Older patients were more likely to have retreatment than younger patients (OR 1.06 per year increase in age; 95% CI 1.04 to 1.07). We found no association between year of the procedure and failure at 4 months.
Table 1.
Logistic regression results for probability of retreatment at 4 months after the procedure*
| 95% Confidence Intervals |
||||
|---|---|---|---|---|
| Effects | OR | Lower | Upper | P-values |
| Medications Used before Procedure | ||||
| None | ref | |||
| 5-ARI | 2.92 | 2.33 | 3.66 | <0.001 |
| Alpha Blocker | 1.95 | 1.69 | 2.25 | <0.001 |
| Anti-Spasmodic | 5.19 | 3.16 | 8.53 | <0.001 |
| Multiple Medications | 2.49 | 1.98 | 3.13 | <0.001 |
| Age (Per year) | 1.06 | 1.04 | 1.07 | <0.001 |
| Comorbidity | ||||
| 0 | ref | |||
| 1 | 1.16 | 0.98 | 1.38 | 0.088 |
| >=2 | 1.39 | 1.11 | 1.76 | 0.005 |
| Surgery Year | ||||
| 2009 | ref | |||
| 2007 | 1.02 | 0.87 | 1.20 | 0.776 |
| 2008 | 1.04 | 0.90 | 1.21 | 0.590 |
| Laser vs. TURP | 1.28 | 1.13 | 1.45 | <0.001 |
Retreatment was defined as filled prescriptions for medical therapy or surgery up to 4 months after the initial surgical procedure.
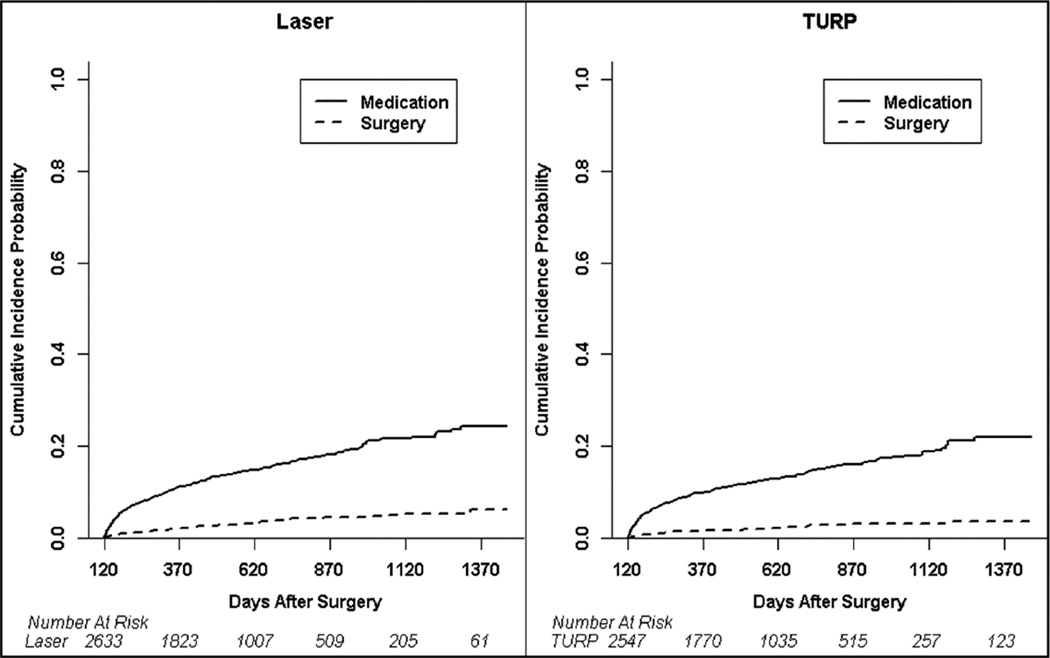
New use of surgical or medical therapy after 4 months post-surgery was rare among the 2633 laser patients and 2547 TURP patients who were initial responders. At three years after surgery (Figure 2), 6% (95% CI 4–8%) of laser treated and 4% (95% CI 2–5%) of TURP treated patients had repeat surgical intervention, and both laser and TURP treated patients had an estimated new use of medication rate of 22% (95% CI 18–25% laser and 20–25% TURP). In a Cox proportional hazards model analyzing time to failure within 3 years after the index procedure (Table 2), the strongest predictor of intervention after surgery was pre-operative antispasmodic use (HR 2.49; 95% CI 1.41 to 4.43). Increasing age, comorbidity, and use of multiple medications prior to surgical intervention were all associated with intervention after initially successful surgery for LUTS. Laser therapy showed a higher hazard rate for subsequent intervention compared to TURP (HR 1.22; 95% CI 1.06 to 1.40).
Figure 2. Efficacy of laser and TURP procedures.
Patients off medical therapy and without failure by four months after surgery were examined for long-term efficacy of the procedures. The estimated probability of freedom from medical or surgical therapy at 3 years was 73.6% in the laser patients (95% CI, 71% to 76.2%) compared to 78.8% in the TURP patients (95% CI, 76.5% to 81.2%)
Table 2.
Adjusted Analysis of Time to Intervention after TURP and Laser procedures*
| 95% Confidence Intervals |
||||
|---|---|---|---|---|
| Effects | HR | Lower | Upper | P- values |
| Medications Used before Procedure | ||||
| None | ref | |||
| 5-ARI | 0.98 | 0.73 | 1.32 | 0.887 |
| Alpha Blocker | 1.04 | 0.90 | 1.21 | 0.581 |
| Anti-Spasmodic | 2.49 | 1.41 | 4.43 | 0.002 |
| Multiple Medications | 1.37 | 1.07 | 1.75 | 0.014 |
| Age (years) | 1.08 | 1.06 | 1.10 | <0.001 |
| Comorbidity | ||||
| 0 | ref | |||
| 1 | 1.10 | 0.91 | 1.32 | 0.331 |
| >=2 | 1.39 | 1.08 | 1.78 | 0.011 |
| Surgery Year | ||||
| 2009 | ref | |||
| 2007 | 1.02 | 0.86 | 1.21 | 0.838 |
| 2008 | 0.96 | 0.81 | 1.14 | 0.619 |
| Laser vs. TURP | 1.22 | 1.06 | 1.40 | 0.004 |
A Cox proportional hazards model was fit with the outcome being use of medical or surgical therapy after initial successful surgical therapy with either laser or TURP. Medication used reflect the pre-operative medications used by patients.
Discussion
We found that surgery for BPH is successful in eliminating the need for medical therapy in over 75% of patients who use medication prior to surgery. However up to 10% of patients who are not using medical therapy for LUTS prior to surgery are using medications after the procedure. A significant difference exists in the risk of continued and new medical therapy comparing TURP and laser procedures. However, medication use prior to surgical intervention had a stronger association with new or continued medication use after surgery.
These results focus attention on the risks and benefits of surgical intervention for BPH. In properly selected patients, TURP and laser procedures are highly effective in decreasing LUTS.3 These improvements in symptom scores are far greater than can be achieved with medical therapy.12 Despite these improvements, all interventions have risks. Our results highlight the risk of new medical therapy in men who are not using medications at the time of surgery. For the 50% of patients who received surgical therapy while on no medications, this likely represents an unexpected complication of therapy. In 2008 in the Medicare program alone, over 101,000 men received surgical intervention for LUTS.13 Therefore, a large population of men is at risk for new or continued medication use after surgery intended to definitively treat their symptoms.
The use of medical therapy around the time of surgical intervention has been poorly characterized. Many randomized studies of surgical intervention for patients with BPH do not include information on use of medications before and after surgical intervention.14,15 When information on initial post operative medication use is provided, it is in the context of post operative urinary urgency and the use of antispasmodic medications, and specific information on discontinuation or new use of medication is not provided.16 Furthermore, long-term efficacy results for laser and TURP procedures lack the important outcome of resumption of medical therapy. Single institution studies have provided some information on use of medications after surgery, and consistent with our study found many men were not on medications prior to intervention and many men continued medical therapy after the procedure.17 Our study expands on these prior results in a population-based framework.
By quantifying the risk of continued or new medical therapy after surgery, our study provides additional information for patients and surgeons on the risks and benefits of surgical intervention for BPH. A detailed discussion of intervention options is central to decision making for surgical therapy in BPH, and is called for in current AUA guidelines.18 Full disclosure on possible continued or new medication use is needed for all patients prior to choosing surgical intervention. This information may affect decision making regarding surgery since most men with BPH who see a urologist do not choose surgery for their symptoms.19 Also, improved knowledge of possible medication use after surgical intervention better sets patient expectations regarding surgery and will help improve satisfaction with the surgical intervention. This is especially true among men who are already using antispasmodic medications at the time of surgery who are at the highest risk for both short- and long-term retreatment. Many of these men will continue to require medication for their bladder instability, even if their overall voiding symptoms improve.
The results found in this paper need to be considered within the context of the following limitations. First, the data was from an administrative database from which patient symptom scores or objective measures of disease severity are not available. Therefore, we chose to measure success of therapy by reuse of surgery or medical therapy. Second, our population was men between 39 and 65 years of age. Over 98% of men were over 45 years of age, over 94% were older than 50 years of age, and over 42% were over 60 years of age. These men are at an age where initial LUTS symptoms and treatments occur. However, results may be different in an older group of men. Third, we examined medication use for one year prior to surgery. We cannot determine if longer use of medications prior to BPH surgery would lead to different results. Fourth, the study was observational and not randomized. There may be differences between the types of patients treated with laser and TURP that could account for the small difference in retreatment rates between the two procedures. Finally, medication use was determined by the filling of a prescription. The use of filled prescriptions likely accounts for the seemingly high rate of surgery in men receiving surgery while not on BPH related medication. In unpublished data from our own institution, we found about 25% of patients had surgery when there was no active BPH related medication on their chart. Since many patients do not fill prescribed medication, the actual use of medication at the time of surgery is likely closer to that seen in the current data set. Finally, in both administrative data and chart review, patient compliance with medication cannot be assessed. By assessing results at 4 months after surgery we assured that no men were still covered by prescriptions filled prior to or just after surgical intervention.
Conclusions
Our results show a need for effective patient counseling about continued or new use of medical therapy after laser and TURP procedures. Antispasmodic medication use prior to surgery is most associated with new or continued medication use after surgery. However, most patients experience durable improvement after surgical intervention for BPH without need for subsequent medical or surgical intervention.
Acknowledgement
Additional support for this publication was provided by the Washington University KL2 Career Development Awards Program (KL2 TR000450) and a National Institute of Diabetes and Digestive and Kidney Diseases Clinical Investigator Award (1K08DK097302-01A1).
The Center for Administrative Data Research is supported in part by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH), and Grant Number R24 HS19455 through the Agency for Healthcare Research and Quality (AHRQ).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Appendix 1
Codes for repeat surgery
| Code Type | Procedure Name | Code |
|---|---|---|
| Transurethral incision of prostate | 52450 | |
| Transurethral electrosurgical resection of prostate | 52601 | |
| Transurethral resection; residual or regrowth of obstructive tissue | 52620 | |
| Transurethral resection; residual or regrowth of obstructive tissue | 52630 | |
| Transurethral resection of postoperative bladder neck contracture | 52640 | |
| Laser coagulation of prostate | 52647 | |
| Laser vaporization of prostate | 52648 | |
| Laser enucleation of prostate | 52649 | |
| Transurethral microwave therapy (TUMT) | 53850 | |
| Transurethral needle ablation (TUNA) | 53852 | |
| Prostatectomy, perineal, subtotal | 55801 | |
| Prostatectomy, suprapubic, subtotal | 55821 | |
| Prostatectomy, retropubic, subtotal | 55831 | |
| ICD-9 | Incision of prostate | 600.0 |
| Transurethral prostatectomy | 602.0 | |
| Ablation contact or non-contact by laser | 602.1 | |
| Other transurethral prostatectomy | 602.9 | |
| Suprapubic prostatectomy | 603.0 | |
| Retropubic prostatectomy | 604.0 | |
| Local excision of prostatic lesion | 606.1 | |
| Control of postoperative hemorrhage of prostate | 609.4 | |
| Transurethral balloon dilation of the prostatic urethra | 609.5 | |
| Transurethral microwave therapy (TUMT) | 609.6 | |
| Other transurethral destruction of prostatic tissue | 609.7 |
Appendix 2
Demographics and Baseline Medication use in the Cohort
| TURP | Laser | p-value | |
|---|---|---|---|
| Number of Patients | 3096 | 3334 | |
| Age (Years) | Mean 58.5 Median 60 IQR 56 to 62 |
Mean 58.4 Median 60 IQR 56 to 62 |
0.557 |
| Follow Up Time (Days) | Mean 639 Median 573 IQR 387.5 to 857 |
Mean 639 Median 582.5 IQR 393 to 857 |
0.932 |
| Procedure Codes (Laser) | |||
| 52647 | 340 | ||
| 52648 | 2931 | ||
| 60.21 | 63 | ||
| Procedure Codes (TURP) | |||
| 52450 | 245 | ||
| 52601 | 2745 | ||
| 60.0 | 19 | ||
| 60.00 | 0 | ||
| 60.2 | 0 | ||
| 60.20 | 0 | ||
| 60.29 | 87 | ||
| Year of Surgery | |||
| 2007 | 27.7% | 27.8% | 0.933 |
| 2008 | 32.4% | 32.7% | |
| 2009 | 39.9% | 39.5% | |
| Comorbidity | 0.048 | ||
| 0 | 75.6% | 78.0% | |
| 1 | 16.6% | 15.5% | |
| ≥2 | 7.8% | 6.5% | |
| Medication Use | 0.047 | ||
| 5-alpha Reductase Inhibitor | 7.85% | 6.21% | |
| Alpha Blocker | 32.62% | 34.16% | |
| Anti-spasmodic | 0.94% | 1.17% | |
| Multiple | 7.56% | 6.78% | |
| None | 51.03% | 51.68% |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Yu X, Elliott SP, Wilt TJ, McBean AM. Practice patterns in benign prostatic hyperplasia surgical therapy: the dramatic increase in minimally invasive technologies. J Urol. 2008;180:241–245. doi: 10.1016/j.juro.2008.03.039. discussion 245. [DOI] [PubMed] [Google Scholar]
- 2.Te AE, Malloy TR, Stein BS, Ulchaker JC, Nseyo UO, Hai MA, Malek RS. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia: 12-month results from the first United States multicenter prospective trial. J Urol. 2004;172:1404–1408. doi: 10.1097/01.ju.0000139541.68542.f6. [DOI] [PubMed] [Google Scholar]
- 3.Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, Speakman MJ, Stief CG. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol. 2010;58:384–397. doi: 10.1016/j.eururo.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Bachmann A, Tubaro A, Barber N, d'Ancona F, Muir G, Witzsch U, Grimm MO, Benejam J, Stolzenburg JU, Riddick A, et al. 180-W XPS GreenLight laser vaporisation versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6-month safety and efficacy results of a European Multicentre Randomised Trial--the GOLIATH study. Eur Urol. 2014;65:931–942. doi: 10.1016/j.eururo.2013.10.040. [DOI] [PubMed] [Google Scholar]
- 5.Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, McVary K, Novara G, Woo H, Madersbacher S. A Systematic Review and Meta-analysis of Functional Outcomes and Complications Following Transurethral Procedures for Lower Urinary Tract Symptoms Resulting from Benign Prostatic Obstruction: An Update. Eur Urol. 2015;67:1066–1096. doi: 10.1016/j.eururo.2014.06.017. [DOI] [PubMed] [Google Scholar]
- 6.Kuntz RM, Lehrich K, Ahyai SA. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol. 2008;53:160–166. doi: 10.1016/j.eururo.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 7.Al-Ansari A, Younes N, Sampige VP, Al-Rumaihi K, Ghafouri A, Gul T, Shokeir AA. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol. 2010;58:349–355. doi: 10.1016/j.eururo.2010.05.026. [DOI] [PubMed] [Google Scholar]
- 8.Capitan C, Blazquez C, Martin MD, Hernandez V, de la Pena E, Llorente C. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia: a randomized clinical trial with 2-year follow-up. Eur Urol. 2011;60:734–739. doi: 10.1016/j.eururo.2011.05.043. [DOI] [PubMed] [Google Scholar]
- 9.Elliott SP, Yu X, Strope SA, McBean AM. Comparative Effectiveness of Surgical Therapies for Benign Prostatic Hyperplasia. J Urol. 2012;187:e28–e29. [Google Scholar]
- 10.Strope SA, Yang L, Nepple KG, Andriole GL, Owens PL. Population based comparative effectiveness of transurethral resection of the prostate and laser therapy for benign prostatic hyperplasia. J Urol. 2012;187:1341–1345. doi: 10.1016/j.juro.2011.11.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klabunde CN, Legler JM, Warren JL, Baldwin LM, Schrag D. A refined comorbidity measurement algorithm for claims-based studies of breast, prostate, colorectal, and lung cancer patients. Ann Epidemiol. 2007;17:584–590. doi: 10.1016/j.annepidem.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 12.McConnell JD, Roehrborn CG, Bautista OM, Andriole GL, Jr, Dixon CM, Kusek JW, Lepor H, McVary KT, Nyberg LM, Jr, Clarke HS, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2387–2398. doi: 10.1056/NEJMoa030656. [DOI] [PubMed] [Google Scholar]
- 13.Malaeb BS, Yu X, McBean AM, Elliott SP. National trends in surgical therapy for benign prostatic hyperplasia in the United States (2000–2008) Urology. 2012;79:1111–1116. doi: 10.1016/j.urology.2011.11.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar A, Vasudeva P, Kumar N, Nanda B, Jha SK, Mohanty N. A prospective randomized comparative study of monopolar and bipolar transurethral resection of the prostate and photoselective vaporization of the prostate in patients who present with benign prostatic obstruction: a single center experience. J Endourol. 2013;27:1245–1253. doi: 10.1089/end.2013.0216. [DOI] [PubMed] [Google Scholar]
- 15.Autorino R, Damiano R, Di Lorenzo G, Quarto G, Perdona S, D'Armiento M, De Sio M. Four-year outcome of a prospective randomised trial comparing bipolar plasmakinetic and monopolar transurethral resection of the prostate. Eur Urol. 2009;55:922–929. doi: 10.1016/j.eururo.2009.01.028. [DOI] [PubMed] [Google Scholar]
- 16.Montorsi F, Naspro R, Salonia A, Suardi N, Briganti A, Zanoni M, Valenti S, Vavassori I, Rigatti P. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2004;172:1926–1929. doi: 10.1097/01.ju.0000140501.68841.a1. [DOI] [PubMed] [Google Scholar]
- 17.Han HH, Ko WJ, Yoo TK, Oh TH, Kim DY, Kwon DD, Byun SS, Kim SI, Jung TY. Factors associated with continuing medical therapy after transurethral resection of prostate. Urology. 2014;84:675–680. doi: 10.1016/j.urology.2014.04.027. [DOI] [PubMed] [Google Scholar]
- 18.McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, Foster HE, Jr, Gonzalez CM, Kaplan SA, Penson DF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011;185:1793–1803. doi: 10.1016/j.juro.2011.01.074. [DOI] [PubMed] [Google Scholar]
- 19.Strope SA, Wei JT, Smith A, Wilt TJ, Saigal CS, Elliott SP. Evaluative care guideline compliance is associated with provision of benign prostatic hyperplasia surgery. Urology. 2012;80:84–89. doi: 10.1016/j.urology.2012.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]