Abstract
Introduction
Prospective clinical audit of trauma care improves outcomes for the injured in high-income countries (HICs). However, equivalent, context-appropriate audit filters for use in low- and middle-income country (LMIC) district-level hospitals have not been well established. We aimed to develop context-appropriate trauma care audit filters for district-level hospitals in Ghana, was well as other LMICs more broadly.
Methods
Consensus on trauma care audit filters was built between twenty panelists using a Delphi technique with four anonymous, iterative surveys designed to elicit: i) trauma care processes to be measured; ii) important features of audit filters for the district-level hospital setting; and iii) potentially useful filters. Filters were ranked on a scale from 0 – 10 (10 being very useful). Consensus was measured with average percent majority opinion (APMO) cut-off rate. Target consensus was defined a priori as: a median rank of ≥9 for each filter and an APMO cut-off rate of ≥0.8.
Results
Panelists agreed on trauma care processes to target (e.g. triage, phases of trauma assessment, early referral if needed) and specific features of filters for district-level hospital use (e.g. simplicity, unassuming of resource capacity). APMO cut-off rate increased successively: Round 1 - 0.58; Round 2 - 0.66; Round 3 - 0.76; and Round 4 - 0.82. After Round 4, target consensus on 22 trauma care and referral-specific filters was reached. Example filters include: triage - vital signs are recorded within 15 minutes of arrival (must include breathing assessment, heart rate, blood pressure, oxygen saturation if available); circulation - a large bore IV was placed within 15 minutes of patient arrival; referral - if referral is activated, the referring clinician and receiving facility communicate by phone or radio prior to transfer.
Conclusion
This study proposes trauma care audit filters appropriate for LMIC district-level hospitals. Given the successes of similar filters in HICs and obstetric care filters in LMICs, the collection and reporting of prospective trauma care audit filters may be an important step toward improving care for the injured at district-level hospitals in LMICs.
Keywords: trauma, quality improvement, global surgery, developing country, Ghana
Introduction
Injuries are responsible for 5 million deaths and incur 52 million disability-adjusted life years annually, comprising 15% of the global disease burden.1 The urgency of and resource deficiencies for trauma care improvement vary immensely between high-income countries (HICs), where 10% of these deaths occur each year, and low- and middle-income countries (LMICs), where 90% occur.2, 3 Nonetheless, certain tools from trauma care quality improvement in HICs, such as prospective clinical audit, may be useful to LMICs working to reduce avertable death and disability due to injury.4, 5
Given critical resource deficiencies, trauma care improvements should rely on increasing the efficiency and quality of care using low-cost interventions, instead of relying on a bolus of resources.6, 7 Preventable death panel reviews from several LMICs suggest that there is an opportunity to improve trauma care outcomes through low-cost improvements in quality.8 As example, a tertiary hospital in Brazil found that 61% of in-hospital trauma deaths might have been preventable by meeting trauma care standards.9 Similarly, a multidisciplinary panel review of traumatic deaths at a tertiary hospital in Ghana found that 60% of deaths were potentially preventable.10 Similar conclusions from Iran and Pakistan suggest that these findings are not isolated.11, 12 These studies imply that improving the processes of trauma care can prevent death and disability, even in centers with insufficient resources.
In addition to tracking crude or risk-adjusted outcomes (e.g. in-hospital death) or preventable death rates, trauma care can be evaluated by audit filters.13 Audit filters are routinely tracked actions, processes or expectations of care that can be used to identify when standards are not being met.5, 14 In HICs, routinely collected audit filters are used by trauma centers and systems to evaluate care efficiency and quality.15 However, commonly used filters assume a high-level of resources (e.g. sufficient and highly trained personnel, timely access to advanced diagnostics).16 Given that the assumed level of resources is not appropriate for many LMIC hospitals, these filters are not applicable.3 While context-appropriate filters have been used successfully for maternal health quality improvement initiatives in LMICs, audit filters useful for monitoring and evaluating trauma care processes are not well established.4, 17
To address this gap, we aimed to use the Delphi technique to develop consensus on trauma care audit filters that would be accurate proxies of quality trauma care, simple to measure and feasible to collect at district-level hospitals in Ghana. By doing so, the proposed filters could be used to benchmark, monitor and evaluate trauma care processes and quality improvement initiatives at first-level hospitals in LMICs more broadly.
Methods
Setting
Ghana is a heavily indebted, lower-middle income country in West Africa with a population of 26 million people and an annual per capita income of US$ 1,760.18 Like other LMICs, the burden of injury is large.2 The age-standardized injury death rate is 58 per 100,000 persons, which is more than 20% higher than that in HICs.2 Most injured are brought to the hospital by commercial vehicles, often only after payment.19 Given long pre-hospital times and lack of care, 80% of trauma deaths occur in the pre-hospital setting.20 The injured that reach hospital care, particularly those injured in rural areas, almost uniformly encounter facilities without trained trauma teams or essential resources.3 District-level hospitals are usually the first point of healthcare contact for injured patients; the most senior clinician is usually a medical officer or a non-physician provider.21-23 Rarely are surgeons or physician anesthetists available.24 Nevertheless, many district-level hospitals offer some surgical services, namely cesarean section, and usually have between 50 – 100 beds.23 As examples of trauma care resource deficiencies, the majority of district-level hospitals in Ghana are unable to provide basic airway support, transfuse blood, take an X-ray or perform a trauma laparotomy for most patients in need, particularly during an emergency.7 Injuries that require more complex care have to be identified and referred to regional or tertiary hospitals, which face similar resource challenges.7 Referral often requires prohibitively expensive pre-payment that prevents transfer.25 Therefore, strengthening district-level trauma care may have greater than expected impact on the avertable death and disability from injury in Ghana given its importance in the ad hoc trauma care system.26
Delphi technique
We used the Delphi technique to develop consensus on a set of useful district-level hospital trauma care audit filters from panelists with relevant expertise. The Delphi technique is an iterative, anonymous, data-driven survey method that facilitates expert-group consensus building.27 The four defining characteristics of the Delphi technique are: i) anonymity; ii) iteration; iii) controlled feedback; and iv) statistical group response.28 These tenets were upheld throughout the study.
Panelist selection
To ensure that the final trauma care audit filters were both appropriate for the Ghanaian district-level hospital context and represented quality trauma care, we approached experts that met the following criteria: i) Ghanaian professionals or professionals that have significant experience with the Ghanaian healthcare system; and ii) expertise in an area relevant to the development of district-level hospital trauma care audit filters. Significant experience was defined as at least one year of work in a district-level hospital and/or currently overseeing trauma care at a district-level hospital(s). These areas included trauma care, clinical district-level hospital experience, anesthesia, nursing, hospital administration, and healthcare policy and evaluation (e.g. Ghana Health Service officials). Obstetricians have been collecting audit filters for maternal care in LMICs for many years;17 thus, an obstetrician with administrative experience was included. In total, 20 panelists who met the aforementioned criteria were approached. All approached panelists participated in the Delphi process (i.e. participation rate 100%). The breakdown of the participants’ primary area of expertise was as follows:
Trauma care – 6 panelists
District-level hospital care – 6 panelists
Anesthesia – 1 panelist
Nursing – 2 panelists
Healthcare administration – 2 panelists
Healthcare policy and evaluation – 2 panelists
Obstetric care – 1 panelist
Note that these represent only primary areas of expertise. Most panelists were able to provide expertise in more than one area (e.g. a surgeon who was also a healthcare administrator and teaches trauma care courses to district hospital staff).
Survey methods
Potential panelists were approached with an email that described the aims of the study, the Delphi technique and expected outputs. This was followed by a telephone communication to ensure the email was received. Potential panelists were asked to respond with a confirmatory email if they wanted to take part; all potential panelists responded. All communication was blinded; none of the panelists knew whom the other panelists were until consensus had been met to avoid social response bias.
For each round, responses to open-ended questions were examined using a content analysis framework.29 First, qualitative responses were grouped into categories based on codes that represented clustered responses. Then, categories were further refined into useful themes and described. Responses were triangulated between panelists to evaluate the extent of theme convergence. Particularly unique responses were also described and evaluated by panelists in the subsequent survey round.
In addition to open-ended questions, panelists were asked to rank proposed audit filters each round. Filters with a median rank <7 out of 10 were not included in subsequent rounds. Target consensus (i.e. terminating point for the Delphi technique) was defined a priori as: a median rank of ≥9 for each proposed audit filter on a scale from 0 to 10 and an average percent majority opinion (APMO) cut-off rate of ≥0.8. The APMO cut-off rate is a consensus measure that is calculated by subtracting agreements from disagreements and dividing the difference by all responses; agreement was defined as an audit filter rank of ≥7.28 As a sensitivity assessment, consensus was also measured using the coefficient of variance per round and per filter. By doing so, we could evaluate consensus between rounds without having to rely on our definition of agreement (i.e. rank ≥7). SurveyMonkey was used for data collection and Stata v12 (College Station, TX, USA) was used for data analysis.
Survey rounds
Round 1 consisted of three parts. Panelists were first asked to propose specific target processes to be measured by the audit filters, as well as important features of filters to be used in the district-hospital setting. Next, panelists were asked to rank a list of potential filters on a scale from 0 to 10 (0 was useless, 5 was somewhat useful and 10 was very useful). Lastly, panelists were asked to propose audit filters to be ranked during the next round.
The findings from Round 1 were presented in Round 2 so that each panelist could consider and evaluate process targets and important features of audit filters offered by other panelists. Panelists were given the opportunity to support, modify or reject each of the proposed process targets and important features. Next, filters with a median rank of ≥7 from the first round, as well as those proposed by the panelists in Round 1, were ranked/re-ranked. Then, open-ended questions regarding highly ranked filters (i.e. median rank ≥9) and low ranked filters (i.e. median rank <7) were asked to further understand components of both very useful and less useful filter features. Panelists were again given an opportunity to propose new filters for the next round.
Round 3 was designed to challenge successful filters. First, findings from the previous round were presented and an opportunity was given to support, modify or reject the findings. Second, highly ranked filters from previous rounds and newly proposed filters from Round 2 were grouped into each of the respective district-level hospital-based trauma care categories identified as essential targets by the panelists in Round 1 (e.g. triage, airway, breathing, circulation, disability, exposure/burn, identification of shock, early referral of patients in need of a higher-level of care, resuscitation, reassessment, outcome). Panelists then ranked the grouped filters side-by-side. By doing so, the most useful filter(s) in each trauma care category could be elicited. Additionally, open-ended questions followed each category of filters, which aimed to identify modifications that might improve the filters. Lastly, panelists were again given an opportunity to propose new filters for the next round.
In Round 4, all filters with median rank ≥7 in previous rounds and newly proposed filters from Round 3 were ranked/re-ranked within trauma care categories to force panelists to judge one against others that represented same process. Target consensus was reached after Round 4 (i.e. median rank of ≥9 for each proposed audit filter and an APMO cut-off rate of ≥0.8).
Results
Important processes to measure
Processes that emerged as important targets for monitoring and evaluation included: triage; components of the primary assessment; early identification of shock; early referral of patients in need of a higher-level of care or patients at high-risk for deterioration; resuscitation; reassessment; basic fracture management and a composite measure of care (Table 1).
Table 1.
Trauma care processes that panelists agreed should be monitored by basic and expanded audit filters with examples for district-level hospitals.
| Basic | Expanded | Example filter |
|---|---|---|
| Pre-hospital care | Patient arrived by National Ambulance Service | |
| Time since injury | Patient arrived within one hour of injury | |
| Triage | Vital signs are recorded within 15 minutes of patient arrival (must include breathing assessment, heart rate, blood pressure, oxygen saturation if available). | |
| Components of primary assessment | Examination for pneumo- or haemo-thorax was done within 15 minutes of patient arrival by listening to both sides of the chest with a stethoscope AND bilateral percussion. | |
| Identification of shock | If difficulty breathing, OR shock present at triage (HR >100, OR SBP <110)* OR oxygen saturation ≤95%, a senior provider (e.g. in-charge, medical officer) is made aware of the patient within 10 minutes. | |
| Identification of patients in need of referral | Referral activation is done within 15 minutes of detecting or suspecting: free abdominal fluid or haemoperitoneum with no ability to operate (should not delay resuscitation). | |
| Resuscitation | Advanced resuscitation | Basic: A large bore IV was placed within 15 minutes of patient arrival. Advanced: Two litters of fluid is given to adult patient (or 20cc/kg for a child) with low blood pressure or tachycardia (as determined by triage vitals). |
| Injury diagnostics | If ultrasound machine is present at the hospital, a FAST (focused assessment with sonography for trauma) scan was performed within 30 minutes of patient arrival. | |
| Re-assessment | A second head-to-toe physical exam is performed within 1 hour of primary assessment. | |
| Timely surgical intervention | Patient with free abdominal fluid or haemoperitoneum and shock has laparotomy within 2 hours. | |
| Life-threatening injury specific | If AVPU is V or P or U AND the patient is not in shock head of the bed is elevated to 45 degrees. | |
| Fracture management | Long bone fracture is reduced with analgesia and/or splinted within 2 hours of admission or prior to transfer. | |
| Comprehensive care | Time and date of referral, discharge or in-hospital death. | |
| Rehabilitation | Patient with a fracture is evaluated by physiotherapist prior to discharge. |
National Ambulance Service – Ghana has a national ambulance service that is growing to meet the demand for scene responses; HR – heart rate; SBP – systolic blood pressure
pediatric-specific vital signs representing shock should be available to practitioners and be applied when appropriate; IV – intravenous catheter; FAST – focused assessment with sonography for trauma; AVPU – a validated clinical neurological assessment endorsed by the World Health Organization: A is alert, V is responds to voice, P is responds to pain, and U is unresponsive; Proposed audit filters target essential trauma care processes for non-ambulatory patients and those triaged yellow, orange or red using the South African Triage Scale.[30]
For hospitals with more resources (i.e. advanced district hospitals, regional or tertiary hospitals) or an established trauma care system, an expanded set of audit filter target processes was agreed upon. These included pre-hospital care, advanced resuscitation, injury diagnostics, timely surgical intervention, life-threatening injury specific filters, and rehabilitation.
Important features of audit filters
Panelists agreed on a number of important features of audit filters for district-level hospitals. These included features related to their accuracy of process measurement, feasibility of data collection, applicability to the district-level hospital setting (i.e. acknowledging differential resource constrains between hospitals) and inclusiveness of facilities regardless of resources to aid comparison. Several particularly informative features are described (Table 2).
Table 2.
Important features of district-level hospital trauma care audit filters supported by panelists.
| Audit filters SHOULD... | Audit filters SHOULD NOT... |
|---|---|
| focus on assessment and early identification of patients that need immediate referral. | rely heavily on resources that may or may not be available to most patients at district-level hospitals (e.g. ability to intubate, perform X-ray or FAST scan, or operate). |
| measure early identification and treatment of shock. | include optional actions that do not have proven efficacy or that are not value-added (e.g. haemoglobin assessment) |
| be collected mostly during the assessment and resuscitation phase to avoid losses to follow-up once the patient is moved from the casualty ward. | inadvertently cause inexperienced staff to perform procedures that they are not trained to do (e.g. intubation, laparotomy), which could be more dangerous than early referral. |
| exist within the national framework for trauma and emergency care. | be a burden to collect. |
| be the same across hospitals for apposite comparison, but be expandable for hospitals with more resources or an established trauma care system. | be a comprehensive checklist of expectations for trauma care. |
| be useful for nurse, non-physician providers, medical officers and surgeons alike. | reflect a patient's ability to pay for advanced services. |
| consider the differences in rural versus urban case mix (i.e. rural cases tend to be less severe given most die in the pre-hospital setting; urban cases more often present with severe injuries but alive). | incorporate the time it takes to get a patient transferred, such as proximity of a vehicle or hospital, gathering payment, etc., but instead reflect timely referral process activation for a patient in need of a higher level of care. |
| stress early communication between referring and receiving facilities. | rely on technology, which might be broken or insufficient in number at a hospital. |
| stress the importance of physical exam and serial assessment. | detract resources from other patients who might require similar attention (e.g. obstetric emergencies, pediatric sepsis, etc.) |
| be used for all patients, save those who are minimal risk, low-acuity or require minimal treatment (e.g. isolated sport-related injury, simple laceration). | neglect the importance of timing; however, they must consider hospitals with large case-loads and few human resources to manage all the patients. |
| be tied into a pre-existing referral activation process. | be collected on low-acuity patients. |
| focus on common situations, not more rare but serious ones (e.g. electrical injury, urethral injury). | incorporate more than one step if possible, which might make data collection more difficult if done by a non-clinician. |
| reflect internationally accepted standards for triage, assessment, and resuscitation in the district-hospital context (e.g. Primary Trauma Care). | underestimate district-hospital capabilities; filters should set the bar slightly above current care but attainable with quality improvement processes, even with the current level of resources. |
| be proxies of quality care, not checklists. | be pediatric or adult specific, but universal. |
| consider late presentations, particularly for burn injury. | require longitudinal data collection (e.g. following urine output) |
| include basic data in order to track injury epidemiology and risk-stratify patients for future initiatives. | use GCS; AVPU should be used instead given its simplicity. |
| include user-friendly data collection forms for non-clinicians. | expect that X-ray or ultrasound exams would be done at bedside. |
FAST – focused assessment with sonography for trauma; GCS – Glasgow coma scale; AVPU – a validated clinical neurological assessment endorsed by the World Health Organization: A is alert, V is responds to voice, P is responds to pain, and U is unresponsive. Proposed audit filters target essential trauma care processes for non-ambulatory patients and those triaged yellow, orange or red using the South African Triage Scale.[30]
Among features most stressed by panelists were simplicity and feasibility, both with regards to the actions expected and data collection mechanism itself. For example, panelists discouraged the use of compound filters (i.e. if ‘x,’ then ‘y’ was done) or filters that assumed a higher-than-average level of resources (e.g. functioning X-ray, focused assessment with sonography for trauma [FAST] scan training, ability to intubate or operate). Panelists also agreed that the primary aim for trauma care at hospitals without surgical care capacity is to quickly identify and refer patients who are in need of more advanced treatment or at high-risk of deterioration. Therefore, filters that required significant longitudinal data collection (e.g. monitoring of urine output, details of post-resuscitation or post-operative care), while important, were not prioritized. It was also agreed that filters should be useful for comparing all district-level hospitals; however, those with greater resources or an established trauma care system should be able and encouraged to collect a greater number of and/or more advanced filters at their discretion.
Other considerations for audit filters were agreed upon. For example, trauma care audit filters SHOULD:
align with national trauma care guidelines, as well as internationally accepted standards for trauma care;
be useful for all potential district-hospital providers (e.g. nurses, non-physician providers, medical officers);
rely on physical exam and serial assessment rather than diagnostic studies that may or may not be available (e.g. X-ray, lactate determination); and
be proxies of quality trauma care, not comprehensive checklists.
Additionally, panelists agreed that trauma care audit filters SHOULD NOT:
require data to be collected on low-risk or low-acuity patients to streamline the care process (e.g. ambulatory patients, those triaged green using the South African Triage Scale);30
inadvertently cause inexperienced staff to perform procedures beyond their scope of practice in an effort to increase the hospital's audit score, which might be more dangerous than early referral (e.g. difficult intubation, trauma laparotomy);
be linked to a patient's ability or inability to pay;
neglect the importance of timing and effective triage, but appreciate the large case-loads and insufficient number of staff to manage all of the patients rapidly; and
underestimate district-level hospital capabilities by setting the bar too low; instead, the bar should be set slightly higher than the current situation but attainable with low-cost quality improvement measures.
Building consensus
In addition to the open-ended questions regarding the target trauma care processes and important features of audit filters at district-level hospitals, specific filters were proposed and ranked in each round. Consensus was measured by APMO cut-off rate with agreement set at rank ≥7 on a scale from 0 – 10, as well as the coefficient of variance.
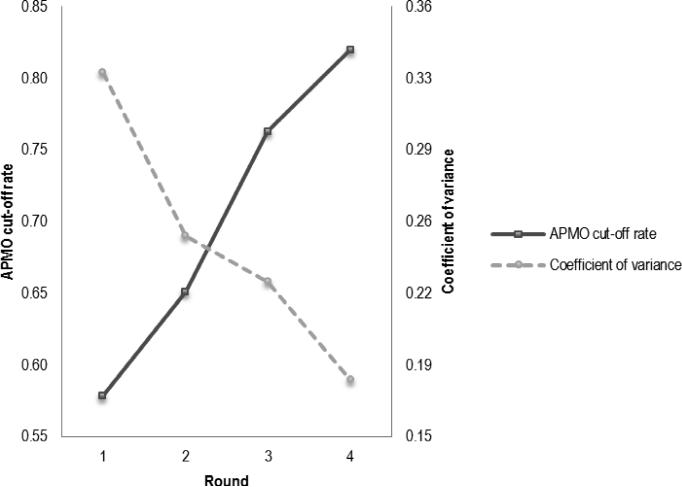
APMO cut-off rate increased consistently from one round to the next, which demonstrates consensus building: Round 1 - 0.58; Round 2 - 0.66; Round 3 - 0.76; and Round 4 - 0.82 (Figure 1). Given that all audit filters in Round 4 had a median rank of ≥9 and the APMO cut-off rate was ≥0.80, the process was terminated (i.e. target consensus was reached). The sensitivity analysis using coefficient of variance did not depend on a specified level of agreement (i.e. rank ≥7). Supporting the finding of consensus using APMI cut-off rate, the coefficient of variance decreased in consecutive rounds from 0.33 in Round 1 to 0.18 in Round 4. These values of both metrics across successive rounds demonstrated improving and strong consensus among panelists.
Figure 1.
Average percent of majority opinion (APMO) cut-off rate and coefficient of variance for each round using the Delphi technique.
APMO – average percent of majority opinion; Panelist agreement with the audit filter was defined as a median rank of 7 or above. An APMO cut-off rate of 0.80 was selected as a Delphi end-point a priori.
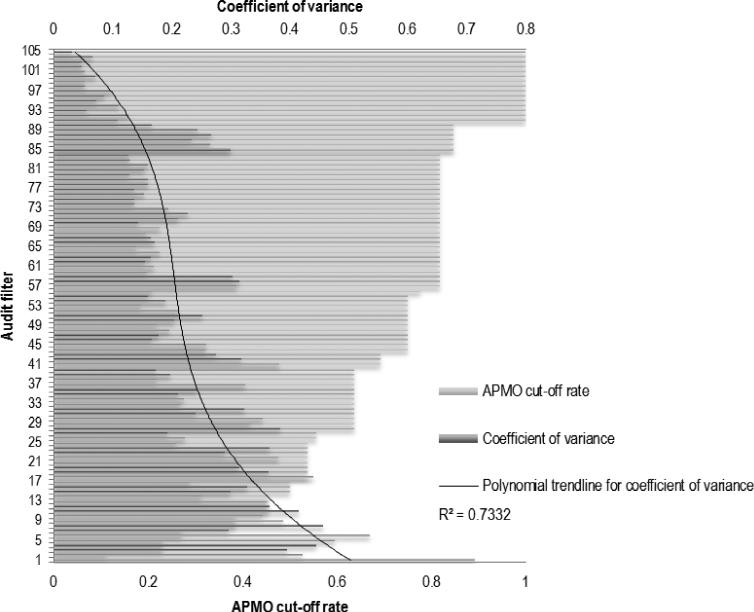
Consensus was also examined per filter, opposed to per round as above. In Figure 2, ranked filters are consecutively numbered from 1 to 105. The APMO cut-off rate increased steadily across filters. Consensus within successive filters is demonstrated by the 3rd degree polynomial trendline for coefficient of variance in the same figure (R2=0.73).
Figure 2.
Average percent of majority opinion (APMO) cut-off rate and coefficient of variance for each audit filter proposed using the Delphi technique.
APMO – average percent of majority opinion; Panelist agreement with the audit filter was defined as a median rank of 7 or above. An APMO cut-off rate of 0.80 was selected as a Delphi end-point a priori; Numbers on the y-axis represent consecutively rated audit filters; The 3rd degree polynomial trendline for coefficient of variance was selected based on best fit (R2=0.73).
Audit filters
There were 22 trauma care audit filters agreed upon by the panelists after Round 4; 13 of these are for triage, primary trauma assessment and outcome and 9 are specific to the referral process. The list of audit filters that achieved consensus and the target process of care that they represent are given in Tables 3 and 4. For each of the district-level hospital trauma care processes, there are one or two representative filters. When there are two filters, the first was meant to be more basic or assessment-centered and the second slightly more advanced and action-centered. For example, for evaluation of breathing during the primary assessment, panelists agreed on two filters: i) examination for pneumo- or haemo-thorax was done within 15 minutes of patient arrival by listening to both sides of the chest with a stethoscope AND bilateral percussion; and ii) if pneumo-or haemo-thorax is suspected or confirmed AND oxygen saturation was less than 98%, a chest tube was placed within 30 minutes of patient arrival. Other examples of audit filters that achieved consensus include:
If difficulty breathing, OR shock present at triage (HR >100, OR SBP <110)* OR oxygen saturation ≤95%, a senior provider (e.g. in-charge, medical officer) is made aware of the patient immediately.
A large bore IV was placed within 15 minutes of patient arrival.
Long bone fracture is reduced with analgesia and/or splinted within 2 hours of admission or prior to transfer.
The fluid order for a burn patient using the Parkland formula is recorded within 1 hour for burns over 15% total body surface area that occurred less than 24 hours from patient arrival.
Table 3.
District-level hospital trauma care audit filters with panelist consensus using the Delphi technique.
| Target process | Proposed audit filter |
|---|---|
| Triage | 1.Vital signs are recorded within 15 minutes of arrival (must include breathing assessment, heart rate, blood pressure, oxygen saturation if available). 2.If difficulty breathing, OR shock present at triage (HR >100, OR SBP <110)* OR oxygen saturation ≤95%, a senior provider (e.g. in-charge, medical officer) is made aware of the patient immediately. |
| Airway | 1.The clinician asked the patient a question and listened for a response to assess airway patency. 2.Patient with difficulty or obstructed breathing received basic airway maneuver assistance (i.e. sweep, chin-lift-jaw-thrust, oral or nasal airway, suction). |
| Breathing | 1.Examination for pneumo- or haemo-thorax was done within 15 minutes of patient arrival by listening to both sides of the chest with a stethoscope AND bilateral percussion. 2.If pneumo- or haemo-thorax is suspected OR confirmed AND oxygen saturation was less than 98%, a chest tube was placed within 30 minutes of patient arrival. |
| Circulation | 1.A large bore IV was placed within 15 minutes of patient arrival. 2.If there is external bleeding at patient arrival, pressure is applied and maintained until definitive control is performed. |
| Disability | 1.If AVPU is not ‘A’ AND the patient is not in shock, the head of the bed is elevated to 45 degrees. 2.Long bone fracture is reduced with analgesia and/or splinted within 2 hours of admission or prior to transfer. |
| Exposure | 1.Patient is completely undressed, fully examined and covered for privacy within 30 minutes of arrival. 2.The fluid order for a burn patient using the Parkland formula is recorded within 1 hour for burns over 15% total body surface area that occurred less than 24 hours from patient arrival. |
| Outcome | • Date and time and hospital discharge, referral or death. |
HR – heart rate; SBP – systolic blood pressure
pediatric-specific vital signs representing shock should be available to practitioners and be applied when appropriate; IV – intravenous catheter; AVPU – a validated clinical neurological assessment endorsed by the World Health Organization: A is alert, V is responds to voice, P is responds to pain, and U is unresponsive. Proposed audit filters target essential trauma care processes for non-ambulatory patients and those triaged yellow, orange or red using the South African Triage Scale.[30]
Table 4.
District-level hospital trauma care audit filters for referral with panelist consensus using the Delphi technique.
| Target process | Referral activation is done within 15 minutes of detecting/suspecting: |
|---|---|
| Airway | • need for intubation (should not delay intubation if able). |
| Breathing | 1.chest tube needing to be placed (should not prevent a chest tube from being placed if able). 2.oxygen saturation <92% at any two immediately consecutive checks (should not delay oxygen supplementation, airway assessment or looking for haemo- or pneumo-thorax). |
| Circulation | 1.free abdominal fluid or haemoperitoneum with no ability to operate (should not delay resuscitation). 2.pelvic fracture OR two long bone fractures by clinical exam or X-ray (should proceed with reduction and stabilization/splinting as able). 3.any penetrating injury to the neck, thorax, back or abdomen and no ability to operate. |
| Disability | • abnormal neurological exam on two checks 30 minutes apart (should not delay neuro-protection steps). |
| Exposure | • partial thickness burn >15%; circumferential burn; any burn over face, hand, genitals, joint; inhalation injury (resuscitation should proceed as required by history and burn). |
| Communication | • If referral is activated, the referring clinician and receiving facility communicate by phone or radio prior to transfer. |
Proposed audit filters target essential trauma care processes for non-ambulatory patients and those triaged yellow, orange or red using the South African Triage Scale.[30]
Given the importance of early identification of a patient in need of referral from a district-level hospital, panelists proposed and developed consensus on 9 audit filters that reflect quality referral practices. Panelists suggested and agreed that district-level hospitals should have a ‘referral activation plan.’ This would entail having a pre-designated person(s) quickly make standardized arrangements for transfer to a facility that can provide a higher level of care. Therefore, the clinician taking care of an injured patient can focus his or her attention on the patient without simultaneously trying to coordinate transfer. All of the referral practice audit filters expect that the referral plan would be activated within 15 minutes of identifying specific injuries or care needs. For example, referral activation is done within 15 minutes of detecting or suspecting: need for intubation (should not delay intubation if able); or an abnormal neurological exam on two checks 30 minutes apart (should not delay neuroprotection steps if able). In addition, communication was considered to be particularly important by the panelists. Therefore, a representative audit filter was agreed upon: if referral is activated, the referring clinician and receiving facility communicate by phone or radio prior to transfer.
Discussion
This study used the Delphi technique to develop trauma care audit filters that would be accurate proxies of quality trauma care, simple to measure and feasible to collect at district-level hospitals in Ghana. After four iterative rounds of open-ended questions, controlled feedback, and filter ranking, 22 filters were agreed upon. The proposed filters aim to measure quality triage, trauma assessment, referral practices and outcomes. These filters represent an important step toward routine, prospective monitoring and evaluation of the trauma care process and/or quality improvement initiatives at first-level hospitals in Ghana, as well as LMICs more broadly.
While trauma care audit filters have been used for a long time to monitor and evaluate care processes at trauma centers and systems in HICs, they have not been used widely in LMICs.14 Examples of LMIC trauma care audit filter use are namely from larger hospitals in urban centres and/or require resources typically absent at district-level hospitals (e.g. a patient with a Glasgow Coma Scale <13 receives a head computed tomography scan within 2 hours of arrival; a patient with an abdominal injury and hypotension receives a laparotomy within 1 hour of arrival).4, 5, 7 A study of trauma quality improvement programs in Asian-Pacific LMICs that included representatives from China, India, Malaysia, Philippines, Sri Lanka, Thailand, and Vietnam reported that no rural hospitals in these countries used audit filters to monitor and evaluate processes of trauma care.4 Among the reasons for the lack of audit filter use at small hospitals proposed by the authors included a lack of standardized data collection mechanisms, limited resources (i.e. human and physical) and insufficient engagement by local healthcare leaders.4 Defining standard, context-appropriate audit filters and obtaining the support of local healthcare leadership are important initial steps to improving trauma care in Ghana, as well as in other LMICs.
Opportunely, obstetric care audit has been performed with success in LMICs.31 Obstetric audit filters have ranged from composite measurements of quality care (e.g. obstetric case fatality rate, caesarean section rate, proportion of pregnant women receiving antenatal services) to more granular filters that evaluate specific processes of care.17 Examples of audit filters used for assessing care for obstetric haemorrhage at district-level hospitals include: IV line was established; blood type and cross-match was performed; and oxytocics given and genital tract explored in cases of continuing post-partum haemorrhage.17 The filters proposed by this study are similar; thus, important lessons for clinical audit of trauma care can be learned from previous development and implementation of audit filters for obstetric care in LMICs.
There are several examples of obstetric clinical audit from LMICs that are particularly useful. In Sierra Leone, obstetric filters were used to evaluate the effectiveness of a capacity improvement package at a district-level hospital that was in need of significant support.31 The package consisted of two trained physicians with obstetric skills, courses in emergency obstetric care for nurses and midwives, refurbishment of an unused operating theatre, and installation of a generator and blood bank. The hospital tracked the number of obstetric emergencies, obstetric case fatality rate and proportion of abortion-related procedures. The case-fatality rate decreased from 32% to 5% in 5 years despite a tripling in patient volume. However, the ability to identify breakdowns in specific processes of care was not possible; more granular filters were required. Four district-hospitals in Ghana and Jamaica successfully tracked 31 filters that reflected detailed processes of emergency obstetric care (e.g. delivery of the fetus within 2 hours of identifying obstructed labor, select lab investigations performed for a woman with severe pre-eclampsia, broad-spectrum antibiotics including metronidazole given for a woman with genital tract sepsis).32 Filters were tracked for one year with regular feedback given to hospitals regarding the proportion of successfully completed filters and specific processes that needed improvement. Clinical audit and feedback were able to significantly improve obstetric care (e.g. increase in the proportion of women with obstetric haemorrhage who underwent blood typing and crossmatch – 49 to 74%; proportion of women treated with antibiotics for genital tract sepsis – 65 to 93%). These examples from obstetrics demonstrate that clinical audit of trauma care at the district-level hospital is feasible and might allow useful evaluation of the quality of care provided.
District-level hospital referral is an important component of healthcare systems in LMICs.25, 33 Given the global and level-specific lack of resources, almost all patients with one or more serious injury that arrive at district-level hospitals must be transferred.3 Expectedly, early identification of patients in need of referral, brisk resuscitation and effective inter-facility communication can prevent death and disability.8, 34, 35 Therefore, auditing the district-level hospital referral process might be as important as auditing trauma care itself. In Malawi, a referral audit process resulted in significantly improved outcomes for obstetric emergencies.36 Using audit feedback alone, health facilities were able to improve upon two filters in only three months: i) proportion of adequately resuscitated patients prior to referral; and ii) delay of less than two hours from referral activation to arrival at receiving facility. Other filters were audited, but had high compliance at both the initial and repeat assessment, including: i) all patients referred with referral form; and ii) short-wave radio communication regarding referral. With the clinical audit examples above and this successful referral audit, the potential utility of audit filters that span the district-hospital trauma care continuum becomes evident.
The way forward regarding the use of these audit filters will require pilot study prior to their implementation. Using feedback from the pilot, the filters might be made user-friendlier and more accurate proxies of trauma care. Subsequently, the number of hospitals taking part would need to be increased, data reported centrally and audit results compared with known levels of quality care to ensure the filters’ validity. Should the filters be proven useful, hospital performance should be serially or continuously monitored and evaluated and timely feedback given so that care can be improved.5 All hospitals in Ghana use a demographic and health information management system (DHIMS-II) to routinely collect and report data to the Ministry of Health.37 The majority of the indicators used in this system are not granular and none reflect trauma care. To align with DHIMS-II or other national reporting schemes, the proposed filters could be captured on checklist forms and consolidated into a composite metric (e.g. the proportion of successfully performed audit filters per injured person) or into a few filters that are highly correlated with the successful completion of the others. By doing so, trauma care audit filters could be more feasibly collected and included into national healthcare data reporting platforms. Then, quality improvement targets could be identified and strategic interventions evaluated at both the hospital and national levels.
Although this study used a rigorously preformed Delphi technique, there are several limitations that should be considered. First, the filters were developed for the Ghanaian context. However, the human and physical resource limitations known to the panelists are not unique to Ghana.3 Therefore, these filters are likely generalizable to many other LMIC hospitals, particularly those in sub-Saharan Africa. Given widespread resource deficiencies, the proposed filters might also be useful for primary health centres, and referral and tertiary hospitals in LMICs.38, 39 Second, while the filters were designed to serve as proxies for quality trauma care at the district-level hospital, they may not represent meaningful clinical or patient-centered outcomes.40 Piloting of these filters in parallel with routine collection of detailed injury outcome data or from hospitals with known levels of quality will be required for validation. Next, in higher functioning hospitals and as trauma care improves at district-level hospitals, these filters might become too simple to reflect opportunities for quality improvement. Serial revision of the audit filters to maintain contextual appropriateness should be considered. Additionally, as hospitals become more compliant with trauma care standards, the filters’ effectiveness as quality improvement tools might decrease.41 Lastly, these filters are meant to supplement, not replace, other effective and less complex methods of trauma care quality monitoring, such as use of routine morbidity and mortality conferences and multidisciplinary preventable death reviews.5, 10 Despite these limitations, this study has developed potentially useful trauma care audit filters for low-resourced hospitals in Ghana, as well as other LMICs that face similar resource limitations.
Conclusions
This study proposes 22 audit filters that are meant to reflect quality district-level hospital trauma care and referral practices. Quality improvement programs using these filters might allow hospitals and health care systems to monitor and evaluate hospital-based trauma care. While examples of trauma care audit filters used at district-level hospitals in LMICs are rare, similar filters to the those proposed here have been used extensively by the obstetrics field for benchmarking healthcare facilities and as indicators for quality improvement interventions in LMICs. Given the proven utility of clinical audit to improve care quality in HICs, addition of prospective trauma care audit at district-level hospitals is an important step toward improving care for the injured in LMICs.
Acknowledgments
Grant support: This study was funded by grants (R25TW009345; D43-TW007267) from the Fogarty International Center, US National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: No real or potential conflicts to disclose.
Contributor Information
Barclay T Stewart, Department of Surgery, University of Washington, Seattle, WA, USA; School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana; Department of Surgery, Komfo Anokye Teaching Hospital, Kumasi, Ghana.
Adam Gyedu, Department of Surgery, Komfo Anokye Teaching Hospital, Kumasi, Ghana; School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana.
Robert Quansah, Department of Surgery, Komfo Anokye Teaching Hospital, Kumasi, Ghana; School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana.
Wilfred Larbi Addo, Eastern Regional Health Directorate, Ghana Health Service, Koforidua, Ghana.
Akis Afoko, Department of Surgery, Tamale Teaching Hospital, Tamale, Ghana.
Pius Agbenorku, Department of Surgery, Komfo Anokye Teaching Hospital, Kumasi, Ghana; School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana.
Forster Amponsah-Manu, Department of Surgery, Eastern Regional Hospital, Koforidua, Ghana.
James Ankomah, Department of Surgery, Komfo Anokye Teaching Hospital, Kumasi, Ghana.
Ebenezer Appiah-Denkyira, Ghana Health Service, Accra, Ghana.
Peter Baffoe, Department of Obstetrics and Gynecology, Upper East Regional Hospital, Bolgatanga, Ghana.
Sam Debrah, Department of Surgery, University of Cape Coast, Cape Coast, Ghana.
Peter Donkor, Department of Surgery, Komfo Anokye Teaching Hospital, Kumasi, Ghana; School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana.
Theodor Dorvlo, Department of Surgery, Eastern Regional Hospital, Koforidua, Ghana.
Kennedy Japiong, Department of Emergency Medicine, Police Hospital, Accra, Ghana.
Adam L Kushner, Surgeons OverSeas (SOS), New York, NY, USA; Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA; Department of Surgery, Columbia University, New York, NY, USA.
Martin Morna, Department of Surgery, University of Cape Coast, Cape Coast, Ghana.
Anthony Ofosu, Ghana Health Service, Accra, Ghana.
Victor Oppong-Nketia, Department of Anesthesia, Komfo Anokye Teaching Hospital, Kumasi, Ghana.
Stephen Tabiri, Department of Surgery, Tamale Teaching Hospital, Tamale, Ghana; Department of Surgery, University of Development Studies, Tamale, Ghana.
Charles Mock, Harborview Injury Prevention & Research Center, Seattle, WA, USA; Department of Surgery, University of Washington, Seattle, WA, USA; Department of Global Health, University of Washington, Seattle, WA, USA.
References
- 1.GBD_Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Data VisualizationsGlobal Burden of Disease Cause Patterns. Institute of Health Metrics and Evaluation; Seattle, WA: 2013. [Google Scholar]
- 3.Wong EG, Gupta S, Deckelbaum DL, Razek T, Kushner AL. Prioritizing injury care: a review of trauma capacity in low and middle-income countries. Journal of Surgical Research. 2014 doi: 10.1016/j.jss.2014.08.055. [DOI] [PubMed] [Google Scholar]
- 4.Stelfox HT, Joshipura M, Chadbunchachai W, Ellawala RN, O'Reilly G, Nguyen TS, et al. Trauma quality improvement in low and middle income countries of the Asia-Pacific region: a mixed methods study. World journal of surgery. 2012;36:1978–1992. doi: 10.1007/s00268-012-1593-1. [DOI] [PubMed] [Google Scholar]
- 5.Mock C, Julliard C, Brundage S, Goosen J, Joshipura M. Guidelines for trauma quality improvement programmes. World Health Organization; Geneva: 2009. [Google Scholar]
- 6.Peabody JW, Taguiwalo MM, Robalino DA, Frenk J. Disease Control Priorities in Developing Countries. 2nd edition. The International Bank for Reconstruction and Development/The World Bank Group; Washington, D.C.: 2006. [PubMed] [Google Scholar]
- 7.Stewart B, Quansah R, Gyedu A, Ankomah J, Donkor P, Mock C. Strategic assessment of trauma care technology availability in Ghana. World journal of surgery. 2014 doi: 10.1007/s00268-015-3132-3. In press. [DOI] [PubMed] [Google Scholar]
- 8.Mock C, Abantanga F, Goosen J, Joshipura M, Juillard C. Strengthening care of injured children globally. Bulletin of the World Health Organization. 2009;87:382–389. doi: 10.2471/BLT.08.057059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Costa CDdS. Scarpelini S Evaluation of the quality of trauma care service through the study of deaths in a tertiary hospital. Rev. Col. Bras. Cir. 2012;39:249–254. doi: 10.1590/s0100-69912012000400002. [DOI] [PubMed] [Google Scholar]
- 10.Yeboah D, Mock C, Karikari P, Agyei-Baffour P, Donkor P, Ebel B. Minimizing preventable trauma deaths in a limited-resource setting: a test-case of a multidisciplinary panel review approach at the Komfo Anokye Teaching Hospital in Ghana. World journal of surgery. 2014;38:1707–1712. doi: 10.1007/s00268-014-2452-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zafarghandi MR, Modaghegh MH, Roudsari BS. Preventable trauma death in Tehran: an estimate of trauma care quality in teaching hospitals. The Journal of trauma. 2003;55:459–465. doi: 10.1097/01.TA.0000027132.39340.FE. [DOI] [PubMed] [Google Scholar]
- 12.Jat AA, Khan MR, Zafar H, Raja AJ, Hoda Q, Rehmani R, et al. Peer review audit of trauma deaths in a developing country. Asian journal of surgery / Asian Surgical Association. 2004;27:58–64. doi: 10.1016/s1015-9584(09)60247-5. [DOI] [PubMed] [Google Scholar]
- 13.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. The New England journal of medicine. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 14.Evans C, Howes D, Pickett W, Dagnone L. Audit filters for improving processes of care and clinical outcomes in trauma systems. The Cochrane database of systematic reviews. 2009:CD007590. doi: 10.1002/14651858.CD007590.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glance LG, Dick AW, Mukamel DB, Osler TM. Association between trauma quality indicators and outcomes for injured patients. Archives of surgery. 2012;147:308–315. doi: 10.1001/archsurg.2011.1327. [DOI] [PubMed] [Google Scholar]
- 16.Copes WS, Staz CF, Konvolinka CW, Sacco WJ. American College of Surgeons audit filters: associations with patient outcome and resource utilization. The Journal of trauma. 1995;38:432–438. doi: 10.1097/00005373-199503000-00027. [DOI] [PubMed] [Google Scholar]
- 17.Graham W, Wagaarachchi P, Penney G, McCaw-Binns A, Antwi KY, Hall MH. Criteria for clinical audit of the quality of hospital-based obstetric care in developing countries. Bulletin of the World Health Organization. 2000;78:614–620. [PMC free article] [PubMed] [Google Scholar]
- 18.CIA World Factbook . United States Central Intellegence Agency; Ghana, Washington, D.C.: 2014. [Google Scholar]
- 19.Tiska MA, Adu-Ampofo M, Boakye G, Tuuli L, Mock CN. A model of prehospital trauma training for lay persons devised in Africa. Emergency medicine journal : EMJ. 2004;21:237–239. doi: 10.1136/emj.2002.002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mock C, Jurkovich G, nii-Amon-Kotei D. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. Journal of Trauma. 1998;44:804–814. doi: 10.1097/00005373-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Fulton BD, Scheffler RM, Sparkes SP, Auh EY, Vujicic M, Soucat A. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Human resources for health. 2011;9:1. doi: 10.1186/1478-4491-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ologunde R, Vogel JP, Cherian MN, Sbaiti M, Merialdi M, Yeats J. Assessment of cesarean delivery availability in 26 low- and middle-income countries: a cross-sectional study. American journal of obstetrics and gynecology. 2014 doi: 10.1016/j.ajog.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 23.Choo S, Perry H, Hesse AA, Abantanga F, Sory E, Osen H, et al. Assessment of capacity for surgery, obstetrics and anaesthesia in 17 Ghanaian hospitals using a WHO assessment tool. Tropical medicine & international health : TM & IH. 2010;15:1109–1115. doi: 10.1111/j.1365-3156.2010.02589.x. [DOI] [PubMed] [Google Scholar]
- 24.Choo S, Perry H, Hesse AA, Abantanga F, Sory E, Osen H, et al. Surgical training and experience of medical officers in Ghana's district hospitals. Academic medicine : journal of the Association of American Medical Colleges. 2011;86:529–533. doi: 10.1097/ACM.0b013e31820dc471. [DOI] [PubMed] [Google Scholar]
- 25.Gyedu A, Baah EG, Boakye G, Ohene-Yeboah M, Otupiri E, Stewart BT. Quality of referrals for elective surgery at a tertiary care hospital in a developing country: An opportunity for improving timely access to and cost-effectiveness of surgical care. International journal of surgery. 2015;15C:74–78. doi: 10.1016/j.ijsu.2015.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chokotho L, Mulwafu W, Jacobsen KH, Pandit H, Lavy C. The burden of trauma in four rural district hospitals in Malawi: a retrospective review of medical records. Injury. 2014;45:2065–2070. doi: 10.1016/j.injury.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 27.Hsu C-C, Sandford BA. The Delphi Technique: Making Sense Of Consensus Practical Assessment. Research and Evaluation. 2007;12 [Google Scholar]
- 28.Gracht HAvd. Consensus measurement in Delphi studies: Review and implications for future quality assurance. Technological Forecasting & Social Change. 2012;79:1525–1536. [Google Scholar]
- 29.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health services research. 2007;42:1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gottschalk SB, Wood D, DeVries S, Wallis LA, Bruijns S, Cape Triage G. The Cape Triage Score: a new triage system South Africa. Proposal from the Cape Triage Group. Emergency medicine journal : EMJ. 2006;23:149–153. doi: 10.1136/emj.2005.028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leigh B, Kandeh HB, Kanu MS, Kuteh M, Palmer IS, Daoh KS, et al. Improving emergency obstetric care at a district hospital, Makeni, Sierra Leone: The Freetown/Makeni PMM Team. Internatioanl Journal of Gynaecology and Obstetrics. 1997;59(Suppl 2):S55–65. doi: 10.1016/s0020-7292(97)00148-3. [DOI] [PubMed] [Google Scholar]
- 32.Wagaarachchi PT, Graham WJ, Penney GC, McCaw-Binns A, Yeboah Antwi K, Hall MH. Holding up a mirror: changing obstetric practice through criterion-based clinical audit in developing countries. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2001;74:119–130. doi: 10.1016/s0020-7292(01)00427-1. discussion 131. [DOI] [PubMed] [Google Scholar]
- 33.Mock CN, Donkor P, Gawande A, Jamison DT, Kruk ME, Debas HT. Essential surgery: key messages from Disease Control Priorities. The Lancet. (3rd edition) 2015 doi: 10.1016/S0140-6736(15)60091-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wisborg T, Montshiwa TR, Mock C. Trauma research in low- and middle-income countries is urgently needed to strengthen the chain of survival. Scandinavian journal of trauma, resuscitation and emergency medicine. 2011;19:62. doi: 10.1186/1757-7241-19-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sa'avu M, Duke T, Matai S. Improving paediatric and neonatal care in rural district hospitals in the highlands of Papua New Guinea: a quality improvement approach. Paediatrics and international child health. 2014;34:75–83. doi: 10.1179/2046905513Y.0000000081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kongnyuy EJ, Mlava G, van den Broek N. Criteria-based audit to improve a district referral system in Malawi: a pilot study. BMC health services research. 2008;8:190. doi: 10.1186/1472-6963-8-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kayode GA, Amoakoh-Coleman M, Brown-Davies C, Grobbee DE, Agyepong IA, Ansah E, et al. Quantifying the validity of routine neonatal healthcare data in the Greater Accra Region. Ghana PloS one. 2014;9:e104053. doi: 10.1371/journal.pone.0104053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stewart BT, Quansah R, Gyedu A, Ankomah J, Donkor P, Mock C. Strategic Assessment of Trauma Care Capacity in Ghana World journal of surgery. 2015 doi: 10.1007/s00268-015-3132-3. [DOI] [PubMed] [Google Scholar]
- 39.Carlson LC, Lin JA, Ameh EA, Mulwafu W, Donkor P, Derbew M, et al. Moving from Data Collection to Application: A Systematic Literature Review of Surgical Capacity Assessments and their Applications. World journal of surgery. 2015;39:813–821. doi: 10.1007/s00268-014-2938-8. [DOI] [PubMed] [Google Scholar]
- 40.Willis CD, Gabbe BJ, Cameron PA. Measuring quality in trauma care. Injury. 2007;38:527–537. doi: 10.1016/j.injury.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 41.Jamtvedt G, Young JM, Kristoffersen DT, O'Brien MA, Oxman AD. Does telling people what they have been doing change what they do? A systematic review of the effects of audit and feedback Quality & safety in health care. 2006;15:433–436. doi: 10.1136/qshc.2006.018549. [DOI] [PMC free article] [PubMed] [Google Scholar]