Abstract
Background
Current literature provides conflicting data regarding seasonal variability in dietary intake.
Objective
To examine seasonal variation in dietary intake in healthy adults from the metropolitan Washington, DC area.
Design
This study utilized an observational cohort design.
Participants/setting
Male and female healthy volunteers (n=103) between the ages of 18–75 years were recruited from the metropolitan Washington, DC area to participate in a clinical study at the National Institutes of Health Clinical Center from February 2011 to June 2014.
Main outcome measures
Three to seven day food records were collected from subjects (n=76) at three time points (12–15 weeks apart). Subjects were excluded from analysis (n=27) if they completed less than three time points. Food records were reviewed by nutrition staff, assigned to a season and coded in Nutrient Data System for Research for energy, macronutrient, micronutrient and food group serving analysis.
Statistical Analyses
Multivariate general linear models were run on energy, macronutrient, micronutrient, and food group intakes while being adjusted for age, sex, race, and BMI.
Results
Subjects had an average BMI of 25 ± 3.9 kg/m2 (mean ± SD) and average age of 34 ± 12.4 years. Subject demographics were 71.1% White, 9.2% Black/African American, 13.2% Asian, and 6.6% unknown race with 44.7% males and 55.3% females. Mean intake of energy across seasons was 2214.6 ± 623.4 kcal with 17.3 ± 4.1%, 33.6 ± 5.5%, 46.6 ± 8.0%, and 2.7 ± 3.2% of calories from protein, fat, carbohydrate, and alcohol, respectively. Intakes of energy, macronutrients, micronutrients, and food groups did not differ between seasons.
Conclusions
People living in the metropolitan Washington, DC area did not exhibit seasonal variation in dietary intake. Therefore, when designing studies of nutrient intake in a metropolitan population, these findings suggest that investigators do not need to consider the season during which diet is examined.
Five keywords or descriptive phrases: seasonal variation in dietary intake, healthy adults, macronutrients, micronutrients, food groups
Introduction
A variety of methods are used to assess human dietary intake, including 24-hour recalls, food records, food frequency questionnaires (FFQs), and biomarkers.1 Previous studies cite intraindividual variation as the main barrier in obtaining representative dietary intake data from each of these collection methods.1 Factors that influence within-subject variation include day to day, weekday to weekend and, relevant to this study, season to season variation.1 The possibility of seasonal variation in dietary intake raises concerns regarding the accuracy of intake data in studies spanning multiple seasons. Similarly, if seasonality exists in dietary intake, researchers would incorporate seasonal bias when generalizing their results across all seasons if data were collected only in a single season. In many regions of the world, it is well-established that dietary patterns change with the seasons related to cyclical availability of food.2 However, there are limited data examining the seasonality of dietary intake in developed countries where it is believed that there is a more limited effect of season on access to food.
Current literature is inconsistent regarding seasonal variation of energy, macronutrient, and micronutrient intakes in industrialized regions. For example, in adults living in the United States, increases in overall energy intake were seen in the fall,3 while in a sample of young, Spanish adults, greatest energy intake occurred in the winter.4 Many investigators have reported seasonal changes in macronutrient intakes, even after adjusting for any seasonal changes in total energy intake.2, 4–6 Seasonal differences in fat and protein intake have been described,2, 4–9 but seasonality of carbohydrate intake is most consistent across studies with several researchers showing highest intakes in the summer.2, 4, 6, 8 Additionally, while a lack of seasonal differences in vitamin6, 8 and mineral6–8, 10–16 intakes has been shown, some reports have noted equivocal seasonal changes in select micronutrients. For instance, a few studies identify summer as the season with the highest intake of vitamin C, vitamin A, vitamin D, thiamin, and vitamin B6,4, 5, 7, 11 but contrastingly, others have demonstrated lowest intakes of vitamin C and vitamin A in summer.4, 10, 17 Furthermore, sodium, zinc, and magnesium intakes have been noted to increase in the winter compared to the summer,9 however others have reported that intake of these minerals was highest in the spring.17 These inconsistencies in the data may be attributed to different methodologies, including use of FFQs, food records of various lengths, and 24-hour diet recalls, as well as to dissimilar samples of participants.
Researchers have also focused on seasonal differences in the consumption of various food groups. Three studies found increases in vegetable consumption among women in the summer months compared with winter.2, 4, 7 Reports regarding seasonal changes in protein-based food groups, such as eggs, meat, seafood, and legumes, have been inconsistent; some have stated a lack of seasonality,2, 7, 18 while others have shown increases in protein-based foods in the winter months compared to summer months.4, 6, 9, 19 From the studies reviewed, there were no significant differences in grain,2, 4, 6, 7 oils or fats,2, 4, 7 or sugar-based foods or sweets.2, 4, 7, 18 Findings regarding seasonality of fruit, beverage, and dairy intake were demonstrated in single studies and were not considered to be trends of seasonal intake.2, 18
Of the aforementioned studies, those that took place in the United States limited their analysis to select nutrients or food groups.3, 12, 13, 20, 21 To our knowledge, a broad analysis of seasonality in dietary patterns has not yet been conducted in a metropolitan area of the United States. The objective of this observational cohort study was to examine if seasonal variation in dietary intake exists in a sample of healthy, adult men and women from the metropolitan Washington, DC area. A review of the literature does not indicate common patterns in seasonal variation in dietary intake, and multiple analyses demonstrate a lack of seasonal variation altogether. Therefore, we hypothesize that there will be a lack of seasonal variation in dietary intake as assessed by food records in a population of healthy adults from the metropolitan Washington, DC area.
Methods
Subjects
Subjects were enrolled in a clinical pilot study carried out at the National Institutes of Health (NIH) Clinical Center in Bethesda, MD (clinicaltrials.gov identifier NCT01131299) from February 2011 to June 2014. The trial was approved by the NIH National Heart Lung and Blood Institute Institutional Review Board, informed consent was obtained from all subjects prior to study initiation, and procedures were carried out in accordance with Institutional Review Board regulations. Male and female (n=103) volunteers between the ages of 18–75 years were recruited through the NIH Clinical Center Patient Recruitment Office from the metropolitan Washington, DC area. Subjects were excluded from enrolling in this protocol if they were pregnant or breastfeeding, had a BMI less than 18.5, had an unstable weight that varied greater than 10% over the previous 3 months, were following a low fat diet (<20% of total energy intake), or routinely consumed fewer than 3 meals/snacks per day. Protocol exclusion criteria also included use of unstable doses of medications known to affect fat absorption, anticoagulants, anticonvulsants, antidysrhythmics, cyclosporine, mycophenolate, or thyroid hormone supplementation; vitamin A, D, E and/or K deficiencies; type I or II diabetes; or gastrointestinal conditions that could affect intestinal fat absorption.
Dietary Assessment
Dietary intake was assessed at baseline and at two additional visits with 12 – 15 weeks between each visit, thus each subject recorded their intake in three different seasons. Subjects were instructed not to change their typical diet or physical activity during the study period. Three to seven day food records (average of 6.0 + 1.5 days), including a minimum of 2 weekdays and 1 weekend day, were kept by the subjects during the week prior to each visit. Food records were collected and reviewed for additional detail by nutrition department staff. To reflect the marketplace throughout the study, dietary intake data were coded using Nutrition Data System for Research software versions 2009 through 2013, developed by the Nutrition Coordinating Center (NCC), University of Minnesota, Minneapolis, MN. Food groups included fruits (all fruit including citrus), citrus fruits, vegetables (excluding legumes), grains, dairy, protein (including legumes and seafood), seafood, discretionary (fats, oils, sugar, condiments), non-alcoholic beverages (excluding 100% fruit juice, dairy, and water), and alcoholic beverages. Food group servings are based on the recommendations made by the 2000 Dietary Guidelines for Americans22 or on Food and Drug Administration serving sizes23 for foods not included in the guidelines. Season assignment was based on the season during which most days of recorded intake occurred, with seasons defined as winter (December 21 – March 20, n=54), spring (March 21 – June 20, n=60), summer (June 21 – September 20, n= 60), and fall (September 21 – December 20, n=54). All 228 food records were analyzed for macronutrient and mineral intake. Vitamin analysis removed one subject for unusually high vitamin B12 intake secondary to clam consumption and one subject for unusually high retinol intake secondary to liver consumption (n=226). One subject was removed prior to food group analysis because fruit intake was zero and thus the data could not be log transformed (n=227).
Statistical Analysis
Of the 103 subjects who were enrolled in the study, 76 were included in the statistical analysis. Subjects were excluded if they completed fewer than three visits. Analyses were performed using Statistical Package for Social Sciences (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY). Subject demographic data were obtained from medical records at baseline. Height, weight, calculated BMI, and age were described as mean (± SD) and frequency of race and sex were described as percent. For each season, mean energy (kcals), macronutrient (g per 1000 kcals or percent of energy), micronutrients (weight/1000 kcals), and food group (servings per 2000 kcals) intake were calculated. Multivariate general linear models were run with energy, macronutrient, micronutrient, and food group intake as dependent variables and season as a categorical independent variable. All models used age, sex, race, and BMI as covariates and covariates that were not significant within each model were dropped from the final models. Analysis for vitamins removed BMI as a covariate and the analyses for minerals and food groups both removed sex as a covariate. Fruit group data were log transformed for normality. Significance was determined if p<0.05.
Results
Subject Demographics
Subject demographic data (n=76) are provided in Table 1. Participants in this study had a mean BMI of 25 ± 3.9 kg/m2 and a mean age of 34 ± 12.4 years. Overall, the population of healthy volunteers was 71.1% White and 55.3% female.
Table 1.
Subject demographics of healthy volunteers (n=76) from the metropolitan Washington, DC area.
| Mean ± SDa | |
|---|---|
| BMI (kg/m2) | 25 ± 3.9 |
| Age (years) | 34 ± 12.4 |
| % | |
| Race | |
| White | 71.1 |
| Black/African American | 9.2 |
| Asian | 13.2 |
| Unknown | 6.6 |
| Sex | |
| Male | 44.7 |
| Female | 55.3 |
SD=standard deviation.
Energy and Macronutrients
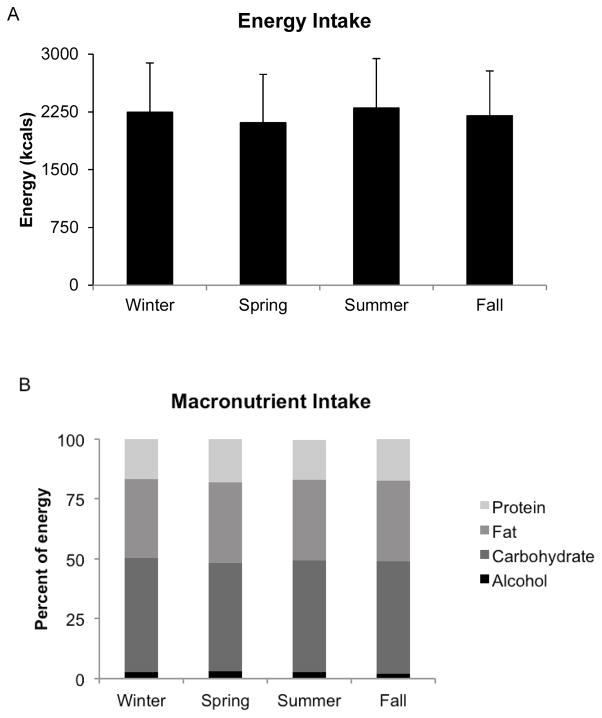
Across seasons, the mean energy intake in our population was 2214.6 ± 623.4 kcals with 17.3± 4.1%, 33.6 ± 5.5%, 46.6 ± 8.0%, and 2.7 ± 3.2% of energy from protein, fat, carbohydrate and alcohol, respectively (Table 2). Neither energy (p=0.24) nor the percent of energy from protein (p=0.32), fat (p=0.82), carbohydrate (p=0.51), nor alcohol (p=0.51) significantly differed between seasons (Figure 1). Means of macronutrient weight per unit energy (grams per 1000 kcals) did not significantly differ by season (data not shown). Means of fiber (grams/1000 kcals, p=0.65) and cholesterol (mg/1000 kcals, p=0.93) were not significantly different between seasons (data not shown).
Table 2.
Mean dietary intakea of macronutrients and food groupsb across seasons in healthy volunteers (n=76) from the metropolitan Washington, DC area.
| Nutrient/Food Groupc | Mean ± SDd |
|---|---|
| Energy (kcals) | 2214.6 ± 623.4 |
| Protein (%) | 17.3 ± 4.1 |
| Fat (%) | 33.6 ± 5.5 |
| Carbohydrate (%) | 46.6 ± 8.0 |
| Alcohol (%) | 2.7 ± 3.2 |
| Grains (servings) | 6.9 ± 2.0 |
| Fruits (servings) | 1.9 ± 1.5 |
| Vegetables (servings) | 3.7 ± 1.6 |
| Protein (servings) | 6.6 ± 2.9 |
| Dairy (servings) | 2.1 ± 1.1 |
Data were derived from analysis of food records (n=228 for energy and macronutrients, n=227 for food groups).
Protein, fat, carbohydrate, and alcohol intake reported as percent of total energy (kcals). Food group intake reported as servings per 2000 kcals.
Food groups included grains, fruits, vegetables (excluding legumes), protein (including legumes), and dairy.
SD=standard deviation.
Figure 1.
Seasonality of energy and macronutrient intake of healthy volunteers (n=76) from the metropolitan Washington, DC area. A) No significant difference in energy intake (kcals, adjusted for age, sex, BMI, and race) between seasons (winter, 2248.3±638.0; spring, 2110.2±627.2; summer, 2301.0±642.5; fall, 2200.7±581.3, p=0.236). Data shown are means ± standard deviation. B) No significant difference in percent of energy from macronutrients (adjusted for age, sex, BMI, and race). Data shown are means with all p>0.05. Winter (n=54), spring (n=60), summer (n=60), fall (n=54).
Micronutrients
The mean intake of vitamins and minerals across seasons and within seasons is shown in Table 3 and Table 4. We found no significant differences in seasonal intake of vitamins (Table 3) or minerals (Table 4).
Table 3.
Mean vitamin intakea across and within seasonsb in healthy volunteers (n=76) from the metropolitan Washington, DC area.
| Retinol (mcgc) | Vitamin D (mcg) | Vitamin E (mg c) | Vitamin K (mcg) | Vitamin C (mg) | Thiamin (mg) | Riboflavin (mg) | Niacin (mg) | Pantothenic Acid (mg) | Vitamin B6 (mg) | Folate (mcg) | Vitamin B12 (mcg) | Beta-carotene (mcg) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Across Seasons | |||||||||||||
| Mean | 205.5 | 61.8 | 5.1 | 158.4 | 84.7 | 1.5 | 1.8 | 21.6 | 5.0 | 1.8 | 411.8 | 4.2 | 4036.9 |
| SDc | 102.9 | 43.7 | 2.5 | 145.9 | 49.7 | 0.5 | 0.6 | 9.0 | 2.2 | 0.8 | 191.4 | 2.5 | 3575.0 |
| Winter | |||||||||||||
| Mean | 200.6 | 62.8 | 4.9 | 175.8 | 86.8 | 1.5 | 1.8 | 21.3 | 4.9 | 1.8 | 396.5 | 3.7 | 4330.4 |
| SD | 92.4 | 43.5 | 2.0 | 165.1 | 48.0 | 0.4 | 0.6 | 7.5 | 1.9 | 0.6 | 151.5 | 2.1 | 3445.2 |
| Spring | |||||||||||||
| Mean | 209.2 | 57.1 | 5.3 | 182.2 | 88.5 | 1.4 | 1.8 | 21.4 | 4.9 | 1.8 | 399.2 | 4.2 | 4692.4 |
| SD | 126.8 | 36.7 | 2.4 | 194.1 | 52.4 | 0.4 | 0.6 | 9.3 | 2.0 | 0.8 | 147.9 | 2.6 | 4278.4 |
| Summer | |||||||||||||
| Mean | 193.9 | 64.9 | 5.2 | 135.3 | 86.4 | 1.5 | 1.8 | 21.8 | 4.9 | 1.8 | 415.4 | 4.5 | 3829.9 |
| SD | 98.6 | 56.3 | 3.2 | 89.1 | 52.0 | 0.6 | 0.6 | 10.0 | 2.3 | 0.8 | 233.8 | 2.4 | 3556.1 |
| Fall | |||||||||||||
| Mean | 218.8 | 62.4 | 5.1 | 139.2 | 76.6 | 1.6 | 1.9 | 22.1 | 5.1 | 1.8 | 437.2 | 4.4 | 3237.3 |
| SD | 87.7 | 35.7 | 2.1 | 103.3 | 46.2 | 0.7 | 0.8 | 9.2 | 2.5 | 1.0 | 219.9 | 2.8 | 2671.8 |
| Multivariate Analysis of Difference Between Seasons | |||||||||||||
| P value | 0.53 | 0.81 | 0.87 | 0.21 | 0.74 | 0.54 | 0.40 | 0.90 | 0.70 | 0.77 | 0.53 | 0.26 | 0.19 |
Intake of micronutrients expressed as weight per 1000 kcals adjusted for age, sex and race.
Across seasons (n=226), winter (n=54), spring (n=60), summer (n=58), fall (n=54).
mcg=micrograms, mg=milligrams, SD=standard deviation.
Table 4.
Mean mineral intakea across and within seasonsb in healthy volunteers (n=76) from the metropolitan Washington, DC area.
| Calcium (mg c) | Phosphorus (mg) | Magnesium (mg) | Iron (mg) | Zinc (mg) | Selenium (mcg c) | Sodium (mg) | Potassium (mg) | |
|---|---|---|---|---|---|---|---|---|
| Across Seasons | ||||||||
| Mean | 418.6 | 647.2 | 161.2 | 8.3 | 5.7 | 61.5 | 1621.2 | 1355.3 |
| SDc | 116.2 | 118.3 | 43.2 | 3.1 | 2.1 | 16.9 | 339.4 | 284.0 |
| Winter | ||||||||
| Mean | 404.9 | 648.7 | 164.3 | 8.3 | 5.5 | 60.2 | 1673.9 | 1360.8 |
| SD | 113.0 | 143.2 | 47.6 | 3.4 | 2.0 | 17.3 | 329.8 | 279.2 |
| Spring | ||||||||
| Mean | 433.7 | 658.4 | 163.7 | 8.4 | 5.9 | 63.4 | 1642.0 | 1394.2 |
| SD | 110.8 | 113.5 | 36.0 | 2.6 | 2.3 | 17.3 | 272.1 | 304.3 |
| Summer | ||||||||
| Mean | 402.6 | 639.4 | 161.6 | 8.2 | 5.6 | 60.8 | 1574.1 | 1359.8 |
| SD | 104.4 | 97.6 | 46.0 | 3.6 | 1.7 | 14.3 | 413.2 | 293.2 |
| Fall | ||||||||
| Mean | 433.3 | 641.7 | 154.7 | 8.3 | 5.8 | 61.4 | 1597.5 | 1301.8 |
| SD | 135.2 | 119.4 | 43.0 | 2.5 | 2.2 | 18.8 | 325.2 | 252.7 |
| Multivariate Analysis of Difference Between Seasons | ||||||||
| P value | 0.30 | 0.91 | 0.69 | 0.99 | 0.69 | 0.63 | 0.39 | 0.60 |
Intake of micronutrients expressed as weight per 1000 kcals adjusted for age, BMI, and race.
Across seasons (n=228), winter (n=54), spring (n=60), summer (n=60), fall (n=54).
mg=milligrams, mcg=micrograms, SD=standard deviation.
Food Groups
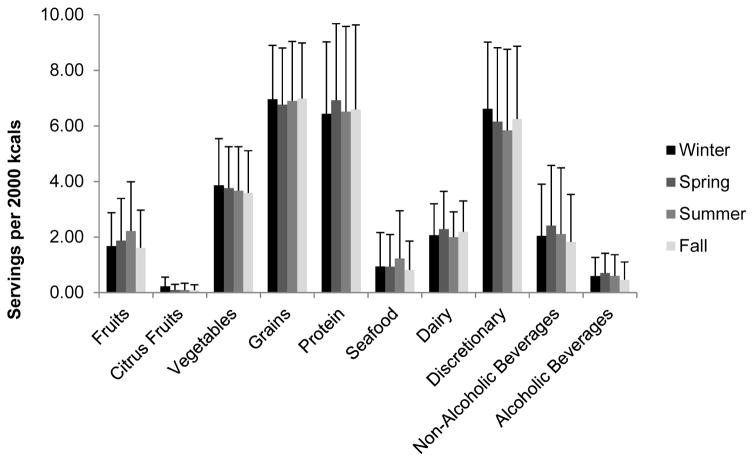
The mean intake of food groups analyzed across seasons was 6.9 ± 2.0, 1.9 ± 1.5, 3.7 ± 1.6, 6.6 ± 2.9, and 2.1 ± 1.1 servings of grains, fruits, vegetables, protein and dairy per 2000 kcals, respectively (Table 2). We found no significant differences in the number of servings per 2000 kcals of fruits, citrus fruits, vegetables, grains, protein, seafood, dairy, discretionary, non-alcoholic beverages, or alcoholic beverages between seasons (Figure 2).
Figure 2.
Mean number of servings per 2000 kcals (adjusted for age, race, and BMI) of healthy volunteers (n=76) from the metropolitan Washington DC area. Data is reported as the number of servings per 2000 kcals and shown as means ± standard deviation. Data was derived from analysis of food records; winter (n=54), spring (n=60), summer (n=59), fall (n=54). Food groups included fruits (all fruit including citrus), citrus fruits, vegetables (excluding legumes), grains, protein (including legumes and seafood), seafood, dairy, discretionary (fats, oils, sugar, condiments), non-alcoholic beverages (excluding 100% fruit juice, dairy, and water), and alcoholic beverages. All p values were >0.05.
Discussion
Clinical studies that analyze dietary intake utilizing food records may not consider the possibility of seasonal variation. Understanding the impact of seasonality on dietary intake is hampered by inconsistencies in study design and analysis. Previous research is not consistent in its comparison of seasons. Although most studies have looked at differences across all four seasons,2, 3, 6–8, 10–13, 17, 18, 20, 21, 24 a few have only analyzed differences between summer and winter.4, 5, 9, 19 The nutrients analyzed, the division and definition of food groups and seasons, and adjustment for confounding factors are also inconsistent across studies. Research performed internationally regarding the impact of season on dietary intake in metropolitan populations shows conflicting results. Within metropolitan populations in the United States, studies have specifically analyzed intakes of macronutrients,20 iron,12 magnesium,13 carotenoids, fruits and vegetables.21 The inconsistencies reported in international studies and the lack of research within the United States raises concerns regarding the accuracy of dietary intake data in studies spanning multiple seasons. To our knowledge, this was the first study to perform a broad analysis of seasonality in dietary patterns in a metropolitan area of the United States. Our results indicate that people living in the metropolitan Washington, DC area do not exhibit seasonal variation in dietary intake.
We found no difference in energy or macronutrient (fat, carbohydrate, protein, and alcohol) intake across seasons in our population, which is consistent with results from multiple studies.2, 3, 5–7, 9, 10, 19, 20, 24 In contrast to our results, some studies found differences in energy, carbohydrate, and protein intake across seasons.2–4, 6, 8, 11, 20 In a study by Ma et al,20 which is perhaps the study with the most similar population to the current study, differences in daily caloric intake by season were reported. However, their study collected 24 hour recalls and the mean age of the study participants (47.6 years) was higher than in our study participants.20 Other studies that reported differences in energy and macronutrient intake also used different dietary assessment instruments such as 24-hour recalls5, 8 or FFQs,6, 11 or different study populations. 2, 4, 6 This could partially explain the difference between their results and those obtained in this study. Furthermore, many of the reported findings occurred when dietary intake analysis was stratified by sex,2, 4–6, 8 race,20 or age.8
Though our study found no seasonal difference in fiber consumption, other investigators reported higher consumption among women only in the winter 2, 4, 5 and lower consumption among pregnant women in the summer.7, 17 Findings from these studies are a result of data that were analyzed for differences within or across sexes or from a non-comparable population. Only five of the reviewed studies measured cholesterol intake.4, 5, 8–10, 19 The differences reported were sex-specific and non-conclusive.4, 5, 9, 19
Our analysis found no seasonal differences in vitamin or mineral intake. Although some published findings align with our results,6, 8 other studies found seasonal variation in certain vitamins.4, 5, 7, 9–11, 17, 25 Similar to previously reported macronutrient variations, these findings of seasonality in vitamin intake were often sex-specific and inconsistent. Intake of vitamins C, A, D, E, B6 and thiamin was reported to be the highest in summer.4, 5, 7, 11 However, in other studies consumption of vitamins C and A was also found to be lowest during this season.4, 10, 17, 25 Additional trends were noted in vitamins C, A, D, E, B6, and thiamin, along with niacin and folate, with highest intakes reported during winter.4, 5, 7, 9, 17, 25 The above-mentioned differences may once again be a result of a different population studied and/or diet assessment method used. The majority of previous studies are consistent with our finding of a lack of seasonal variation in mineral intake.6–8, 10–14, 17
We did not observe differences across seasons in the consumption of food groups. Previous studies did not report seasonal differences in the intake of grain,2, 4, 6, 7 oil/fat,2, 4, 7 or sugar/sweets.2, 4, 7, 18 Three studies observed an increase in vegetable consumption among women in the summer months2, 4, 7 and an increase in protein-based food groups (i.e., eggs, poultry, meat, seafood, legumes) in the winter.4, 6, 9, 19 These studies differ from ours in their investigation of sex-specific differences,4 use of FFQs to assess dietary intake,6, 9, 19 and lack of control for total energy intake.6 It is interesting to note that although we found no differences with regard to the number of servings of each food group consumed, it is unknown if the types of foods chosen from within each group vary with season. When compared to a nationally representative sample, mean intake of all food groups across seasons was higher in our study population, with the largest differences in fruit and vegetable intake26.
The lack of seasonal variation in nutrient and food group intake in a metropolitan area in the US could be due to several factors. Although we were unable to collect socioeconomic data for our study population, it is possible that participants in our study have more disposable income available, allowing for the purchase of produce regardless of seasonality. A higher socioeconomic class would also allow for better overall food access. It is also possible that food manufacturing and distribution practices in the US allow for a more consistent food supply throughout the year compared to less developed countries. Our study was not designed to answer these questions and further research in this area is necessary.
This study was strengthened by use of repeated dietary intake reports which were collected using multiple-day food records immediately prior to each participant visit. Our study had an average of six day food records, which is more representative of usual intake than a single day.27 All food records were reviewed for accuracy by trained nutrition staff using three dimensional food models and coded into a robust database. Food records do not rely on memory, and are assumed to approximate actual intake with greater face validity than other methods like diet histories or FFQs.1 However, food records do have limitations including under-reporting and potential for subjects to alter dietary intake while recording1.
Although our study adjusted for sex, BMI, age, and race, studies with a greater number of subjects would need to be conducted in order to conduct stratified analyses for sex or race. In addition, it is possible that a larger sample size may allow detection of differences in seasonal dietary intake that our sample size did not allow us to identify. Additionally, our study examined a homogenous group of primarily White and relatively young subjects residing in a metropolitan region. While the average age of the study population may be younger than studies in other geographical areas, the District of Columbia median age is 33.9 years which is similar to our study population28. We were unable to collect data on the socioeconomic status of these participants, therefore, the extent to which this variable may affect seasonal variation remains unclear. Additional studies must address these differences to determine whether seasonal variation exists within specific populations.
Conclusions
Determining if and to what extent variation exists in nutrient intake across seasons will contribute to clinical research by guiding researchers on making necessary adjustments that would account for possible seasonal effects. Given that we were unable to find seasonal variation in energy, macronutrient, micronutrient or food group intake in our population of healthy volunteers from a metropolitan area, investigators may not need to consider the season during which diet is examined when designing studies of nutrient intake in similar populations.
Acknowledgments
Funding/support:
This study was funded by the National Institutes of Health Intramural Research Program.
This work could not have been completed without the help and support of Maryann Kaler, Clinical Nurse Practitioner; Dilalat O. Bello, Metabolic Research Technician; Merel Kozlosky, Dietetic Internship Director; and Madeline Michael, Chief, Clinical Nutrition Services at the NIH Clinical Center. This research was supported by the National Institutes of Health Intramural Research Program. Please note that author sequence follows the “first-last-author-emphasis” norm as described in Tscharntke T, Hochberg ME, Rand TA, Resh VH, Krauss J (2007) Author sequence and credit for contributions in multiauthored publications. PLos Biol 5(1):e18. doi:10.1371/journal.pbio.0050018.
Footnotes
Statement of potential conflict of interest:
No potential conflict of interest was reported by the authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Shanna Bernstein, Email: shanna.bernstein@cc.nih.gov, Metabolic Research Dietitian, Nutrition Department, Clinical Center, National Institutes of Health, Building 10, Room B2-2426, 10 Center Drive, MSC 1078, Bethesda, MD 20892, 301-496-8170 (office), 301-496-0622 (fax).
Kirsten Zambell, Email: zambellk@cc.nih.gov, Clinical Research Dietitian, Nutrition Department, Clinical Center, National Institutes of Health, Building 10, Room B2-2426, 10 Center Drive, MSC 1078, Bethesda, MD 20892, 301-827-0885 (office), 301-496-0622 (fax).
Marcelo J. Amar, Email: marcelo.amar@nih.gov, Pulmonary and Vascular Medicine Branch, National Heart, Lung and Blood Institute, National Institutes of Health, 10 Center Drive, MSC 1666, Bethesda, MD 20892, 301-402-0521 (office), 301-402-0190 (fax).
Carolina Arango, Email: carolina.arango@nih.gov, Dietetic Intern, Nutrition Department, Clinical Center, National Institutes of Health, Building 10, Room B2-2426, 10 Center Drive, MSC 1078, Bethesda, MD 20892, 301-496-9873 (office), 301-496-0622 (fax).
Rachel C. Kelley, Email: Rachel.kelley@nih.go, Dietetic Intern, Nutrition Department, Clinical Center, National Institutes of Health, Building 10, Room B2-2426, 10 Center Drive, MSC 1078, Bethesda, MD 20892, 301-594-6881 (office), 301-496-0622 (fax).
Susan G. Miszewski, Email: susan.miszewski@nih.go, Dietetic Intern, Nutrition Department, Clinical Center, National Institutes of Health, Building 10, Room B2-2426, 10 Center Drive, MSC 1078, Bethesda, MD 20892, 301-594-9429 (office), 301-496-0622 (fax).
Samantha Tryon, Email: Samantha.tryon@nih.go, Dietetic Intern, Nutrition Department, Clinical Center, National Institutes of Health, Building 10, Room B2-2426, 10 Center Drive, MSC 1078, Bethesda, MD 20892, 301-594-4114 (office), 301-496-0622 (fax).
Amber B. Courville, Email: courvillea@cc.nih.gov, Metabolic Research Dietitian, Nutrition Department, Clinical Center, National Institutes of Health, Building 10, Room B2-2426, 10 Center Drive, MSC 1078, Bethesda, MD 20892, 301-594-8051 (office), 301-496-0622 (fax).
References
- 1.Johnson RK, YB, Hankin J. Dietary Assessment and Validation. In: Horn EMaLV., editor. Research: Successful Approaches. 3. American Dietetic Association; 2008. pp. 187–204. [Google Scholar]
- 2.Van Staveren WA, Deurenberg P, Burema J, De Groot LC, Hautvast JG. Seasonal variation in food intake, pattern of physical activity and change in body weight in a group of young adult Dutch women consuming self-selected diets. Int J Obes. 1986;10:133–145. [PubMed] [Google Scholar]
- 3.de Castro JM. Seasonal rhythms of human nutrient intake and meal pattern. Physiol Behav. 1991;50:243–248. doi: 10.1016/0031-9384(91)90527-u. [DOI] [PubMed] [Google Scholar]
- 4.Capita R, Alonso-Calleja C. Differences in reported winter and summer dietary intakes in young adults in Spain. Int J Food Sci Nutr. 2005;56:431–443. doi: 10.1080/09637480500407875. [DOI] [PubMed] [Google Scholar]
- 5.Costa AF, Yokoo EM, Antonio dos Anjos L, et al. Seasonal variation of food intake of adults from Niteroi, Rio de Janeiro, Brazil. Rev Bras Epidemiol. 2013;16:513–524. doi: 10.1590/S1415-790X2013000200025. [DOI] [PubMed] [Google Scholar]
- 6.Fowke JH, Schlundt D, Gong Y, et al. Impact of season of food frequency questionnaire administration on dietary reporting. Ann Epidemiol. 2004;14:778–785. doi: 10.1016/j.annepidem.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Prasad M, Lumia M, Erkkola M, et al. Diet composition of pregnant Finnish women: changes over time and across seasons. Public Health Nutr. 2010;13:939–946. doi: 10.1017/S1368980010001138. [DOI] [PubMed] [Google Scholar]
- 8.Rossato SL, Olinto MT, Henn RL, Anjos LA, Bressan AW, Wahrlich V. Seasonal effect on nutrient intake in adults living in Southern Brazil. Cad Saude Publica. 2010;26:2177–2187. doi: 10.1590/s0102-311x2010001100019. [DOI] [PubMed] [Google Scholar]
- 9.Shahar DR, Yerushalmi N, Lubin F, Froom P, Shahar A, Kristal-Boneh E. Seasonal variations in dietary intake affect the consistency of dietary assessment. Eur J Epidemiol. 2001;17:129–133. doi: 10.1023/a:1017542928978. [DOI] [PubMed] [Google Scholar]
- 10.Mansour A, Ahadi Z, Qorbani M, Hosseini S. Association between dietary intake and seasonal variations in postmenopausal women. J Diabetes Metab Disord. 2014;13:52. doi: 10.1186/2251-6581-13-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tokudome Y, Imaeda N, Nagaya T, et al. Daily, weekly, seasonal, within- and between-individual variation in nutrient intake according to four season consecutive 7 day weighed diet records in Japanese female dietitians. J Epidemiol. 2002;12:85–92. doi: 10.2188/jea.12.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miles CW, Collins JS, Holbrook JT, Patterson KY, Bodwell CE. Iron intake and status of men and women consuming self-selected diets. Am J Clin Nutr. 1984;40:1393–1396. doi: 10.1093/ajcn/40.6.1393. [DOI] [PubMed] [Google Scholar]
- 13.Lakshmanan FL, Rao RB, Kim WW, Kelsay JL. Magnesium intakes, balances, and blood levels of adults consuming self-selected diets. Am J Clin Nutr. 1984;40:1380–1389. doi: 10.1093/ajcn/40.6.1380. [DOI] [PubMed] [Google Scholar]
- 14.Kim DW, Kyung Park M, Kim J, et al. Sources of variation in nutrient intake and the number of days to assess usual intake among men and women in the Seoul metropolitan area, Korea. Br J Nutr. 2013;110:2098–2107. doi: 10.1017/S0007114513001554. [DOI] [PubMed] [Google Scholar]
- 15.Cai H, Yang G, Xiang Y-B, et al. Sources of variation in nutrient intakes among men in Shanghai, China. Public Health Nutr. 2005;8:1293–1299. doi: 10.1079/phn2005748. [DOI] [PubMed] [Google Scholar]
- 16.Cai H, Shu XO, Hebert JR, et al. Variation in nutrient intakes among women in Shanghai, China. Eur J Clin Nutr. 2004;58:1604–1611. doi: 10.1038/sj.ejcn.1602013. [DOI] [PubMed] [Google Scholar]
- 17.Watson PE, McDonald BW. Seasonal variation of nutrient intake in pregnancy: effects on infant measures and possible influence on diseases related to season of birth. Eur J Clin Nutr. 2007;61:1271–1280. doi: 10.1038/sj.ejcn.1602644. [DOI] [PubMed] [Google Scholar]
- 18.Krauchi K, Wirz-Justice A. The four seasons: food intake frequency in seasonal affective disorder in the course of a year. Psychiatry Res. 1988;25:323–338. doi: 10.1016/0165-1781(88)90102-3. [DOI] [PubMed] [Google Scholar]
- 19.Shahar DR, Froom P, Harari G, Yerushalmi N, Lubin F, Kristal-Boneh E. Changes in dietary intake account for seasonal changes in cardiovascular disease risk factors. Eur J Clin Nutr. 1999;53:395–400. doi: 10.1038/sj.ejcn.1600761. [DOI] [PubMed] [Google Scholar]
- 20.Ma Y, Olendzki BC, Li W, et al. Seasonal variation in food intake, physical activity, and body weight in a predominantly overweight population. Eur J Clin Nutr. 2006;60:519–528. doi: 10.1038/sj.ejcn.1602346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ziegler RG, Wilcox HB, 3rd, Mason TJ, Bill JS, Virgo PW. Seasonal variation in intake of carotenoids and vegetables and fruits among white men in New Jersey. Am J Clin Nutr. 1987;45:107–114. doi: 10.1093/ajcn/45.1.107. [DOI] [PubMed] [Google Scholar]
- 22.Bowman SA, FJ, Moshfegh A. MyPyramid Equivalents Database, 2.0 for USDA Survey Foods, 2003–2004 Beltsville Human Nutrition Research Center, Agricultural Research Service, U.S. Department of Agriculture. Beltsville, MD: Food Surveys Research Group; 2008. [Google Scholar]
- 23.US Food and Drug Administration. [Accessed March 3, 2015];US Food and Drug Administration Code of Federal Regulations Title 21. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=101.9. Updated April 2014.
- 24.Fehilly AM, Phillips KM, Sweetnam PM. A weighed dietary survey of men in Caerphilly, South Wales. Hum Nutr Appl Nutr. 1984;38:270–276. [PubMed] [Google Scholar]
- 25.Rasanen L. Nutrition survey of Finnish rural children. VI. Methodological study comparing the 24–hour recall and the dietary history interview. Am J Clin Nutr. 1979;32:2560–2567. doi: 10.1093/ajcn/32.12.2560. [DOI] [PubMed] [Google Scholar]
- 26.National Cancer Institute. Usual Dietary Intakes: Food Intakes, US Population, 2007–10. [Accessed July 8, 2015];Applied Research Probram Website. http://appliedresearch.cancer.gov/diet/usualintakes/pop/2007-10/. Updated May 22, 2014.
- 27.Block G. A review of validations of dietary assessment methods. Am J Epidemiol. 1982;115:492–505. doi: 10.1093/oxfordjournals.aje.a113331. [DOI] [PubMed] [Google Scholar]
- 28.City-Data.com website. Washington: District of Columbia; [Accessed July 14, 2015]. http://www.city318data.com/city/Washington-District-of-Columbia.html. [Google Scholar]