Abstract
Objective
Isolated renal artery aneurysms are rare and controversy remains about indications for surgical repair. Little is known about the impact of endovascular therapy on patient selection and outcomes of renal artery aneurysms.
Methods
We identified all patients undergoing open or endovascular repair of isolated renal artery aneurysms in the Nationwide Inpatient Sample (NIS) from 1988 to 2011 for epidemiologic analysis. Elective cases were selected from the period of 2000 to 2011, to create comparable cohorts for outcome comparison. We identified all patients with a primary diagnosis of renal artery aneurysms undergoing open surgery (reconstruction or nephrectomy) or endovascular repair (coil or stent). Patients with a concomitant aortic aneurysms or dissections were excluded. We evaluated patient characteristics, management, and in-hospital outcomes for open and endovascular repair, and we examined changes in management and outcomes over time.
Results
We identified 6,234 renal artery aneurysm repairs between 1988 and 2011. Total repairs increased after the introduction of endovascular repair (8.4 in 1988 to 13.8 in 2011 per 10million(M) US population, P=0.03). Endovascular repair increased from 0 in 1988 to 6.4 in 2011 per 10M US population (P<.0001). However, there was no concomitant decrease in open surgery (5.5 in 1988 to 7.4 in 2011 per 10M US population, P=0.28). From 2000–2011 there were 1,627 open and 1,082 endovascular elective repairs. Patients undergoing endovascular repair were more likely to have a history of coronary artery disease (18% vs. 11%, P<0.001), prior myocardial infarction (5.2% vs. 1.8%, P<0.001) and renal failure (7.7% vs. 3.3%, P<0.001). In-hospital mortality was 1.8% for endovascular and 0.9% for open reconstruction (P=0.037), and 5.4% for nephrectomy (P<.001 compared to all revascularization). Complication rates were 12.4% for open repair vs 10.5% for endovascular repair (P=0.134), including more cardiac (2.2% vs. 0.6%, P=0.001) and peripheral vascular complications (0.6% vs. 0.0%, P=0.014) with open repair. Open repair had a longer length of stay (6.0 vs. 4.6 days, P<0.001). After adjustment for other predictors of mortality, age (OR 1.05 per decade, 95% CI 1.0–1.1, P=0.001), heart failure (OR 7.0, 95% CI 3.1–16.0, P<.001) and dysrhythmia (OR 5.9, 95% CI 2.0–16.8, P=0.005), Endovascular repair was still not protective (OR 1.6, 95% CI 0.8–3.2, P=0.145).
Conclusion
More renal artery aneurysms are being treated with the advent of endovascular techniques, without a reduction in operative mortality or a reduction in open surgery. Indications for repair of renal artery aneurysms should be re-evaluated.
INTRODUCTION
Isolated renal artery aneurysms are rare, with an estimated incidence cited between 0.1 and 1.3% in the general population.1–4 The natural history of these aneurysms is uncertain, and therefore the indications for surgical intervention remain controversial.5, 6 The majority of patients are asymptomatic at time of discovery of a renal artery aneurysms.4, 7 The increased rate of incidental discovery is largely attributable to the use of non-invasive imaging for evaluation of other conditions.6 Potential complications of renal artery aneurysms include rupture, distal embolization, infarction, hypertension, dissection, renal failure, and arteriovenous fistula.8, 9 The mortality rate of rupture is reported to be as high as 80%.10
Generally, intervention is undertaken for aneurysm diameter > 2.0 cm, ruptured aneurysm, dissection, localized symptoms, female gender within childbearing years, and renovascular hypertension.6, 11–15 Before the advent of endovascular techniques, open repair was the conventional method of treatment, with techniques including excision with primary repair or patch angioplasty, excision with reconstruction using bypass, extracorporeal reconstruction with autotransplantation, and nephrectomy.13, 16 The less invasive alternative, endovascular repair, includes coil embolization or the use of a stent graft. The technical success and safety of the endovascular treatment for renal artery aneurysms in experiences hands have been demonstrated, with a low morbidity and mortality.17–21
The purpose of this population based retrospective study is to evaluate the impact of the introduction of endovascular treatment on total repair rates in the United States, and compare mortality and morbidity outcomes between endovascular and open surgical repair.
METHODS
DATASET
All patients who had an isolated renal artery aneurysm in the period from 1988 to 2011 were extracted from the Nationwide Inpatient Sample (NIS). The NIS is the largest US all-payer inpatient database, and has been collected as part of the Healthcare Cost and Utilization Project (HCUP). It represents 20% of U.S. hospitalizations, and contains sampling weights to approximate total U.S. population estimates. The sampling weights were applied on our entire analysis. The NIS database contains de-identified data only without any protected health information. Therefore Institutional Review Board approval and patient consent were waived.
PATIENTS
Using the International Classification of Diseases, edition 9 (ICD9) code 442.1, we identified all patients with a primary diagnosis of renal artery aneurysm undergoing open or endovascular repair in the NIS from 1988 to 2011. We excluded patients with concomitant diagnoses of aortic aneurysms, as well as those with a thoracic aneurysm and/or aortic dissection (ICD9 441, 441.0, 441.1, 441.2, 441.3, 441.4, 441.5, 441.6, 441.7, 441.9, 441.00, 441.01, 441.02, 441.03). The open repair cohort consisted of patients who underwent either nephrectomy (ICD9 554, 555.1, 555.2) or an open reconstruction (ICD9 380.6, 381.6, 383.6, 384.6, 386.6, 388.6, 392.4, 392.6, 395.0, 395.2, 395.5) and the endovascular cohort consisted of patients who had a coil embolization (ICD9 397.9) or a stent placement (ICD9 399.0, 397.1). We documented demographics including age, sex, race, and co-morbid conditions including but not limited to coronary artery disease, hypertension, dysrhythmia, prior myocardial infarction, heart failure, chronic obstructive pulmonary disease, acute renal failure, chronic renal failure, and peripheral vascular disease.
OUTCOMES
We examined trends in management of total repairs and the proportion of elective and urgent open vs. endovascular repairs during our entire study period (1988–2011). However, for our outcomes comparison, we limited our analysis to elective repairs during the years 2000 to 2011, to create contemporaneous comparable cohorts with results relevant to current patient care. Since outcomes for open repair improved over time, inclusion of the results from a period no longer representative of current outcomes would unfairly bias against open surgery. We compared open surgical revascularizations to endovascular interventions and subsequently compared nephrectomy to all other repairs. Outcomes included in-hospital deaths, post-operative complications and length of stay. Multivariable logistic regression was used to adjust for other potential predictors of mortality including age, coronary artery disease, prior myocardial infarction, chronic renal failure, peripheral vascular disease, heart failure, and dysrhythmia. Nephrectomy patients were included in the multivariable analysis.
STATISTICAL ANALYSIS
Statistical analysis was completed using SPSS statistical software (version 20; IBM Corp, Armonk, NY). Where appropriate, continuous variables were compared using two-tailed independent sample t-test, and Chi-square or Fischer’s exact test were used for categorical variables. The Cochran-Armitage test for trend was used to determine changes over time. Statistical significance was defined as P < 0.05.
RESULTS
EPIDEMIOLOGIC TRENDS
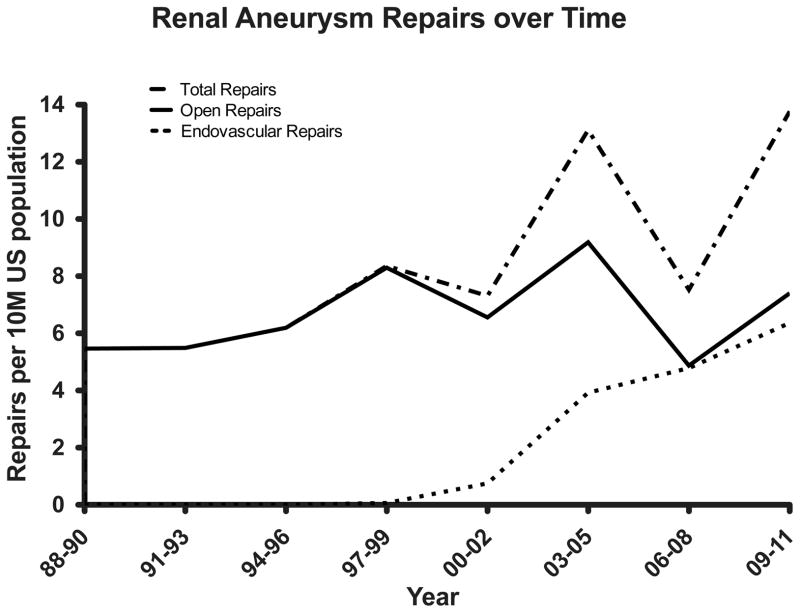
We identified 6,234 patients undergoing renal artery aneurysm repairs between 1988 and 2011, encompassing both elective and urgent procedures. Both the overall total repair rate and the endovascular repair rate were noted to increase steadily over time (total repairs from 8.4 in 1988–1990 to 13.8 in 2009–2011 per 10M US population, P=0.03 and endovascular repairs from 0 in 1988–1990 to 6.4 in 2009–2011 per 10M US population, P<.0001) shown in Figure 1. After the introduction of endovascular repairs, the rate of open repair did not decrease significantly (5.5 in 1988–1990 to 7.4 in 2009–2011 per 10M US population, P =0.28), indicating that endovascular procedures are not replacing open procedures.
Figure 1.
Quantitative comparison of endovascular and open repairs (including both elective and urgent procedures)
ELECTIVE ENDOVASCULAR VS. OPEN REPAIR 2000–2011
There were 2,709 elective procedures from 2000 to 2011; 1,627 open repairs and 1,082 endovascular repairs. Patients undergoing endovascular repair were more likely to have a history of coronary artery disease (18% vs. 11%, P<0.001), prior myocardial infarction (5.2% vs. 1.8%, P<0.001), chronic renal failure (7.7% vs. 3.3%, P<0.001) and dysrhythmia (4.0 vs. 2.4%, P=0.019) and less likely to have peripheral arterial disease (9.2% vs.14%, P<0.01). Age and other pre-operative comorbidities, including hypertension, heart failure, and chronic pulmonary disease, were comparable between the two groups, as demonstrated in Table I.
Table I.
Pre-Operative characteristics of patients undergoing elective endovascular and open repair of renal artery aneurysm from 2000–2011
| Pre-operative Demographics | Open (N=1627) | EVAR (N=1082) | P-value |
|---|---|---|---|
| Age | 57 | 58 | 0.087 |
| Female | 57% | 42% | <.001 |
| Coronary Artery Disease | 11% | 18% | <.001 |
| Hypertension | 61% | 58% | 0.168 |
| Dysrhythmia | 2.4% | 4.0% | 0.019 |
| Atrial fibrillation | 6.6% | 6.4% | 0.837 |
| Prior myocardial infarction | 1.8% | 5.2% | <.001 |
| Heart failure | 5.0% | 4.9% | 0.922 |
| Chronic obstructive pulmonary disease | 6.2% | 7.7% | 0.123 |
| Chronic Renal Failure | 3.3% | 7.7% | <.001 |
| Cardiovascular disease | 0.9% | 1.5% | 0.133 |
| Peripheral vascular disease | 14% | 9.2% | <.001 |
In-hospital mortality was significantly higher for endovascular repairs compared to all open repairs (1.8% vs. 0.9%, P=0.037). (Table II) Overall complication rates were 12.4% for open repairs vs 10.5% for endovascular repairs (P=0.134). (Table II) This included more cardiac (2.2% vs. 0.6%, P=0.001) and peripheral vascular complications (0.6% vs. 0.0%, P=0.014) with open repair. The rates of respiratory complications, wound dehiscence, bleeding complications, and infection were not significantly different between groups, as shown in Table II. Open repair was associated with a longer length of stay (6.0 vs. 4.6 days, P<0.001).
Table II.
In hospital outcomes of elective endovascular and open renal artery aneurysm repairs from 2000–2011
| Open (N=1627) | Endo (N=1082) | P-value | |
|---|---|---|---|
| In-hospital Mortality | 0.9% | 1.8% | 0.037 |
| Cardiac complications | 2.2% | 0.6% | 0.001 |
| Respiratory complications | 4.6% | 4.3% | 0.658 |
| Peripheral vascular complications | 0.6% | 0.0% | 0.014 |
| Acute renal failure | 10% | 6.8% | 0.001 |
| Wound dehiscence | 0.3% | 0.0% | 0.068 |
| Bleeding complications | 5.2% | 5.0% | 0.842 |
| Infection | 0.9% | 0.8% | 0.983 |
| Any complication | 12.4% | 10.5% | 0.134 |
| Length of Stay (days) | 6.0 | 4.6 | <.001 |
Nephrectomy patients had a higher in hospital mortality than the overall repair group (5.4% vs. 1.3% p<0.001) and length of stay was longer (8 vs. 6 days, P<.001). (Table III) Infection, wound dehiscence, respiratory complications, and total complications were higher after nephrectomy.
Table III.
In hospital outcomes after nephrectomy versus any revascularization for renal artery aneurysm from 2000–2011
| Post-operative Outcomes | Nephrectomy (N=459) | All Repairs (N=2709) | P-value |
|---|---|---|---|
| In-hospital Mortality | 5.4% | 1.3% | <.001 |
| Cardiac complications | 2.4% | 1.5% | 0.169 |
| Respiratory complications | 19.6% | 4.5% | <.001 |
| Peripheral vascular complications | 0.0% | 0.3% | 0.217 |
| Wound dehiscence | 3.5% | 0.2% | <.001 |
| Bleeding complications | 5.4% | 5.0% | 0.721 |
| Infection | 2.2% | 0.8% | 0.009 |
| Any complication | 24.0% | 11.6% | <.001 |
| Length of Stay (days) | 7.9 | 5.5 | <.001 |
Multivariable predictors of mortality after a renal artery aneurysm were heart failure (OR 4.8, 95% CI 2.3–9.8, P<.001), dysrhythmia (OR 7.4, 95% CI 3.5–15.7, P<.001) and undergoing a nephrectomy (OR 9.4, 95% CI 2.9–30.7, P<.001). After adjustment, endovascular repair was neither protective nor predictive of mortality (OR 1.7, 95% CI 0.9–3.4, P=0.110).
DISCUSSION
Our study shows that there has been an increase in total repairs since the introduction of endovascular techniques, without any decrease in open surgery. Patients undergoing endovascular repair had more pre-operative cardiac comorbidities and higher in-hospital mortality compared to open repair patients, although adjusted mortality was similar after accounting for differences in baseline characteristics. However, cardiac and peripheral complication rates were higher for the open repair group, and they had a longer length of stay. Henke et al reviewed 168 patients with 252 aneurysms, where 121 patients underwent surgery. Three patients presented with ruptured renal artery aneurysm. They found no perioperative deaths or late postoperative deaths due to renal artery aneurysm surgery.6 In a retrospective analysis of forty-four renal artery aneurysm repairs from 2000 to 2012, Tsilimparis et al. reported no mortality and equivalent perioperative complication rates of 15% and 17% for open repair and endovascular repair patients respectively. We found a lower rate of endovascular interventions for renal artery aneurysms than Tsilimparis et al., who found that 55% of renal aneurysms were treated in an endovascular fashion. This suggests that nationally, practitioners are not as aggressive with an endovascular approach as centers of excellence. Thus, a relative lack of experience with endovascular techniques may explain the lack of difference in mortality between open and endovascular repair seen previously. Furthermore, this study is reflective of general practice, rather than selected experiences at centers of excellence. Additionally, they showed that endovascular repair was associated with a significantly shorter hospitalization of 2.3 days, in comparison to 6.3 days for open repair, which was comparable to our findings.22 Zhang et al. endorse the use of endovascular repair as a first-line technique for renal artery aneurysm treatment.21 In their study of 15 patients treated with endovascular techniques, they had no peri-procedural mortality or major complications, with a technical success rate of 100%. While our analysis found fewer complications and shorter length of stay with endovascular techniques, we found no reduction in operative mortality.
The Low Frequency Disease Consortium reported an analysis in support of more conservative management and surveillance rather than aggressive surgical treatment, proposing that the current recommendations for renal artery aneurysm treatment at a diameter of 2 cm may be too aggressive.23 In their retrospective study of 40 patients, they found a rate of aneurysm rupture and death to be zero over a mean 36-month follow-up period, and a very low growth rate of 0.60 ± 0.16 mm/year.23
An analysis by Hislop et al. using the New York State inpatient database noted a significant increase in both the total number of renal artery aneurysm repairs as well as an increase in the proportion of endovascular repairs performed from 2000 to 2006.9 Our study confirms this finding with a longer time period including the pre-endovascular era and is representative of the entire United States. In their retrospective review of 215 patients undergoing renal artery aneurysm repair, endovascular therapy was also associated with a lower incidence of complications, and a significantly lower length of stay.9 Additionally, the favorable postoperative outcomes reported for the endovascular repairs were comparable to those observed in our analysis and lend support to the notion that endovascular repairs may also be economically more favorable as indicated by the lower median cost and earlier discharge. The mortality rate was 1.1% in their endovascular cohort and 3.2% in the open repair group.9 This however, was not significantly different. In our larger, national analysis of 2709 procedures, endovascular repairs had significantly higher in-hospital mortality than open repairs. This was in part attributed to the comorbidities of the patients who received an endovascular treatment compared to those in the open repair cohort. While this finding was unexpected, endovascular procedures may also be associated with technique-specific complications, including hemorrhage, renal artery dissection, postembolization syndrome and coil migration.21 Additionally, there is likely a publication bias in that centers may not choose to publish their results if they find that their endovascular patients fared worse than open surgical patients or worse than prior reports of endovascular treatment. This highlights the benefit of a national analysis such as this, which is reflective of general practice, rather than selected experiences at centers of excellence. While we are able to study a large sample size, our study is limited in that it is not a randomized controlled trial. It is an observational study of administrative data and is subject to coding errors. Our data lack information on aneurysm diameter, renal size and the location of the renal artery aneurysm, whether it is found in the main renal artery or the hilum of the kidney, which renders us unable to comment on the appropriate threshold for intervention. After adjustment for co-existing conditions, the increased mortality with endovascular repair was no longer significant (OR 1.7, 95% CI 0.9–3.4). The dataset provides in-hospital data only, with no information available regarding prior endovascular or open procedures or follow-up after discharge. It is possible that some patients undergoing endovascular procedures are being treated as outpatients and thus would not be included in the NIS. Although we feel this is unlikely, if this were a substantial proportion of procedures, this would likely cause our analysis to overestimate the procedural complication rate and underestimate the proportion of patients treated with endovascular means. Nevertheless, our study represents one of the larger American series and may be broadly generalizable due to both academic and community hospitals that the NIS incorporates.
CONCLUSION
This retrospective review demonstrates that more renal artery aneurysms are being treated after the introduction of endovascular techniques. Although there is evidence supporting a significantly lower rate of post-operative complications and a shorter length of stay with endovascular repair, there has not been a reduction in operative mortality nor has there been a reduction in open surgical procedures. Therefore, re-evaluation of the indications of repair of isolated renal artery aneurysms, by in particular endovascular, but also by open techniques, is warranted.
Acknowledgments
Supported by grant 5R01HL105453-03 from the NHLBI and the NIH T32 Harvard-Longwood Research Training in Vascular Surgery grant HL007734.
Footnotes
Presented at the SVS 2014 Vascular Annual Meeting held on June 4–7 in Boston, MA.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hageman JH, Smith RF, Szilagyi E, Elliott JP. Aneurysms of the renal artery: problems of prognosis and surgical management. Surgery. 1978;84(4):563–72. [PubMed] [Google Scholar]
- 2.Stanley JC, Rhodes EL, Gewertz BL, Chang CY, Walter JF, Fry WJ. Renal artery aneurysms. Significance of macroaneurysms exclusive of dissections and fibrodysplastic mural dilations. Arch Surg. 1975;110(11):1327–33. doi: 10.1001/archsurg.1975.01360170067009. [DOI] [PubMed] [Google Scholar]
- 3.Henriksson C, Bjorkerud S, Nilson AE, Pettersson S. Natural history of renal artery aneurysm elucidated by repeated angiography and pathoanatomical studies. European urology. 1985;11(4):244–8. doi: 10.1159/000472506. [DOI] [PubMed] [Google Scholar]
- 4.Tham G, Ekelund L, Herrlin K, Lindstedt EL, Olin T, Bergentz SE. Renal artery aneurysms. Natural history and prognosis. Annals of surgery. 1983;197(3):348–52. doi: 10.1097/00000658-198303000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.English WP, Pearce JD, Craven TE, Wilson DB, Edwards MS, Ayerdi J, et al. Surgical management of renal artery aneurysms. J Vasc Surg. 2004;40(1):53–60. doi: 10.1016/j.jvs.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 6.Henke PK, Cardneau JD, Welling TH, 3rd, Upchurch GR, Jr, Wakefield TW, Jacobs LA, et al. Renal artery aneurysms: a 35-year clinical experience with 252 aneurysms in 168 patients. Annals of surgery. 2001;234(4):454–62. doi: 10.1097/00000658-200110000-00005. discussion 62–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallagher KA, Phelan MW, Stern T, Bartlett ST. Repair of complex renal artery aneurysms by laparoscopic nephrectomy with ex vivo repair and autotransplantation. J Vasc Surg. 2008;48(6):1408–13. doi: 10.1016/j.jvs.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 8.Giulianotti PC, Bianco FM, Addeo P, Lombardi A, Coratti A, Sbrana F. Robot-assisted laparoscopic repair of renal artery aneurysms. J Vasc Surg. 2010;51(4):842–9. doi: 10.1016/j.jvs.2009.10.104. [DOI] [PubMed] [Google Scholar]
- 9.Hislop SJ, Patel SA, Abt PL, Singh MJ, Illig KA. Therapy of renal artery aneurysms in New York State: outcomes of patients undergoing open and endovascular repair. Annals of vascular surgery. 2009;23(2):194–200. doi: 10.1016/j.avsg.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Abath C, Andrade G, Cavalcanti D, Brito N, Marques R. Complex renal artery aneurysms: liquids or coils? Techniques in vascular and interventional radiology. 2007;10(4):299–307. doi: 10.1053/j.tvir.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 11.Cohen JR, Shamash FS. Ruptured renal artery aneurysms during pregnancy. J Vasc Surg. 1987;6(1):51–9. doi: 10.1067/mva.1987.avs0060051. [DOI] [PubMed] [Google Scholar]
- 12.Hidai H, Kinoshita Y, Murayama T, Miyai K, Matsumoto A, Ide K, et al. Rupture of renal artery aneurysm. European urology. 1985;11(4):249–53. doi: 10.1159/000472507. [DOI] [PubMed] [Google Scholar]
- 13.Hupp T, Allenberg JR, Post K, Roeren T, Meier M, Clorius JH. Renal artery aneurysm: surgical indications and results. European journal of vascular surgery. 1992;6(5):477–86. doi: 10.1016/s0950-821x(05)80620-6. [DOI] [PubMed] [Google Scholar]
- 14.Martin RS, 3rd, Meacham PW, Ditesheim JA, Mulherin JL, Jr, Edwards WH. Renal artery aneurysm: selective treatment for hypertension and prevention of rupture. J Vasc Surg. 1989;9(1):26–34. [PubMed] [Google Scholar]
- 15.Sorcini A, Libertino JA. Vascular reconstruction in urology. The Urologic clinics of North America. 1999;26(1):219–34. x–xi. doi: 10.1016/s0094-0143(99)80018-4. [DOI] [PubMed] [Google Scholar]
- 16.Robinson WP, 3rd, Bafford R, Belkin M, Menard MT. Favorable outcomes with in situ techniques for surgical repair of complex renal artery aneurysms. J Vasc Surg. 2011;53(3):684–91. doi: 10.1016/j.jvs.2010.10.050. [DOI] [PubMed] [Google Scholar]
- 17.Bui BT, Oliva VL, Leclerc G, Courteau M, Harel C, Plante R, et al. Renal artery aneurysm: treatment with percutaneous placement of a stent-graft. Radiology. 1995;195(1):181–2. doi: 10.1148/radiology.195.1.7892464. [DOI] [PubMed] [Google Scholar]
- 18.Dib M, Sedat J, Raffaelli C, Petit I, Robertson WG, Jaeger P. Endovascular treatment of a wide-neck renal artery bifurcation aneurysm. Journal of vascular and interventional radiology: JVIR. 2003;14(11):1461–4. doi: 10.1097/01.rvi.0000096765.74047.68. [DOI] [PubMed] [Google Scholar]
- 19.Tateno T, Kubota Y, Sasagawa I, Sawamura T, Nakada T. Successful embolization of a renal artery aneurysm with preservation of renal blood flow. International urology and nephrology. 1996;28(3):283–7. doi: 10.1007/BF02550487. [DOI] [PubMed] [Google Scholar]
- 20.Klein GE, Szolar DH, Breinl E, Raith J, Schreyer HH. Endovascular treatment of renal artery aneurysms with conventional non-detachable microcoils and Guglielmi detachable coils. British journal of urology. 1997;79(6):852–60. doi: 10.1046/j.1464-410x.1997.00157.x. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Z, Yang M, Song L, Tong X, Zou Y. Endovascular treatment of renal artery aneurysms and renal arteriovenous fistulas. J Vasc Surg. 2013;57(3):765–70. doi: 10.1016/j.jvs.2012.09.042. [DOI] [PubMed] [Google Scholar]
- 22.Tsilimparis N, Reeves JG, Dayama A, Perez SD, Debus ES, Ricotta JJ., 2nd Endovascular vs open repair of renal artery aneurysms: outcomes of repair and long-term renal function. Journal of the American College of Surgeons. 2013;217(2):263–9. doi: 10.1016/j.jamcollsurg.2013.03.021. [DOI] [PubMed] [Google Scholar]
- 23.Klausner JQ, Harlander-Locke MP, Plotnik AN, Lehrman E, DeRubertis BG, Lawrence PF. Current treatment of renal artery aneurysms may be too aggressive. J Vasc Surg. 2014;59(5):1356–61. doi: 10.1016/j.jvs.2013.11.062. [DOI] [PubMed] [Google Scholar]