Abstract
Introduction
The study conducts a cost-effectiveness analysis (CEA) of a continuing care Telephone Monitoring and Counseling (TMC) intervention for adults diagnosed with cocaine dependence. Participants were randomly assigned to a control condition of intensive outpatient treatment only (treatment-as-usual, or TAU; N = 108), or to one of two treatment conditions featuring TMC (N = 106) and TMC plus incentives (TMC-plus; N = 107). Follow-up assessments were conducted over a 2-year period.
Methods
Intervention and client costs were collected with the program and client versions of the Drug Abuse Treatment Cost Analysis Program (DATCAP). Effectiveness was measured as the number of days abstinent during follow-up. Secondary analyses consider alternative measures of effectiveness and the reduced societal costs of physical and mental health problems and criminal justice involvement.
Results
From the societal perspective, TMC dominates both TAU and TMC-plus as a cost-effective and cost-saving intervention. Results varied by substance-using status, however, with the subgroup of participants in TMC-plus that were using drugs at intake and early in treatment having the greatest number of days of abstinence and generating similar savings during follow-up than the TMC subgroup using drugs at intake.
Conclusions
Telephone monitoring and counseling appears to be a cost-effective and potentially cost-saving strategy for reducing substance use among chronic substance users. Providing client incentives added to total intervention costs but did not improve overall effectiveness.
Clinical trial registration
Clinical Trials.gov Number: NCT00685659.
Keywords: Continuing care, Cost-effectiveness analysis, Substance use disorders, Economic evaluation
1. Introduction
Substance use disorders are now commonly viewed as a chronic condition, ranking within the top 10 non-genetic causes of mortality in the United States and comprising more than 5% of the global burden of disease (Degenhardt et al., 2013; Mokdad et al., 2000). In the US alone, substance use disorders generate around $600 billion annually in medical services, crime, and productivity costs (National Institute on Drug Abuse, 2011). Historically, addressing substance use disorders focused on acute episodes of treatment in traditional modalities (e.g., 28-day residential treatment, standard outpatient treatment). The current clinical perspective on treating substance use disorders embraces a chronic disease model in recognition of the fact that for many individuals, multiple treatment episodes are required to achieve long-term recovery (Hser et al., 1997; McKay, 2001; McKay and Hiller-Sturmhöfel, 2011; Dennis and Scott, 2007). As with any chronic disease, the objectives for promoting successful long-term management of substance use disorders feature regular screening, monitoring, and assistance linking with additional care as needed (McKay, 2009; Dennis et al., 2014). Extending treatment and recovery services beyond an initial treatment episode is intuitively appealing from a clinical perspective but also implies long-term costs, creating a need to find both effective and economically viable continuing care strategies for individuals with substance use disorders.
Continuing care is provided in a variety of formats and modalities, including group counseling, individual therapy, telephone counseling, brief checkups, and peer-support meetings, and encompasses both stand-alone interventions and step-down approaches (e.g., from residential to intensive outpatient; McKay, 2009). The literature reports generally mixed evidence of the effectiveness of continuing care (McKay et al., 2005; McKay, 2009; McKay et al., 2013; Godley et al., 2014; Van Horn et al, 2011). However, a recent meta-analysis of 19 studies concluded that, on average, continuing care was more effective than minimal or no continuing care as an extension to formal modalities of treatment (Blodgett et al, 2014). Continuing care approaches that are more adaptive, have longer durations, and use motivational incentives to increase participation in treatment performed better than average (Dennis et al., 2014).
Despite evidence supporting the effectiveness of continuing care protocols in treating substance use disorders, there is limited funding and no formal reimbursement mechanism for many of these services. One major limitation is the scarcity of economic evidence showing the return-on-investment (ROI) of continuing care interventions to rally support among providers, health insurance companies, and Medicare/Medicaid. This study adds to the limited economic data on continuing care for substance use disorders by performing the first cost-effectiveness analysis (CEA) of Telephone Monitoring and Counseling (TMC), a continuing care intervention developed by McKay and colleagues, which seeks to promote long-term recovery while reducing the participation burden among patients (McKay et al., 2010; McKay et al., 2011). The CEA estimates and compares intervention costs and outcomes among three study conditions: TMC, TMC plus incentives (TMC-plus), and treatment as usual (TAU). Multiple analytic perspectives are represented, thus in addition to calculating cost-effectiveness ratios with direct intervention costs, we also take into account client costs as well as societal costs attributable to medical and psychiatric problems, and illegal activity. This study was approved by the University of Pennsylvania and University of Miami Institutional Review Boards.
1.1. Economic studies of continuing care
Recent economic studies of continuing care interventions report mixed results. Godley et al. (2010) evaluated the cost-effectiveness of Motivational Enhancement Therapy/Cognitive Behavior Therapy (MET/CBT), with and without Assertive Continuing Care (ACC) for adolescents and found no statistically significant differences in the incremental effectiveness of ACC following outpatient treatment. Thus, the least expensive option (MET/CBT without ACC) was deemed most cost effective. More supportive evidence is presented in McCollister et al. (2013), which conducted a CEA of Recovery Management Checkups (RMC), a quarterly monitoring and relapse prevention protocol for individuals with substance use disorders. Relative to outcome monitoring only (OM-only), RMC was both cost-effective in reducing substance use and cost saving after factoring in reductions in the costs associated with health care utilization, other social services, unemployment, and criminal activity.
Popovici et al. (2008) conducted a systematic review of published economic studies featuring unique types of continuing care, including step-down from hospital inpatient or residential treatment to outpatient treatment, methadone maintenance, and corrections-based treatment with aftercare. Findings suggest that among the few existing economic studies in this area, the majority of continuing care/aftercare programs appear to be more cost-effective than a single (acute) treatment approaches, but the review also notes several evidence gaps and methodological challenges in this literature. For instance, many of these studies focus on special or priority populations such as criminal offenders, minorities, and women, which limits generalizability of the economic findings to other populations and settings. In addition, the authors note that many of these studies are limited by quasi-experimental designs, short follow-ups, and nonstandard approaches to estimating intervention costs and consequences.
The current study makes an important contribution to the literature on continuing care for substance use disorders and addresses evidence gaps noted in the Popovici et al. (2008) review. The sample includes males and females from an urban setting with cocaine dependence. The study followed individuals over 2 years providing a long-term perspective on the clinical and economic impact of the TMC interventions. Finally, the analysis features multiple perspectives on costs and consequences generating results of interest to providers, patients, and other stakeholders.
2. Data and measures
2.1. Telephone monitoring and counseling (TMC)
Data for the current study come from a randomized trial of TMC for cocaine dependent patients (McKay et al., 2013). TMC consists of telephone-based continuing care counseling sessions in which the counselor uses a cognitive-behavioral approach to monitor substance use, identify relapse risk factors, develop and rehearse coping strategies, and help clients link to community support groups. Results from the trial showed that augmenting an intensive outpatient program (IOP) with TMC produced better substance use outcomes than IOP only, for participants who were actively using cocaine or alcohol when they entered IOP or during the first few weeks of IOP (McKay et al., 2013).
Participants who had been in IOP for 2 weeks were randomly assigned to three study conditions. The control group (TAU) received IOP only, which provided approximately 9 h of group-based treatment per week, and patients could typically attend for up to 3–4 months (McKay et al, 2010). Participants in the TMC conditions had one or two initial face-to-face sessions in the first week of the intervention (which occurred in weeks 3–4 of IOP) and then received brief telephone calls (on average 16.4 min) for up to 24 months. The calls were weekly for the first 2 months, but then tapered to twice monthly for the remainder of the first year, monthly during months 13–18, and every other month for the rest of the second year.
The mean number of continuing care sessions received by participants who completed their orientations was 15.5 (SD = 14.1) in TMC and 26.0 (SD = 12.8) in TMC-plus, F (1, 164) = 26.30, p < 0.0001. The mean duration of sessions was 21.1 min (SD = 13.6) in TMC and 20.1 min (SD = 11.8) in TMC-plus. The percentage of sessions completed in person, as opposed to over the telephone, was 46.4% in TMC and 42.4% in TMC-plus. In person sessions were longer than telephone sessions (25.9 vs. 16.4 min, respectively).
Participants in TMC-plus experienced the same as TMC, with the addition of financial incentives for attending treatment sessions. Participants received a $10 gift coupon for each regularly scheduled or step-care session attended in the first year, and a bonus $10 gift card every time three consecutively scheduled sessions were completed. The gift cards were for department stores and a local grocery store chain (McKay et al., 2013). Additional details on the randomization procedures are provided in McKay et al. (2013).
2.2. Sample characteristics
Participants were recruited from two publicly funded intensive outpatient programs (IOP) in Philadelphia. A total of 773 individuals were screened for the study. Of these, 321 met criteria for lifetime cocaine dependence, reported using cocaine in 6 months prior to entering the study, and were willing to participate in research (McKay et al., 2013). The participants were on average 43 years old and had 11.3 years of education. The majority of participants were male (76%) and African American (89%). Thirty-four percent of participants reported using alcohol at least one time in the 30 days preceding the baseline interview (a period that included the first 3 weeks of IOP), and 42% reported using cocaine at least one time during this period. Table 1 is adapted from McKay et al. (2013) and summarizes selected sample characteristics at baseline by study condition.
Table 1.
Sample Characteristics at Baseline
| Variable | TAU (N = 108) | TMC (N = 106) | TMC-plus (N = 107) |
|---|---|---|---|
| Demographics | |||
| Race | |||
| African American (%) | 90.7 | 84.0 | 91.6 |
| White (%) | 7.5 | 9.4 | 5.6 |
| Other (%) | 1.9 | 6.6 | 2.8 |
| Gender (%male) | 75.9 | 75.5 | 77.6 |
| Age | 42.9 (8.0) | 43.3 (7.8) | 43.4 (6.48) |
| Education | 11.4 (1.9) | 11.8 (1.6) | 11.5 (1.8) |
| Ever married (%) | 38.9 | 41.5 | 38.3 |
| Substance use | |||
| Prior treatments for substance use | 4.4 (5.2) | 4.4 (5.7) | 4.6 (5.9) |
| Years of regular cocaine use | 14.9 (7.6) | 14.3 (7.7) | 15.9 (7.4) |
| Years of regular alcohol use | 13.7 (11.1) | 14.0 (11.0) | 16.6 (11.5) |
Adapted from Table 1 in McKay et al., (2013). Standard deviations in parentheses. No significant differences were noted on any of the sample characteristics at baseline.
3. Methods
The cost-effectiveness analysis of TMC encompasses three analytic perspectives: the provider, the client, and society. The cost analysis was conducted using primary data on intervention costs and client costs. Cost data are reported in 2008 dollars reflecting the midpoint in the TMC trial when service delivery was steady. Sensitivity analyses were conducted to examine and compare the societal costs associated with medical and psychiatric problems and illegal activity (including incarceration), which represents a broader perspective on the economic impact of TMC. Finally, we conduct secondary cost-effectiveness analyses using alternative measures of abstinence that were featured in the Main Findings studies from the TMC trial.
3.1. Cost analysis
3.1.1. Intervention costs
Intervention cost data were collected with the Drug Abuse Treatment Cost Analysis Program (DATCAP; French, 2003; www.datcap.com). The DATCAP is a program-level data collection instrument designed to collect and organize detailed information on resources used in service delivery and their associated costs. Resource categories include personnel, supplies and materials, contracted services, buildings and facilities, equipment, and miscellaneous items (e.g., food, telephone charges). In addition to estimating total annual intervention costs, the average cost per session was calculated by dividing total annual cost by total sessions attended by intervention participants. For individual-level treatment episode costs, the average cost per session was multiplied by the unique number of sessions attended by each participant.
3.1.2. Client costs
The Client DATCAP instrument was developed to broaden the evaluation perspective of the Program DATCAP by measuring costs incurred by treatment clients, an important but often-unmeasured opportunity cost of addiction treatment. Client costs were comprised of the opportunity cost of time invested to travel to and attend a counseling session in person, or the time spent receiving scheduled monitoring and counseling over the phone. Transportation costs and other expenditures (e.g., child care) were included in total client costs. The Client DATCAP was administered to participants by research staff. The survey takes about 10–20 min to complete. Clients are asked to reflect on time and expenditures during the average week of treatment, which can then be translated into a total client cost per episode by multiplying average client costs per week by the number of weeks actively participating in the intervention.
3.1.3. Societal costs
Apart from the main intervention/client cost analysis, we also examined the reductions in societal costs using baseline and follow-up data collected with the Addiction Severity Index (ASI; McLellan et al, 1980). Societal costs are reported for each study condition (overall), and for two subgroups of TMC/TMC-plus participants: (i) participants that were using substances at intake and continued using early in treatment, and (ii) participants not using at intake/early in treatment. A total of four measures were analyzed: days experiencing medical problems, days experiencing psychiatric problems, days in jail, and days of illegal activity. We compared the four measures at baseline and each follow-up point, and the differences in these outcomes were then converted into dollar values using monetary conversion factors developed by French and colleagues (French et al, 2002a; French et al, 2002b). Based on these four measures, we calculated the reduction in societal costs over the 24-month follow-up period.
3.1.4. Outcomes
The primary measure of effectiveness is the number of days abstinent during follow-up, collected with the ASI. At each follow-up point, clients were asked to recount the total days of substance use (across 11 different substances) during the 30 days prior to the assessment. The majority of clients reported polysubstance use so the most frequently reported substance was selected to determine total abstinence days. For instance, if a client reported 12 days of alcohol use and 3 days of cocaine use, total abstinence for the month is recorded as 18 days (12 days of most frequent substance use, subtracted from 30) regardless of how often these substances may have been used separately or on the same day. To translate 30-day use reported at each assessment to cover the 3-month timeframe between assessments, we multiplied the estimated past-30 days abstinent by 3 (or by 6 at the 18- and 24-month assessments). Total days abstinent, therefore, represents the sum of the number of days participants reported not using any alcohol or other drugs over the 24-month follow-up, with a possible range of 0–720 days.
We also conducted a sensitivity analysis using alternative measures of abstinence that were the primary outcomes featured in the Main Findings papers from the trial (McKay et al., 2013). Results from the main trial focused on self-reported cocaine and alcohol use and urine toxicology screens over the 24-month follow-up period. At each follow-up point, Time-Line Follow-Back (TLFB) calendar assessment techniques were used to gather substance use during the preceding 3 or 6 months (depending on which follow-up assessment). Urine samples were also requested at each follow-up point to provide a more objective measure of cocaine use. For participants that agreed to provide a sample for the urine toxicology screen and reported no substance use on the TLFB, their self-reported abstinence was confirmed or denied by the results of the drug test. Anyone with a positive drug screen was also categorized as non-abstinent for that assessment period. Based on self-reported substance use and urine toxicology results at all six follow-up points, we calculated the percentage of time participants were abstinent over the entire 24 months.
These measures are less tenable for a cost-effectiveness analysis, as they make the interpretation of results more challenging. For instance, a dichotomous outcome like “abstinence vs. any use” will produce a cost-effectiveness ratio that describes the “cost to achieve a one percentage point increase in abstinence.” Because CEA ultimately tries to connect results to the societal willingness to pay per unit of outcome (in this case abstinence), it is more cumbersome to interpret society’s willingness to pay per increased percent abstinent versus society’s willingness to pay for a full day of abstinence. For this reason we present this as a secondary cost-effectiveness analysis and focus instead on days of abstinence as the primary measure of effectiveness.
3.2. Cost-effectiveness analysis
Cost-effectiveness analysis is a common approach to conducting a full economic evaluation where both the costs and the consequences of treatments are examined (Drummond et al., 2005; Gold et al., 1996). It is particularly useful for determining the costs among competing programs to achieve a desired clinical outcome such as reduced days of substance use, which is often difficult to translate into a monetary equivalent (McCollister et al., 2013). The difference in intervention costs is divided by the difference in effectiveness to calculate an incremental cost-effectiveness ratio (ICER):
| (1) |
Eq. (1) shows the calculation of the ICER, where IC is the incremental cost of TMC relative to TAU and IE is the incremental effectiveness of TMC relative to TAU. The ICER describes the additional cost of TMC relative to TAU to achieve an additional day of abstinence. These “cost-per-outcome” metrics provide a sense of the return-on-investment in one treatment approach relative to another, and are intended to offer empirical guidance for making more efficient (socially optimal) resource allocation decisions.
Two sets of CEAs were conducted for the primary analysis. The first CEA considers only direct intervention costs in calculating the incremental cost per day abstinent in TMC/TMC-plus relative to TAU, and in TMC-plus relative to TMC. The second CEA factors in client and other societal costs such that the calculation of incremental costs is equal to direct intervention costs plus client costs, minus any savings resulting from reduced medical/psychiatric problems, illegal activity, and incarceration. Incorporating societal costs serves as a sensitivity analysis allowing us to examine how results of the CEA change when costs in these other areas are added to the direct intervention costs.
3.2.1. Cost-effectiveness acceptability curve (CEAC)
The process of calculating the ICER is relatively straightforward, but there remains some degree of uncertainty associated with this ratio due to the typically skewed distributions of costs and outcomes (i.e., sampling variability) (Briggs and Gray, 1999). In addition to these statistical issues, we do not know how society values increased abstinence, which would establish a willingness-to-pay (WTP) threshold. However, we can project a value or range of values for WTP per unit of outcome to interpret the ICER in terms of net benefit (NB) and incremental net benefit (INB). For instance, if society values a day of abstinence at $100, the NB of each study condition is the number of days abstinent over follow-up multiplied by $100 minus intervention costs. The INB is simply the difference in NB between study conditions (Stinnett and Mullahy, 1998).
To address the uncertainty surrounding the ICER (a point estimate), non-parametric bootstrap methods are used to produce 1000 replicates of mean costs and effects; each one generating unique ICER, NB, and INB estimates. Based on those 1000 replicates, the proportion for which TMC or TMC-plus generate a positive INB over the range of potential WTP values is used to plot a cost-effectiveness acceptability curve (CEAC). The CEAC represents the likelihood that TMC/TMC-plus is cost-effective as compared to TAU over a range of WTP values. Therefore, although it is not known what society will pay for one more day of abstinence, the CEAC illustrates how likely TMC/TMC-plus is to be cost-effective relative to TAU over a range of WTP values.
4. Results
4.1. Cost analyses
All participants (TAU, TMC, and TMC-plus) received intensive outpatient treatment (IOP), which cost $1764 for the average treatment episode (approximately $138 per week). Table 2 shows total annual intervention costs as well as cost per episode for each treatment condition. Based on the patient caseflow in the main trial, it cost a total of $49,632 annually to deliver TMC (to all participants), and $66,564 annually to deliver TMC-plus (to all participants). Because TMC-plus participants attended more sessions than TMC, the average cost per TMC-plus session is lower than the average cost per TMC session. The average cost per episode, however, was greater for the TMC-plus group ($561) relative to the TMC group ($342). The additional cost per episode of TMC-plus was mainly driven by the additional number of sessions attended by participants in this group and by the incentives.
Table 2.
TMC and TMC-plus intervention cost analyses (2008 dollars).
| Intervention costs | Summary cost, TMC (N = 106) | Summary cost, TMC-plus (N = 107) |
|---|---|---|
| Personnel | $41,216 | $41,216 |
| Buildings/facilities | $5292 | $5292 |
| Equipment | $1800 | $1800 |
| Supplies/miscellaneous | $1324 | $1324 |
| Additional staff time | $3632 | |
| Client incentives | $13,300 | |
| Total annual intervention cost | $49,632 | $66,564 |
| Cost per sessiona | $30.55 | $26.83 |
| Average cost per episode | $342 (41.52) | $561 (39.66) |
Notes: All study participants received IOP treatment. The average cost of IOP treatment was $1764 per treatment episode or approximately $138 per week. Cost data collected with the Drug Abuse Treatment Cost Analysis Program (DATCAP). Standard deviations in parentheses.
Cost per session is based on N = 1623 sessions delivered in TMC and N = 2496 sessions delivered in TMC-plus.
Table 3 presents the client costs associated with TMC and TMC-plus. In addition to the time clients spent receiving intervention services, they reported out-of-pocket travel expenses for in-person sessions. Results are summarized “per contact” and also over the duration of the intervention (i.e., client costs per episode). The opportunity cost of a client’s time was the largest cost, averaging $25.53 (intervention plus travel time) for TMC and $27.45 for TMC-plus per session. The total TMC client cost per contact was $30.24, and $31.94 for TMC-plus. Over the duration of the intervention TMC clients incurred $734 in time and travel costs and TMC-plus clients incurred $1015 in time and travel costs.
Table 3.
Client costs for TMC and TMC-plus in 2008 dollars.
| TMC (N = 70) | TMC-plus (N = 88) | |
|---|---|---|
| Client costs per contact | ||
| Opportunity cost of time in intervention | 16.95 (7.29) [16.13] |
17.97 (8.08) [16.55] |
| Opportunity cost of travel time | 8.58 (6.35) [9.17] |
9.48 (6.54) [8.79] |
| Additional travel costs | 3.47 (1.97) [4.00] |
3.46 (1.68) [4.00] |
| Total client cost | 30.24 (13.46) [27.75] |
31.94 (14.25) [30.73] |
| Client costs per episode | ||
| Opportunity cost of time in intervention | 343 (348.9) [284] |
531 (415) [480] |
| Opportunity cost of travel time | 216 (288) [130] |
295 (282) [256] |
| Additional travel costs | 80.77 (70.9) [60.24] |
103 (67.6) [106] |
| Total client cost | 734 (691) [596] |
1015 (736) [926] |
Notes: Standard deviations in parentheses. Median estimates in brackets. Total number of contacts includes orientations and regular counseling sessions (conducted either via phone or in person). Core sample was N = 158 (TMAC = 70; TMC-plus = 88), but sample sizes vary for client cost categories due to missing data. Where possible, missing values were imputed using sample averages and/or supplementary data. For example, missing hourly wage data was imputed using the federal minimum wage in 2008 ($7.25).
Table 4 shows the reduction in societal costs and net savings over the 24-month follow-up associated with reductions in days of illegal activity, days experiencing medical problems, days experiencing psychiatric problems, and days in jail. Overall, TMC generated the greatest savings (i.e., reductions in societal costs of $1564 on average), driven largely by the subgroup that was using alcohol and/or cocaine at intake ($2780 on average). The TAU group and TMC-plus group actually increased societal costs over the follow-up period (−$1545 and −$191 on average, respectively), driven largely by the subgroup that was not using alcohol/or cocaine at intake (−$2813 and −$2380 on average, respectively). For the TMC group, net savings remained positive after considering both intervention and client costs. However, it is noteworthy that the TMC-plus subgroup using alcohol and/or cocaine at intake had positive total ($2679) and net savings ($2138 from provider perspective, and $1343 from societal perspective).
Table 4.
Societal costs.
| Treatment Condition | Reduction in societal costs over 24-month follow-up ($) | Net savings from provider perspective (savings minus intervention costs) | Net savings from societal perspective (savings minus intervention plus client costs) |
|---|---|---|---|
| TMC (N = 106) | 1564 (10,997) | 1222 (11,000) | 838 (11,018) |
| Subgroup using alcohol and/or cocaine (N = 42) | 2780 (15,377) | 2396 (15,415) | 1921 (15,447) |
| Subgroup not using alcohol and/or cocaine (N = 64) | 734(6551) | 420 (6506) | 98.6 (6527) |
| TMC-plus (N = 107) | −191 (20,514) | −750 (20,477) | −1497 (20,414) |
| Subgroup using alcohol and/or cocaine (N = 47) | 2679 (9064) | 2138 (9026) | 1343 (8879) |
| Subgroup not using alcohol and/or cocaine (N = 60) | −2380 (25,958) | −2952 (25,912) | −3663 (25,869) |
| TAU (N = 108) | −1545 (23,195) | −1545 (23,195) | −1545 (23,195) |
| Subgroup using alcohol and/or cocaine (N = 54) | −325 (17,962) | −325 (17,962) | −325 (17,962) |
| Subgroup not using alcohol and/or cocaine (N = 54) | −2813 (27,748) | −2813 (27,748) | −2813 (27,748) |
Notes: Cost estimates presented in 2008 dollars. Standard deviations are in parentheses. Reductions in societal costs (i.e., total savings) were calculated as the monetary value of reductions in days of illegal activity, days experiencing medical problems, days experiencing psychiatric problems, and days in jail captured with the Addiction Severity Index (ASI). Net savings were calculated by subtracting intervention costs (with and without client costs) from total savings. The societal cost per day experiencing medical problems is $25.25; per day experiencing psychiatric problems is $10.22; per day engaging in illegal activity is $998.41; and per day incarcerated is $60.35.
4.2. Cost-effectiveness analysis
Table 5 shows the results of the CEA for total days of abstinence. The top half of the table shows the direct intervention cost, broader societal costs (intervention plus client costs, savings to health and criminal justice systems) and days abstinent during follow-up. The bottom half of Table 5 presents the incremental cost-effectiveness analysis for three comparisons. First, relative to TAU, the incremental cost of TMC was $342 and this group had 18.4 more days abstinent over follow-up. Thus, the incremental cost-effectiveness ratio (ICER) for TMC relative to TAU was $18.6 per additional day of abstinence. The incremental cost of TMC-plus relative to TAU was $561, with an incremental effectiveness of 4.2 more days of abstinence. Therefore, the ICER for TMC-plus relative to TAU was $133 per additional day of abstinence. In comparing the two intervention groups, TMC cost less and generated more days of abstinence than TMC-plus, and therefore dominates TMC-plus in terms of cost-effectiveness. When the societal costs are applied to the CEA instead, TAU is dominated by both TMC and TMC-plus, mainly because TAU did not generate any savings over the follow-up period. TMC-plus is still dominated by TMC.
Table 5.
Cost-effectiveness analysis—days of abstinence.
| Treatment Condition | Intervention Cost ($) | Societal cost (intervention plus client costs minus savings) ($) | Days abstinent during follow-up |
|---|---|---|---|
| TAU (N = 108) | 0 | 1545 (23,195) | 590 (201) |
| TMC (N = 106) | 342 (41.52) | −838 (11,018) | 609 (180) |
| TMC-plus (N = 107) | 561 (39.66) | 1497 (20,414) | 595 (184) |
| Cost-effectiveness comparison | Incremental intervention cost ($) | Incremental societal cost ($) | Incremental days abstinent | ICER with intervention cost | ICER with societal cost |
|---|---|---|---|---|---|
| TMC vs. TAU | 342 [257, 426] | −2,383 [−8,435, 1,565] | 18.4 [−39.1, 65.5] | 18.6 [4.32, 1030] | N/A (TMC dominates) |
| TMC-plus vs. TAU | 561 [488, 639] | −47.6 [−5,961, 6,573] | 4.23 [−45.7, 53.9] | 133 [61.5, 33,959] | N/A (TMC-plus dominates) |
| TMC-plus vs. TMC | 219 [103, 329] | 2335 [−1260, 8132] | −14.2 [−62.1, 32.9] | N/A (TMC dominates) | N/A (TMC dominates) |
Notes: Standard deviations in parentheses. Bootstrapped confidence intervals in brackets.
Fig. 1 shows the CEACs for days of abstinence for both TMC and TMC-plus. The vertical axis shows the probability that TMC or TMC-plus is cost-effective relative to TAU. The horizontal axis indicates a range of potential societal willingness-to-pay (WTP) values per day of abstinence between $0 and $100. TMC has a high likelihood of being cost-effective at a relatively low WTP per day of abstinence. If society values a day of abstinence at $30, the probability that TMC is cost-effective approximates 60%. At $80, the probability approaches 80%. TMC-plus however, has a very low probability of being cost-effective across a wide range of WTP per day of abstinence. Even at a WTP of $100 per day of abstinence, the probability that TMC-plus will be cost effective relative to TAU is only around 50%.
Fig. 1.
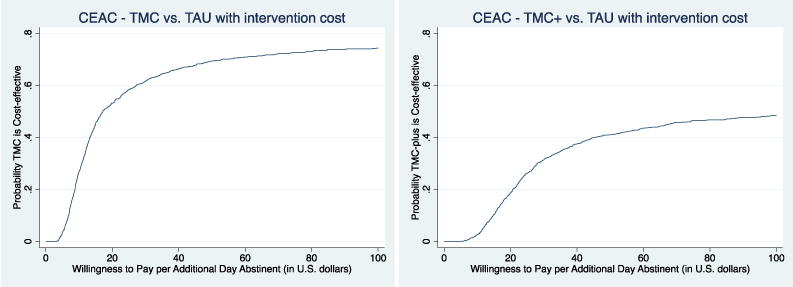
Cost-effectiveness acceptability curve (CEAC) for abstinence.
4.3. Secondary CEA analyses
A secondary CEA was conducted using self-reported cocaine and alcohol use and urine toxicology results as alternative effectiveness measures. For self-reported cocaine and alcohol use, only TMC had greater abstinence than TAU (2.37% greater) generating an incremental cost-effectiveness ratio of $196 per one percent increase in abstinence in TMC relative to TAU. TMC-plus was dominated by both TMC and TAU. Both TMC and TMC-plus had fewer positive urine toxicology screens than TAU, generating ICERS of $109 (TMC vs. TAU) and $223 (TMC-plus vs. TAU) per percent decrease in positive urine toxicology screens. As with the other analyses, TMC cost less and generated fewer positive urine toxicology screens than TMC-plus.
5. Discussion
The study evaluated the cost-effectiveness of TMC with and without incentives as a continuing care protocol for individuals with substance use disorders, diagnosed with cocaine dependence. Results suggest that, for the average client, TMC is a cost-effective strategy for reducing substance use, particularly if society is willing to pay more than $30 per day of abstinence. TMC-plus on the other hand, is only cost-effective relative to TAU at a very high WTP threshold and is dominated by TMC in terms of intervention costs and days abstinent.
The results are reinforced by the societal cost analysis, which indicates TMC to be generating the greatest reduction in societal costs overall ($1564 on average). The net savings for TMC remain positive even after factoring in direct intervention costs and client expenditures. However, the TMC-plus subgroup using alcohol and/or cocaine at intake also had very high total ($2679) and net savings ($2138 from provider perspective, and $1343 from societal perspective). This finding illustrates the fact that, from an economic perspective, there is value to screening treatment-seeking individuals with substance use disorders for current use at intake and carefully monitoring use early in treatment. Information from these assessments could be used to identify higher-risk individuals who are more likely to require more extensive and expensive interventions like TMC-plus in order to have good outcomes over longer periods of time. The results of this study suggest that for such individuals, the added costs of the more expensive continuing care intervention will be more than offset by increased societal benefit. Within health care, there is an increasing focus on personalizing treatment protocols to optimize outcomes while reducing costs (Kranzler and McKay, 2012). Further research is needed to more fully determine effective and efficient treatment regimens for subgroups of individuals with substance use disorders, including those who do not respond well to the initial treatment provided.
5.1. Limitations
Results should be interpreted with the following limitations in mind. First, we had missing data on some outcomes. Across the full sample, 9–30% of the observations on “self-reported cocaine and alcohol use and urine toxicology screens” at each follow-up point were missing and this varied by study condition and follow-up point. The four ASI measures used to calculate societal costs had 1–2% missing, which did not vary by study condition. We used a multiple imputation procedure to fill in missing values for these measures.
Second, although variables from the ASI have been used in benefit-cost analyses before, these aggregated measures of health problems or illicit behavior are less precise for estimating societal costs than data on actual service utilization (e.g., times in the emergency department, number of inpatient hospital days, number of group counseling sessions) or counts of the frequency and types of criminal offenses being committed (e.g., times committing a robbery, times stealing a motor vehicle). Thus, the estimates of societal costs here likely underrepresent the cost-savings generated by the intervention.
Third, although we look descriptively at the differences in societal costs among TMC and TMC-plus subgroups (Table 4), such analyses are subject to potential biases associated with self-selection, absence of a pure control condition, and unobserved individual heterogeneity. Still, we believe it is worth noting that the economic analyses of the higher risk TMC and TMC-plus subgroups support the findings in the clinical trial in that the subgroup of TMC-plus participants that had higher cocaine and alcohol use at intake and early in treatment had greater reductions in substance use over follow-up and generated the greatest reductions in societal costs relative to all other groups.
6. Conclusion
The results of this study support TMC as a cost-effective and potentially cost-saving continuing care intervention for individuals with substance use disorders. The cost per additional day of abstinence ($18.6) is relatively low—especially when considering that abstinence is linked to a number of positive outcomes such as increased productivity, greater family stability, less criminal activity and incarceration, and less unnecessary health services utilization. Providing financial incentives to clients does not pay-off in this setting, although this raises a question regarding the extent to which providers can identify higher risk patients and effectively direct these patients to alternative (i.e., more intensive or featuring incentives) forms of extended care. More costly protocols may be warranted for certain categories of patients and may prove to be more cost-effective and cost saving for society at large.
Acknowledgments
Role of funding source
Financial assistance for this study was provided by the National Institute on Drug Abuse (NIDA; grant numbers R01 DA020623 & R01 DA031785). The funding sources had no involvement in the study design, in the collection, analysis and interpretation of the data, in the writing of the report, or in the decision to submit the article for publication.
Footnotes
Contributors
All authors contributed to the design and execution of this study. Intervention and client cost data were collected by Dr. McCollister with the assistance of Dr. McKay’s research staff. Outcome data were provided by Dr. McKay and come from the main clinical trial. Analyses of data and the manuscript draft were produced by Ms. Yang under the direction of Dr. McCollister, and all authors contributed to and have approved the final manuscript.
Conflict of interest
No conflict declared.
References
- Blodgett JC, Maisel NC, Fuh IL, Wilbourne PL, Finney JW. How effective is continuing care for substance use disorders? A meta-analytic review. J Subst Abuse Treat. 2014;46:87–97. doi: 10.1016/j.jsat.2013.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs AH, Gray AM. Handling uncertainty when performing economic evaluation of healthcare interventions. Health Technol Assess. 1999;3:1–134. [PubMed] [Google Scholar]
- Degenhardt L, Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Hall WD, Freedman G, Burstein R, Johns N, Engell RE, Flaxman A, Murray CJ, Vos T. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1564–1574. doi: 10.1016/S0140-6736(13)61530-5. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK. Managing addiction as a chronic condition. Addict Sci Clin Pract. 2007;4:45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Laudet A. Beyond bricks and mortar: recent research on substance use disorder recovery management. Curr Psychiatry Rep. 2014;16:1–7. doi: 10.1007/s11920-014-0442-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. 3rd. Oxford University Press; New York: 2005. [Google Scholar]
- French MT. Drug Abuse Treatment Cost Analysis Program (DATCAP): Program Version. 8th. University of Miami; Coral Gables: 2003. Available at www.DATCAP.com. [Google Scholar]
- French MT, McCollister KE, Sacks S, McKendrick K, DeLeon G. Benefit-cost analysis of a modified therapeutic community for mentally ill chemical abusers. Eval Prog Plan. 2002a;25:137–148. [Google Scholar]
- French MT, Salomé HJ, Carney M. Using the DATCAP and ASI to estimate the costs and benefits of residential addiction treatment in the State of Washington. Soc Sci Med. 2002b;55:2267–2282. doi: 10.1016/s0277-9536(02)00060-6. [DOI] [PubMed] [Google Scholar]
- Godley SH, Garner BR, Passetti LI, Funk RR, Dennis ML, Godley MD. Adolescent outpatient treatment and continuing care: main findings from a randomized clinical trial. Drug Alcohol Depend. 2010;110:44–54. doi: 10.1016/j.drugalcdep.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL, Petry NM. A randomized trial of assertive continuing care and contingency management for adolescents with substance use disorders. J Consult Clin Psychol. 2014;82:40–51. doi: 10.1037/a0035264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-effectiveness in Health and Medicine. Oxford University Press; New York: 1996. [Google Scholar]
- Hser YI, Anglin DM, Grella C, Longshore D, Prendergast ML. Drug treatment careers: a conceptual framework and existing research findings. J Subst Abuse Treat. 1997;14:543–558. doi: 10.1016/s0740-5472(97)00016-0. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, McKay JR. Personalized treatment of alcohol dependence. Curr Psychiatry Rep. 2012;14:486–493. doi: 10.1007/s11920-012-0296-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCollister KE, French MT, Freitas DM, Dennis ML, Scott CK, Funk RR. Cost-effectiveness analysis of Recovery Management Checkups (RMC) for adults with chronic substance use disorders: evidence from a 4-year randomized trial. Addiction. 2013;108:2166–2174. doi: 10.1111/add.12335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR. Effectiveness of continuing care interventions for substance abusers implications for the study of long-term treatment effects. Eval Rev. 2001;25:211–232. doi: 10.1177/0193841X0102500205. [DOI] [PubMed] [Google Scholar]
- McKay JR. Continuing care research: what we have learned and where we are going. J Subst Abuse Treat. 2009;36:131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24-month outcomes. Arch Gen Psychiatry. 2005;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- McKay JR, Van Horn DHA, Lynch KG, Ivey M, Cary MS, Drapkin ML, Coviello DM, Plebani JG. An adaptive approach for identifying cocaine dependent patients who benefit from extended continuing care. J Consult Clin Psychol. 2013;81:1063–1073. doi: 10.1037/a0034265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Van Horn DHA, Oslin DW, Ivey M, Drapkin ML, Coviello DM, Yu Q, Lynch KG. Extended telephone-based continuing care for alcohol dependence: 24-month outcomes and subgroup analyses. Addiction. 2011;106:1760–1769. doi: 10.1111/j.1360-0443.2011.03483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Hiller-Sturmhöfel S. Treating alcoholism as a chronic disease. Approaches to long-term continuing care. Alcohol Res. 2011;33:356–370. [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Van Horn DHA, Oslin DW, Lynch KG, Ivey M, Ward K, Drapkin ML, Becher JR, Coviello DM. A randomized trial of extended telephone-based continuing care for alcohol dependence: within-treatment substance use outcomes. J Consult Clin Psychol. 2010;78:912–923. doi: 10.1037/a0020700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. J Nerv Ment Dis. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States. JAMA. 2000;291:238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Understanding Drug Abuse and Addiction. Bethesda, MD: 2011. [Google Scholar]
- Popovici I, French MT, McKay JR. Economic evaluation of continuing care interventions in the treatment of substance abuse: recommendations for future research. Eval Rev. 2008;32:547–568. doi: 10.1177/0193841X08316311. [DOI] [PubMed] [Google Scholar]
- Stinnett AA, Mullahy J. Net Health Benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making. 1998;18(Suppl):S68–S80. doi: 10.1177/0272989X98018002S09. [DOI] [PubMed] [Google Scholar]
- Van Horn DHA, Drapkin ML, Ivey M, Thomas T, Domis SW, Abdalla O, Herd D, McKay JR. Voucher incentives increase treatment participation in telephone-based continuing care for cocaine dependence. Drug Alcohol Depend. 2011;114:225–228. doi: 10.1016/j.drugalcdep.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


