Abstract
Background
Tree stand falls are the most common injury to hunters in the USA, but there is limited research on the topic. This study examined the 5-year trends in incident tree stand fall injuries in rural north-central Wisconsin and described patient demographics and injury features.
Methods
A retrospective analysis was conducted on five prior hunting seasons, 2009–2013. Cases were ascertained from electronic health records via natural language processing that identified patients from the Marshfield Epidemiologic Study Area who received medical attention for a tree stand fall. Annual incidence rates were calculated using the number of hunting license holders in the target population, per administrative data from the Wisconsin Department of Natural Resources.
Results
There were 16,556–16,902 deer hunters in any given year, with 39 (92% male) confirmed medically-attended tree stand fall injuries in 2009–2013. Injuries mainly occurred in the lower extremities (n=23), and included two fatalities and one paralysis case. The risk of tree stand fall injuries went from 6.0 (95% CI: 3.2, 11.1) per 10,000 hunters in 2009 to 3.6 (95% CI: 1.6, 7.9) per 10,000 hunters in 2013, which was not a significant change over five years (p=0.79). Most falls occurred among archery hunters, in the evening and when descending from a tree stand. Cases were demographically similar to the general population of Wisconsin deer hunters.
Conclusions
The current seasonal incidence rate of tree stand fall injuries is relatively low in rural Wisconsin, but with limited signs of improvement. Continued efforts are needed to promote the long-term safety of the hunting public.
Keywords: Hunters, Falls, Injuries, Epidemiology
Introduction
Whitetail deer hunting is a popular autumn recreational activity across much of the U.S. and Canada. Deer hunting is generally a safe sport, but hunting accidents and injuries occur each year and some are very serious, including paralysis, traumatic brain injury, or death. Perhaps unknown or underappreciated by the general public, firearm accidents are increasingly rare among hunters today, presumably due to widespread hunter safety training. Falls from elevated platforms, 10–30 feet off the ground and usually connected to trees (i.e., tree stands), are now the most common form of injury to whitetail deer hunters (1–3). Surveys have estimated that, over a 10-year timeframe, 7 of every 100 deer hunters who use tree stands will fall (4). Over a lifetime, that risk may rise to as high as one in three (5). The impact from a tree stand fall can be up to 30 miles per hour, and the typical patient treated in a hospital for such injuries is a middle-aged male who fell from a height of about 15 feet and suffered multiple musculoskeletal injuries such as extremity fractures, truncal lacerations, and/or acute sprains (6).
From a public health perspective, injuries from tree stand falls are of particular concern in areas with the strongest traditions of whitetail deer hunting because they tend to have the greatest number of individuals at-risk. The state of Wisconsin (USA) has one of the largest such populations with over one-half million residents participating in the annual deer hunting season, which includes about 10% of the state’s total population (7). Rigorous scientific research on the topic of tree stand falls is scarce, but a 2008 study in Wisconsin found that about two-thirds of all hunting-related injuries presented to a Level-I trauma center, including all trauma center deaths, were due to falls from tree stands (1). Time trends from both Pennsylvania (8) and Ohio (2) trauma registries suggest an increasing number of serious tree stand injuries among hunters over the previous decade, likely reflecting the growing popularity of hunting from tree stands, which most whitetail deer hunters now do (4, 6). But previous investigations of tree stand falls have relied almost exclusively on registry data from specialized trauma or spinal care centers, or were limited to select periods of the hunting season (e.g., firearms season only). Such methods tend to underestimate the risk of tree stand falls (6, 9) because off-peak or non-acute injuries are not captured.
Tree stand falls are preventable, but they are rarely subject to injury surveillance. In order to determine recent trends in tree stand falls and potentially improve hunter safety, better epidemiologic information is needed beyond specialized trauma environments or dated surveys. The widespread adoption of electronic health records (EHR) by healthcare delivery systems presents opportunities to reuse clinical data for population-based research (10, 11). Such methods have not been applied to examine hunter safety trends in a defined population beyond trauma registries, but Marshfield Clinic’s EHR data repository presents a unique prospect to study the epidemiology of tree stand fall injuries due to several key regional features. Notably, the Marshfield Clinic healthcare system captures nearly all medical encounters of residents in central and northern Wisconsin, an area where deer hunting remains very popular, with a large whitetail deer population and deer hunter density ratios likely among the highest in the country (12, 13). The purpose of this study was to estimate 5-year trends in tree stand fall injuries, as well as to describe the demographics of injured patients and fall injury features and precipitating factors.
Materials and Methods
Design and setting
A retrospective study was used to examine five previous deer hunting years, 2009–2013. The preponderance of annual deer hunting activities occur over five months between late summer and early winter, and include scouting, site identification, stand placement/removal, as well as active deer hunting with archery equipment or firearms. Each deer hunting year (which included both archery and firearms hunting seasons) was treated as an independent cross-sectional sample in this study and all tree stand fall injury data were extracted from Marshfield Clinic’s research data warehouse, which stores patients’ medical and administrative information documented in the system EHR during routine clinical encounters. The target population was the Marshfield Epidemiologic Study Area (MESA) (14). MESA is a regional population-based health research resource that tracks person-time from individuals who receive medical care from Marshfield Clinic and reside in one of 24 postal codes that surround primary service areas in central and northern Wisconsin. This region is predominantly rural and small towns, covering several thousand square miles, and has about 78,000 total residents who receive approximately 90% of their inpatient and outpatient healthcare from facilities and/or providers affiliated with Marshfield Clinic (15).
Sample
For each deer hunting year, the source population included individuals who resided in one of the MESA postal codes. Specific eligibility criteria for identified cases were: (1) received medical attention for a tree stand fall injury (described further below), (2) had a residential address in one of the MESA postal codes on the date of their index medical encounter for a tree stand fall injury, and (3) were age ≥10 years on the date of their index medical encounter. These criteria captured medically-attended tree stand fall cases that occurred among hunting age-eligible patients who lived in the target population during each deer hunting season. Because this was a retrospective analysis of existing healthcare data, the study was approved by the Marshfield Clinic Institutional Review Board with a waiver of informed consent and HIPAA authorization.
Tree stand falls
The outcome was medically-attended injuries from tree stand falls. These were ascertained using a two-phase approach that combined electronic natural language processing plus manual confirmatory chart audits. In the first phase, the occurrence of free-text expressions that indicated a fall from an elevated position as part of a hunting activity were searched for in medical encounter chart notes from each annual deer hunting season. Individuals who had the text expression pattern outlined in Figure 1 present in a medical encounter note (on the same date) were flagged as candidate cases. These electronically identified candidate cases were then subjected to a manual chart audit to verify whether or not a medically-attended injury from a tree stand fall actually occurred. The text expression pattern in this study was informed by suggestions and methods from other studies (8, 9), preliminary exploratory chart reviews, and clinical consensus among study investigators. As done in some previous studies (6, 16, 17), supplemental diagnostic codes indicative of an external injury caused by an accidental fall from an elevated position (i.e., E880.9, E881.0, E881.1, E882, E884.9, E929.3) were initially evaluated for possible integration into the final case-finding logic. However, preliminary chart reviews revealed that these fall codes were not commonly present, thus were not considered in our case-finding logic.
Figure 1.
Text expression pattern used to electronically identify candidate tree stand fall injury cases in the Marshfield Epidemiologic Study Area. Each individual who had this text pattern present in their medical chart notes on the same day was subjected to a manual chart review to confirm a medically-attended tree stand fall injury.
Exposures
In addition to year, several other exposure variables were extracted from the clinical data repository to describe patient demographic and clinical characteristics, salient features of tree stand fall injuries, and precipitating factors that may have contributed to the fall. These variables included the most recently known (relative to the date of the tree stand fall injury) values for age, sex, race/ethnicity, health insurance status, MESA region, number of outpatient medical encounters over the previous three years, body mass index, and presenting treatment site (e.g., hospital, clinic, emergency room [ER]). Where available from the index encounter, blood alcohol level was also reported. All exposure variables were previously collected as part of routine medical care by trained clinic staff using standard medical procedures.
Chart audits
All candidate tree stand fall cases identified via the electronic algorithm from each season were subjected to a manual chart audit conducted by a trained Research Coordinator. This chart audit included a review of all clinical notes documented on and near the date of the index medical encounter in order to: (1) confirm the presence or absence of a medically-attended injury from a tree stand fall, and (2) record possible functions of disagreements with the initial electronic identification of candidate cases (e.g., documentation errors, language sensitivities, irrelevant past medical histories). For confirmed cases, chart audits further included extraction of the clinical features of the tree stand fall injury, as well as documented precipitating circumstances associated with each tree stand fall. Chart audits focused on free-text documentation of the injury presentation (e.g., location, severity), as well as recorded fall antecedents such as the timing of hunting activities, environmental conditions, use of safety devices, and mechanical failures, among other relevant factors. Approximately 10% of all candidate cases were re-audited by a different Research Coordinator to detect and correct possible inter-rater discrepancies or chart review inconsistencies.
Analyses
Analytical procedures were conducted using SAS Version 9.3 (Cary, NC). Reasons for discrepancies were reported for the electronically identified initial candidate cases versus the manual chart audit confirmed cases. Summary statistics were reported on all confirmed cases. The annual incidence rate for tree stand fall injuries was estimated for each of the five deer hunting years by dividing the total number of confirmed cases by the total number of unique MESA residents who purchased a Wisconsin deer hunting license (archery and/or firearms). The denominator for this calculation was established from aggregated hunting license sales data from the Wisconsin Department of Natural Resources (DNR). Poisson regression with robust error variances (18) was performed to examine the 5-year trend in the rate of tree stand fall injuries. No age-sex standardization techniques were used due to the relatively small MESA study region, where the population of at-risk hunters was stable during the brief study timeframe and tree stand falls were considered rare events that would likely be absent in several age-sex strata.
Results
The number of unique deer hunters in MESA was stable over all five seasons, varying within a ±2% margin that ranged from a low of 16,556 hunters in 2010 to a high of 16,902 hunters in 2012. This represents about one-fourth of the total Census-estimated, hunting age-eligible MESA population, which is over twice the proportion of deer hunters in MESA as compared to the rest of Wisconsin. Of all MESA deer hunters in a given year, 57% purchased a firearms hunting authorization only, 4% purchased an archery hunting authorization only, and 39% purchased both a firearms and archery hunting authorization.
There were 261 initial candidate cases that were electronically identified from text expression patterns in chart notes, ranging from 39 to 69 candidate cases in a given season. Of these, manual chart reviews confirmed 39 (15%) tree stand fall injuries overall. Inter-rater agreement with chart re-audits was 96%, with the only inconsistency observed on one confirmed case where it was initially unclear if the injured patient actually fell from an elevated position. The most common reasons for manual chart audits that failed to confirm candidate cases involved language over-sensitivities in the electronic algorithm. Most unconfirmed patients indeed received medical attention for a fall injury, but their chart notes often listed ‘hunting’ as a hobby activity (unrelated to the presenting fall injury) and/or abilities to ‘stand’ as part of their clinical assessment of physical functioning. Descriptive characteristics of all confirmed tree stand fall cases are outlined in Table 1. The distribution of age, gender, race, and residency among tree stand fall patients appeared unremarkable compared to the general Wisconsin hunting population (19, 20), with cases being predominantly male, non-Hispanic White, and most living in the more populous central MESA region. Of note though, about twice as many tree stand fall patients were without health insurance relative to the general Wisconsin (21) and MESA (22) populations. Also, nearly nine of ten tree stand fall patients were overweight or obese, a level that is about 30% higher than that observed in the general adult MESA population.
Table 1.
Descriptive Characteristics of Central and Northern Wisconsin Residents who Received Medical Attention for a Tree Stand Fall Injury during the 2009–2013 Deer Hunting Seasons.
| Characteristics | Confirmed cases N = 39 |
|---|---|
| Age (years) | |
| 10–19 | 6 (15%) |
| 20–29 | 4 (10%) |
| 30–39 | 5 (13%) |
| 40–49 | 9 (23%) |
| 50–59 | 5 (13%) |
| 60–69 | 6 (15%) |
| ≥ 70 | 4 (10%) |
|
| |
| Sex | |
| Female | 3 (8%) |
| Male | 36 (92%) |
|
| |
| Race/Ethnicity | |
| White, non-Hispanic | 38 (97%) |
| Non-White, non-Hispanic | 1 (3%) |
|
| |
| Health insurance | |
| Commercial only | 15 (38%) |
| Public assisted | 14 (36%) |
| None | 10 (26%) |
|
| |
| Marshfield Epidemiologic Study Area region | |
| Central | 29 (74%) |
| North | 10 (26%) |
|
| |
| Number of medical visits in 3 years before fall | |
| 1–6 | 9 (23%) |
| 7–19 | 11 (28%) |
| 20–45 | 9 (23%) |
| ≥ 46 | 10 (26%) |
|
| |
| Body mass index | |
| Obese (≥ 30.0 kg/m2) | 20 (51%) |
| Overweight (25.0–29.9 kg/m 2) | 15 (38%) |
| Not overweight or obese (< 25.0 kg/m2) | 4 (10%) |
All values are reported as frequency (% of total).
In terms of injury features, the mean (SD) fall height was 12.5 ±5.9 feet and the time between the fall and presentation to a medical care facility was 3.4 ±4.0 hours. Most patients presented to a hospital ER (69%), with the remainder presenting to a clinic urgent care center (26%) or ancillary clinic service line such as physical therapy or nurse call line (5%). One-third arrived via ambulance, including one air ambulance transport. Among the 13 hospitalized patients, the length of stay was 5.1 ±3.2 days. As expected, severe pain was a feature in most presenting injuries, but a more detailed summary of other principal injury types is presented in Table 2. The most common injury location was lower extremities (60%), followed by upper extremities (33%), head (33%), torso (31%), and spine/neck (23%). Internal organs/systems injuries were documented in three cases, and there were two hospital fatalities linked to the patient’s fall from a tree stand.
Table 2.
Principal Injury Features of Central and Northern Wisconsin Residents who Received Medical Attention for a Tree Stand Fall Injury during the 2009–2013 Deer Hunting Seasons (N = 39).
| General location (number of cases with injury) |
Injury description | Number (%) of injuries by general location |
|---|---|---|
| Lower extremities (n = 23) |
Fracture | 11 (48%) |
| Laceration/abrasion | 8 (35%) | |
| Ankle sprain | 3 (13%) | |
|
| ||
| Upper extremities (n = 13) |
Laceration/abrasion | 5 (38%) |
| Fracture | 5 (38%) | |
| Shoulder dislocation | 1 (8%) | |
|
| ||
| Head (n = 13) |
Concussion | 5 (38%) |
| Laceration/abrasion | 5 (38%) | |
| Unconsciousness | 3 (23%) | |
| Fracture | 1 (8%) | |
|
| ||
| Torso (n = 12) |
Laceration/abrasion | 3 (25%) |
| Rib fracture | 2 (17%) | |
|
| ||
| Spine/neck (n = 9) |
Vertebrae fracture | 6 (67%) |
| Vertebrae compression | 3 (33%) | |
|
| ||
| Internal organs/systems (n = 3) |
Spleen laceration | 1 (33%) |
| Adrenal contusion | 1 (33%) | |
| Renal laceration | 1 (33%) | |
Percentages do not sum to 100% in some rows because some cases had multiple injuries and, for some other cases, pain was the only presenting injury (which is not reflected here).
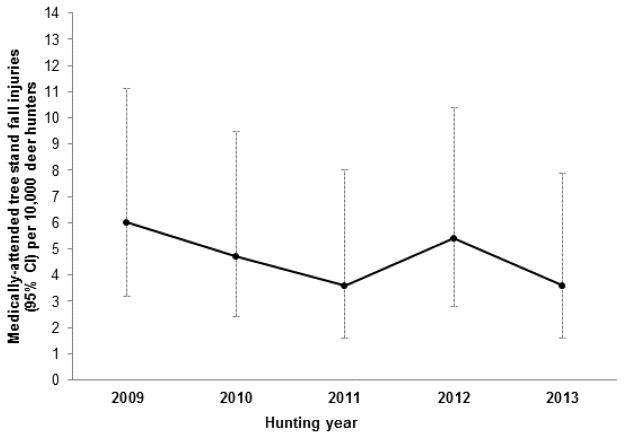
As outlined in Figure 2, the annual incidence rate of medically-attended tree stand fall injuries did not significantly change during the 5-year study timeframe (P for trend = 0.79). There was a high of 6.0 (95% confidence interval [CI]: 3.2, 11.1) fall injury cases per 10,000 hunters in 2009, and a low of 3.6 (95% CI: 1.6, 7.9) fall injury cases per 10,000 hunters in 2013. No year-to-year comparisons were significantly different. Medical chart note documentation of possible precipitating fall factors was limited. Most cases (77%) occurred during archery-only times of the deer hunting season, and the most common activities at the time of the fall were climbing down from a tree stand (28%) in the evening (36%). Documentation of a safety device was only available in four cases, with half reporting actual use of a safety belt and half reporting no use. A blood alcohol test was available in 23% of fall patients, with one having evidence of recent alcohol consumption. Structural failures (e.g., broken stand parts) were noted in 18% of falls, and only one environmental factor (i.e., ladder frost) was noted.
Figure 2.
Estimated annual incidence rate of medically-attended tree stand fall injuries among central and northern Wisconsin deer hunters, 2009–2013.
Discussion
Over the past five years, about 5 per 10,000 hunters per year in MESA experienced a medically-attended tree stand fall, a rate nearly identical to that observed in a previous national study of hospital data (6) and similar to that observed in a study of ER-based hunter injury cases conducted in Marshfield two decades ago (23). Contrary to findings in specialty care centers from prior time periods (2, 8), fall injury risk in MESA was statistically stable between 2009 and 2013. Also, tree stand falls injuries in this study were, as also observed in national hospital data (6, 24), most common during archery season and in middle-age males, routinely resulting in serious injuries to the upper and lower extremities, with head, neck, and spine injuries also present. With the possible exceptions of higher rates of obesity and uninsured, the profile of tree stand fall injury patients largely reflected the general population of Wisconsin deer hunters (19, 20).
A casual interpretation of these findings may intimate that deer hunters today are less apt to fall out of a tree stand relative to estimates generated years ago (4, 5), thus a closer examination of the epidemiologic context of this study is warranted. All cases were medically-attended and falls that resulted in minor or no injury, as well as falls resulting in a fatality in the field, could not be captured. The study occurred during a time period of diminishing health insurance benefits (25), which may have been accelerated in hunters due to their predominantly labor-oriented occupations (hardest hit by economic recession) (26), and presumably resulting in a lower propensity to seek care for less acute injuries. Also, some MESA fall victims may have received episodic care at an unaffiliated facility outside of the Marshfield Clinic service area, where clinical fall injury data would have been unavailable. In addition to the potential case undercount, there was likely some level of inflation in the at-risk denominator population. In any given season, some deer hunting license holders do not actually go hunting or do not hunt from tree stands. This quantity is unknown in MESA, but a previous statewide survey in 2013 (______ ______ [author name blinded], Wisconsin DNR, email communication, 2015) indicated that <1% of deer hunting license holders do not actually go hunting, and an estimated 9% of archery hunters and 16% of firearms hunters do not use tree stands. Assuming such findings are roughly representative of current MESA deer hunters, the seasonal denominators used in this study could have comprised about 2,500 fewer at-risk individuals, yielding a higher ‘true’ incidence rate of tree stand falls.
These methodological factors likely render the tree stand fall risk observed in this study conservative, particularly when viewed from an annual timeframe. Whitetail deer hunting remains a unique recreational pastime in parts of the U.S. and Canada, where generations of families engage in the activity year-over-year. As such, the population of active deer hunters is fairly consistent, making the lifetime risk of a fall greater than that observed in a single season. To illustrate this point, the annualized fall risk in this study was 0.06% among the estimated number of deer hunters who used tree stands. Transposed to a given individual who goes deer hunting from a tree stand for 50 annual seasons would translate into an approximate 1-in-33 lifetime risk of a potentially debilitating tree stand fall injury requiring medical attention. The lifetime risk of any tree stand fall, with major injury or not, may be ten times greater (5). By comparison, the current risk of a gunshot wound among deer hunters appears to be at least 90% lower (24, 27).
Given the lack of a significant decline in medically-attended tree stand fall injuries, fall prevention initiatives need to be accelerated for deer hunters. However, few tested models exist to guide such efforts. A Louisiana public awareness campaign in the mid 1990’s appeared to help reduce severe spinal cord injuries among deer hunters by promoting the use of safety harnesses (28). It is unclear if a similar approach would be helpful two decades later in other parts of the country, or now that safety harnesses are routinely recommended. Public education on tree stand safety is available from many state and healthcare organizations (e.g., dnr.wi.gov/topic/hunt/treeStand.html, shine365.marshfieldclinic.org/tag/couch-to-deer-camp/). Given the positive influence of physician advice for other health risks (29, 30), as well as the fact that most individuals see a medical professional with some regularity, primary care initiatives could complement public health, tree stand manufacturing industry, and hunter education efforts by screening for tree stand fall risks and providing fall prevention advice in the clinical setting.
Due to the scant medical documentation of fall antecedents, the etiology of tree stand falls remains largely speculative. There were some leads from this study; most falls occurred during archery-only timeframes, in the evening, and when climbing down from a tree stand. This may reflect increased risks among archery hunters who tend to spend more time afield and during low-light conditions when fatigue is a factor (23). But there are many unknown factors still, such as how consistently/correctly safety harnesses are used, the influence of obesity on some injuries, or how healthcare coverage impacts attainment of medical care for falls (a potentially shifting factor in light of American healthcare reforms). Direct comparisons between rigorously defined tree stand fall cases and controls are needed. More detailed insights are also required on specific, timely, and relevant prevention factors to target for stakeholders, including hunters, tree stand manufacturers, and purveyors of hunter safety curriculum. Assuming MESA is representative of all Wisconsin deer hunters, 200–250 medically-attended tree stand falls can be expected statewide each year, thus the economic sequelae of tree stand fall injuries seems to be a relevant line of further inquiry because the impact of such injuries on workplace productivity and healthcare costs is currently unknown.
Strengths of this study included the systematic capture of hospital and ambulatory medical care from a defined population over multiple deer hunting seasons. In addition, suspected tree stand fall injury cases were confirmed via manual chart review. With further refinements to improve specificity (31), the natural language processing algorithm used here could provide a useful technical innovation in population-level surveillance of hunter safety. As previously discussed, selection biases related to the retrospective use of medical records to identify cases was the chief study limitation. Individuals who did not receive medical attention for their fall were not captured, thus incidence rates in this study do not reflect the risk of any fall and cannot be generalized to deer hunters across the country. Also, the at-risk denominator population had to be approximated from aggregate counts of unique deer hunting license holders in MESA because neither medical records, nor hunting license sales data, can precisely identify all individuals who deer hunted from tree stands in a given season.
Conclusion
This was the first population-level study of medically-attended tree stand fall injuries among deer hunters within a regional healthcare system that included a full range of inpatient and outpatient medical care environments. In this rural area of north-central Wisconsin, the current seasonal incidence rate of such injuries is relatively low, but with limited signs of improvement. Most tree stand fall injuries examined in this study, as in others, were quite serious, with broken bones commonplace, along with complex medical follow-up procedures required, and some paralysis and fatalities. As such, continued efforts are needed to promote the long-term safety of the deer hunting public, particularly in rural areas where hunting injuries are more apt to occur and clinic-community partnered tree stand fall prevention initiatives may be most impactful.
Acknowledgments
This work was supported by the Marshfield Clinic Dean Emanuel Endowed Chair in Agricultural Medicine (Keifer), as well as the Clinical and Translational Science Award program through the National Center for Advancing Translational Sciences at the National Institutes of Health (grant UL1TR000427).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Halanski MA, Corden TE. Wisconsin firearm deer hunting season: injuries at a level I trauma center, 1999–2004. WMJ. 2008;107:20–24. [PubMed] [Google Scholar]
- 2.Crockett A, Stawicki SP, Thomas YM, et al. Tree stands, not guns, are the midwestern hunter's most dangerous weapon. Am Surg. 2010;76:1006–1010. [PubMed] [Google Scholar]
- 3.National Shooting Sports Foundation. [Accessed April 9, 2015];Firearms-related injury statistics. 2014 www.nssf.org/PDF/research/IIR_InjuryStatistics2014.pdf.
- 4.International Hunter Education Association. [Accessed December 1, 2014];Safety Issues related to Hunting in Elevated Stands. www.ihea.com/_assets/documents/Elevated_StandReport.pdf.
- 5.Deer and Deer Hunting. [Accessed December 1, 2014];One in Three Hunters Will Fall. www.deeranddeerhunting.com/articles/deer-hunting-tips/p3_one_in_three_hunters_will_fall.
- 6.Terry J, Griffin R, Rue LW, 3rd, McGwin G., Jr Epidemiology of tree stand-related injuries in the United States from 2000 to 2007. J Trauma. 2010;68:712–715. doi: 10.1097/TA.0b013e3181a3a903. [DOI] [PubMed] [Google Scholar]
- 7.Wisconsin Department of Natural Resources. [Accessed October 30, 2014];Detailed 2013 License Sales. dnr.wi.gov/topic/hunt/documents/DeerSales.pdf.
- 8.Smith JL, Lengerich EJ, Wood GC. Injuries due to falls from hunters' tree stands in Pennsylvania. Am J Prev Med. 2009;37:433–436. doi: 10.1016/j.amepre.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Gates RL, Helmkamp JC, Wilson SL, Denning DA, Beaver BL. Deer stand-related trauma in West Virginia: 1994 through 1999. J Trauma. 2002;53:705–708. doi: 10.1097/00005373-200210000-00014. [DOI] [PubMed] [Google Scholar]
- 10.VanWormer JJ. Methods of using the electronic health record for population level surveillance of coronary heart disease risk in the Heart of New Ulm project. Diabetes Spectrum. 2010;23:161–165. [Google Scholar]
- 11.Acharya A, VanWormer JJ, Waring SC, Miller AW, Fuehrer JT, Nycz GR. Regional epidemiologic assessment of prevalent periodontitis using an electronic health record system. Am J Epidemiol. 2013;177:700–707. doi: 10.1093/aje/kws293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wisconsin Department of Natural Resources. [Accessed December 1, 2014];Fall Deer Densities 2013. dnr.wi.gov/topic/hunt/maps.html/falldeerperdr.pdf.
- 13.Wisconsin Deer Management Unit Stakeholder Review Panel. [Accessed December 1, 2014];Hunter Pressure opening Day 2008. dmureview.editme.com/files/Topic-1234236832591/hunter%20pressure%20opening%20day%2008.pdf.
- 14.DeStefano F, Eaker ED, Broste SK, et al. Epidemiologic research in an integrated regional medical care system: The Marshfield Epidemiologic Study Area. J Clin Epidemiol. 1996;4:643–652. doi: 10.1016/0895-4356(96)00008-x. [DOI] [PubMed] [Google Scholar]
- 15.Kieke AL, Kieke BA, Kopitzke SL, et al. Validation of health event capture within the Marshfield Epidemiologic Study Area. Clin Med Res. doi: 10.3121/cmr.2014.1246. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Metz M, Kross M, Abt P, Bankey P, Koniaris LG. Tree stand falls: a persistent cause of sports injury. South Med J. 2004;97:715–719. doi: 10.1097/00007611-200408000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Pierre CA, Plog BA, Srinivasan V, Srinivasan K, Petraglia AL, Huang JH. Tree stand falls: A persistent cause of neurological injury in hunting. World J Clin Cases. 2014;2:345–350. doi: 10.12998/wjcc.v2.i8.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 19.Huck J, Winkler R. [Accessed December 1, 2014];Deer hunter demography: Projecting future deer hunters in Wisconsin. www.apl.wisc.edu/publications/APL_hunter_brief_final.pdf.
- 20.Winkler R, Klass R. [Accessed December 14, 2014];Declining deer hunters: Wisconsin’s gun deer hunter numbers are continuing to decline. www.huntersnetwork.org/wp-content/uploads/2010/08/APL_hunters2011_web.pdf.
- 21.Kaiser Family Foundation. [Accessed December 21, 2014];Health insurance coverage of the total population. kff.org/other/state-indicator/total-population/?state=WI.
- 22.VanWormer JJ, Miller AW, Rezkalla SH. Identifying opportunities to improve aspirin utilization for the primary prevention of cardiovascular disease in a regional healthcare system. WMJ. 2014;113:190–195. [PMC free article] [PubMed] [Google Scholar]
- 23.Stueleand D, Carpenter WS, Cleveland D. Summary of hunting injuries in central Wisconsin: A 4-year experience at a rural referral center. Wilderness Environ Med. 1995;6:196–202. doi: 10.1580/1080-6032(1995)006[0196:sohiic]2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 24.Loder RT. Epidemiology of hunting stand injuries presenting to US emergency departments, 2004–2012. Wilderness Environ Med. doi: 10.1016/j.wem.2014.07.004. In press. [DOI] [PubMed] [Google Scholar]
- 25.Schoen C, Radley DC, Collins SR. State trends in the cost of employer health insurance coverage, 2003–2013. The Commonwealth Fund. 2015 Jan; [PubMed] [Google Scholar]
- 26.American Sportfishing Association. Responsive Management, Oregon Department of Fish and Wildlife, Southwick Associates. [Accessed April 8, 2015];Exploring recent increases in hunting and fishing participation. www.responsivemanagement.com/download/reports/Hunt_Fish_Increase_Report.pdf.
- 27.Wisconsin Department of Natural Resources. [Accessed August 3, 2015];Hunter Education Annual Report. 2014 dnr.wi.gov/topic/hunt/incidentreport.html.
- 28.Lawrence DW, Gibbs LI, Kohn MA. Spinal cord injuries in Louisiana due to falls from deer stands, 1985–1994. J La State Med Soc. 1996;148:77–79. [PubMed] [Google Scholar]
- 29.Bandi P, Cokkinides VE, Weinstock MA, Ward EM. Physician sun protection counseling: prevalence, correlates, and association with sun protection practices among US adolescents and their parents, 2004. Prev Med. 2010;51:172–177. doi: 10.1016/j.ypmed.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Reed DB, Browning SR, Westneat SC, Kidd PS. Personal protective equipment use and safety behaviors among farm adolescents: gender differences and predictors of work practices. J Rural Health. 2006;22:314–320. doi: 10.1111/j.1748-0361.2006.00052.x. [DOI] [PubMed] [Google Scholar]
- 31.Luther SL, McCart JA, Berndt DJ, et al. Improving identification of fall-related injuries in ambulatory care using statistical text mining. Am J Public Health. 2015;105:1168–1173. doi: 10.2105/AJPH.2014.302440. [DOI] [PMC free article] [PubMed] [Google Scholar]