Abstract
Background
A remarkably high rate of traumatic event reexposure has been demonstrated in community-based substance users which negatively impacts their substance use disorder (SUD). The rate and effect of such reexposure in treatment is unknown. Despite increasing evidence that a diagnosis of posttraumatic stress disorder (PTSD) has little influence on long-term SUD treatment outcomes, it is possible that PTSD symptom fluctuations could have effects.
Methods
This prospective longitudinal study examined the rate and effect of traumatic event reexposure and PTSD symptoms in 169 male and female methadone maintenance patients with a comorbid psychiatric disorder who were participating in a parent study. Traumatic events and PTSD symptoms were tested for association with drug use, treatment interruption, and counseling adherence in the same month, one month later, and two months later.
Results
Approximately 18% of patients were reexposed to a traumatic event each month during the 12-month study. Reexposure was associated with about twice the risk of treatment interruption in the same month and one month later. Every 10% increase in PTSD symptom severity was associated with a 36% increased risk of treatment interruption two months later. No effects were seen on drug use or counseling adherence.
Conclusions
SUD patients have a relatively high rate of traumatic event reexposure. Both traumatic events and PTSD symptoms are associated with increased risk of treatment interruption, resulting in SUD patients leaving treatment at precisely the time they could benefit from treatment support.
Keywords: traumatic event, PTSD, substance use disorder, treatment outcome, gender differences
1. INTRODUCTION
Both traumatic events and subsequent posttraumatic stress disorder (PTSD) have significant and serious effects in substance use disordered (SUD) patients. Nearly all SUD patients have a history of traumatic events, which have been associated with a number of negative sequelae including poorer mental and physical health (Gilbert et al., 2015) and a risk of developing PTSD and other psychiatric disorders (Green et al., 2010). An important but often overlooked outcome in SUD patients is the potential for traumatic event reexposure or revictimization. Our previous work documented that 27% of active injecting substance users with little treatment contact experienced a new traumatic event each month (Peirce et al., 2012). Although these men and women were polysubstance users, nearly all injected heroin. Risk factors for reexposure in substance users and non-users alike include psychiatric treatment history and past traumatic event exposure, among others (Breslau et al., 1995; Cohen et al., 2013; Peirce et al., 2014). Reexposure in the above SUD sample was associated with an increased risk of later drug use and a desire for SUD treatment, without a corresponding increase in treatment enrollment (Peirce et al., 2013). The rate of traumatic event reexposure is unknown in SUD patients enrolled in treatment, nor is there data to determine the potential effect of such reexposure on treatment outcomes.
PTSD is comparatively well-studied in SUD patients. One-quarter to one-third of SUD patients in treatment meet diagnostic criteria for current PTSD, which has been consistently associated with greater psychiatric distress, poor social support, and poor physical health in mixed drug users (Driessen et al., 2008; Reynolds et al., 2005) and opioid users (Mills et al., 2005, 2007; Peirce et al., 2009). Studies on the relationship between PTSD and SUD treatment outcomes have had mixed results. Although early work suggested PTSD was associated with more in-treatment drug use or faster relapse to drug use in mixed samples (Brown et al., 1996) and in opioid users (Hien et al., 2000), more recent prospective studies have failed to find this relationship in mixed samples (Norman et al., 2010) and in opioid users (Mills et al., 2007; Trafton et al., 2006). A recent review concluded that a diagnosis of PTSD does not consistently affect SUD treatment outcomes (Hildebrand et al., 2014). However, the clinical belief that PTSD does negatively affect SUD treatment response persists. As most studies in this area diagnose PTSD at one time (usually treatment entry) and measure outcomes months or years later, it is possible that more frequent assessments of PTSD symptoms and SUD outcomes would identify a significant and more dynamic relationship between PTSD and SUD. This possibility is supported by studies in which a diagnosis of PTSD made at treatment entry had no relationship to SUD outcomes but PTSD that remained symptomatic predicted worse outcomes, although these studies had only a minority of opioid users (Ouimette et al., 2007; Read et al., 2004). Much of the literature on outcomes has focused on psychosocial-only treatment settings and more data is needed on patients in medication-assisted treatment, especially considering opioid users’ higher risk of traumatic events and PTSD (Dabbs et al., 2014; Meier et al., 2014). Given the reexposure risk associated with psychiatric treatment history in active substance users, SUD patients with a comorbid psychiatric disorder could be a high-risk subgroup worthy of increased focus.
The present study was designed to address these gaps in the literature. First, we wished to document the rate of traumatic event reexposure in a sample of SUD patients comorbid for another psychiatric disorder and enrolled in methadone maintenance. We expected that the rate would be non-trivial, but likely lower than that found in our previous work with active injecting drug users. Second, we examined the relationship of any traumatic event reexposure and qualitatively different types of traumatic events to the specific treatment outcomes of drug use, treatment interruption, and counseling adherence over short proximal time frames. We expected that traumatic event exposure, and more severe types of traumatic events in particular, would be associated with poorer SUD treatment response. Third, we evaluated the relationship of PTSD symptom severity to these same outcomes. We expected that PTSD severity would not be associated with SUD treatment outcomes.
2. MATERIALS AND METHODS
2.1 Participants
Study participants were drawn from a parent study comparing integrated onsite psychiatric care to offsite care for substance abusers enrolled in methadone maintenance treatment (Brooner et al., 2013). Inclusion criteria for the parent study were: 1) current opioid dependence and enrolled in the methadone maintenance treatment setting; 2) current comorbid psychiatric disorder; and 3) willingness to receive psychiatric care. See Brooner et al. (2013) for complete information. The traumatic event and PTSD symptom assessments were added to the parent study after it was underway. No inclusion or exclusion criteria were added or modified for the present study. Of 316 randomized participants in the parent study, 169 received the present study measures. Comparison of the 147 participants excluded from the present study with the 169 included participants on several demographic, psychiatric, and drug use characteristics found no significant differences. The present report focuses on the substance abuse treatment outcomes and does not include the psychiatric treatment outcomes.
2.2 Measures
Sample characteristics were measured with a purpose-made demographic questionnaire, administered at entry into the study. The Structured Clinical Interview for DSM-IV (SCID; First et al., 1998) was administered at study entry to assess lifetime and current psychiatric disorders, including posttraumatic stress disorder (PTSD). Followups were scheduled monthly while the participant remained in treatment.
2.2.1 Traumatic events and PTSD symptoms
The Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000) was administered at study entry to document lifetime exposure to traumatic events and monthly thereafter to assess exposure to new events. The TLEQ probes for exposure to 22 specific potential traumatic events and a 23rd ‘other’ category, as defined in the DSM-IV-TR criteria for PTSD (American Psychiatric Association, 2000). These probes are followed by questions to determine whether the event meets DSM-IV-TR criterion A(2) (i.e., a response of extreme fear, helplessness or horror); all events reported here met criterion A(2). We note that this standard is more restrictive than that for the current DSM-V (American Psychiatric Association, 2013). The TLEQ is considered a ‘gold standard’ in traumatic event assessments (Gray et al., 2004; Weathers and Keane, 2007), and appears to detect traumatic events better than other measures in SUD populations (Peirce et al., 2009). Similar types of lifetime events were grouped together for concise presentation. Specifically, physical assault with and without weapon were grouped into “physical assault;” motor vehicle accidents and other types of accidents were grouped into “accident;’ sexual harassment and stalking were grouped into “other threats;” and abortion, miscarriage, and other events were grouped into “other events.”
The TLEQ was also administered at monthly follow-ups, for a total of 1242 administrations. It was modified for follow-up administration by removing event probes for childhood events and prefacing each remaining event probe with ‘In the past 30 days...’. For the main analyses, the TLEQ provided a dichotomous measure of traumatic event re-exposure in a given month (exposure to any type of event versus no exposure). A second set of analyses examined the specific effects of any death or injury of loved one (defined as unexpected death of loved one or illness/injury of loved one) and any assault (defined as physical or sexual assault) on the same treatment outcomes.
The Modified Posttraumatic Stress Scale-Revised (MPSS-R; Falsetti et al., 1993) was used to assess current PTSD symptoms at follow-up months 4, 8 and 12; it was administered 271 times. It consists of 17 questions targeted to the 17 DSM-IV-TR symptoms, with scales to rate frequency (0–3) and severity (0–4) of each symptom,which are summed for a total severity score. The MPSS-R has shown good reliability and validity in SUD populations (Coffey et al., 1998). The total severity score (range 0–119) was recoded into deciles (range 1–10) to facilitate the interpretation of results, so that the outcomes are expressed as a function of a 10% increase in PTSD symptom severity. Participants scored in the lower deciles more frequently, but all deciles were populated. The MPSS-R was also used for a putative PTSD diagnosis, defined as meeting criteria for 1 reexperiencing, 3 avoidance/numbing, and 2 hypervigilance symptoms. A PTSD symptom was coded positive when the frequency was rated 1 or more (once per week) and severity was rated 2 or more (moderate distress).
2.2.2 Treatment outcomes
Drug use, treatment interruption (missing one week of treatment services), and counseling adherence indicated participants’ response to treatment in the same month, one month later, and two months after the predictor. Drug use and counseling adherence were assessed while participants were in treatment regardless of follow-up attendance; treatment interruption was coded for all 12 months. Drug use was assessed with urine test results. Urine sample collection was observed and collected on a weekly semi-random schedule (Monday, Wednesday, or Friday). Missed samples were considered “positive.” Because distribution of the proportion of drug-positive urine tests was non-normal (i.e., largely flat with peaks at 0% and 100%), we used a dichotomous outcome of positive for any drug versus negative for all drugs. Of 1408 months in which urine results were available, 58% (814) were coded drug-positive. Attrition—typically defined as leaving treatment without returning—is relatively rare in methadone maintenance after the first month of treatment (Mancino et al., 2010) and was rare in this sample during this short study period, although missing treatment is considered clinically significant. We operationalized an alternative to attrition we are calling treatment interruption. Treatment interruption was defined as being absent from all treatment for at least one week during a given month. This definition also approximates the standard methadone maintenance procedure to discharge a patient who misses at least 3 days of medication. (Participants in this clinic could return to treatment after a treatment interruption, however.) Of 2028 months (169 participants with 12 follow-up months), 37% (749) were coded as having a treatment interruption. Participants were assigned to individual and group substance abuse counseling based on our evidence-based Motivated Stepped Care model (Brooner et al., 2013, 2004). Adherence to counseling was strongly negatively skewed to 100%, so we used a dichotomous outcome of 100% adherent versus <100% adherent. Of 1373 months with substance abuse counseling assigned, 48% (665) were coded 100% adherent.
2.2.3 Statistical approach
The purpose of this cohort study was to determine the impact of traumatic event re-exposure and PTSD symptoms on proximal treatment outcomes in the same month, 1 month later, and 2 months later, using data from intake and 12 monthly follow-ups. All data were analyzed using IBM SPSS statistics version 21 for Mac.
Sample characteristics were measured with means and proportions. The present study sample was compared to the sample included in the parent study (Brooner et al., 2013) but excluded for this study using t-tests and chi-square tests. Gender differences in participant characteristics and lifetime traumatic event exposure were also examined with t-tests and chi-square tests.
The main analyses examined the effect of any traumatic event exposure and PTSD symptoms on the dichotomous treatment outcomes of any drug use, treatment interruption, and 100% counseling adherence (all Y/N) using generalized estimating equations (GEE; Genlin procedure; Liang and Zeger, 1986), specifying a binomial distribution with a logit link. GEE are particularly useful in longitudinal studies with sporadic missing data because the analysis takes advantage of all available data without imputation while accounting for within-subject correlation. As noted above, any traumatic event exposure (Y/N) was coded in each attended monthly follow-up and PTSD symptom decile (1-10) was coded in each attended 4-month follow-up.
Each unadjusted model associates the binary dependent variable outcome (e.g., treatment interruption) as a function of follow-up month (1-12) with the independent variable (e.g., traumatic event exposure); note that the independent variable is a time-dependent covariate. For analyses of association between variables in the same month, each model would have 12 repeated measures per participant. Analyses of outcomes one month later would have 11 measures and outcomes two months later would have 10 measures per participant. This is because we do not have measures of the outcome beyond 12 months (e.g., no way to measure the association between traumatic event in follow-up month 12 with outcome in month 13 or 14). Unadjusted results are presented as odds ratios (OR) with 95% confidence intervals (CI). Fixed covariates were chosen based on their known relationship to either dependent or independent variables, including parent study treatment condition (onsite vs. offsite), gender (women vs. men; women more likely to have PTSD; Peirce et al., 2008), minority status (nonwhite vs. white; minorities more likely to leave treatment; Magruder et al., 2009) and age (i.e., older patients more likely to remain in and adhere to treatment; Korte et al., 2011). Because ongoing drug use seemed likely to mediate the effect of traumatic event re-exposure and PTSD symptoms on drug use outcomes, adjusted models for this outcome also included the time-varying covariate of the previous month's proportion of positive urine results. Thus, final models included each independent (time-varying) variable, the fixed covariates, previous month's drug use (drug use outcome only), and each of the outcomes at each time period, for a total of 9 models for each predictor. Adjusted results are presented as adjusted odds ratios (AOR).
Men attended more follow-ups than women [men 8.20 (4.15) vs women 6.84 (4.32); t(167) = 2.02; p = 0.05], although there was no association with minority status [nonwhite 6.95 (4.49) vs white 7.61 (4.16); t(167) = .971; p = 0.33] or age [r = .13; p = 0.09] and participants in both conditions attended an average of 7 follow-ups [t(167) = .006; p = 0.99].
3. RESULTS
3.1. Traumatic events and PTSD during treatment
3.1.1. Traumatic events
Nearly all participants (97%) had at least one lifetime traumatic event, with a total average of 18 traumatic events. Table 1 shows the frequency of each type of event by gender. As expected, women were more likely than men to report a history of sexual assault at any age and intimate partner violence, as well as other threats (i.e., sexual harassment and stalking). Men were more likely than women to endorse a history of physical assault and witnessing physical assault.
Table 1.
Lifetime traumatic event exposure overall and by gender, expressed as percent of column (n).
| All participants N = 167a | Men n = 63 | Women n = 104 | |
|---|---|---|---|
| Natural disaster | 5 (8) | 3 (2) | 6 (6) |
| Accident | 45 (75) | 49 (31) | 42 (44) |
| Death of loved one | 62 (104) | 57 (36) | 65 (68) |
| Illness or injury of loved one | 29 (48) | 35 (22) | 25 (26) |
| Life-threatening illness | 29 (49) | 30 (19) | 29 (30) |
| Combat | 1 (1) | 2 (1) | 0 (0) |
| Adult physical assault* | 64 (106) | 81 (51) | 53 (55) |
| Witness assault* | 40 (67) | 54 (34) | 32 (33) |
| Threatened with assault | 29 (49) | 29 (18) | 30 (31) |
| Witness family violence | 47 (79) | 46 (29) | 48 (50) |
| Child physical assault | 26 (43) | 24 (15) | 27 (28) |
| Intimate partner violence* | 49 (82) | 11 (7) | 72 (75) |
| Child sexual assault*b | 29 (48) | 14 (9) | 38 (39) |
| Young adult sexual assault* | 11 (19) | 2 (1) | 17 (18) |
| Adult sexual assault* | 19 (31) | 3 (2) | 28 (29) |
| Other threats* | 26 (43) | 8 (5) | 37 (38) |
| Other events | 52 (86) | 43 (27) | 57 (59) |
| Any traumatic event | 97 (162) | 97 (61) | 97 (101) |
Gender difference: p < 0.01
Two participants are missing data.
One participant refused to answer child sexual assault questions.
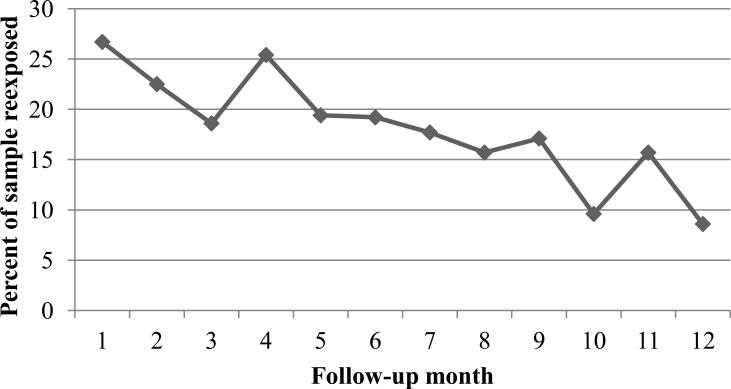
Traumatic event reexposure was also relatively common, with an average of 18% of participants reporting a new traumatic event each month during the study (see Figure 1). Women and men were equally likely to be reexposed [OR (95% CI) = 1.33 (0.90 - 1.97)]. Visual inspection suggested that the likelihood of reexposure decreased over time, so the model was reanalyzed including time. Each month was associated with a 5% decreased likelihood of reexposure [AOR (95% CI) = 0.95 (0.92 - 0.98)] and gender remained a nonsignificant factor [1.29 (0.88 - 1.89)]. In six months, 54% of the sample had experienced at least one new traumatic event; this number increased slightly to 61% by the end of the 12-month study.
Figure 1.
Percent of sample with traumatic event reexposure each month.
3.1.2. Posttraumatic stress disorder
Women were more likely than men to meet criteria for PTSD on the SCID at study entry (31% vs. 13%; n = 168; χ2(1) = 7.29; p = 0.007). Women remained twice as likely to meet criteria for a putative diagnosis of PTSD on the MPSS-R during treatment [AOR (CI) = 2.57 (1.25 – 5.28)], and there was no change over time [Month AOR (CI) = 0.99 (0.94 - 1.05)].
3.2 Effects of traumatic events on SUD treatment outcomes
Table 2 presents the effects of any traumatic event reexposure, adjusted for treatment condition, age, gender, race, and past month drug use (drug use outcome only). There was no significant effect of traumatic event reexposure on drug use or counseling adherence. Traumatic events were associated with more than double the risk of treatment interruption in the same month as the event and nearly double the risk in the following month. Unadjusted models were nearly identical.
Table 2.
Effect of any traumatic event exposure on proximal treatment outcomes, expressed as adjusted odds ratios with 95% confidence interval.
| Same month | One month later | Two months later | |
|---|---|---|---|
| Any positive urine (y/n) | 1.19 (0.81 – 1.74) | 1.04 (0.78 – 1.40) | 1.03 (0.75 – 1.41) |
| Treatment interruption (y/n) | 2.71 (1.59 – 4.60)* | 1.91 (1.29 – 2.83)* | 1.11 (0.85 – 1.45) |
| 100% counseling adherence (y/n) | 0.82 (0.61 – 1.10) | 0.89 (0.66 – 1.19) | 1.00 (0.73 – 1.39) |
p ≤ 0.001
We explored the occurrence and effect of qualitatively different types of traumatic events. Approximately 9% (range: 3% to 14%) of the sample reported an unexpected death or injury to a loved one each month and 2% (range: 0% to 6%) reported a physical or sexual assault each month during the study. Effects on treatment outcomes are shown in Table 3. The pattern of results for death or injury to a loved one mirrored the “any event” results, with over twice the risk of treatment interruption in the same month and 64% increased risk in the following month, but no other significant associations. The pattern of effects for physical and sexual assault were somewhat different. The effect of assault on treatment interruption was in the same direction and of a similar magnitude as the effect of other traumatic events, although the relationship did not reach significance. However, participants who were assaulted were less than half as likely to be counseling adherent one and two months after exposure. We note that the confidence intervals around the odds ratios are a bit larger for physical/sexual assault than death or injury, likely because assault occurred less frequently.
Table 3.
Effects of a death or injury to a loved one and a physical or sexual assault occurring to the participant on proximal treatment outcomes, expressed as adjusted odds ratios with 95% confidence intervals.
| Death or injury to loved one | |||
|---|---|---|---|
| Same month | One month later | Two months later | |
| Any positive urine (y/n) | 1.22 (0.78 – 1.88) | 1.02 (0.70 – 1.49) | 1.14 (0.74 – 1.76) |
| Treatment interruption (y/n) | 2.21 (1.15 – 4.27)* | 1.64 (1.03 – 2.62)* | 1.05 (0.75 – 1.49) |
| 100% counseling adherence (y/n) | 0.99 (0.68 – 1.44) | 0.98 (0.71 – 1.35) | 1.02 (0.65 – 1.62) |
| Physical or sexual assault | |||
| Any positive urine (y/n) | 1.24 (0.54 – 2.86) | 1.47 (0.81 – 2.70) | 1.20 (0.77 – 1.88) |
| Treatment interruption (y/n) | 2.18 (0.68 – 7.00) | 1.94 (0.80 – 4.69) | 1.86 (0.97 – 3.58) |
| 100% counseling adherence (y/n) | 0.89 (0.47 – 1.68) | 0.29 (0.12 – 0.75)* | 0.46 (0.25 – 0.84)* |
p < 0.05
3.3 Effects of PTSD symptoms on SUD treatment outcomes
An increase of 10% in PTSD symptom severity was associated with a 36% increased risk of treatment interruption two months later (see Table 4). PTSD symptoms were not associated with drug use or counseling adherence over any time period. Unadjusted models were nearly identical.
Table 4.
Effect of a 10% increase in PTSD symptom severity on proximal treatment outcomes, expressed as adjusted odds ratios with 95% confidence intervals.
| Same month | One month later | Two months later | |
|---|---|---|---|
| Any positive urine (y/n) | 1.07 (0.94 – 1.22) | 1.06 (0.89 – 1.25) | 1.07 (0.92 – 1.24) |
| Treatment interruption (y/n) | 1.09 (0.87 – 1.36) | 1.23 (0.97 – 1.56) | 1.36 (1.16 – 1.59)* |
| 100% counseling adherence (y/n) | 0.88 (0.78 – 1.01) | 0.96 (0.83 – 1.10) | 0.89 (0.78 – 1.03) |
p < 0.001
4. DISCUSSION
An extremely high rate of reexposure to traumatic events was found in this sample of patients with severe substance use disorder and comorbid psychiatric disorders. Traumatic events are extreme stressors that are accompanied by a number of negative sequelae, including loss of tangible resources, emotional and sometimes physical distress, and possible development of psychiatric symptoms and disorders, including PTSD. The present study suggests that as many as 1 in 5 opioid-dependent patients in treatment experience a new traumatic event each month, adding considerable challenges to their ability to cope with the demands of daily life and recovery. Whether people using other drugs would have lower rates of reexposure is not known, although opioid use has been associated with greater lifetime traumatic event exposure (Lawson et al., 2013). More than half the sample had experienced at least one traumatic event during 6 months and, when juxtaposed with the monthly rate, suggests that reexposure was not limited to a small number of higher risk patients. Somewhat heartening is the fact that the monthly trauma reexposure rate in this treatment sample is lower than the rate reported in syringe exchange participants with less exposure to treatment and higher rates of drug use (Peirce et al., 2012), although the cumulative reexposure rate is similar. The reasons for the high rate of traumatic event reexposure remain unknown, although treatment nonparticipation and higher rates of drug use are strong candidates for future investigation (Peirce et al., 2014).
Traumatic event reexposure was associated with poorer treatment response; specifically, a higher risk of short-term treatment interruption. This is the first study to document the disruptive impact of traumatic events on substance use disorder treatment that occur in addition to the other well-known sequelae of trauma. Treatment interruption raises the risk of opiate use in the context of methadone withdrawal, often results in treatment discharge, and may presage longer interruptions or permanent attrition. Attrition from methadone maintenance treatment is strongly associated with subsequent relapse to drug use (Teesson et al., 2008). Although this study found no direct proximal relationship between traumatic events and drug use, there may be an increased risk later secondary to leaving treatment. Results of this study also suggest that different types of traumatic events could be associated with different patterns of negative outcomes. The two traumatic event exemplars examined here were chosen because they are qualitatively and quantitatively different in many ways, including perceived responsibility for the event, possible relationship to drug-related activities, resources needed to cope with the event, and risk for related psychiatric symptoms or disorder (Ozer et al., 2003). In this study, a traumatic event happening to a loved one was associated with a likelihood of complete treatment interruption around the time of the event, while assault was associated with poorer counseling adherence later. Although data were not collected from participants about their reasons for nonadherence with treatment after these traumatic events, we infer that treatment activities became a lower priority than competing activities for some period of time. Even if the competing activity was pro-social (e.g., spending time with family after a traumatic death), it separated participants from a main source of recovery support and participation at times when they are likely to most benefit from help coping with these challenging events (Olff et al., 2005).
PTSD symptom severity was also related to episodes of treatment interruption, although to a lesser extent and later than the effect of traumatic events. The absence of a direct relationship between PTSD symptoms and drug use found in other studies was supported here, although we note again that the risk of drug use typically increases after a patient leaves treatment. All participants were offered psychiatric care that may have resulted in PTSD symptom scores in the lower deciles later in treatment, but it is unlikely that the nature of the relationship between PTSD symptoms and treatment outcomes would be significantly affected. The present findings for both traumatic events and PTSD fit with a more nuanced interpretation of the potential relationship between PTSD and SUD. The influence of PTSD on SUD and response to treatment appears to be relatively subtle and based primarily on how symptomatic the substance user is. Several studies of PTSD treatment in SUD patients have suggested that improvements in PTSD symptoms precede improvements in SUD symptoms (Hien et al., 2010; Morgan-Lopez et al., 2014), which supports this conceptualization. It is also possible that studies that appeared to show a stronger direct relationship between PTSD and SUD were instead capturing the effect of new traumatic event exposure, which appears to be rather frequent and has not commonly been assessed. Finally, PTSD itself conveys numerous negative consequences that are very relevant for substance users, including poor social support, emotional distress, risk for suicide, poor somatic health, and poor overall quality of life, all of which have been associated with a higher relapse risk for SUD patients with PTSD (Norman et al., 2007; Ouimette et al., 2007; Sharkansky et al., 1999). These and other findings strongly support the need for continued assessment of and treatment for PTSD, despite its relatively subtle direct relationship to substance abuse treatment outcomes.
The primary limitation of the present study is that results may not fully generalize to other populations of substance users. The sample was unique in two important ways that might impact generalizability: 1) it is comorbid for opioid dependence and at least one other psychiatric disorder, and 2) it is an inner-city Baltimore sample, which is characterized by high rates of poverty and violent crime. It is probable that the rate and effect of traumatic event reexposure would be different in a less severely impaired population with fewer environmental and psychosocial stressors. But it is also possible that other severely psychiatrically impaired populations, who commonly endorse high rates of lifetime traumatic event exposure (Grubaugh et al., 2011), would have significant rates of reexposure as well. We also note that only a few indicators of treatment response were examined in the present study and a different pattern could emerge if other outcome variables were included. For example, we used a categorical definition of drug use based on objective urinalysis test results; a semi-continuous measure such as self-reported days of use might show different outcomes. Finally, the study was conducted using the then-current DSM-IV-TR definitions for traumatic events and PTSD symptoms, and so may not be generalizable to the current DSM-V. These limitations notwithstanding, the prospective longitudinal design and careful repeated assessments are substantial strengths of the current study that add to its value.
Traumatic event reexposure may be more common in SUD treatment than previously recognized. Even a reexposure rate lower than the 18% per month found in this study would be troubling, if only because traumatic events convey serious negative effects in substance users and non-users alike. The burden of new traumatic events in substance users additionally appears to disrupt their treatment course, resulting in increased treatment interruption, which is likely to worsen their course of recovery. Interventions to reduce traumatic event reexposure in this population or at least to ameliorate the negative effects of reexposure on treament participation might be very beneficial. We are not aware of any such interventions under development or in use in SUD treatment settings, although some have been tested in emergency medicine settings or post-disaster mental health care (e.g., Smith et al., 2013; Walton et al., 2010). Interventions such as Psychological First Aid (National Child Traumatic Stress Network and National Center for PTSD, 2006) could be adapted for provision in substance abuse treatment settings where new traumatic events seem common and patients may be less able to cope effectively with them on their own.
highlights.
Traumatic event reexposure is relatively common in methadone maintenance patients.
Traumatic event reexposure increases the risk of later treatment interruption.
Posttraumatic stress disorder severity is associated with treatment interruption.
Drug use and counseling adherence are unaffected by either events or symptoms.
Acknowledgements
The authors wish to thank the ATS assessment team for their years of passion and hard work conducting research with a difficult and needy population.
Role of Funding Source: This research was supported by the following grants: NIH-NIDA K23DA015739 (Peirce) and NIH-NIDA R01DA016375 (Brooner). The sponsor had no involvement in study design or collection, analysis, or interpretation of data, nor in the writing or submission of this report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors: Jessica Peirce proposed the study, analyzed the results, and wrote drafts of the manuscript. Robert Brooner and Michael Kidorf modified the study design, directed data collection, provided feedback on results, and revised the manuscript. Van King monitored compliance with data collection and contributed to manuscript revision. All authors have approved the final submission.
Author Disclosures
Effect of traumatic event reexposure and PTSD on substance use disorder treatment response
Conflict of Interest: No conflict declared.
REFERENCES
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders—Text Revision. fourth ed. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. fifth ed. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- Breslau N, Davis GC, Andreski P. Risk factors for PTSD-related traumatic events: a prospective analysis. Am. J. Psychiatry. 1995;152:529–535. doi: 10.1176/ajp.152.4.529. [DOI] [PubMed] [Google Scholar]
- Brooner RK, Kidorf MS, King VL, Peirce J, Neufeld K, Stoller K, Kolodner K. Managing psychiatric comorbidity within versus outside of methadone treatment settings: a randomized and controlled evaluation. Addiction. 2013;108:1942–1951. doi: 10.1111/add.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooner RK, Kidorf MS, King VL, Stoller KB, Peirce JM, Bigelow GE, Kolodner K. Behavioral contingencies improve counseling attendance in an adaptive treatment model. J. Subst. Abuse Treat. 2004;27:223–232. doi: 10.1016/j.jsat.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Brown PJ, Stout RL, Mueller T. Posttraumatic stress disorder and substance abuse relapse among women: a pilot study. Psychol. Addict. Behav. 1996;10:124–128. [Google Scholar]
- Coffey SF, Dansky BS, Falsetti SA, Saladin ME, Brady KT. Screening for PTSD in a substance abuse sample: psychometric properties of a modified version of the PTSD Symptom Scale self-report. J. Trauma. Stress. 1998;11:393–399. doi: 10.1023/A:1024467507565. [DOI] [PubMed] [Google Scholar]
- Cohen LR, Field C, Campbell AN, Hien DA. Intimate partner violence outcomes in women with PTSD and substance use: a secondary analysis of NIDA Clinical Trials Network “Women and Trauma” multi-site study. Addict. Behav. 2013;38:2325–2332. doi: 10.1016/j.addbeh.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dabbs C, Watkins EY, Fink DS, Eick-Cost A, Millikan AM. Opiate-related dependence/abuse and PTSD exposure among the active-component U.S. military, 2001 to 2008. Mil. Med. 2014;179:885–890. doi: 10.7205/MILMED-D-14-00012. [DOI] [PubMed] [Google Scholar]
- Driessen M, Schulte S, Luedecke C, Schaefer I, Sutmann F, Ohlmeier M, Kemper U, Koesters G, Chodzinski C, Schneider U, Broese T, Dette C, Havemann-Reinicke U, TRAUMAB-Study Group Trauma and PTSD in patients with alcohol, drug, or dual dependence: a multi-center study. Alcohol. Clin. Exp. Res. 2008;32:481–488. doi: 10.1111/j.1530-0277.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- Falsetti SA, Resnick HS, Resick PA, Kilpatrick DG. The Modified PTSD Symptom Scale: a brief self-report measure of posttraumatic stress disorder. Behav. Ther. 1993;16:161–162. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM–IV Axis I disorders (Patient ed.) Biometrics Research, New York State Psychiatric Institute; New York: 1998. [Google Scholar]
- Gilbert LK, Breiding MJ, Merrick MT, Thompson WW, Ford DC, Dhingra SS, Parks SE. Childhood adversity and adult chronic disease: an update from ten states and the District of Columbia, 2010. Am. J. Prev. Med. 2015;48:345–349. doi: 10.1016/j.amepre.2014.09.006. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch. Gen. Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubaugh AL, Zinzow HM, Paul L, Egede LE, Frueh BC. Trauma exposure and posttraumatic stress disorder in adults with severe mental illness: a critical review. Clin. Psychol. Rev. 2011;31:883–899. doi: 10.1016/j.cpr.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Jiang H, Campbell AN, Hu MC, Miele GM, Cohen LR, Brigham GS, Capstick C, Kulaga A, Robinson J, Suarez-Morales L, Nunes EV. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA's Clinical Trials Network. Am. J. Psychiatry. 2010;167:95–101. doi: 10.1176/appi.ajp.2009.09091261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Nunes E, Levin FR, Fraser D. Posttraumatic stress disorder and short-term outcome in early methadone treatment. J. Subst. Abuse Treat. 2000;19:31–37. doi: 10.1016/s0740-5472(99)00088-4. [DOI] [PubMed] [Google Scholar]
- Hildebrand A, Behrendt S, Hoyer J. Treatment outcome in substance use disorder patients with and without comorbid posttraumatic stress disorder: a systematic review. Psychother. Res. 2014;26:1–18. doi: 10.1080/10503307.2014.923125. [DOI] [PubMed] [Google Scholar]
- Korte JE, Rosa CL, Wakim PG, Perl HI. Addiction treatment trials: how gender, race/ethnicity, and age relate to ongoing participation and retention in clinical trials. Subst. Abuse Rehabil. 2011;2:205–218. doi: 10.2147/SAR.S23796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol. Assess. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Lawson KM, Back SE, Hartwell KJ, Moran-Santa MM, Brady KT. A comparison of trauma profiles among individuals with prescription opioid, nicotine, or cocaine dependence. Am. J. Addict. 2013;22:127–131. doi: 10.1111/j.1521-0391.2013.00319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Magruder KM, Ouyang B, Miller S, Tilley BC. Retention of under-represented minorities in drug abuse treatment studies. Clin. Trials. 2009;6:252–260. doi: 10.1177/1740774509105224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancino M, Curran G, Han X, Allee E, Humphreys K, Booth BM. Predictors of attrition from a national sample of methadone maintenance patients. Am. J. Drug Alcohol Abuse. 2010;36:155–160. doi: 10.3109/00952991003736389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier A, Lambert-Harris C, McGovern MP, Xie H, An M, McLeman B. Co-occurring prescription opioid use problems and posttraumatic stress disorder symptom severity. Am. J. Drug Alcohol Abuse. 2014;40:304–311. doi: 10.3109/00952990.2014.910519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills KL, Lynskey M, Teesson M, Ross J, Darke S. Post-traumatic stress disorder among people with heroin dependence in the Australian treatment outcome study (ATOS): prevalence and correlates. Drug Alcohol Depend. 2005;77:243–249. doi: 10.1016/j.drugalcdep.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, Darke S. The impact of post-traumatic stress disorder on treatment outcomes for heroin dependence. Addiction. 2007;102:447–454. doi: 10.1111/j.1360-0443.2006.01711.x. [DOI] [PubMed] [Google Scholar]
- Morgan-Lopez AA, Saavedra LM, Hien DA, Campbell AN, Wu E, Ruglass L, Patock-Peckham JA, Bainter SC. Indirect effects of 12-session seeking safety on substance use outcomes: overall and attendance class-specific effects. Am. J. Addict. 2014;23:218–225. doi: 10.1111/j.1521-0391.2014.12100.x. [DOI] [PubMed] [Google Scholar]
- National Child Traumatic Stress Network and National Center for PTSD Psychological First Aid: Field Operations Guide. (2nd Edition) 2006 Available on: www.nctsn.org and www.ncptsd.va.gov.
- Norman SB, Tate SR, Anderson KG, Brown SA. Do trauma history and PTSD symptoms influence addiction relapse context? Drug Alcohol Depend. 2007;90:89–96. doi: 10.1016/j.drugalcdep.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Norman SB, Tate SR, Wilkins KC, Cummins K, Brown SA. Posttraumatic stress disorder's role in integrated substance dependence and depression treatment outcomes. J. Subst. Abuse Treat. 2010;38:346–355. doi: 10.1016/j.jsat.2010.01.013. [DOI] [PubMed] [Google Scholar]
- Olff M, Langeland W, Gersons BP. The psychobiology of PTSD: coping with trauma. Psychoneuroendocrinology. 2005;30:974–982. doi: 10.1016/j.psyneuen.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Ouimette P, Coolhart D, Funderburk JS, Wade M, Brown PJ. Precipitants of first substance use in recently abstinent substance use disorder patients with PTSD. Addict. Behav. 2007;32:1719–1727. doi: 10.1016/j.addbeh.2006.11.020. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol. Bull. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Peirce JM, Brooner RK, Kolodner K, Schacht RL, Kidorf MS. Prospective effects of traumatic event re-exposure and post-traumatic stress disorder in syringe exchange participants. Addiction. 2013;108:146–153. doi: 10.1111/j.1360-0443.2012.04003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirce JM, Burke CK, Stoller KB, Neufeld KJ, Brooner RK. Assessing traumatic event exposure: comparing the Traumatic Life Events Questionnaire to the Structured Clinical Interview for DSM-IV. Psychol. Assess. 2009;21:210–218. doi: 10.1037/a0015578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirce JM, Kindbom KA, Waesche MC, Yuscavage AS, Brooner RK. Posttraumatic stress disorder, gender, and problem profiles in substance dependent patients. Subst. Use Misuse. 2008;43:596–611. doi: 10.1080/10826080701204623. [DOI] [PubMed] [Google Scholar]
- Peirce JM, Kolodner K, Brooner RK, Kidorf MS. Traumatic event re-exposure in injecting drug users. J. Urban Health. 2012;89:117–128. doi: 10.1007/s11524-011-9619-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirce JM, Schacht RL, Brooner RK, King VL, Kidorf MS. Prospective risk factors for traumatic event reexposure in community syringe exchange participants. Drug Alcohol Depend. 2014;138:98–102. doi: 10.1016/j.drugalcdep.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Brown PJ, Kahler CW. Substance use and posttraumatic stress disorders: symptom interplay and effects on outcome. Addict. Behav. 2004;29:1665–1672. doi: 10.1016/j.addbeh.2004.02.061. [DOI] [PubMed] [Google Scholar]
- Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug Alcohol Depend. 2005;77:251–258. doi: 10.1016/j.drugalcdep.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Sharkansky EJ, Brief DJ, Peirce JM, Meehan JC, Mannix LM. Substance abuse patients with posttraumatic stress disorder (PTSD): identifying specific triggers of substance use and their associations with PTSD symptoms. Psychol. Addict. Behav. 1999;13:89–97. [Google Scholar]
- Smith R, Dobbins S, Evans A, Balhotra K, Dicker RA. Hospital-based violence intervention: risk reduction resources that are essential to success. J. Trauma Acute Care Surg. 2013;74:976–980. doi: 10.1097/TA.0b013e31828586c9. [DOI] [PubMed] [Google Scholar]
- Teesson M, Mills K, Ross J, Darke S, Williamson A, Havard A. The impact of treatment on 3 years’ outcome for heroin dependence: findings from the Australian Treatment Outcome Study (ATOS). Addiction. 2008;103:80–8. doi: 10.1111/j.1360-0443.2007.02029.x. [DOI] [PubMed] [Google Scholar]
- Trafton JA, Minkel J, Humphreys K. Opioid substitution treatment reduces substance use equivalently in patients with and without posttraumatic stress disorder. J. Stud. Alcohol. 2006;67:228–235. doi: 10.15288/jsa.2006.67.228. [DOI] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010;304:353–527. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Keane TM. The criterion A problem revisited: controversies and challenges in defining and measuring psychological trauma. J. Trauma. Stress. 2007;20:107–121. doi: 10.1002/jts.20210. [DOI] [PubMed] [Google Scholar]