Abstract
The inclusion of engineering ideas and approaches makes medicine a quantitative and systems-based discipline that facilitates precision diagnostics and therapeutics to improve health care delivery for all.
Engineering and technological advances have played a major role in medical discoveries and their clinical translation since the invention of x-rays by Roentgen in 1895. Since then, many of the Nobel Prizes have been awarded for novel technology development that led to improvements in health care, including polymerase chain reaction, magnetic resonance imaging, several forms of spectroscopy and microscopy, and human genome sequencing. This year’s Nobel Prize in Chemistry, for the development of super-resolution microscopy and its biomedical application, further exemplifies how engineering is broadly advancing our basic knowledge and its medical translation. The recent list of the top 100 cited papers includes many technological innovations and tools that have accelerated biology and medicine (1).
Groundbreaking inventions in mechanics, optics, materials, electronics, and computing in the past decades have ideally positioned the integration of the life sciences and engineering to address major challenges in medicine and health care. With uneven access to modern medicine across the globe, there is a pressing need for democratization of health care to deliver high-quality, cost-effective care; engineering can play a major role in meeting this critical need by enabling technologies that allow early detection, precise diagnostics, mobile health, and data-sharing for the realization of precision medicine.
THE NEXT FRONTIER
Major engineering advances in health care over the past few decades have been summarized by the American Institute for Medical and Biological Engineering (http://aimbe.org/milestones-of-innovation). Recent progresses at the interface of biology, medicine, and engineering have provided us with state-of-the-art technologies that allow diagnosis, monitoring, treatment, and prevention of human diseases and have facilitated the maintenance and enhancement of health. For instance, valve prostheses, vascular stents, and heart rhythm control systems have improved interventional cardiology for the treatment of valvular disease, obstructive atherosclerosis, and arrhythmias. Modern biomedical imaging techniques and novel biosensors have enabled the noninvasive detection and dynamic tracking of clinically relevant indicators, such as circulating tumor cells, microRNA, and viral DNA. Such sensors allow for early diagnosis and monitoring of disease status and therapeutic efficacy in every field from cancer to metabolic disease to transplant medicine. Noninvasive biosensors and portable devices have begun to play an important role in both healthy lifestyles and continuous disease monitoring in the emerging concept of “mobile health,” or mHealth (2, 3). For example, some pharmacies now transmit medical data and video images to a health care provider for disease management. As a next step, engineering will play an important role in the multiscale integration of such physiological measurements with molecular, –omic, and cellular data to provide a comprehensive view of personal health, susceptibility to disease, and tailored therapeutics.
Another field that promises to bring modern medicine to a personalized level is stem cell engineering. We can now transform an individual’s somatic cells into induced pluripotent stem cells (iPSCs) and into almost any lineage, thus making possible the study of disease mechanisms. iPSC technology allows for personalized disease modeling, which can then lead to optimized therapeutics. Engineering advances also provide the fundamental basis to explore the physical forces that shape the cell and tissue microenvironments that modulate physiological and pathological functions.
These new frontiers of translational advances in engineering and technology have resulted in substantial clinical impact to date, but the potential has not been fully realized. State-of-the-art technologies should be more widely available to patients—especially those among the resource-limited, disadvantaged, and underrepresented populations—and at affordable costs. Achieving this vision of higher-quality health care globally while containing or reducing its rising costs presents conflicting demands, and it is a challenge for engineering and medicine to tackle these important socioeconomic problems. The consumer electronics industry was able to address similar challenges through technological innovations, as stipulated by “Moore’s Law”—in which increasing functionality is accompanied by an adjusted lower cost and increased usage.
In view of the continuous rise in health care costs, we need to effectively create the equivalent of a Moore’s Law for health care delivery, in which technological innovations should reduce cost, increase quality, and democratize health care delivery. Although the differences in the health care and electronics industries do not allow the quantitative transfer of Moore’s Law to health care, the principle is still applicable. New engineering approaches and technologies should be integrated into medicine and health care delivery to reduce the cost of development, manufacturing, and dissemination, thus maximizing the benefit to the patient. For example, the reduction in cost of genome sequencing that resulted from technological improvements has now made sequencing available to patients for cancer diagnostics and management. Similarly, mobile health technologies promise to reduce costs by bringing diagnostics to patients for management of health and wellness.
EDUCATING AT THE FRONTIER
The U.S. National Institutes of Health (NIH) has steadily increased funding for biomedical engineering (as well as other areas of engineering) since 2000, in comparison with NIH funding as a whole, suggesting an emphasis on engineering in health research (Fig. 1). In parallel with the incorporation of engineering in biomedical research, medical education should also integrate engineering principles. Traditionally, medical research and practice have not included the principles and techniques used in engineering, and the differences in the educational programs and cultures between medicine and engineering led to their dichotomy, with relatively few interactions. In recent years, however, it has been increasingly recognized that the full understanding of biological processes and the effective management of clinical conditions require quantitative and time-variant considerations, which are the hallmarks of engineering, in addition to feedback control, systems approaches, and multiscale modeling. The cultural differences between biomedicine and engineering are being narrowed, but there is still a need to accelerate the cross-fertilization of the cultures of engineering and medicine so that the engineers are cognizant of the critical problems and challenges in clinical medicine (4, 5), while the clinicians are appreciative of the quantitative and systems aspects of biomedical research and education.
Fig. 1. NIH funding to biomedical and other engineering disciplines.
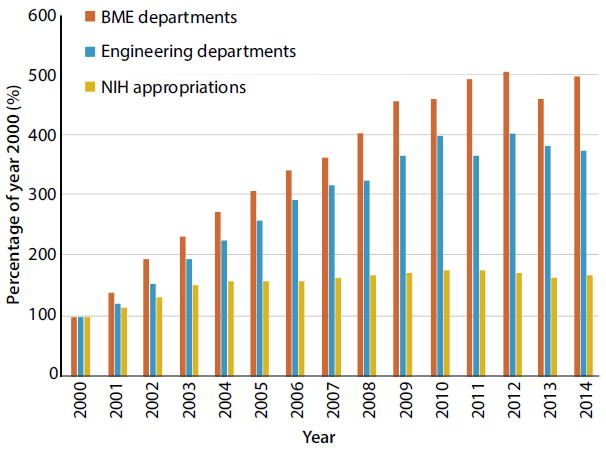
The graph also includes NIH appropriation, from 2000 to 2014, plotted as percentages of year 2000. [Data provided by T. Merchak (NIBIB)]
Several approaches can achieve this goal of intertwining medical and engineering education and training. One option, already in practice but with limitation in numbers, is to have individuals trained in both disciplines, such as an M.D.-Ph.D. majoring in bioengineering. New models of financial support for the physician-engineers need to be developed to further incentivize and encourage students to choose this career path. The current financial support for M.D.-Ph.D. training comes primarily from the NIH. Although it is desirable to increase the government support, there is a critical need for additional sources of support for this important group of the future generation of health care personnel from foundations and other private sources. The recent emergence of the professional Master’s programs in translational medicine, clinical sciences, and medical devices also provides important sources of training of health care personnel at the interface of engineering and medicine (6). There has been an increase in development of these programs, as well as postgraduate biomedical technology innovation training programs, not only in the United States but also in Europe and other parts of the world.
Another option is to train teams of engineers and clinicians who understand each other’s culture and language so that they can communicate and collaborate effectively to practice engineering-based translational medicine. Several federal and private foundation programs have been created with this goal in mind. An example is the Howard Hughes Medical Institute (HHMI)–National Institute of Biomedical Imaging and Bio-engineering (NIBIB) Interfaces program, which created 10 new university curricula to educate and train graduate students to be the next generation of team scientists (www.hhmi.org/programs/hhmi-nibib-interfaces-initiative). The Institutes of Engineering in Medicine at several universities contribute substantially to such team efforts.
A third option is a new engineering-based medical education paradigm that includes engineering principles and the quantitative sciences in addition to clinical and basic medical sciences. Hence, a new medical curriculum—at the nexus of engineering, medicine, and biology and based on a solid grounding of math, physics, and chemistry—is the next educational frontier for translational medicine aiming at improving human health and quality of life. Medical education should incorporate more math and physics, whereas engineering education should include physiology and other medical sciences. In this way, physicians will be comfortable using new technologies and engineering approaches to benefit their patients, and engineers will understand the unmet clinical needs and design effective solutions. The first example of this approach is the most recent establishment of a college of medicine at the University of Illinois at Urbana-Champaign (UIUC) in partnership with Carle Foundation Hospital, focused from the beginning on the intersection of engineering and medicine (www.medicine.illinois.edu)
We believe that this major change toward a curriculum incorporating engineering into medicine is possible. Just as the bioengineering curriculum has evolved over the past three decades, new pedagogical approaches for the medical curriculum can be developed by fusing engineering and medicine to establish the foundations of systems and precision medicine. This could be achieved by revamping the first two years of medical school—for instance, by integrating systems engineering perspectives into medicine; using modeling, simulation, and visualization to teach and demonstrate biological and medical examples; and integrating the latest advances in data sharing and curating, imaging, genomics, and cellular and molecular engineering into the curriculum. The third and fourth years provide an ideal opportunity for innovation; problem-solving by using engineering, technology, and computing approaches; and team projects with medical and engineering students working together to solve translational problems. Physician-innovators can be taught not only to learn the complexities of the clinical and medical ecosystems but also to improve and reengineer them.
PLAYING THE PART
Institutions of higher education, funding agencies, industry, and professional societies need to work together to integrate the frontiers of engineering into medicine in promoting translational research and education. Funding of academic translational centers that join engineering and medicine and of training programs (M.D.-Ph.D. and Master’s), including public-private partnerships, could be pivotal in enhancing the goal-oriented translational research. Professional societies can facilitate the promotion of the quantitative and engineering concepts in the medical curriculum and help to transform medicine as a quantitative discipline. Project-based, self-motivated learning in the medical curriculum could be performed in collaboration with industry so that the solutions developed would lead to translatable innovations that have a licensing and commercialization pathway. Academia-industry consortia could develop programs to better educate the translational workforce.
Because the ultimate goal of medicine is to improve human health and well-being, any new paradigm for educating and training physicians and engineers must also encompass topics related to the humanities and social sciences, such as ethics, teamwork, industrial experience, and regulatory science. Physician-scientists/engineers need to be grounded in compassion and should be knowledgeable of social, cultural, and translational factors that influence (and sometimes limit) health care delivery. Medical education is beginning to take cues from the innovative science, technology, engineering, and math (STEM) programs, which use instruction inversion, group learning, real-world problem solving, and peers as educational resources (7). This approach would make it possible for medical students to learn essential subjects without lengthening the education process.
A NEW ERA
On 20 January 2015, President Obama launched a “Precision Medicine Initiative” to realize cures for diseases and to personalize health (www.whitehouse.gov/precisionmedicine). In an accompanying perspective on this initiative, and the challenges and promise of precision medicine, NIH director Francis Collins and NCI director Harold Varmus challenged the next generation of scientists to develop creative new approaches for detecting, measuring, and analyzing a wide range of biomedical information (8). We posit that the integration of engineering into medicine, and medicine into engineering—until boundaries vanish—will play a critical role in achieving the broad and specific goals of this exciting new initiative.
Engineers can help realize the vision of high-quality, precision, and quantitative medicine while also reducing health care costs. Just as the revolution in medicine created by the advent of molecular biology in the past century, engineering will be the new driving force for the progress of medical research and education in this century and beyond. Robert Goddard, an aerospace pioneer, once said, “It is difficult to say what is impossible, for the dream of yesterday is the hope of today and the reality of tomorrow.” is certainly true, and it is the collaboration between engineering and medicine that will turn our dreams in health care into the reality of tomorrow.
Acknowledgments
We thank T. Merchak (NIBIB) for providing the data for Fig. 1 and S. Subramaniam (University of California, San Diego) for valuable comments and suggestions. We acknowledge the Grainger Engineering Breakthroughs Initiative at UIUC for sponsoring the Frontiers in Bioengineering Workshop, where the topics in this article were discussed (http://graingerinitiative.engineering.illinois.edu/frontiersinbioengineering).
REFERENCES AND NOTES
- 1.Van Noorden R, Maher B, Nuzzo R. The top 100 papers. Nature. 2014;514:550–553. doi: 10.1038/514550a. [DOI] [PubMed] [Google Scholar]
- 2.Kim D-H, Lu N, Ma R, Kim Y-S, Kim R-H, Wang S, Wu J, Won S-M, Tao H, Islam A, Yu K-J, Kim T-I, Chowd-hury R, Ying M, Xu L, Li M, Chung H-J, Keum H, Mc-Cormick M, Liu P, Zhang Y-W, Omenetto FG, Huang Y, Coleman T, Rogers JA. Epidermal electronics. Science. 2011;333:838–843. doi: 10.1126/science.1206157. [DOI] [PubMed] [Google Scholar]
- 3.Danaher BG, Brendryen H, Seeley JR, Tyler MS, Woolley T. From black box to toolbox: Outlining device functionality, engagement activities, and the pervasive information architecture of mHealth interventions. Inter-net Interv. 2015;2:91–101. doi: 10.1016/j.invent.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yock PG, Brinton TJ, Zenios SA. Teaching biomedical technology innovation as a discipline. Sci Transl Med. 2011;3 doi: 10.1126/scitranslmed.3002222. 92cm18. [DOI] [PubMed] [Google Scholar]
- 5.Meyers FJ, Pomeroy C. Creating the future biomedical research workforce. Sci Transl Med. 2011;3 doi: 10.1126/scitranslmed.3003209. 102fs5. [DOI] [PubMed] [Google Scholar]
- 6.Kurpinski K, Johnson T, Kumar S, Desai T, Li S. Mastering translational medicine: Interdisciplinary education for a new generation. Sci Transl Med. 2014;6 doi: 10.1126/scitranslmed.3006858. 218fs2. [DOI] [PubMed] [Google Scholar]
- 7.Maton KI, Pollard SA, McDougall Weise TV, Hrabowski FA. The Meyerhoff Scholars Program: A strengths-based institution wide approach to increasing diversity in STEM. Mt Sinai J Med. 2012;79:610–623. doi: 10.1002/msj.21341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med. 2015;372:793–795. doi: 10.1056/NEJMp1500523. [DOI] [PMC free article] [PubMed] [Google Scholar]


